ABSTRACT
Brugada syndrome is a genetic disease with a characteristic electrocardiogram (ECG) findings of ST elevation in leads V1–V3 with a right bundle branch block (RBBB) appearance called Brugada ECG pattern and a tendency to develop malignant polymorphic ventricular arrhythmias that may lead to syncope or cardiac arrest. Common triggers for Brugada ECG pattern include fever, tricyclic antidepressants, lithium, cocaine and alcohol. This ECG pattern together with clinical findings mentioned above is termed Brugada Syndrome. We report a case of a 51-year-old male with a past medical history of hypertension presented to emergency department with 2-day complaint of fever, chills, sore throat, nasal congestion, malaise, productive cough, was positive for Influenza B and on ECG found to have type-I (coved) Brugada ECG pattern. Influenza fever associated with Brugada ECG pattern is a rare manifestation; in fact, to the best of our knowledge, only three case reports have been published in the literature to date.
KEYWORDS: Fever, influenza, Brugada Pattern, Brugada Syndrome, STEMI
1. Introduction
Brugada syndrome is a genetic disorder that carries significant risk of sudden cardiac death. This autosomal dominant genetic defect affects myocardial sodium channels triggering abnormal electrical activity in the heart [1,2]. Patients can present with syncopal episodes and fatal ventricular arrhythmias, including ventricular fibrillation and polymorphic ventricular tachycardia that can lead to sudden cardiac death. Brugada pattern electrocardiogram (ECG) shows persistent ST elevation in leads V1–V3 with a right bundle branch block (RBBB) appearance referred to as pseudo-right bundle branch block. The most recognized Brugada ECG phenotype, Type 1, referred to as Coved type shows elevated ST segment that descends with an upward convexity followed by inverted T wave. Type 2 has ‘saddle back’ ST morphology in which elevated ST segment descends towards baseline before rising to an upright or biphasic T wave.
Arrhythmias in Brugada syndrome can occur at rest; and fever is one of the important causes among others [3]. The main aim of treatment in patients with this disorder is to prevent sudden cardiac death by lifestyle modifications to avoid triggers, medications, implantable defibrillator and radiofrequency catheter ablation. Here, we are presenting a case of Brugada pattern triggered by fever associated with influenza.
2. Case Presentation
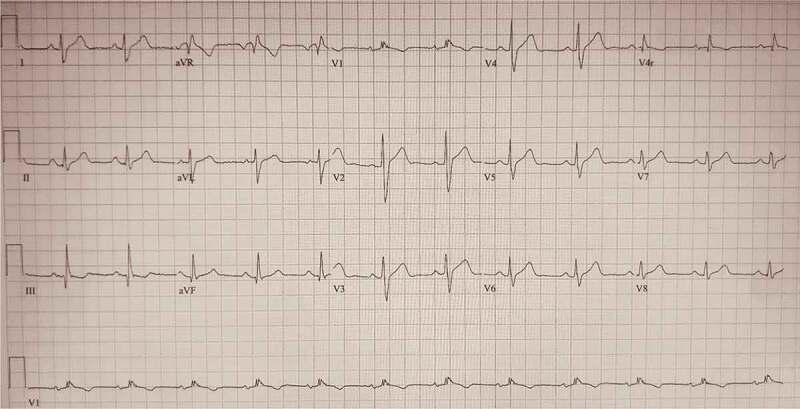
We report a 51-year-old Hispanic male with a past medical history of hypertension who presented to emergency department complaining of fever and chills for 2 days. Associated symptoms included body aches, nasal congestion, sore throat and cough. He denied chest pain or shortness of breath at rest or exertion, dizziness or lightheadedness, palpitations, abdominal pain, nausea, vomiting, constipation or diarrhea. He denied any history of syncope, orthopnea, paroxysmal nocturnal dyspnea. There was no history of sudden cardiac death or ischemic heart disease in the family. He reported that he did not receive flu shot this year. Vital signs on presentation: temperature 102.8 F, blood pressure 130/80, heart rate 106 beats per minute, respiratory rate 20 per minute and oxygen saturation 95% on room air. Complete blood count on presentation – hemoglobin 14.9 gm/dl (14–18 gm/dl), platelets 103 K (130 K-400 K), white blood count 9.6 K/UL (4.8–10.8 K/UL), absolute neutrophil count of 8.2 K/UL (1.4–6.5 K/UL). Complete metabolic profile showed creatinine 0.67 mg/dl (0.7–1.2 mg/dl), sodium 129 mmol/L (136–144 mmol/L), potassium 2.3 mmol/L (3.6–5.1 mmol/L), magnesium 1.7 mg/dl (1.8–2.5 mg/dl), brain natriuretic peptide (BNP) 25 pg/ml (<100 pg/ml), d-dimer 240 ng/ml (0–230 ng/ml) and Troponin was 0.00 (0.00–0.08). Electrocardiogram on presentation showed ST-segment elevation more than 2 mm with T-wave inversion in leads V1–V2 consistent with a type-I (coved) Brugada ECG pattern (Figure 1). Echocardiogram demonstrated ejection fraction of 60–65%. Patient was positive for Influenza B. Patient was treated with Oseltamivir and Tylenol. ECG changes corrected with the resolution of fever.
Figure 2.
Electrocardiogram showing resolution of Brugada pattern with treatment of influenza-associated fever.
Figure 1.

Electrocardiogram showing ST-segment elevation more than 2 mm with T-wave inversion in leads V1–V2 consistent with a type-I (coved) Brugada ECG pattern.
3. Discussion
We searched PubMed for literature review using search terms ‘influenza’ and ‘Brugada pattern’ and only three case reports have been reported so far [4–6]. Baranchuk et al. reported a 45-year-old with Brugada Syndrome with influenza infection. Patient presented with recurrent episodes of syncope and had a positive family history of sudden cardiac death.
Prevalence of asymptomatic Brugada pattern remains rare with reported incidence of 0.1–1% of the general population occurring more commonly in males and strongly associated in patients with schizophrenia [7]. The pathogenesis of the characteristic findings seen on an electrocardiogram of pseudo-right bundle branch block with persistent ST-elevation in V1 and V2 are multifactorial- genetics, anatomic factors, toxic stimuli and systemic fever have all been implicated in playing an important role. Loss of function sodium-influx channel gene mutations in the epicardial tissue has been found in 15–30% of patients with Brugada pattern of ECG. An increased parasympathetic effect has been implicated in patients with Brugada pattern as evident from the increased nocturnal occurrence of associated tachyarrhythmias and from studies detailing augmentation of the ST-elevation during the period of exercise recovery.
Cocaine and other psychotropic drugs including neuroleptic drugs and cyclic anti-depressants are known triggers of Brugada pattern due to their direct effects on myocardial sodium-channels. Systemic fever remains a unique provoking factor for both the characteristic ECG changes as seen in Brugada pattern and incidence of sustained tachyarrhythmias resulting in cardiac arrests [8]. Animal studies have helped discern the effect of hyperthermia resulting in the reduction of sodium current causing changes of action potentials. Evidence of the association between Brugada pattern and fever is based largely on a retrospective study that has demonstrated that Brugada pattern on ECG is 20x more common in patients with fever; another study determined that 18% of patient with diagnosed Brugada syndrome had a documented fever prior to incidence of cardiac arrest. Additionally, in a multicenter survey of 588 patients with Brugada syndrome, 6% of the patients had an arrhythmic event during a febrile episode. Studies have noted that cardiac sodium channel mutations can result in temperature gated sodium channels whose potential for causing arrhythmias increases with higher temperatures [3]. Our patient had type 1 Brugada ECG pattern induced by influenza-associated fever.
Treatment is primarily focused around prevention of sudden cardiac arrest and the termination of any ventricular arrhythmias. Implantable Cardiac Defibrillator device placement is the first line of therapy in cases that need intervention and is indicated in those who have survived sudden cardiac arrest or those with a history of syncope due to ventricular tachyarrhythmias. For those refusing ICD implantation or are not a candidate for ICD implantation due to reduced life expectancy/significant comorbidities or having recurrent arrhythmias, treatment with antiarrhythmics (quinidine and amiodarone) is recommended [9,10]. In patients who do not meet the criteria for ICD placement or antiarrhythmic at the time of initial diagnosis, an electrophysiologic study would be beneficial to further evaluate the condition. In patients with asymptomatic Brugada ECG pattern but with no personal history of syncope, arrhythmias or family history of sudden cardiac death, no specific treatment would be needed except for avoiding the triggers mentioned earlier [9,10]
4. Conclusion
In conclusion, we report a case of a 51-year-old male with a past medical history of hypertension presented to emergency department with upper respiratory symptoms, was positive for Influenza B and on ECG found to have type-I (coved) Brugada ECG pattern. Our case and review of literature reveals that health-care providers should be aware of the rare manifestation of influenza-fever-associated Brugada ECG pattern and high index of suspicion should be kept in mind for the appropriate clinical scenario.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1].Brugada J, Campuzano O, Arbelo E, et al. Present status of Brugada syndrome. JACC. 2018;72(9):1046–1059. [DOI] [PubMed] [Google Scholar]
- [2].Brugada R, Campuzano O, Sarquella-Brugada G, et al. Brugada syndrome. Methodist Debakey Cardiovasc J. 2014;10(1):25–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Lamelas P, Labadet C, Spernanzoni F, et al. Brugada electrocardiographic pattern induced by fever. World J Cardiol. 2012;4(3):84–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Baranchuk A, Simpson CS.. Brugada syndrome coinciding with fever and pandemic (H1N1) influenza. Cmaj. 2011;183(5):582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].González RL, Medrano JC, Castaño AJ, et al. [Asymptomatic Brugada syndrome unmasked by influenza virus subtype H1N1 infection]. Med Clin (Barc). 2011;136(5):226–227. [DOI] [PubMed] [Google Scholar]
- [6].Kusaka K, Yamakawa J, Kawaura K, et al. Brugada-like electrocardiographic changes during influenza infection. J Int Med Res. 2003;31(3):244–246. [DOI] [PubMed] [Google Scholar]
- [7].Blom MT, Cohen D, Seldenrijk A, et al. Brugada syndrome ECG is highly prevalent in schizophrenia. Circ Arrhythm Electrophysiol. 2014;7(3):384–391. [DOI] [PubMed] [Google Scholar]
- [8].Amin AS, Klemens CA, Verkerk AO, et al. Fever-triggered ventricular arrhythmias in Brugada syndrome and type 2 long-QT syndrome. Neth Heart J. 2010;18(3):165–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Belhassen B, Glick A, Viskin S.. Efficacy of quinidine in high-risk patients with Brugada syndrome. Circulation. 2004;110(13):1731–1737. [DOI] [PubMed] [Google Scholar]
- [10].Márquez MF, Bonny A, Hernández-Castillo E, et al. Long-term efficacy of low doses of quinidine on malignant arrhythmias in Brugada syndrome with an implantable cardioverter-defibrillator: a case series and literature review. Heart Rhythm. 2012;9(12):1995–2000. [DOI] [PubMed] [Google Scholar]


