ABSTRACT
Infective endocarditis (IE) involving multiple cardiac valves is uncommon and has more risk of complications. We present an interesting case of infective endocarditis involving both aortic and tricuspid valves, suspected based on clinical presentation. He is a 54-year-old male with history of intravenous drug abuse (IVDA) who presented with exertional dyspnea, fevers/chills, fatigue, and temporarily vision loss. On exam, he had a low-grade fever, systolic murmur, bilateral crackles in lungs, and left hemineglect. He had leukocytosis and elevated BNP. First EKG showed first-degree AV block. CT head showed a subacute stroke in the right posterior cerebral artery (PCA) distribution. Transthoracic echocardiogram revealed a large tricuspid valve vegetation. He developed a second-degree heart block and a transcutaneous pacemaker was placed. Due to high concern for aortic valve involvement, a transesophageal echocardiogram was done revealing a large mobile tricuspid valve vegetation and an aortic valve ring abscess. He underwent abscess debridement and replacement of the aortic and tricuspid valve. He was found to have a ventricular septal defect which was also repaired. He recently had antibiotics for presumed pneumonia that is likely the reason for negative cultures. He received an 8-week course of Ceftriaxone for culture negative infective endocarditis and subsequently recovered well. This case report highlights that, although rare, the presence of right and left sided IE is possible and suspicion of aortic valve involvement is crucial in the setting of AV nodal blocks and peripheral embolic events. In patients with progressive heart blocks, transvenous pacemaker placement and valve replacement should be considered immediately to prevent further morbidity and mortality.
KEYWORDS: Infective endocarditis, Multi-valvular endocarditis, heart block, stroke
1. Introduction
Infective endocarditis is an infection of the endocardial surface of the heart. The pathogen is usually staphylococci or streptococci sp., however, in more than 19% of cases, the cultures are negative [1–3]. The modified Duke criteria can be helpful however it should not supersede clinical judgement [3–5]. Treatment is antibiotics and sometimes surgery for valve replacement if certain criteria are met. The in-hospital mortality is about 18% but can increases up to 79% in aortic valve endocarditis [6].
Multi-valvular IE is uncommon and has more risk of complications compared to single valve IE. Multi-valvular IE holds a complicated clinical course with a higher incidence of heart failure, perivalvular complications, and often requires heart surgery, however mortality is similar likely in relation to more aggressive treatment [2,6–8].
2. Case presentation
We present a case of infective endocarditis involving both aortic and tricuspid valves, suspected based on clinical presentation. A 54-year-old Caucasian male with a past medical history significant for Hepatitis C, COPD, and intravenous drug abuse presented with worsening exertional SOB, fevers/chills, night sweats, and weakness for more than 2 months. The patient also complained of transient vision loss which occurred 3 days prior to presentation. The patient reported that he was an active drug user with his last use of heroin about 1 month ago. He also informed us that he was reusing old needles and recently received a tattoo. Of note, within the month leading up to hospitalization, he was recently treated with multiplecourses of antibiotics for presumed pneumonia.
On arrival, the patient had a low-grade temperature of 37.8 C, heart rate of 90 beats per minute, respiratory rate of 18 breaths per minute, and blood pressure of 121/70 mmHg. He was awake, alert, and in mild distress. He had no JVD or cervical lymphadenopathy. On lung exam, he had faint bibasilar crackles. On heart exam, he had normal S1, S2, regular rate, and rhythm with a crescendo decrescendo systolic murmur 4/6 loudest over the tricuspid area. His abdomen was soft, not distended, and non-tender. Although the patient stated that his vision was intact, he was found to have left-sided hemineglect. He had normal strength and range of motion in extremities. He didn’t have any edema or tenderness. Skin exam was notable for track marks around the right knee, but he had no Janeway lesions or Osler’s nodes.
Laboratory analysis was significant for a neutrophilic predominant leukocytosis of 24x10(3)/ul. Troponin I was normal at 0.16 ng/mL. Brain Natriuretic Peptide (BNP) was 882 pg/mL. His initial EKG revealed a first-degree AV block with a PR interval of 300 ms (Figure 1). The chest x-ray showed pulmonary congestion (Figure 2). A CT of the head was ordered to further evaluate his neurologic deficits which showed a subacute stroke in PCA territory (Figure 3). A bedside echocardiogram revealed a large tricuspid valve vegetation (Figure 4).
Figure 1.
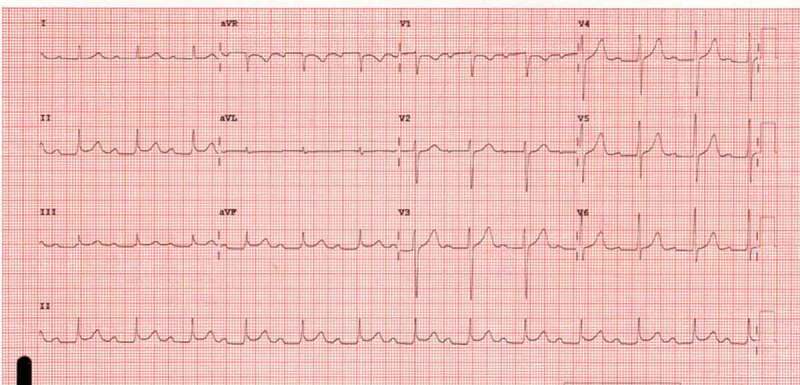
EKG showed first-degree AV block.
Figure 2.
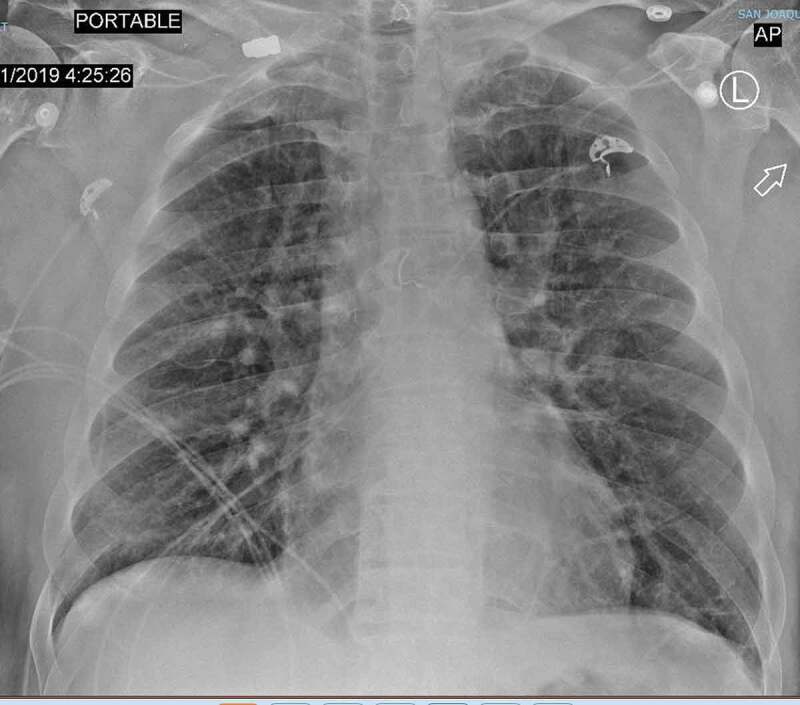
CXR showed pulmonary congestion.
Figure 3.

CT head showed ischemic changes in the right PCA territory.
Figure 4.

TTE showed tricuspid vegetation.
Shortly within 12 hours, the patient developed an intermittent second-degree type I heart blocks so a transvenous pacemaker was inserted due to concern of a progressing heart block. There was high clinical suspicion for aortic valve involvement due to conduction abnormalities and an embolic brain lesion. We choose to pursue further with a transesophageal echocardiogram (TEE) which discovered a 3.9 × 0.94 cm mobile tricuspid valve vegetation and an aortic valve ring abscess (Figure 5). He also had moderate aortic and tricuspid regurgitation with a preserved ejection fraction.
Figure 5.
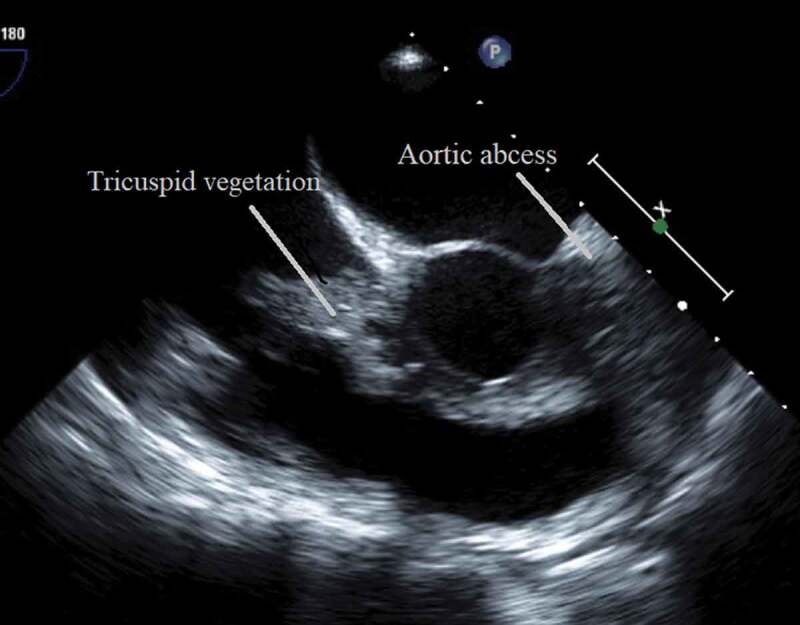
TEE showed tricuspid and aortic vegetation.
A left heart catheterization was performed revealing essentially normal epicardial vessels. On hospital day 5, he successfully underwent aortic valve replacement with a bioprosthetic valve and tricuspid valve repair with a 28 mm MCT3 ring after debridement of the abscess. After abscess removal, he was found to have a membranous ventricular septal defect that was patched during the surgery. Prior to developing endocarditis, he didn’t have sign or symptoms of shunt of the underlying VSD (Figure 6).
Figure 6.
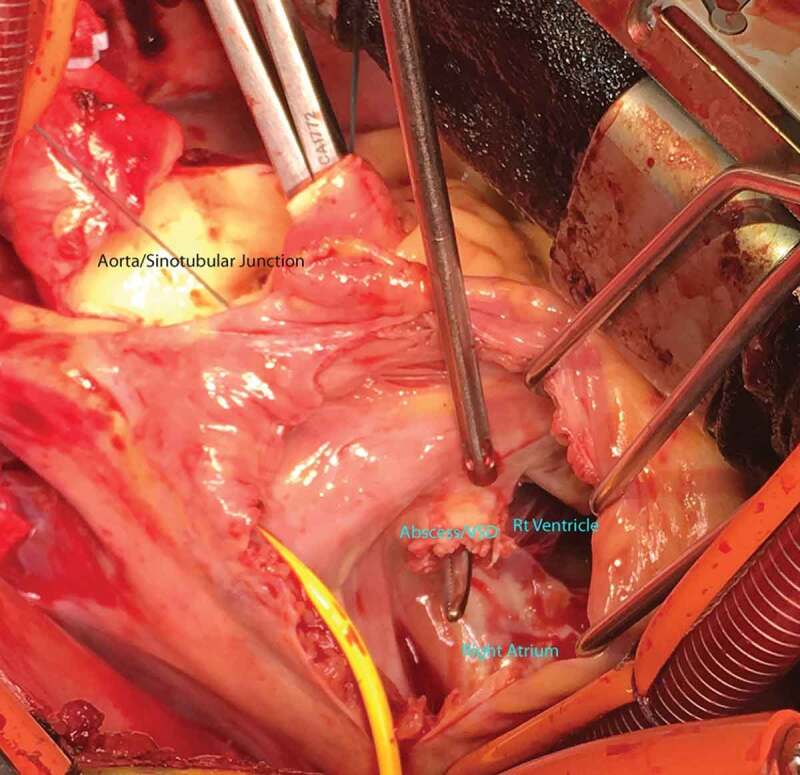
Aortic and tricuspid replacement and VSD repair.
Throughout his hospitalization blood cultures were negative. We also checked for Coxiella, Bartonella, and fungal cultures which were also all negative. Pathology showed fragments of valvular tissue with necrosis, fibrinopurulent exudate, and collection of bacterial organisms. Cultures of the native valves were negative. It is important to note that he had received multiple antibiotic courses prior to this admission for the treatment of pneumonia. He received total of 8 weeks of ceftriaxone for the treatment of culture-negative infective endocarditis. Given the recent stroke, he was not started on any anticoagulation. He was discharged on day 15 on Aspirin. On follow up visits 2 months after the discharge, patient was doing well clinically. He changed his lifestyle and he quit using any type of drugs anymore.
3. Discussion
Infective endocarditis (IE) refers to an infection of the endocardium. Despite improvements in diagnostic modalities, clinicians need to be alert especially in high-risk patient populations as poor recognition in IE can easily become a life-threatening disease [1–3].
IE can affect 3–9 cases per 100,000 per year. In developed countries, hospital mortality can be as high as 15–22% with an overall 5-year mortality up to 40%. Staphylococcus and streptococcus sp. usually account for up to 80% of cases, with Staphylococcus being most common in those with prosthetic valves. On occasion, blood cultures may be negative in situations where the patient has been previously exposed to antibiotics, similar to our patient who received antibiotic courses prior to his admission. Furthermore, if the organism is a fastidious grower such as Bartonella, Coxiella, or those who belong to the HACEK group, blood cultures can be negative making the choice of antibiotic challenging [4].
IE may affect native or prosthetic heart valves and those with congenital heart defects. Moreover, while usually only a single heart valve becomes affected, literature has shown that those with multiple affected valves tend to have a poorer clinical course and a higher risk for developing heart failure and perivalvular complications. These patients usually require aggressive and invasive treatment by means of cardiac surgery [7].
Patient with IE typically presents with a fever and new or worsening heart murmur. They can sometimes present with skin and nail changes. The modified Duke Criteria is a scoring system which is useful in disease detection and has a high negative predictive value however it should not be used in replacement of clinical judgement. Additionally, patients may present septic, meningitis, with heart failure, or with other signs of peripheral embolic events. An elevation of inflammatory markers can also be seen but is non-specific [3–5,7]
Patients with IE can also develop heart blocks. Usually, heart blocks occur when the cardiac valves on the left side of the heart are affected. The occurrence of first-degree AV blocks is clinically significant not only because these heart blocks can progress, as it did in our patient, but its presence strongly suggests a perivalvular extension of an aortic abscess [9]. Furthermore, the conduction system of the heart is easily affected due to the proximity of the aortic valve with the bundle of His in turn leading to problems with AV blocks or bundle branch blocks. It is particularly prudent to monitor these patients on telemetry as disruptions in the conduction system carry increased mortality and overall a poorer prognosis. The presence of an AV block alone carries a 97% specificity in the detection of perivalvular aortic involvement [9,10].
In intravenous drug users, like our patient, the tricuspid valve is the most commonly affected valve. However, left-sided IE poses the highest risk for developing peripheral embolic events including neurologic complications. Clinical manifestations for neurologic disease include ischemia or hemorrhagic strokes, brain or spinal abscesses, meningitis, infected intracranial aneurysms, encephalopathy or seizures [11]. Vegetations on the anterior leaflet of the mitral valve, left-sided endocarditis, or uncontrolled infection due to delays in antibiotics particularly with S. Aureus increases the likelihood of CNS events [12]. In our patient, his complaint of transient vision loss led us to obtain a CT of the brain in which we found a PCA stroke which led us to obtain a TEE where we discovered a left-sided vegetation.
Diagnosis is made with transthoracic echocardiogram (TTE) and/or transesophageal echocardiogram (TEE), and blood cultures. When TTE and TEE are combined, vegetation can be seen in 90% of the cases and it is also useful in finding regurgitation and abscess [13]. For our patient, a focused bedside echocardiogram performed by the admitting team revealed a large tricuspid vegetation. However, as a tricuspid vegetation alone was not explanatory for the cerebral manifestations or AV block, a TEE was done confirming the presence of an aortic valve ring abscess along with a 3.9 × 0.94 cm mobile tricuspid valve vegetation.
The treatment of endocarditis should be a concerted effort with the primary physician, cardiologist, infection disease specialist, and often a cardiothoracic surgeon. All patients with IE will need antibiotic therapy and the duration of treatment is dependent upon on if a native or prosthetic valve is affected.
The management of patients who develop strokes in the setting of IE differs from those of noninfectious causes. When there is a concern for septic emboli, anticoagulation, antiplatelet, and thrombolytic therapy are contraindicated due to the very significant risk of hemorrhage [14]. Additionally, patients with CNS manifestations should strongly be considered for valve repair. The American College of Cardiology (ACC) recommends that surgery should be considered in native valve endocarditis with mobile vegetation >10 mm (level of evidence: class IIB) and the European Society of Cardiology (ESC) agrees with urgent surgery for vegetation >10 mm and other predictors of a complicated course such as heart failure, persistent infections, and specific to our patient, abscess formation (class I). Lastly, while ACC and ESC both agree on surgical consideration, there have been no large studies or consensus on the ideal time for surgical intervention [5,15].
Other indications for cardiac surgery include heart failure especially in the setting of severe regurgitation or obstruction, poor control of infection which sometimes is the case in fungal or multidrug-resistant infections, or vegetations at high risk for peripheral embolic event [4,16]. Rapid surgical intervention is warranted to prevent hemodynamic instability, poor control of the infection, or the mobilization of large vegetations [9]. However, when the emergent aforementioned situations are not present, choosing the best and optimal time for surgery can be difficult to decide especially when the patient is a suboptimal surgical candidate. With our patient, we felt that early surgical intervention was beneficial to prevent further morbidity and mortality.
4. Conclusion
Multi-valvular IE is uncommon with more risk of complications compared of single-valve IE. In this case report, we present a rare case of endocarditis involving both the tricuspid and aortic valves, suspected based on the patient’s clinical presentation. Although our initial transthoracic echocardiogram showed only a large tricuspid valve vegetation, our clinical suspicion for aortic valve involvement was high due to a progressing AV block and a subacute embolic stroke. A transesophageal echocardiogram confirmed the presence of a tricuspid valve vegetation and aortic ring abscess which prompted both valves and a VSD to be surgically repaired. We believe that due to our prompt recognition and diagnostic diligence in the confirmation of multi-valvular IE, we were able to prevent this patient from developing septic shock, additional embolic events, and even mortality.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1].Cahill TJ, Prendergast BD.. Infective endocarditis. Lancet. 2016. February 27;387(10021):882–893. Epub 2015 Sep 1. [DOI] [PubMed] [Google Scholar]
- [2].Baddour LM, Wilson WR, Bayer AS, et al. Infective Endocarditis in Adults: Diagnosis, Antimicrobial Therapy, and Management of Complications: A Scientific Statement for Healthcare Professionals From the American Heart Association [published correction appears in Circulation. 2015 Oct 27;132(17):e215] [published correction appears in Circulation. 2016 Aug 23;134(8):e113] [published correction appears in Circulation. 2018 Jul 31;138(5):e78-e79]. Circulation. 2015;132(15):1435-1486. doi:10.1161/CIR.0000000000000296. doi: 10.1161/CIR.0000000000000296. [DOI] [PubMed]
- [3].DynaMed [Internet]. Ipswich (MA): EBSCO Information Services. 1995 -. Record No. T113919, Infective Endocarditis; [updated 2018 Nov 30; cited 2020 April25]. Available from https://www.dynamed.com/topics/dmp~AN~T113919. Registration and login required. [Google Scholar]
- [4].Hoen B, Duval X.. Infective endocarditis. N Engl J Med. 2013;368:1425–1433. [DOI] [PubMed] [Google Scholar]
- [5].Habib G, Lancellotti P, Antunes MJ et al. 2015. ESC Guidelines for the management of infective endocarditis: the task Force for the management of infective endocarditis of the European society of cardiology (ESC). Endorsed by: European association for ca
- [6].Murdoch DR, Corey GR, Hoen B, et al. Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis-Prospective Cohort Study. Arch Intern Med. 2009;169(5):463-473. doi:10.1001/archinternmed.2008.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].López J, Revilla A, Vilacosta I, et al. Multiple-valve infective endocarditis: clinical, microbiologic, echocardiographic, and prognostic profile. Medicine (Baltimore). 2011;90(4):231-236. doi:10.1097/MD.0b013e318225dcb0. [DOI] [PubMed] [Google Scholar]
- [8].Paterick TE, Paterick TJ, Nishimura RA, Steckelberg JM. Complexity and subtlety of infective endocarditis. Mayo Clin Proc. 2007;82(5):615-621. doi:10.4065/82.5.615. [DOI] [PubMed] [Google Scholar]
- [9].Tabas J, Varosy PD, Marcus GM, et al. Significance of first-degree atrioventricular block in acute endocarditis—diagnosis. JAMA Intern Med. 2013;173(9):726. [DOI] [PubMed] [Google Scholar]
- [10].Brancheau D, Degheim G, Machado C.. Timing for pacing after acquired conduction disease in the setting of endocarditis. Case Rep Cardiol. 2015;2015:4 Article ID 471046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Morris NA, Matiello M, Lyons JL, et al. Neurologic complications in infective endocarditis: identification, management, and impact on cardiac surgery. Neurohospitalist. 2014. October;4(4):213–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Derex L, Bonnefoy E, Delahaye F. Impact of stroke on therapeutic decision making in infective endocarditis. J Neurol. 2010. March;257(3):315–321. [DOI] [PubMed] [Google Scholar]
- [13].Molnar A, Sacui D, Manole S, et al. The value of transthoracic and transesophageal echocardiography for the diagnosis of the native. Med Ultrasonogr. 2016;18:253256. [DOI] [PubMed] [Google Scholar]
- [14].Walker KA, Sampson JB, Skalabrin EJ, et al. Clinical characteristics and thrombolytic outcomes of infective endocarditis-associated stroke. Neurohospitalist. 2012. July;2(3):87–91.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC Guideline for the Management of Patients With Valvular Heart Disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines [published correction appears in Circulation. 2014 Jun 10;129(23):e650]. Circulation. 2014;129(23):2440-2492. doi:10.1161/CIR.0000000000000029. [DOI] [PubMed] [Google Scholar]
- [16].Delahaye F, Célard M, Roth O, et al. Indications and optimal timing for surgery in infective endocarditis. Heart. 2004;90(6):618–620. [DOI] [PMC free article] [PubMed] [Google Scholar]


