In the context of the COVID-19 pandemic, information concerning secondary infections is thus far scarce and variable. While a low rate has been reported in patients with COVID-19 during hospitalization [1], this proportion increases in studies including intensive care unit (ICU) patients [2]. Furthermore, admission to ICUs with increased antimicrobial resistance is of concern. We investigated the incidence, aetiology and impact of ICU-acquired infections in COVID-19 patients admitted to an ICU with a known burden of multi-drug resistance [3]. We focused on bloodstream infections (BSIs) because these represent definite infection events, whereas distinction between colonization and infection is more difficult with other specimen types.
The study included all patients with SARS-CoV-2 infection, confirmed by reverse transcription polymerase chain reaction on nasopharyngeal swabs, consecutively admitted to the 28-bed COVID-ICU at Evangelismos Hospital, in Athens (Greece) between 19th March and 20th May 2020. Baseline clinical and laboratory data and illness severity, assessed by Sequential Organ Failure Assessment (SOFA) score, were recorded. ICU-acquired BSI was defined as a pathogen isolation from ≥1 blood specimen obtained at more than 48 h after ICU admission. In patients with ≥2 BSIs, only the first one was included, unless the subsequent episode was fungal. Comparisons between patients with and without BSI were performed by Mann–Whitney U-test and Chi-squared or Fisher's exact tests, when appropriate. Data were expressed as median (interquartile range) or percentages.
Among 50 patients admitted during the study period, (median age 64 years, 76% male, 82% rate of mechanical ventilation, 72% at least one documented serious comorbidity), 20 (40%) had ≥1 episode of bacteraemia and seven (14%) developed candidaemia. Overall, 50 episodes of ICU-acquired BSIs were registered (incidence 48 episodes per 1000 patient-ICU days).
Gram-negative pathogens predominated, including extensively drug-resistant and pan-drug resistant Acinetobacter baumannii (four and three patients, respectively) and Klebsiella pneumonia carbapenemase-positive K. pneumonia (four patients). Amongst Gram-positive bacteria Enterococcus spp. predominated (six patients). There were four Candida albicans and three C. parapsilosis.
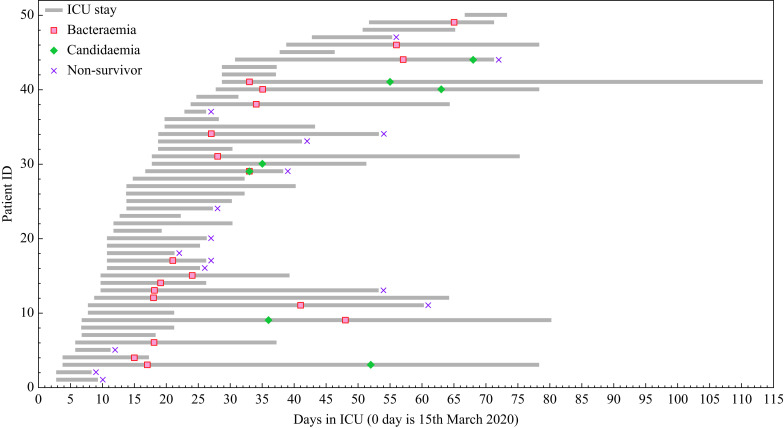
BSI was associated with the following on admission: increased lactate dehydrogenase values (559 (214) vs 421 (173) IU/L, P<0.001) and history of hypertension (50% vs 17%, P<0.01). SOFA score was not associated with BSI acquisition (8 (3) vs 6 (7), P=0.14). Time from ICU admission to BSI onset was 11 (7) days. Specifically, bacterial BSI development occurred 10 (6) days after ICU admission, whereas fungal BSIs had a later onset at 27 (20) days (Figure 1 ).
Figure 1.
Timeline for each individual patient with COVID-19 consecutively admitted to the intensive care unit (ICU) during the first pandemic wave. The case number reflects, for each patient, the date of ICU admission to date of death or discharge from the ICU. Red indicates the day of the first Bacteraemia; green indicates the day of Candidaemia, ×indicates the day of death. A polymicrobial population (one strain of Candida and one strain of Gram-negative bacterium) simultaneously grown by the same blood culture in one patient is shown with both colours.
BSI acquisition was associated with increased duration of mechanical ventilation and length of ICU stay compared with no-BSI acquisition: 33 (26) vs 5 (11) and 38 (31) vs 10 (7) days, respectively, P<0.001). Candidaemia was more frequent among patients with a previous BSI compared with those without (31.5% vs 3.2%, P<0.05). Survival time after the first episode of BSI in those patients who died was 19.5 (23) days. Crude ICU mortality was 32%, not significantly different between patients with and without BSIs (33% and 30%, respectively).
The observed incidence of 40% of bacterial BSIs is in contrast with that of 11.9% in New York City hospitals [4] as well as with an 8.1% of secondary infections in a meta-analysis [5], both proportions reported in COVID-ICU patients. Nevertheless, it is comparable with subsequent findings showing an incidence of ICU-acquired infections up to 51.2%, including a BSI rate at 30.7% [2]; also, with a reported increase in Gram-negative BSIs identified in COVID-ICUs [6]; as well as with an estimated risk of 25% for BSI within 15 days after COVID-ICU admission [7].
Notably, our study period represents the first COVID-19 pandemic wave. At that time, our patients did not receive dexamethasone or other immunomodulatory agents. Unsurprisingly, microbiology and antimicrobial resistance patterns reflected our local ICU ecology, as previously reported [3]. In accordance, among COVID-19 patients, pathogens detected in hospital-acquired BSIs were similar to those of patients without COVID-19 in a recent study [8]. High workloads potentially may have contributed to increased rate in both BSIs and transmissions inside the ICU.
Although an increased mortality rate among COVID-19 patients with ICU-acquired BSI has been reported [2], we did not find such an association. Highly supportive care and administration of synergistic combinations of antimicrobials in pan-drug resistant pathogens, may have contributed to this result. However, since clinical outcome in severe COVID-19 patients is multifactorial, no definite conclusion can be reached.
In summary, among COVID-19 patients we observed an increased incidence of ICU-acquired BSIs, mostly due to multi-drug-resistant pathogens. BSI development was associated with prolonged duration of mechanical ventilation and ICU stay, though without difference in clinical outcome. Infection control and stewardship strategies to prevent dissemination of multi-drug resistance are needed.
Acknowledgements
The authors wish to thank Professor George Ganos for developing the Figure and all ICU staff for their hard work during the pandemic.
Footnotes
This work was presented at the ESCMID Conference on Coronavirus Disease (ECCVID) 23rd–25th September 2020, e-poster ID 00479.
Conflict of interest statement
None declared.
Funding sources
None.
References
- 1.Garcia-Vidal C., Sanjuan G., Moreno-García E., Puerta-Alcalde P., Garcia-Pouton N., Chumbita M. Incidence of co-infections and superinfections in hospitalized patients with COVID-19: a retrospective cohort study. Clin Microbiol Ιnfect. 2020 doi: 10.1016/j.cmi.2020.07.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Soriano M.C., Vaquero C., Ortiz-Fernandez A., Caballero A., Blandino-Ortiz A., de Pablo R. Low incidence of co-infection, but high incidence of ICU-acquired infections in critically ill patients with COVID-19. J Infect. 2020 doi: 10.1016/j.jinf.2020.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Routsi C., Gkoufa A., Arvaniti K., Kokkoris S., Tourtoglou A., Theodorou V. De-escalation of antimicrobial therapy in ICU settings with high prevalence of multidrug-resistant bacteria: a multicentre prospective observational cohort study in patients with sepsis or septic shock. J Antimicrob Chemother. 2020;75:3665–3674. doi: 10.1093/jac/dkaa375. [DOI] [PubMed] [Google Scholar]
- 4.Goyal P., Choi J.J., Pinheiro L.C., Schenck E.J., Chen R., Jabri A. Clinical characteristics of Covid-19 in New York City. N Engl J Med. 2020;382:2372–2374. doi: 10.1056/NEJMc2010419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Langford B.J., So M., Raybardhan S., Raybardhan S., Leung V., Westwood D. Bacterial co-infection and secondary infection in patients with COVID-19: a living rapid review and meta-analysis. Clin Microbiol Infec. 2020 doi: 10.1016/j.cmi.2020.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sturby A., Basarab M., Cotter M., Hager K., Shakespeare D., Shah N. Severe OVID-19 and healthcare-associated infections on the ICU: time to remember the basics? J Hosp Infect. 2020;105:593–595. doi: 10.1016/j.jhin.2020.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Giacobbe D.R., Battaglini D., Ball L., Brunetti I., Bruzzone B., Codda G. Blood stream infections in critically ill patients with COVID-19. Eur J Clin Invest. 2020;50 doi: 10.1111/eci.13319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Engsbro A.L., Israelsen S.B., Pedersen M., Tingsgaard S., Lisby G., Andersen C.Ø. Predominance of hospital-acquired blood stream infection in patients with Covid-19 pneumonia. Infect Dis. 2020;52:919–922. doi: 10.1080/23744235.2020.1802062. [DOI] [PubMed] [Google Scholar]