Abstract
Objective
This integrative review identifies and analyzes the extant literature to examine the integration of social determinants of health (SDoH) domains into electronic health records (EHRs), their impact on risk prediction, and the specific outcomes and SDoH domains that have been tracked.
Materials and Methods
In accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines, we conducted a literature search in the PubMed, CINAHL, Cochrane, EMBASE, and PsycINFO databases for English language studies published until March 2020 that examined SDoH domains in the context of EHRs.
Results
Our search strategy identified 71 unique studies that are directly related to the research questions. 75% of the included studies were published since 2017, and 68% were U.S.-based. 79% of the reviewed articles integrated SDoH information from external data sources into EHRs, and the rest of them extracted SDoH information from unstructured clinical notes in the EHRs. We found that all but 1 study using external area-level SDoH data reported minimum contribution to performance improvement in the predictive models. In contrast, studies that incorporated individual-level SDoH data reported improved predictive performance of various outcomes such as service referrals, medication adherence, and risk of 30-day readmission. We also found little consensus on the SDoH measures used in the literature and current screening tools.
Conclusions
The literature provides early and rapidly growing evidence that integrating individual-level SDoH into EHRs can assist in risk assessment and predicting healthcare utilization and health outcomes, which further motivates efforts to collect and standardize patient-level SDoH information.
Keywords: social determinants of health, electronic health records, behavioral determinants, social factors, systematic review, risk prediction
INTRODUCTION
Social determinants of health (SDoH) are “conditions in which people are born, grow, live, work, and age,”1 and they involve “the complex, integrated, and overlapping social structures and economic systems that are responsible for most health inequalities.”2,3 Healthy People 2020 organizes SDoH around 5 key domains: (1) economic stability, (2) education, (3) health and health care, (4) neighborhood and built environment, and (5) social and community context.4 As population health becomes an important focus of health care delivery, SDoH are increasingly seen as critical factors for identifying potential upstream drivers of poor outcomes and higher costs.5,6 While these are often conflated with social risk factors, which are disadvantageous social conditions that may result in poor health outcomes,7 this review addresses social and behavioral determinants that affect everyone. With SDoH information, it is anticipated that health systems and professionals can classify the complexity of their patients, identify appropriate interventions to meet various needs, and transform care with integrated services and community partnerships to improve health outcomes and reduce health disparities, while saving costs.8–11
The digitization of clinical records presents a new opportunity to integrate SDoH into electronic health records (EHRs) to enhance care delivery and population health.12,13 The 2009 U.S Health Information Technology for Economic and Clinical Health Act incentivized the adoption of EHRs throughout the country. Today, virtually all hospitals and nearly 9 in 10 office-based physicians have adopted an EHR.14,15 With widespread adoption of EHRs, policy is now shifting toward the use of EHR technology in a meaningful manner. Meaningful use criteria were implemented by the Medicare and Medicaid EHR Incentive Programs (now known as the Promoting Interoperability Programs) in 3 time-bound phases. Beginning in 2011, the first 2 stages emphasized capturing data (eg, patients’ medical history, medication orders, vital signs, laboratory results, radiology reports, physician and nurse notes) and optimizing clinical workflows, respectively. The third stage, in 2017, called for all hospitals and eligible healthcare professionals to demonstrate continuous quality improvement of care and elimination of healthcare inequality across all groups.16,17 The integration of SDoH into EHR systems will be central for healthcare institutions to meet Stage 3 objectives and avoid reductions to their Medicare payments for failing to do so.13 More and more, health institutions and clinicians are exploring how to capture data related to social determinants in their EHRs and how to incorporate SDoH-related referral and intervention into routine care, with the goal to assess their quality performance and manage the health of not only individual patients but also of populations.18–21
EHRs systematically collect clinical information about patients such as medical history, vital signs, laboratory tests and results, and medication orders. Nonclinical determinants of health can manifest in the structured data elements such as age, race, ethnicity, and diagnosis codes (eg, homelessness). Some EHRs also have a few lifestyle domains, such as preferred languages, smoking and alcohol use, in a structured format.22 Information on selected environmental and social domains such as housing, social support, and financial resource strain may also be extracted from EHRs’ unstructured data (eg, free-text physician and nurse notes).22 Yet, EHR-derived SDoH data are not sufficient to constitute a complete and accurate set of SDoH domains, and many social and behavioral determinants that may influence health and mortality are not captured. The expansion beyond the traditional clinical information collected in EHRs to include SDoH data requires the identification of what SDoH data to collect and how and when to collect them, and identifying the extent to which the SDoH data collected can be used in risk prediction and interventions to improve outcomes, such as collecting accurate and complete data on patients’ living arrangements and economic stability (2 major domains of SDoH) in predicting the risk of 30-day hospital readmission.23
Prior literature reviews have explored the effectiveness of interventions targeting SDoH24–26 or the evidence relating to screening for the SDoH in clinical care setting27; however, none have explicitly examined the integration of SDoH into EHRs for the purposes of risk prediction and associated analytics. Other systematic reviews have focused on either a specific domain of SDoH such as food insecurity,28 or interventions to improve SDoH among specific disadvantaged groups29; or on specific health outcomes, such as type 2 diabetes,30 pregnancy among young people,31 and adult all-cause mortality.32 Noteworthy results from these systematic reviews illustrate a dearth of generalizable high-quality evidence on the impact of SDoH interventions in the context of population and public health. In perhaps the closest analog to our work, Golembiewski et al33 conducted a rapid review that was limited to U.S.-based articles published between January 2010 and April 2018 and characterized the extent to which existing research has combined nonclinical data derived from external sources with different clinical datasets. Owing to the rapid growth in adoption of EHRs and the pressing needs in the meaningful use of EHRs as a tool to improve health outcomes, it is essential to better understand the type of determinants, data sources, and measures used effectively in the new context of prediction-assisted, EHR-enabled care delivery.
The purpose of this study is to review and analyze the currently available literature to determine whether SDoH can affect health outcomes through risk prediction and targeted intervention, and which SDoH domains have been tracked in the context of EHRs. We are interested in examining quantitative evidence regarding how SDoH may affect various outcomes that have important implications for healthcare cost and quality, such as disease diagnosis, use of healthcare services, referral and other interventions targeted at SDoH and risk of ER visits, and hospital admission or readmissions. To inform efforts to create national standards for representing SDoH information in EHRs, we also analyze the sources and tools used in the studies to collect and screen domains related to SDoH.
MATERIALS AND METHODS
Search strategy
We followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines34 and the PRISMA-Equity 2012 extension for systematic reviews with a focus on health equity35 to conduct our systematic review. The published literature was searched using strategies created with the help of a university librarian for studies that utilized SDoH in the EHR context. The search strategies were established using a combination of standardized terminologies, keywords, and MeSH (Medical Subject Headings). We aimed to be broad and inclusive by adapting wording of SDoH, such as socioeconomic factors, behavioral factors, nonclinical determinants, health disparity, etc. To verify our coverage of all relevant articles, we also compiled an inclusive list of social and behavioral determinants of health measures to search in the literature based on the conceptual frameworks proposed by the World Health Organization and the U.S. Centers for Disease Control and Prevention, and the nonclinical determinants of health measures used in the existing literature review.33
Table 1 shows the domains and dimensions of the health determinants we cover in the review, and the specific measures of these domains and dimensions can be found in Supplementary Table S1.
Table 1.
Examples of search domains and dimensions
| Domains | Dimensions |
|---|---|
| Economic stability | Income, financial resource, employment, basic needs |
| Neighborhood and built environment | Transportation, neighborhood, living arrangements, food access, environmental conditions |
| Health and health care | Insurance status, behavioral health, mental health |
| Education | Education, language |
| Social and community context | Race/ethnicity, social connections, other status, marital status |
Data sources and searches
We queried PubMed (1948-present), CINAHL (1937-present), PsycINFO (1998-present), EMBASE (1947-present), and Web of Science (1965-present) all through July 15, 2019, then updated on March 31, 2020. We intentionally made the search query as broad as possible to make sure that we extract as many results as possible related to the research questions posed in this systematic review. A total of 6687 articles were identified by searching the databases based on the different variations of EHRs and a combination of the standardized SDoH terminologies and keywords representing specific social and behavioral determinants of health (Supplementary Table S1). Duplicate records were identified using the automatic duplication finder in Mendeley36 and Rayyan37 online review software. We removed 361 duplicates using Mendeley and identified 26 more duplicates using Rayyan, ending up with 6300 unique studies for further screening.
Study selection
To be eligible for inclusion, published research had to meet all of the following 4 criteria:
Peer-reviewed research with full text published in English.
Integrated SDoH information into EHRs.
Examined the impact of integrating SDoH into EHRs.
Quantitative analysis.
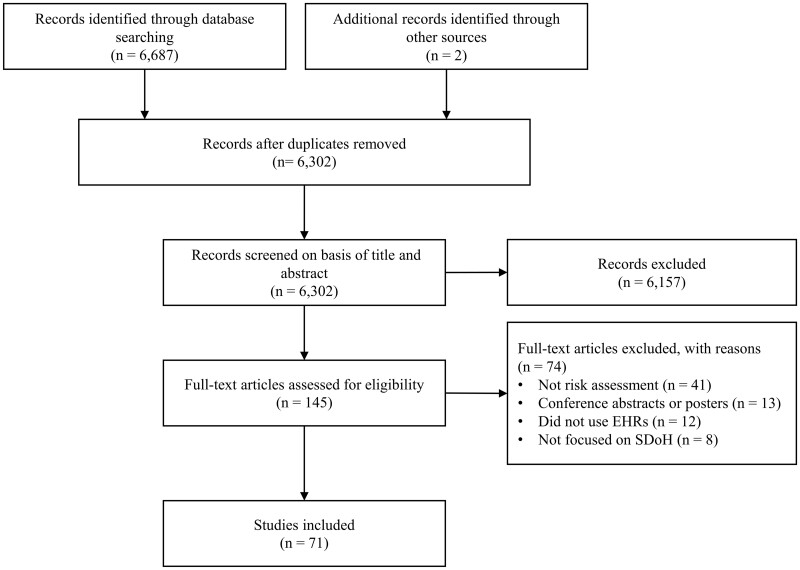
Articles were excluded in 2 stages: a title and abstract review (6157 excluded) and then a full-text review of 143 articles (74 excluded). Studies excluded from the title and abstract screening included (1) systematic reviews/meta-analyses; (2) opinions, commentaries. perspectives, vision articles, guidelines, and protocol articles; (3) qualitative studies; (4) exploratory, conceptual studies, (5) studies prior to 2000; and (6) non–English language studies. During the full-text screening, we excluded conference posters and studies that did not focus on examining the impact of integrating SDoH into EHRs on analysis and risk prediction. This resulted in 69 articles for inclusion. We then used a snowballing technique whereby we searched the reference lists of included articles to identify potentially missed studies that should be considered and searched for the gray literature. We repeated this process on each additional article until no additional articles worthy of inclusion could be identified. This manual search process resulted in 2 more studies added to the pool. At each stage, we resolved conflicts in inclusion or exclusion by discussion and achieving consensus among the 3 independent reviewers. Figure 1 presents our search and screen process.
Figure 1.
Flowchart of literature search and screening process. EHR: electronic health record; SDoH: social determinants of health.
Data extraction and synthesis
From each selected article, we extracted a list of data elements determined by the research team such as year of publication, country of origin, data source, sample size, and level of SDoH measures used, how SDoH information is integrated into EHRs, outcome measures, study method, study purpose, findings, and limitations. Given the heterogeneity within included studies, as well as the lack of standardized or consistent reporting of SDoH domains and outcome measures, meta-analysis was not possible. Therefore, we used narrative synthesis to integrate our findings into descriptive summaries for SDoH and their impact on analysis and risk prediction.
RESULTS
Overall characteristics of the reviewed studies
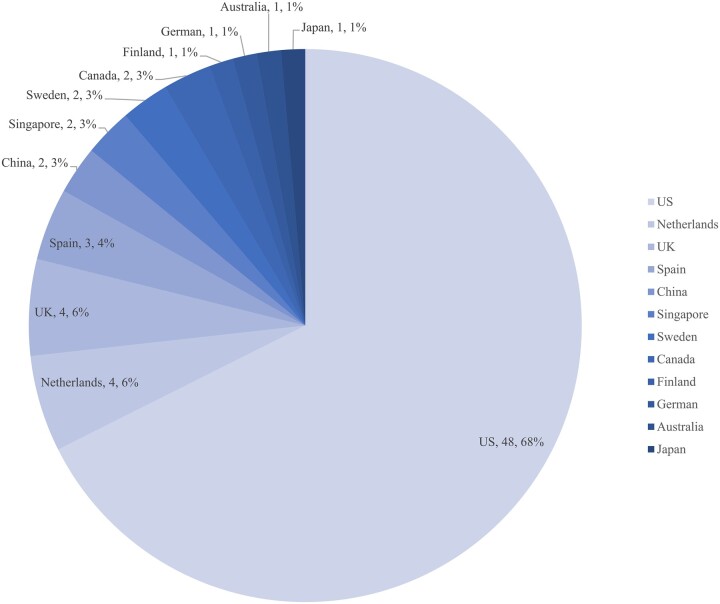
We have summarized the characteristics of the 71 included studies in Table 2. Overall, the literature on integrating SDoH into EHRs is quite new but growing rapidly. All included studies were published between 2008 and 2020, with the majority from 2017 to 2020 (53 studies, or 75%). Most of the studies (68%) were from the United States, and all but 2 studies were from developed countries (Figure 2). There are 2 major approaches reported in the studies to acquire SDoH data: (1) merging SDoH information from external data sources into EHRs and (2) extracting SDoH information from unstructured clinical notes in the EHRs. A total of 56 of the 71 (79%) studies merged SDoH information from external data sources into EHRs, and the most frequently used external data sources were the publicly accessible American Community Survey (ACS) and the U.S. Census. While both the ACS and census data provide neighborhood level SDoH information, the ACS provides more up-to-date information about the social and economic needs of the community at the census-tract or ZIP code level every 5 years and releases estimates at the regional, state, and county levels every year.38 Other studies that merged SDoH into the EHRs used commercial databases such as Nielsen Prime Location39 and the Esri Business Analyst Premium product,40 or initiated their own patient-level health surveys, as in Wagaw et al,41 or community information system, as in Comer et al.42
Table 2.
Characteristics and frequency distribution of the 71 reviewed studies
| Characteristics | n | % |
|---|---|---|
| Publication year | ||
| 2017-2020 | 53 | 75 |
| 2008-2016 | 18 | 25 |
| Major SDoH data source | ||
| ACS or census | 32 | 45 |
| Other health surveys or databases | 24 | 34 |
| EHRs | 15 | 21 |
| SDoH level | ||
| Neighborhood | 41 | 58 |
| Individual | 25 | 35 |
| Both | 5 | 7 |
| Sample size | ||
| <10 000 | 24 | 34 |
| Between 10 000 and 100 000 | 21 | 30 |
| >100 000 | 26 | 37 |
| Outcome | ||
| Disease incidence/diagnosis/health outcome | 41 | 58 |
| Use of healthcare services | 27 | 38 |
| Referral/intervention/prevention of health services | 3 | 4 |
| Type of article | ||
| Association | 58 | 82 |
| Prediction | 13 | 18 |
ACS: American Community Survey; EHR: electronic health record; SDoH: social determinants of health.
Figure 2.
Breakdown of the 71 included articles by country.
Most existing literature (58 studies, or 82%) examined the association between SDoH and outcomes. These studies vary in terms of sample size (from a few hundred to over 6 million observations), region (including a dozen countries), and level of SDoH data (ie, neighborhood-level ACS or census data, individual-level SDoH data extracted from EHRs, and both). However, they all confirmed that SDoH was to some extent associated with outcomes. They found either that better SDoH measures were associated with decreased disease incidence39,43 or improved health intervention44 or that social disadvantages were associated with screening45 or diagnosis,46 use of referral services,47 and adverse health outcomes.48,49
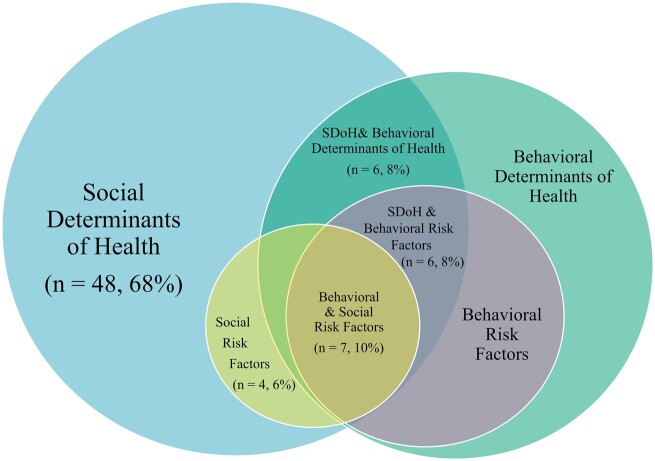
Social and behavioral determinants and risk factors
It is important to note that social (and behavioral) risk factors are sometimes conflated with social (and behavioral) determinants in the rapidly evolving literature. While SDoH affect anyone for better or worse, social risk factors are specific adverse social conditions (eg, homeless, social disadvantage) that are associated with poor health. Further, social risk factors and behavioral risk factors (eg, smoking, lack of exercise) are not the same but can be intertwined. Alderwick and Gottlieb7 provided a timely SDoH lexicon for health care systems. We analyzed the included articles to show how the different terms are utilized in the literature, both as distinct categories as well as intertwined with each other (Figure 3). A total of 68% of the included studies examined SDoH and 6% examined social risk factors. Among the rest of the included studies (26%), 8% examined both social and behavioral determinants of health, another 8% examined SDoH and behavioral risk factors, and 10% examined both social risk factors and behavioral risk factors. Supplementary Table S3 shows the articles that fall into the distinct and intertwined categories. As healthcare initiatives and literature related to the SDoH grow rapidly, greater awareness of this conflation and clarity on key terms and the concepts underlying them could lead to more appropriate usage in future studies and practices.
Figure 3.
Classification of the 71 included articles by coverage. SDoH: social determinants of health.
Added contribution of SDoH in prediction
Thirteen recent articles explicitly examined whether integrating SDoH data into the EHRs can improve risk assessment, prediction, or interventions that address social determinants (Table 3). A total of 85% of these 13 articles were published between 2017 and March 2020. All but 1 study that merged external neighborhood-level SDoH data into the EHRs reported minimum contribution to predictive performance in any of their predictive models, including the prediction for SDoH-related service referrals,50 repeat ED visits,51 hospitalizations, hospital readmissions, and other use of healthcare services.52–54 The only exception found that neighborhood poverty rate was a significant predictor of nonadherence to scheduled screening colonoscopy in multivariate modeling.55 In contrast, the studies that incorporated individual-level SDoH data all reported significantly improved performance, in referrals to a social worker,56 medication adherence,57 risk of hospitalization58 and 30-day rehospitalizations,23 predicted performance of HIV risk assessment,59 and suicide attempts.60,61
Table 3.
Characteristics of the 13 articles on using SDoH for risk prediction
| Characteristics | n | % |
|---|---|---|
| Publication year | ||
| 2017-2020 | 11 | 85 |
| 2012-2016 | 2 | 15 |
| Major SDoH data source | ||
| ACS or Census | 6 | 46 |
| Other health surveys or databases | 2 | 15 |
| EHRs | 5 | 38 |
| SDoH level | ||
| Neighborhood | 6 | 46 |
| Individual | 5 | 38 |
| Both | 2 | 15 |
| Sample size | ||
| <10 000 | 5 | 38 |
| Between 10 000 and 100 000 | 2 | 15 |
| >100 000 | 6 | 46 |
| Outcome | ||
| Disease incidence/diagnosis/health outcome | 3 | 23 |
| Use of healthcare services | 8 | 62 |
| Referral/intervention/prevention of health services | 2 | 15 |
| SDoH contribution to improved prediction | ||
| Contributed | 8 | 62 |
| Minimal contribution | 5 | 38 |
ACS: American Community Survey; EHR: electronic health record; SDoH: Social Determinants of Health.
In summary, the results of our systematic review confirmed that various SDoH measures are associated with health outcomes. However, recent studies that assess whether knowledge of SDoH improves population risk assessment find that linking neighborhood-level (eg, census tract or ZIP code level) information on SDoH may not contribute much more to risk prediction above and beyond what is already provided by the EHR data. It could be due to the lack of variation in demographic characteristics,62 given that these studies are mostly limited to data from a single or 2 EHR systems in 1 geographic region. On the other hand, natural language processing improved predictive models by extracting terms in clinical text indicative of high-risk factors.63–65 Such automated risk prediction methods could leverage longitudinal EHRs alone for population risk assessment and catalyze targeted screening programs, as compared with costly and labor-intensive universal screening.
Table 3. Characteristics of the 13 articles on using SDoH for risk prediction
DISCUSSION
SDoH-EHR integration challenges
EHRs offer tremendous potential to aggregate, analyze, and integrate individual- and community-level data across settings and over time. Integrating SDoH into EHRs can provide a broader perspective on potential drivers of a patient’s health status and can help identify both upstream and downstream approaches for improving the effectiveness of care. There is rapidly growing research on evaluating the impact of both community-level and individual-level SDoH integration in prediction modeling to improve health outcomes and resource utilization.
Information on community-level determinants such as poverty, unemployment, and even air pollution rates is generally available as structured data from the U.S. Census Bureau or other agencies.39,40,66 However, analysis of existing literature shows that such community-level SDoH contributes minimally to the prediction performance, with 1 exception in recent literature that showed a significant impact of neighborhood poverty rate on colonoscopy screening.
While individual-level SDoH data have been found to contribute to prediction performance,51,56,59 they are more challenging to capture accurately. Depending on the outcomes, different social or behavioral measures have been found to be significant in the individual-level prediction articles we reviewed. For instance, individual-level income, housing, employment, and education have been found to contribute to the prediction of 30-day readmissions23; housing stability, drug use, and high-risk sexual activities contributed to predictive performance of HIV risk assessment59; age, substance use, and mental disorders are among the factors that contributed to prediction of suicide attempts60,61; and self-perceived health status was a strong predictor of hospitalization. There are no common measures across these articles that can be recommended as a minimum set of measures to capture and record in the EHR. Further, studies have confirmed that the limited set of SDoH information documented in EHRs (eg, race and ethnicity) is challenged with missing data and other quality issues.67,68 Additionally, individual-level determinants can change rapidly, particularly if patients are successfully referred for appropriate services. The significant gaps in needed electronic health information exchange can hamper the effective collection and use of the ever-changing SDoH information.69
Next, the input of such SDoH information into EHRs is limited to the domain of medical providers.70,71 It is equally important to engage patients in dialogue about their social needs and encourage self-reporting so that providers can ensure that their referrals align with patient priorities and are delivered in an accessible manner. Another key challenge is a lack of consensus on standards for capturing or representing SDoH in EHRs.70 Patient data is siloed in different systems and technology components of the EHRs and must be shared in new ways to enable the effective crosswalking of SDoH data.
Finally, SDoH-EHR integration for predicting risk of adverse events and identifying early intervention opportunities for patients require processes for downstream planning and tools for actionable decisions by providers, particularly if social risk factors are identified for subpopulations, such as homelessness and food insecurity.72 Additionally, workforce training, capacity planning, community resource identification, and easy allocation of such resources at the point of care and similar efforts are necessary for effective and efficient use of the analytic insights.73,74
Current efforts and screening tools for SDoH-EHR integration
There are federal, state, and local efforts that contribute to the integration of SDoH in EHRs, particularly the individual-level determinants. In 2014, the National Academy of Medicine recommended 11 social and behavioral domains to use for data collection in EHRs.75,76 However, consensus has not been reached on which SDoH measures can or should be captured in EHRs.70 Various patient-facing tools related to the SDoH have since emerged, aiming to allow patients to document their own socioeconomic needs and thus improve the validity and relevance of the social information collected.
Most of these screening tools involve either screening checklists or surveys that are meant to be filled out by patients on their own or completed through a facilitated interview with a clinical staff member. The specific SDoH items included in these tools vary from one to another. To inform efforts to create national standards for representing SDoH information in EHRs, we compared the SDoH measures reported in the literature versus those included in the screening tools used in current practice (Table 4).
Table 4.
Comparison of determinants of health in the literature versus the current screening tools
| Domains | Dimensions | PRAPARE | Accountable Health Communities Screening Tool | Health Leads Screening Tool | Upstream Risks Screening Tool |
|---|---|---|---|---|---|
| Economic stability | Income | • | |||
| Financial resource | • | • | • | • | |
| Employment | • | • | • | ||
| Clothinga | • | ||||
| Utilities (phone, gas, electric)a | • | • | • | ||
| Child carea | • | • | |||
| Neighborhood and built environment | Transportation | • | • | • | |
| Neighborhood | • | • | |||
| Living arrangements | • | • | • | • | |
| Food access | • | • | • | • | |
| Environmental conditionsb | |||||
| Health and health care | Insurance status | • | |||
| Behavioral health (diet, physical activity, tobacco usage, etc.) | • | • | • | ||
| Mental health (stress, depression, etc.) | • | • | • | • | |
| Need for assistance | • | • | |||
| Disabilities | • | ||||
| Access to careb | |||||
| Education | Education | • | • | ||
| Language | • | • | • | ||
| Social and community context | Race/ethnicity | • | |||
| Social connections | • | • | • | • | |
| Interpersonal relationship | • | • | • | ||
| Incarceration history | • | ||||
| Migrant/seasonal farmworker/immigration | • | • | |||
| Veteran status | • | ||||
| Refugee statusa | • | ||||
| Marital statusb |
PRAPARE: Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences.
Appeared only in the screening tools.
Appeared only in the reviewed articles.
We focus on the 4 main SDoH screening tools developed in the United States to help identify SDoH in a primary care setting: (1) the Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences (PRAPARE) tool by the National Association of Community Health Centers, (2) the Accountable Health Communities Screening Tool, (3) the Health Leads Screening Tool, and (4) HealthBegins Upstream Risks Screening Tool. We categorize the SDoH measures into the 5 key domains outlined by Healthy People 2020. While most of the measures in Table 4 appeared both in the literature and at least 1 of the screening tools, some measures appeared only in either the reviewed articles or the screening tools. The measures that appeared in the literature but not in the screening tools are related to environmental conditions, access or proximity to healthcare providers, and marital status. Besides the measures of refugee status, the measures screened in practice but not yet evaluated in the literature are mostly in the domains of economic stability (eg, clothing, utilities, and child care).
While all the screening tools cover the 5 domains outlined in Healthy People 2020, they differ in the specific measures they use to screen and collect social and behavior factors within each domain. PRAPARE has the most extensive list of measures in the domains of economic stability, neighborhood and built environment, education, and social and community context. In the domain of health and health care, PRAPARE focuses on insurance status measures while the other screening tools focus on lifestyle (eg, physical activity and dietary pattern), mental health (eg, depression), and need for assistance.
Growing evidence of impact
Although integrating community-based determinants have shown limited impact thus far on improving the performance of risk prediction, area-based SDoH can be used for monitoring disparities.77 They can also be used to develop population-level indicators that describe the health and quality of life of a geographic community, which provide an opportunity to track and enhance population health on a regional or national level.22 In contrast to studies with area-level SDoH data, recent studies that incorporated individual-level SDoH data have all reported significantly improved prediction performance, growing the evidence base with large number of study participants.
In addition to addressing SDoH data collection issues, there is insufficient evidence that social or behavioral risk factors can be effectively addressed through referrals or other action tools. Stronger evidence is needed to demonstrate that data related to SDoH can give a more complete understanding of population risk and improve prediction models. High-quality evidence is also needed to demonstrate that interventions targeting specific SDoH domains, such as referrals to community services, will lead to better clinical outcomes as they help address patients’ social needs. Currently, evaluation criteria for referral programs have focused mostly on process measures.78,79 Yet, most rewards in the era of value-based care are based on improving clinical outcomes and reducing expenditures. More rigorous research with internal validity are needed to focus on the evaluation of both care delivery process and outcomes so that the effectiveness of interventions can be better understood. Finally, there is a need for a greater awareness of the conflation of social (or behavioral) risks with social (or behavioral) determinants. This review suggests that researchers should clarify these key terms and the concepts underlying them in future studies, which could advance policies and practices related to SDoH.
There are limitations to this review. First, although we searched for articles across 5 large databases, we only reported our findings from the published literature and therefore may have failed to capture unpublished studies that might also contain relevant content. Second, owing to the heterogeneity among included studies (eg, different conditions and outcomes studied, various sources and levels of SDoH data elements considered, study designs with or without interventions), it was not possible to systematically apply a quality assessment tool to these studies. Therefore, we included all studies due to their potential to add valuable insight in assessing SDoH’s impact.
CONCLUSION
In summary, this systematic review sheds light on the current status of the literature on the integration of SDoH into EHRs, and particularly on the impact of this integration on the risk assessment goals of studies. Our findings support the current policy efforts to establish national standards for representing data related to social and behavioral determinants of health and create tools to incorporate both community- and individual-level determinants into EHRs. It is also important to incentivize the collection of SDoH data through financial or quality measures. Finally, more studies are needed to expand the body of research that measures the impact of SDoH interventions on healthcare outcomes, costs, and population health management, particularly delineating the impact of social and behavioral risk factors.
AUTHOR CONTRIBUTIONS
MC and RP conceived the idea for this study, and MC, RP, and XT designed the study. MC and XT conducted the analysis and drafted the manuscript with extensive inputs from RP. MC, RP, and XT interpreted the results and revised the manuscript. All authors read and approved the final manuscript.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
Supplementary Material
ACKNOWLEDGMENTS
We would like to thank Sarah J. Hammill, the Business and Online Learning Librarian at Florida International University, for her help with creating search keywords and strategies. We also thank Polina Durneva, a PhD student in the College of Business at Florida International University, for her contributions to the search and screening of the articles. Finally, we sincerely thank the Associate Editor and 2 anonymous reviewers for their helpful comments and suggestions.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1.World Health Organization. Social Determinants of Health. http://www.who.int/social_determinants/sdh_definition/en/ Accessed January 15, 2020.
- 2.Centers for Disease Control and Prevention. Definitions, NCHHSTP Social Determinants of Health. https://www.cdc.gov/nchhstp/socialdeterminants/definitions.html Accessed March 11, 2019.
- 3. Solar O, Irwin A.. A Conceptual Framework for Action on the Social Determinants of Health (Social Determinants of Health Discussion Paper 2). Geneva, Switzerland: World Health Organization; 2010. [Google Scholar]
- 4.Healthy People. Social Determinants of Health. https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-health/interventions-resources Accessed January 27, 2020.
- 5. Daniel H, Bornstein SS, Kane GC; Health and Public Policy Committee of the American College of Physicians. Addressing social determinants to improve patient care and promote health equity: an American College of Physicians position paper. Ann Intern Med 2018; 168 (8): 577–8. doi: 10.7326/m17-2441. [DOI] [PubMed] [Google Scholar]
- 6. Braveman P, Gottlieb L.. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep 2014; 129 (Suppl 2): 19–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Alderwick H, Gottlieb LM.. Meanings and misunderstandings: a social determinants of health lexicon for health care systems. Milbank Q 2019; 97 (2): 407–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rich E, Lipson D, Libersky J, Parchman M.. Coordinating Care for Adults with Complex Care Needs in the Patient-Centered Medical Home: Challenges and Solutions. Rockville, MD: Agency for Healthcare Research and Quality; 2012. [Google Scholar]
- 9. Diez Roux AV, Mair C.. Neighborhoods and health. Ann N Y Acad Sci 2010; 1186 (1): 125–45. [DOI] [PubMed] [Google Scholar]
- 10. Taylor LA, Tan AX, Coyle CE, et al. Leveraging the social determinants of health: what works? PLoS One 2016; 11 (8): e0160217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Adler NE, Stead WW.. Patients in context—EHR capture of social and behavioral determinants of health. N Engl J Med 2015; 372 (8): 698–701. [DOI] [PubMed] [Google Scholar]
- 12. Campanella P, Lovato E, Marone C, et al. The impact of electronic health records on healthcare quality: a systematic review and meta-analysis. Eur J Public Health 2016; 26 (1): 60–4. [DOI] [PubMed] [Google Scholar]
- 13. Venzon A, Le TB, Kim K.. Capturing social health data in electronic systems: a systematic review. Comput Inform Nurs 2019; 37 (2): 90–8. [DOI] [PubMed] [Google Scholar]
- 14. Henry J, Pylypchuk Y, Searcy T, Patel V.. Adoption of Electronic Health Record Systems among U.S. Non-Federal Acute Care Hospitals: 2008-2015. Washington, DC: ONC Data Brief; 2016. [Google Scholar]
- 15.Office of the National Coordinator for Health Information Technology . Office-Based Physician Electronic Health Record Adoption Health IT Quick-Stat #50. https://dashboard.healthit.gov/quickstats/pages/physician-ehr-adoption-trends.php Accessed January 27, 2020.
- 16.Centers for Medicare and Medicaid Services. Stage 3 Program Requirements for Eligible Hospitals, CAHs and Dual-Eligible Hospitals Attesting to CMS. https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Stage3_RequieEH Accessed January 27, 2020.
- 17. The American Academy of Nursing. Academy calls for collective action to include social and behavioral determinants of health in EHR. Am Nurse 2015; 47 (5): 4. [PubMed] [Google Scholar]
- 18. Johnson SR. Hospitals address social determinants of health through community cooperation and partnerships. https://www.modernhealthcare.com/article/20180602/TRANSFORMATION03/180609978 Accessed January 15, 2020.
- 19. Palacio AM, Suarez M, Toro Y, et al. Integrating social determinants of health into the electronic health records of a large health system: a qualitative perspective. Perspect Health Inf Manag 2018, Summer. https://perspectives.ahima.org/integratingsocialdeterminants/ Accessed January 27, 2020. [Google Scholar]
- 20. Bachrach D. Addressing patients’ social needs: An emerging business case for provider investment. https://www.commonwealthfund.org/publications/fund-reports/2014/may/addressing-patients-social-needs-emerging-business-case-provider Accessed January 27, 2020.
- 21. Thomas-Henkel C, Schulman M. Screening for social determinants of health in populations with complex needs: implementation considerations. https://www.chcs.org/resource/screening-social-determinants-health-populations-complex-needs-implementation-considerations/ Accessed January 27, 2020.
- 22. Hatef E, Weiner JP, Kharrazi H.. A public health perspective on using electronic health records to address social determinants of health: the potential for a national system of local community health records in the United States. Int J Med Inform 2019; 124: 86–9. [DOI] [PubMed] [Google Scholar]
- 23. Nijhawan AE, Metsch LR, Zhang S, et al. Clinical and sociobehavioral prediction model of 30-day hospital readmissions among people with HIV and substance use disorder: beyond electronic health record data. J Acquir Immune Defic Syndr 2019; 80 (3): 330–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lucyk K, McLaren L.. Taking stock of the social determinants of health: a scoping review. PLos One 2017; 12 (5): e0177306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Knight R, Shoveller J, Greyson D, Kerr T, Gilbert M, Shannon K.. Advancing population and public health ethics regarding HIV testing: a scoping review. Crit Public Health 2014; 24 (3): 283–95. [Google Scholar]
- 26. Gottlieb LM, Wing H, Adler NE.. A systematic review of interventions on patients’ social and economic needs. Am J Prev Med 2017; 53 (5): 719–29. [DOI] [PubMed] [Google Scholar]
- 27. Andermann A. Screening for social determinants of health in clinical care: moving from the margins to the mainstream. Public Health Rev 2018; 39 (1): 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. De Marchis EH, Torres JM, Benesch T, et al. Interventions addressing food insecurity in health care settings: a systematic review. Ann Fam Med 2019; 17 (5): 436–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Pool MS, Agyemang CO, Smalbrugge M.. Interventions to improve social determinants of health among elderly ethnic minority groups: a review. Eur J Public Health 2017; 27 (6): 1048–54. [DOI] [PubMed] [Google Scholar]
- 30. Walker RJ, Smalls BL, Campbell JA, Strom Williams JL, Egede LE.. Impact of social determinants of health on outcomes for type 2 diabetes: a systematic review. Endocrine 2014; 47 (1): 29–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Maness SB, Buhi ER.. Associations between social determinants of health and pregnancy among young people: a systematic review of research published during the past 25 years. Public Health Rep 2016; 131 (1): 86–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Galea S, Tracy M, Hoggatt KJ, Dimaggio C, Karpati A.. Estimated deaths attributable to social factors in the United States. Am J Public Health 2011; 101 (8): 1456–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Golembiewski E, Allen KS, Blackmon AM, Hinrichs RJ, Vest JR.. Combining nonclinical determinants of health and clinical data for research and evaluation: rapid review. JMIR Public Health Surveill 2019; 5 (4): e12846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P; the PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6 (7): e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Welch V, Petticrew M, Tugwell P, et al. ; PRISMA-Equity Bellagio group. PRISMA-equity 2012 extension: reporting guidelines for systematic reviews with a focus on health equity. PLoS Med 2012; 9 (10): e1001333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Foeckler P, Henning V, Reichelt J. Victor Henning’s Brief Guide to Mendeley. https://www.elsevier.com/connect/victor-hennings-brief-guide-to-mendeley Accessed January 27, 2020.
- 37. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A.. Rayyan—a web and mobile app for systematic reviews. Syst Rev 2016; 5 (1): 210. doi: 10.1186/s13643-016-0384-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.U.S. Census Bureau. Understanding and using ACS single-year and multiyear estimates https://www.census.gov/content/dam/Census/library/publications/2018/acs/acs_general_handbook_2018_ch03.pdf Accessed January 10, 2020.
- 39. Roth C, Foraker RE, Payne PR, Embi PJ.. Community-level determinants of obesity: harnessing the power of electronic health records for retrospective data analysis. BMC Med Inform Decis Mak 2014; 14 (1): 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Tomasallo CD, Hanrahan LP, Tandias A, Chang TS, Cowan KJ, Guilbert TW.. Estimating Wisconsin asthma prevalence using clinical electronic health records and public health data. Am J Public Health 2014; 104 (1): e65–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wagaw F, Okoro CA, Sunkyung K, Park J, Rachman F, Kim S.. Linking data from health surveys and electronic health records: a demonstration project in two Chicago health center clinics. Prev Chronic Dis 2018; 15: 170085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Comer KF, Grannis S, Dixon BE, Bodenhamer DJ, Wiehe SE.. Incorporating geospatial capacity within clinical data systems to address social determinants of health. Public Health Rep 2011; 126: 54–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Ye C, Fu T, Hao S, et al. Prediction of incident hypertension within the next year: prospective study using statewide electronic health records and machine learning. J Med Internet Res 2018; 20 (1): e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Haas JS, Linder JA, Park ER, et al. Proactive tobacco cessation outreach to smokers of low socioeconomic status: a randomized clinical trial. JAMA Intern Med 2015; 175 (2): 218–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Hughes AE, Tiro JA, Balasubramanian BA, Skinner CS, Pruitt SL.. Social disadvantage, healthcare utilization, and colorectal cancer screening: leveraging longitudinal patient address and health records data. Cancer Epidemiol Biomarkers Prev 2018; 27 (12): 1424–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Shulman E, Kargoli F, Aagaard P, et al. Socioeconomic status and the development of atrial fibrillation in Hispanics, African Americans and non-Hispanic whites. Clin Cardiol 2017; 40 (9): 770–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Vest JR, Grannis SJ, Haut DP, Halverson PK, Menachemi N.. Using structured and unstructured data to identify patients’ need for services that address the social determinants of health. Int J Med Inform 2017; 107: 101–6. [DOI] [PubMed] [Google Scholar]
- 48. Casey JA, Pollak J, Glymour MM, Mayeda ER, Hirsch AG, Schwartz BS.. Measures of SES for electronic health record-based research. Am J Prev Med 2018; 54 (3): 430–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Navathe AS, Zhong F, Lei VJ, et al. Hospital readmission and social risk factors identified from physician notes. Health Serv Res 2018; 53 (2): 1110–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Kasthurirathne SN, Vest JR, Menachemi N, Halverson PK, Grannis SJ.. Assessing the capacity of social determinants of health data to augment predictive models identifying patients in need of wraparound social services. J Am Med Inform Assoc 2018; 25 (1): 47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Vest JR, Ben-Assuli O.. Prediction of emergency department revisits using area-level social determinants of health measures and health information exchange information. Int J Med Inform 2019; 129: 205–10. [DOI] [PubMed] [Google Scholar]
- 52. Bhavsar NA, Gao A, Phelan M, Pagidipati NJ, Goldstein BA.. Value of neighborhood socioeconomic status in predicting risk of outcomes in studies that use electronic health record data. JAMA Netw Open 2018; 1 (5): e182716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Sills MR, Hall M, Cutler GJ, et al. Adding social determinant data changes children’s hospitals’ readmissions performance. J Pediatr 2017; 186: 150–7.e1. [DOI] [PubMed] [Google Scholar]
- 54. Jamei M, Nisnevich A, Wetchler E, Sudat S, Liu E.. Predicting all-cause risk of 30-day hospital readmission using artificial neural networks. PLoS One 2017; 12 (7): e0181173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Vutien P, Shah R, Ma K, Saleem N, Melson J.. Utilization of census tract-based neighborhood poverty rates to predict non-adherence to screening colonoscopy. Dig Dis Sci 2019; 64 (9): 2505–13. [DOI] [PubMed] [Google Scholar]
- 56. Vest JR, Menachemi N, Grannis SJ, et al. Impact of risk stratification on referrals and uptake of wraparound services that address social determinants: a stepped wedged trial. Am J Prev Med 2019; 56 (4): e125–33. [DOI] [PubMed] [Google Scholar]
- 57. Molfenter TD, Bhattacharya A, Gustafson DH.. The roles of past behavior and health beliefs in predicting medication adherence to a statin regimen. Patient Prefer Adherence 2012; 6: 643–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Takahashi PY, Ryu E, Olson JE, et al. Health behaviors and quality of life predictors for risk of hospitalization in an electronic health record-linked biobank. Int J Gen Med 2015; 8: 247–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Feller DJ, Zucker J, Yin MT, Gordon P, Elhadad N.. Using clinical notes and natural language processing for automated HIV risk assessment. J Acquir Immune Defic Syndr 2018; 77 (2): 160–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Zheng L, Wang O, Hao S, et al. Development of an early-warning system for high-risk patients for suicide attempt using deep learning and electronic health records. Transl Psychiatry 2020; 10 (1): 72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Walsh CG, Ribeiro JD, Franklin JC.. Predicting suicide attempts in adolescents with longitudinal clinical data and machine learning. J Child Psychol Psychiatry 2018; 59 (12): 1261–70. [DOI] [PubMed] [Google Scholar]
- 62. Ancker JS, Kim M-H, Zhang Y, Zhang Y, Pathak J.. The potential value of social determinants of health in predicting health outcomes. J Am Med Inform Assoc 2018; 25 (8): 1109–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Bejan CA, Angiolillo J, Conway D, et al. Mining 100 million notes to find homelessness and adverse childhood experiences: 2 case studies of rare and severe social determinants of health in electronic health records. J Am Med Inform Assoc 2018; 25 (1): 61–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Kharrazi H, Anzaldi LJ, Hernandez L, et al. The value of unstructured electronic health record data in geriatric syndrome case identification. J Am Geriatr Soc 2018; 66 (8): 1499–507. [DOI] [PubMed] [Google Scholar]
- 65. Feller DJ, Zucker J. Towards the inference of social and behavioral determinants of sexual health: development of a gold-standard corpus with semi-supervised learning. AMIA Ann Symp Proc2018; 2018: 422–9. [PMC free article] [PubMed] [Google Scholar]
- 66.U.S. Census Bureau. American Community Survey (ACS). https://www.census.gov/programs-surveys/acs Accessed January 27, 2020.
- 67. Polubriaginof FCG, Ryan P, Salmasian H, et al. Challenges with quality of race and ethnicity data in observational databases. J Am Med Inform Assoc 2019; 26 (8–9): 730–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Wiebe N, Otero Varela L, Niven DJ, Ronksley PE, Iragorri N, Quan H.. Evaluation of interventions to improve inpatient hospital documentation within electronic health records: a systematic review. J Am Med Inform Assoc 2019; 26 (11): 1389–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Everson J, Adler-Milstein J.. Gaps in health information exchange between hospitals that treat many shared patients. J Am Med Inform Assoc 2018; 25 (9): 1114–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Cantor MN, Thorpe L.. Integrating data on social determinants of health into electronic health records. Health Aff (Millwood) 2018; 37 (4): 585–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Park EY. Patient data on social determinants of health. Health Aff (Millwood) 2018; 37 (8): 1340–41. [DOI] [PubMed] [Google Scholar]
- 72. Kreuter M, Garg R, Thompson T, et al. Assessing the capacity of local social services agencies to respond to referrals from health care providers: an exploration of the capacity of local social service providers to respond to referrals from health care providers to assist low-income patients. Health Aff (Millwood) 2020; 39 (4): 679–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Andermann A. Taking action on the social determinants of health in clinical practice: a framework for health professionals. CMAJ 2016; 188 (17–18): E474–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Centers for Disease Control and Prevention. Tools for Putting Social Determinants of Health into Action. https://www.cdc.gov/socialdeterminants/tools/index.htm Accessed May 2, 2020.
- 75.Institute of Medicine. Capturing Social and Behavioral Domains and Measures in Electronic Health Records: Phase 1. Washington, DC: National Academies Press; 2014. [PubMed] [Google Scholar]
- 76.Institute of Medicine. Capturing Social and Behavioral Domains and Measures in Electronic Health Records: Phase 2. Washington, DC: National Academies Press; 2014. [PubMed] [Google Scholar]
- 77. Berkowitz SA, Traore CY, Singer DE, Atlas SJ.. Evaluating area‐based socioeconomic status indicators for monitoring disparities within health care systems: results from a primary care network. Health Serv Res 2015; 50 (2): 398–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Agency for Healthcare Research and Quality. Strategy 6E: rapid referral programs. https://www.ahrq.gov/cahps/quality-improvement/improvement-guide/6-strategies-for-improving/access/strategy6g-rapid-referral.html Accessed January 27, 2020.
- 79. LaForge K, Gold R, Cottrell E, et al. How 6 organizations developed tools and processes for social determinants of health screening in primary care: an overview. J Ambul Care Manage 2018; 41 (1): 2–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.