Objective:
An interdisciplinary pain team was established at our institution to explore options for improving pain control in patients undergoing orthopedic surgery by identifying traits that put a patient at increased risk for inadequate pain control postoperatively.
Materials and Methods:
The interdisciplinary pain team identified 7 potential risk factors that may lead to inadequate pain control postoperatively including (1) history of physical, emotional, or sexual abuse; (2) history of anxiety; (3) history of drug or alcohol abuse; (4) preoperative nonsteroidal anti-inflammatory drug, or disease-modifying antirheumatic drug use; (5) current opioid use; (6) psychological conditions other than anxiety; and (7) current smoker. Statistical analysis determined which risk factors were associated with increased preoperative and postoperative pain scores.
Results:
A total of 1923 patients undergoing elective orthopedic surgery were retrospectively identified. Hip, knee, and shoulder replacements accounted for 76.0% of the procedures. 78.5% of patients had 3 or fewer risk factors and 17.1% had no risk factors. Anxiety, other psychological conditions, current opioid use, and current smoking were significantly associated with higher preoperative and postoperative pain scores.
Discussion:
We found a significant association between anxiety, current smoking, psychological conditions, and current opioid use with increased preoperative and postoperative reported pain score. We propose that identification of these risk factors should prompt more attention to postoperative pain control plans and will improve communication with patients and providers. We recommend a multimodal approach to postoperative pain control, and developed a pain orderset to help guide providers.
Key Words: pain, opioids, risk factors, perioperative, surgery
The Centers for Disease Control has declared an “opioid epidemic” in the United States.1 Orthopedic surgeons are considered one of the highest prescribers of opioid medications2 and much effort in the orthopedic community has been directed towards decreasing opioid use while providing adequate pain control.3–6 Appropriate pain control following surgery still remains a challenge, and there is no identified standard “recipe” for dealing with patients’ pain postoperatively. There is a growing literature that would support that patients with chronic pain or those who have been on opioids preoperatively will have more difficulty controlling their pain postoperatively.3,7,8 Patients with depression and/or anxiety have also been reported as having increased risk for inadequate pain control postoperatively.5,7–10 There is also literature to support that higher preoperative pain scores will reflect higher postoperative pain scores in the same patient.3,5,7,8
In April 2013, Penn State Hershey Medical Center (PSHMC) convened an interdisciplinary pain team (IPT) to address perioperative pain control. The purpose of this team was to explore options for improving pain control in patients undergoing elective orthopedic surgical procedures. We first recognized that certain patient groups may be more “at risk” for inadequate pain control postoperatively than others and that we must create a standardized way to identify this “at risk” group. We theorized that we could identify certain preoperative traits that would put patients at risk for inadequate pain control postoperatively. The team then tested this theory by developing a proposed list of “at risk” traits, based on the literature, and compared these traits to the first reported pain score in the same day unit (SDU) just before surgery as well as average 24- and 48-hour postoperative pain scores in a cohort of elective orthopedic surgery cases.
MATERIALS AND METHODS
The IPT consisted of representatives from orthopedics, pain management, nursing, physical medicine and rehabilitation, pediatrics, pharmacy, music therapy, physical therapy, anesthesia, quality and safety, information technology (IT), and the chief medical officer. The team met on a monthly basis between April 2013 and December 2014. Relevant literature was reviewed to identify “at risk” factors for inadequate pain control.4–16 The team identified a list of potential “at risk” factors based on the literature and then categorized them into 7 different categories that may put patients at risk for inadequate pain control postoperatively. These included: (1) history of physical, emotional, or sexual abuse; (2) history of anxiety; (3) history of illicit drug (nonopioid) or alcohol abuse; (4) preoperative nonsteroidal anti-inflammatory drug (NSAID) (aspirin, choline and magnesium salicylates, choline salicylate, celecoxib, diclofenac potassium, diclofenac sodium, diflunisal, etodolac, fenoprofen, flurbiprofen, ibuprofen, indomethacin, keoprofen, magnesium salicylate, meclofenamate sodium, mefanamic acid, meloxicam, nabumetone, naproxen, naproxen sodium, oxaprozin, piroxicam, salsalate, sodium salicylate, sulindac, tolmetin sodium, tolmetin sodium) or disease-modifying antirheumatic drug (DMARD) (azathioprine, chlorambucil, cyclophosphamide, cyclosporine, gold sodium, thiomalate, hydroxychloroquine, leflunomide, methotrexate, minocycline, mycophenolate mofetil, sulfasalazine, tofacitinib) use; (5) history of current opioid (oxyCODONE, HYDROcodone, codeine, fentanyl, meperidine, morphine, traMADol, HYDROmorphone, oxyMORPHONE, methadone, buprenorphine) use; (6) psychological conditions other than anxiety (ie, depression, bipolar disorder, schizophrenia, obsessive-compulsive disorder, anorexia, delusional disorder); and (7) current smoker.
The study was given a non-human research determination by our institution’s Institutional Review Board. We retrospectively identified patients who underwent an elective orthopedic procedure at PSHMC between July 2012 and September 2015. We included all patients who had the appropriate data identified in the electronic medical record; nursing intake form, current opioid, NSAID, and DMARD use, pain scores preoperative in the SDU, 24 and 48 hours postoperatively. We excluded patients less than 18 years of age or had any missing information on risk factors. We identified a nursing intake form that was populated electronically on the day the patient arrived for surgery that provided details about history of prior abuse, history of anxiety, history of illicit nonopioid drugs or alcohol abuse, and other psychological conditions. With the help of our IT department, we were also able to retrieve from the electronic medical record current opioid, NSAID, and DMARD use and their reported pain scores preoperatively, in the SDU before surgery, and 24- and 48-hour postoperatively. We compared “at risk” factors to their reported pain scores just before surgery and at 24- and 48-hour postoperatively.
The goal of our statistical analysis was to determine which of the proposed risk factors were significantly associated with preoperative pain scores, 24- and 48-hour postoperative pain scores, and to estimate the magnitude of the association. We also tested whether the total number of risk factors was associated with preoperative pain. We modeled the pain score using simple linear regression, controlling for each potential risk factor and total risk factor burden. The coefficient from these regressions quantified the association with the pain score and a t test was used to test the hypothesis that each coefficient was 0.
RESULTS
We identified 1923 patients undergoing elective orthopedic procedures between July 2012 and September 2015 who had all available information by chart review. The distribution of procedures identified is listed in Table 1. Hip, knee, and shoulder replacement accounted for 76.0% of the procedures. The average baseline pain scores reported in the SDU, 20 to 24, and 24 to 48 hour time frames postoperatively for each of these subspecialty groups are found in Figure 1. Patients undergoing elective trauma procedures (patients with a trauma injury that did not require hospital admission and come back for their surgery as an outpatient) had higher average pain scores before surgery. Table 2 shows the distribution of “at risk” scores. 78.5% of patients had 3 or fewer “at risk” factors and only 17.1% had no “at risk” factors. Table 3 shows the “at risk factors” by type of surgical procedure. Several risk factors were associated with pain scores across all 3 time periods, including anxiety, other psychological conditions, smoking, and use of opioids. In addition, the number of at risk factors had a significant, though diminishing, association with pain at each time period. Each additional risk factor as associated with an increase in pain score of 0.41 (P<0.0001) in the presurgery period. This association fell to 0.34 (P<0.0001) at 20 to 24 hours and 0.30 (P<0.0001) per each additional at risk factor at 24 to 48 hours after surgery.
TABLE 1.
Distribution of Orthopedic Procedures
| Procedure | Frequency | Percent |
|---|---|---|
| Biopsy | 24 | 1.26 |
| Elbow | 29 | 1.53 |
| Foot and ankle | 92 | 4.84 |
| Hand | 13 | 0.68 |
| Hip replacement | 336 | 17.68 |
| Knee other | 33 | 1.74 |
| Lower extremity amputation | 52 | 2.74 |
| Other | 164 | 8.63 |
| Shoulder arthroplasty | 188 | 9.89 |
| Shoulder other | 18 | 0.95 |
| Total knee | 920 | 48.42 |
| Trauma | 31 | 1.63 |
| Total | 1900 | 100.00 |
Knee other indicates knee surgery that is not a “knee joint replacement” surgery.
FIGURE 1.
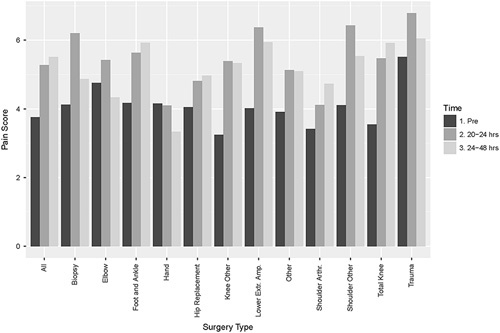
Average preoperative, 20 to 24 hours postoperative, and 24 to 48 hours postoperative pain scores.
TABLE 2.
Distribution of the Total Number of Risk Factors for Patients Undergoing Elective Surgeries
| Risk Factors | N (%) |
|---|---|
| 0 | 325 (17.11) |
| 1 | 712 (37.47) |
| 2 | 544 (28.63) |
| 3 | 236 (12.42) |
| 4 | 71 (3.74) |
| 5 | 12 (0.63) |
| Total | 1900 (100.00) |
TABLE 3.
At-risk Factors by Type of Procedure
| At-risk Factors | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Procedure | N | Abuse (%) | Anxiety (%) | Drugs/Alcohol (%) | Medications (%) | Psychological (%) | Smoking (%) | Narcotics (%) | Anti-inflammatories (%) | No. Risk Factors |
| Biopsy | 24 | 0.00 | 16.67 | 20.83 | 29.17 | 20.83 | 8.33 | 0.00 | 0.00 | 0.96 |
| Elbow | 29 | 3.45 | 17.24 | 44.83 | 37.93 | 17.24 | 3.45 | 0.00 | 0.00 | 1.24 |
| Foot and ankle | 92 | 0.00 | 25.00 | 38.04 | 53.26 | 31.52 | 17.39 | 2.17 | 2.17 | 1.65 |
| Hand | 13 | 0.00 | 15.38 | 53.85 | 38.46 | 15.38 | 38.46 | 0.00 | 0.00 | 1.62 |
| Hip replacement | 336 | 1.19 | 17.86 | 47.92 | 51.49 | 17.26 | 13.69 | 0.89 | 1.49 | 1.49 |
| Knee other | 33 | 0.00 | 21.21 | 39.39 | 51.52 | 33.33 | 15.15 | 3.03 | 3.03 | 1.61 |
| Lower extremity amputation | 52 | 1.92 | 26.92 | 26.92 | 48.08 | 23.08 | 15.38 | 0.00 | 0.00 | 1.42 |
| Other | 164 | 0.61 | 15.24 | 32.32 | 43.29 | 19.51 | 12.20 | 1.22 | 1.83 | 1.23 |
| Shoulder arthroplasty | 188 | 1.06 | 16.49 | 36.70 | 56.91 | 29.26 | 13.30 | 2.13 | 0.00 | 1.54 |
| Shoulder other | 18 | 11.11 | 22.22 | 44.44 | 50.00 | 27.78 | 22.22 | 5.56 | 0.00 | 1.78 |
| Total knee | 920 | 0.76 | 17.39 | 39.57 | 63.04 | 23.26 | 10.65 | 0.22 | 1.30 | 1.55 |
| Trauma | 31 | 3.23 | 22.58 | 29.03 | 51.61 | 29.03 | 9.68 | 0.00 | 0.00 | 1.45 |
Knee other indicates knee surgery that is not a “knee joint replacement” surgery.
Table 4 shows the relationships between “at risk” factors and baseline pain scores. Anxiety (P<0.0001), other psychological conditions (P<0.0001), current opioid use (P=0.009), and current smoker (P<0.0001) were significantly associated with higher preoperative pain scores (presurgical scores in the SDU). In the 20 to 24 hours’ time frame postoperatively, anxiety (P<0.0001), other psychological conditions (P<0.0001), current smoker (P<0.0001), and opioids (P=0.003) or NSAIDs (P=0.019) were significantly associated with higher pain scores. There was a negative correlation (lower pain scores) between alcohol or illicit drug use (nonopioid) and 20 to 24 hours pain scores (P=0.033). In the 24 to 48 hour time frame postoperatively; anxiety (P<0.0001), other psychological conditions (P=0.0), current smoker (P=0.001), and opioids (P=0.035) were also significantly associated with increased pain scores. Again, alcohol or illicit drug use had a negative correlation with increased pain scores at 24 to 48 hours (P=0.035).
TABLE 4.
Simple Linear Regression Results
| Score | Presurgery | 24 h | 48 h | |||
|---|---|---|---|---|---|---|
| Component | Coefficient | P | Coefficient | P | Coefficient | P |
| Abuse | 1.039 | 0.125 | 0.397 | 0.597 | 0.358 | 0.613 |
| Anxiety | 0.848 | <0.0001 | 0.784 | <0.0001 | 0.852 | <0.0001 |
| Drugs/alcohol | 0.086 | 0.535 | −0.326 | 0.033 | −0.295 | 0.035 |
| DMARDs | 0.163 | 0.230 | 0.356 | 0.018 | 0.312 | 0.025 |
| Psychological conditions other than anxiety | 0.923 | <0.0001 | 0.855 | <0.0001 | 0.666 | 0.000 |
| Smoking | 1.016 | <0.0001 | 1.001 | <0.0001 | 0.724 | 0.001 |
| Opioids | 1.988 | 0.009 | 2.763 | 0.003 | 1.667 | 0.035 |
| NSAIDs | 0.050 | 0.936 | 1.646 | 0.019 | −0.026 | 0.967 |
| No. risk factors | 0.411 | <0.0001 | 0.342 | <0.0001 | 0.296 | <0.0001 |
The coefficient represents the effect of the presence of the risk factor on the preoperative, 24-hour, or 48-hour pain score. For example, patients with diagnosed anxiety had on average preoperative pain scores that were 0.848 points higher than patients without diagnosed anxiety.
DMARDs indicates disease-modifying antirheumatic drug; NSAIDs, nonsteroidal anti-inflammatory drugs.
DISCUSSION
Many studies have investigated different aspects of pain and pain control measures including anesthesia type, medication class used, psychosocial risk factors, and others. To better serve our patients, we embarked on a project to investigate “at risk” factors for inadequate perioperative pain control. The results indicate that anxiety, current smoking, other psychological conditions, and preoperative opioid use were significantly associated with higher reported pain scores before surgery, at 20 to 24 hours postoperatively, and at 24 to 48 hours postoperatively, In addition, previous NSAID use was significantly associated with increased pain scores at 20 to 24 hours postoperatively but not with the preoperative or 24 to 48 hours postoperative pain scores. We also showed that history of alcohol or illicit drug use (nonopioid) correlated negatively with the 20 to 24 and 24 to 48 hour postoperative scores, meaning that these patients reported lower pain scores. This is an interesting finding, and the reason is unclear. We propose that patients that have a history of anxiety, current smoking, other forms of psychological distress, and current preoperative opioid use may be “at risk” for inadequate pain control, and that these criteria could be utilized to help identify a patient population that may benefit from specialized pain management approaches preoperatively and postoperatively. We also found that the total burden of at risk factors was associated with pain scores, and greater numbers of at risk factors were significantly associated with higher pain scores at all 3 time periods.
Anxiety and Smoking Risk Factors
Several other studies support that anxiety and other forms of psychological distress are risk factors for increased pain postoperatively. Suffeda et al10 investigated the influence of depression, anxiety, and resilience on postoperative pain on the first day after otolaryngology surgery and found that higher levels of depression and anxiety correlated with higher levels of postoperative pain. The authors concluded that certain psychosocial parameters could be utilized to identify patients at higher risk for increased pain at 24 hours postoperatively. Mulligan et al5 examined psychosocial risk factors associated with inadequate pain control after elective ankle and hindfoot reconstruction. They identified mood disorder as a significant risk factor for increased pain postoperatively, as well as initial postoperative opioid use. Mulligan and colleagues also found that tobacco use was associated with significantly increased pain postoperatively which is similar to our findings. Schreiber et al8 investigated risk factors for chronic pain following breast cancer surgery, and found that psychosocial dysfunction like anxiety and depression increased the risk for chronic pain. Skeppholm et al9 discovered that preoperative emotional distress was associated with poor outcomes following surgery for cervical radiculopathy and emphasized the importance of developing a pathway to help patients with high levels of anxiety and depression. Similarly, Davies et al11 found that 16% of Americans with mental health disorders receive over half of all opioids prescribed in the United States, and recognized this is as a population in need of improved pain control. Shah et al13 investigated rates and risk factors for opioid dependence and overdose after urological surgery and found that risk factors for opioid dependence included baseline depression, and tobacco use. Our findings are consistent with past research and support that anxiety, other forms of psychological distress, and smoking are risk factors for increased reported pain by the patient. We feel that these are important conditions to consider when identifying patients who may be “at risk” for inadequate pain control postoperatively and warrants discussion with these patients preoperatively and possibly a different pain control regimen postoperatively.
Current Opioid Use Risk Factor
Preoperative opioid use has been associated with poor pain control postoperatively.3,5,7,8 There is a growing body of literature that supports that tolerance for opioids and opioid-induced hyperalgesia (OIH) can develop in patients who are on opioids for even short periods of time. Opioid tolerance is a phenomenon where increasing opioid doses are required for analgesia due to desensitization at the opioid receptor. Opioid tolerance can develop quickly in opioid naive patients, and high intraoperative doses have demonstrated increased postoperative pain and opioid requirements.15 An underappreciated phenomenon, OIH is a nociceptive sensitization related to neuroplastic changes in the central and peripheral nervous systems which causes increased pain at higher opioid doses.14–17 To prevent opioid tolerance and OIH, preoperative assessment should include clarification of pre-existing pain and functional limitations, current opioid medications with dosing and frequency, current opioid prescriber and dispensing pharmacy, current nonopioid analgesics, past opioid medications and their effectiveness, review of opioid misuse, and pain level expectations associated with procedure.15 In our analysis, we also identified that preoperative opioid use was a significant risk factor for increased reported pain by patients. This highlights the importance of shifting the focus of pain management away from opioids and using multimodal pain management strategies.16 We found that NSAID/DMARD use preoperatively was not associated with higher pain scores except in the 20 to 24 hours postoperative period. NSAID/DMARD use is often discontinued days before surgery so the use of an NSAID as a bimodal approach to pain control, in addition to opioids, may be even more helpful to patients who were taking these drugs preoperatively.
Multimodal Pain Management Approaches
Multimodal pain management approaches are being developed to limit long-term postoperative opioid use. Hansen et al3 compared length of stay and hospitalization costs for orthopedic surgery patients treated with intravenous acetaminophen and intravenous opioids versus intravenous opioids alone. They found that patients who received intravenous acetaminophen had statistically significant shorter length of stay and lower hospitalization costs when compared with patients treated with intravenous morphine alone. In addition, patients who received acetaminophen also had lower rates of respiratory depression, surgical site infections, and urinary tract infections.3
Adult Pain Management Orderset
In response to our findings, the IPT developed a comprehensive orderset (Figs. 2–4), that can be utilized institution wide, to give providers guidance when ordering pain modalities for patients. It helps to highlight mild, moderate, and severe pain management modality options that can be considered when prescribing medications for pain control. By categorizing the medications options by pain level (mild, moderate, or severe) the prescribing provider is given suggestions of the types of pain modalities to consider for the level of pain that they expect the patient to have relative to their procedure. It may be that the provider feels that the patient needs an opioid drug even though they expect the patient to have mild pain but the orderset serves to remind them that they could prescribe the opioid at a lower dose or even consider using a nonopioid drug if they believe this to be reasonable. We believe that if the provider has options in front of them, and they consider the level of pain, that this will decrease the instinct to provide only opioid drugs for pain control. It also includes a bowel regime recognizing that poor bowel control can also play a role in poor patient satisfaction and pain control. The overarching theme to developing the pain orderset was to try to limit opioid drug options and recognize that there are other effective nonopioid pain modalities. Other nontraditional pain modalities are also highlighted, including music therapy, physical therapy and, when needed, an acute pain team consultation for patients having severe pain or for patients felt to be “at risk” for pain. We are considering instituting preoperative counseling for mood disorders or pathways to reduce opioid use preoperatively as well.
FIGURE 2.
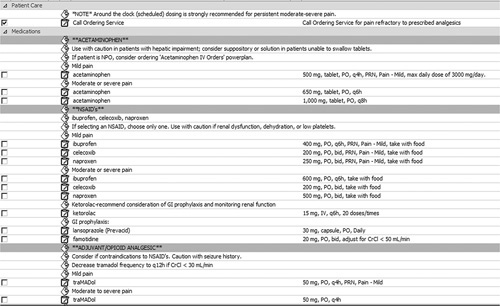
Pain management adult orderset; page 1.
FIGURE 4.
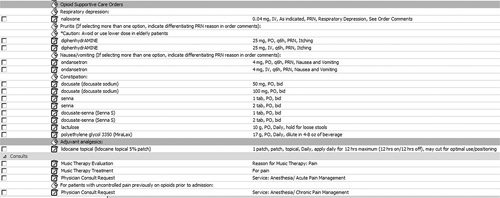
Pain management adult orderset; page 3.
FIGURE 3.
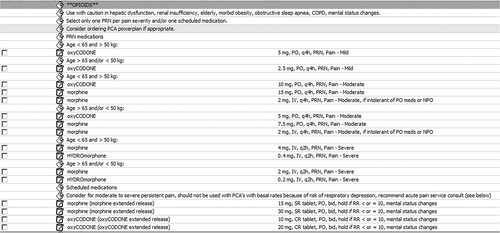
Pain management adult orderset; page 2.
The American Academy of Orthopaedic Surgeons (AAOS) released a set of recommendations in response to the opioid epidemic.2 This has led to the development of a nationwide tracking system to allow pharmacists and surgeons to see all prescriptions filled by patients. It is hoped that this will lead to quality improvement to integrate substance use disorder screening and stricter opioid prescribing, but at the same time appropriately treat patients with terminal illness and other conditions that should have access to chronic pain medications, shifting the focus of pain management away from opioids. These recommendations specifically state that opioids should not be prescribed for preoperative and nonsurgical patients.2 In a recent article, Soffin et al18 described an evidence-based approach to the prescription opioid epidemic in orthopedic surgery and highlighted 5 main components: (1) guidelines for managing patients who are opioid tolerant and/or have a substance abuse disorder; (2) education programs for patients that highlight the role of opioids after elective orthopedic surgery; (3) education programs for prescribers of opioids; (4) the development of surgery-specific prescribing recommendations for opioid naïve patients; and (5) mechanisms to modify prescribing habits to limit unnecessary prescribing of controlled substances. Demsey and colleagues investigated the risk of opioid addiction in plastic surgery patients in the perioperative period and recommended using an opioid risk tool to provide guidance on appropriate screening questions including age, sex, family and/or personal history of substance abuse, psychological disease, and history of preadolescent sexual abuse. They recommend using this tool to communicate to patients their risk preoperatively of becoming addicted to opioids.12 We believe that our findings support all of these recommendations and provide evidence that these “at risk” characteristics do correlate with preoperative and postoperative pain scores. Educating patients and providers about these “at risk” factors can also help guide discussions and treatment plans.
Our study has limitations. It is a retrospective collection of data and the “at risk” factors were only studied in a population of orthopedic surgery patients. Expanding the data to other patient populations offers a direction for future research. Some of the “at risk” factors such as anxiety, depression, other psychological conditions, and abuse history are self-reported to the nurse on the intake form by the patient and may over-state or under-state the real incidence of these conditions. We feel, however, a strength to our study was the large patient population studied.
In summary, we found a significant association between anxiety, current smoking, other psychological conditions, and current opioid use with an increased preoperative, 20 to 24 hours postoperative, and 24 to 48 hours postoperative patient-reported pain score. Since this information can be collected in an automated electronic format, we propose that these “at risk” factors could be utilized to help identify patients that may need more attention to their pain control postoperatively. We feel that these “at risk” factors could be integrated into handoff communication between physicians and facilitate communication with the patient. We support that multimodal pain control options are a better option than just increasing the amount of opioids to control pain postoperatively, and we have developed a pain orderset to help guide providers when prescribing pain modalities.
Footnotes
Interdisciplinary Pain Team included: April Armstrong, MD (Chair), Sanjib Adhikary, MD, Carol Freer, MD, Vitaly Gordin, MD, Susan Hassenbein, CCRP, Everett Hills, MD, James Mooney, MD, Stephen Mrozowski, MHA, NRP, Christopher O'Hara, MD, Susan Riemondy, BSN, RN-BC, Jeffrey Sherwood, PT, Jeffrey Sivik, PharmD, Janice W. Stouffer, MT-BC, and Cynthia Smulligan, RN, ONC. Penn State College of Medicine, Penn State Health Milton S. Hershey Medical Center, 30 Hope Drive, EC089, PO Box 859, Hershey, PA 17033.
The authors declare no conflict of interest.
REFERENCES
- 1.Drug Overdose Death in the United States Continues to Increase; 2015. Available at: CDC.gov/drugoverdose/epidemic Accessed 2016.
- 2.American Academy of Orthopedic Surgeons (AAOS). Information Statement: Opioid Use, Misuse, and Abuse in Orthopedic Practice; 2015. Available at: aaos.org Accessed 2016.
- 3.Hansen RN, Pham A, Strassels SA, et al. Comparative analysis of length of stay and inpatient costs for orthopedic surgery patients treated with IV acetaminophen and IV opioids vs. IV opioids alone for post-operative pain. Adv Ther. 2016;33:1635–1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khalili G, Salimianfard M, Zarehzadeh A. Comparison between paracetamol, piroxicam, their combination, and placebo in postoperative pain management of upper limb orthopedic surgery (a randomized double blind clinical trial). Adv Biomed Res. 2016;5:114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mulligan RP, McCarthy KJ, Grear BJ, et al. Psychosocial risk factors for postoperative pain in ankle and hindfoot reconstruction. Foot Ankle Int. 2016;37:1065–1070. [DOI] [PubMed] [Google Scholar]
- 6.Seangleulur A, Vanasbodeekul P, Prapaitrakool S, et al. The efficacy of local infiltration analgesia in the early postoperative period after total knee arthroplasty: a systematic review and meta-analysis. Eur J Anaesthesiol. 2016;33:816–831. [DOI] [PubMed] [Google Scholar]
- 7.Bateman BT, Franklin JM, Bykov K, et al. Persistent opioid use following cesarean delivery: patterns and predictors among opioid-naive women. Am J Obstet Gynecol. 2016;215:e1–e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schreiber KL, Kehlet H, Belfer I, et al. Predicting, preventing and managing persistent pain after breast cancer surgery: the importance of psychosocial factors. Pain Manag. 2014;4:445–459. [DOI] [PubMed] [Google Scholar]
- 9.Skeppholm M, Fransson R, Hammar M, et al. The association between preoperative mental distress and patient-reported outcome measures in patients treated surgically for cervical radiculopathy. Spine J. 2017;17:790–798. [DOI] [PubMed] [Google Scholar]
- 10.Suffeda A, Meissner W, Rosendahl J, et al. Influence of depression, catastrophizing, anxiety, and resilience on postoperative pain at the first day after otolaryngological surgery: a prospective single center cohort observational study. Medicine (Baltimore). 2016;95:e4256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davis MA, Lin LA, Liu H, et al. Prescription opioid use among adults with mental health disorders in the United States. J Am Board Fam Med. 2017;30:407–417. [DOI] [PubMed] [Google Scholar]
- 12.Demsey D, Carr NJ, Clarke H, et al. Managing opioid addiction risk in plastic surgery during the perioperative period. Plast Reconstr Surg. 2017;140:613e–619e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shah AS, Blackwell RH, Kuo PC, et al. Rates and risk factors for opioid dependence and overdose after urological surgery. J Urol. 2017;198:1130–1136. [DOI] [PubMed] [Google Scholar]
- 14.Webster LR. Risk factors for opioid-use disorder and overdose. Anesth Analg. 2017;125:1741–1748. [DOI] [PubMed] [Google Scholar]
- 15.Wenzel JT, Schwenk ES, Baratta JL, et al. Managing opioid-tolerant patients in the perioperative surgical home. Anesthesiol Clin. 2016;34:287–301. [DOI] [PubMed] [Google Scholar]
- 16.Wibbenmeyer L, Eid A, Kluesner K, et al. An evaluation of factors related to postoperative pain control in burn patients. J Burn Care Res. 2015;36:580–586. [DOI] [PubMed] [Google Scholar]
- 17.Lee M, Silverman SM, Hansen H, et al. A comprehensive review of opioid-induced hyperalgesia. Pain Physician. 2011;14:145–161. [PubMed] [Google Scholar]
- 18.Soffin EM, Waldman SA, Stack RJ, et al. An evidence-based approach to the prescription opioid epidemic in orthopedic surgery. Anesth Analg. 2017;125:1704–1713. [DOI] [PubMed] [Google Scholar]


