Highlights
-
•
Psychiatric emergencies were lower during the COVID-19 period compared to 2019.
-
•
During COVID-19 more schizo psychotic patients were attended in the emergency.
-
•
During COVID-19 fewer anxiety/adaptive patients were attended in the emergency.
-
•
A lower discharge/emergency ratio was observed during the COVID-19 outbreak.
-
•
A higher referral to Internal Medicine ratio was observed during the COVID-19 outbreak.
Keywords: Covid-19, Confinement, State of emergency, Emergency, Psychiatry, Psychosis, Anxiety
Abstract
The SARS-CoV-2 pandemic has caused an unprecedented clinical situation. A retrospective cross-sectional study was designed with the aim to evaluate psychiatric emergencies from March 14 to May 1, 2020, coinciding with the start of the emergency state and the lockdown until the attenuation of the confinement. Data obtained during this period were compared with the emergencies attended in the same period of 2019. A total of 213 psychiatric emergencies were attended in 2020 compared with 367 in 2019. The mean number of emergencies per day was significantly lower during the COVID-19 outbreak in 2020 (M=4.35, SD= 2.04) vs. the same period in 2019 (M=7.50, SD= 3.18). A higher percentage of patients with schizo/psychotic disorders (34.3% in 2020, vs. 24.3% in 2019), as well as a lower percentage of patients with anxiety/adaptive disorders (25.4% in 2020 vs. 35.4% in 2019) was observed during the outbreak. A significant lower mean discharge/emergency ratio (M=42.17, SD= 26.94 in 2020 vs. M=63.43, SD= 17.64 in 2019) and a higher referral to Internal Medicine/emergency ratio (M=20.55, SD= 22.16 in 2020 vs. M=3.32, SD= 6.63 in 2019) was observed. The results suggest important changes in psychiatric emergencies during the most critical period of the COVID-19 outbreak in Spain.
1. Introduction
In December 2019, a cluster of cases of pneumonia of unknown etiology were reported in the Chinese city of Wuhan. Shortly after, a new variety of coronavirus named SARS-CoV-2 was identified (Wu et al., 2020b,a; Zhu et al., 2020; Zhou et al., 2020). This virus is responsible of causing the coronavirus disease 2019 (COVID-19), an outbreak that has rapidly spread worldwide and has caused an unprecedented pandemic that has shocked the entire world population.
Moreover, the high person to person transmission, the risk of developing a severe respiratory syndrome among vulnerable patients with comorbid chronic diseases and in the elderly (Wu et al., 2020b) together with the absence of an effective treatment or vaccine (Peng et al., 2020; Wu, Leung, and Leung, 2020c) forced the WHO to declare COVID-19 outbreak a health emergency of international concern on January 30, 2020 and a state of global pandemic on March 11, 2020 (World Health Organization, 2019). As a consequence, government entities in different countries, including Spain, took drastic measures to restrict the mobility of its inhabitants and imposed a mass quarantine (BOE, 2020).
On January 31, 2020, the first imported case in Spain was detected in La Gomera island, and a few weeks later the trickle of cases hit other peninsular areas from where it spread throughout the rest of the country. On March 4, the first death from coronavirus was registered in Spain when the number of affected cases in the country amounted to 193. The contagion began to increase exponentially and unstoppably, leading the government to decree the state of emergency and order confinement on March 14 (BOE, 2020). In that moment, 4.209 confirmed cases on March, 13 (ISCIII, 2020) and up to 9.191 confirmed cases on March, 16 (ISCIII, 2020) had already been registered in Spain.
From this date, the Spanish general population has been strictly confined, except to ensure that basic food or medical care needs are met. The number of infected cases in Spain started growing alarmingly as well as the number of deaths, leading the Spanish health system to reach a critical situation. Within the different geographical areas in the country, the Community of Madrid has been one of the most affected, with numerous hospitals' intensive care units overcrowded and with a collapse in the emergency services. This situation made it necessary to rapidly build The IFEMA field hospital in Madrid that opened on March 22 and began to admit patients with COVID-19 to support the health system. All these circumstances have generated a situation of social alarm without precedent in the previous decades in Spain. By the end of April, a clear decrease in the number of infected and deceased people began to be observed. As a consequence of this decrease in the number of cases, The IFEMA field hospital was closed on May 1, after having treated up to 4,000 patients with coronavirus. On May 2, for the first time since the beginning of confinement, people were authorized to go outside to walk or play sports in a controlled manner and under strict time slots.
Different published studies have emphasized the impact that this situation of pandemic, mass quarantine, and social alarm has had on the mental health of the general population (Brooks et al., 2020; Campion et al., 2020; Holmes et al., 2020) and in people with serious mental illness (Iasevoli et al., 2020) during the COVID-19 outbreak. However, studies with real quantitative data are still scarce. On the one hand, it could be argued that since this situation has increased the levels of anxiety, depression, and acute stress (Huang and Zhao, 2020), an increase in the number of people consulting for psychiatric emergency care would be expected; however, the fear of contagion in hospitals and the avalanche of information from the media regarding the collapse of emergencies by COVID patients could have had a deterrent effect limiting the demand for urgent psychiatric care and assistance. Thus, the objective of this study is to quantitatively and qualitatively study the functioning of psychiatric emergencies during the most critical period of the COVID-19 outbreak in one of the main hospitals in Madrid, and to compare it with a similar period in the previous year.
2. Methods
We designed a retrospective cross-sectional study evaluating the functioning of psychiatric emergency service utilization in “University Hospital 12 de Octubre” in Madrid, which serves a wide catchment area of around 450.000 inhabitants. The study started on March 14, the start date of the state of emergency and confinement in Spain, and ended on May 1, the day before the measures of confinement were relaxed and going for a walk and practicing sports respecting time slots began to be allowed. During this period, COVID-19 confirmed patients ranged from 4.209 cases on March, 13 (ISCIII, 2020) to 213.435 cases on April, 29 (ISCIII, 2020). Data obtained during this period were compared with the psychiatric emergencies attended in the same hospital during the same period (March 14 to May 1) of the previous year, 2019.
Data regarding age, gender, number of emergency services per day, as well as number of total emergencies throughout the two studied periods were registered. Furthermore, the diagnoses of those patients seeking medical emergency attention was registered and grouped into different diagnostic categories: schizo psychotic disorders, bipolar disorders, depressive disorders, substance use disorders, dementia-degenerative disorders, anxiety/adaptive disorders, personality disorders and other disorders. In the case of people with schizo psychotic disorders, whether they came to the emergency room voluntarily or involuntarily, as well as whether they came because of an exacerbation of psychotic symptoms or for any other different reason was also collected. In addition, the visit-day ratio of discharges, admissions, referrals from Psychiatry Services to Internal Medicine Services, and referrals to different hospitals, in those patients in whom, due to administrative reasons, their medical care could not be attended by the hospital where the study was conducted, were recorded. Finally, in those patients who were admitted to psychiatry hospitalization, PCR for SARS-CoV-2 was performed and the result was collected.
The study was approved by the local clinical research ethics committee.
2.1. Statistical analysis
For descriptive purposes, the mean and standard deviation were used for quantitative variables and percentages for qualitative variables. Comparisons of means between groups were made using the Student's t test. Chi-square comparison between percentages in each group were used. The IBM SPSS Statistics Version 25.0 software package was used to perform the statistical analysis.
3. Results
Regarding patients' gender and age, no significant differences were found between the two evaluated time periods. During the COVID-19 outbreak selected period in 2020, 50.2% of the sample was made up of men, while in the 2019 comparison time frame 43.6% were male (χ2 (1) = 2.39, p = .122). In addition, during the COVID-19 outbreak period in 2020, the mean age of the sample was 42.6 (SD 17.1) years, while in the 2019 comparison period the mean age was 40.8 years (SD 15.8) (t (578) = -1.253, p = .211) with no differences.
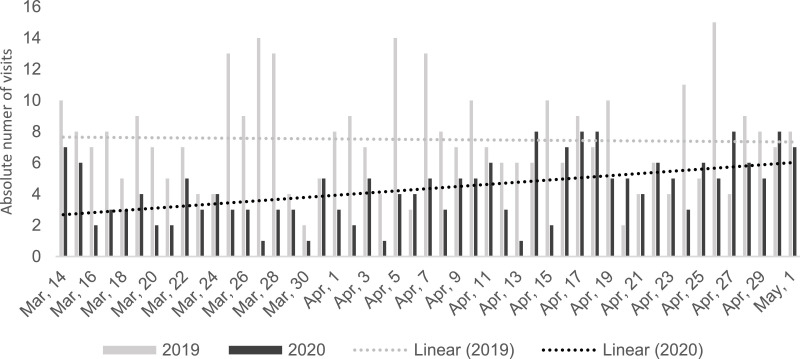
During the studied COVID-19 outbreak period in 2020, a total of 213 emergency cases were attended. In the same period in 2019, up to 367 psychiatric emergencies were registered. The mean number of emergencies per day in the COVID-19 outbreak period in 2020 was 4.35 (SD 2.04) vs. a mean in the 2019 comparison period of 7.50 (SD 3.18), showing a significant decrease in the number of patients seeking psychiatric emergency care in 2020 (t (48) = 5.75, p < .001). Fig. 1 represents the number of visits per day to the psychiatry emergency room in both periods. A progressive trend towards a higher number of emergency room visits as the end of the study period is reached was observed during the COVID-19 outbreak in 2020 (see dotted lines in Fig. 1).
Fig. 1.
Number of visits per day to the psychiatric emergency room from March 14 to May 1, during 2019 and 2020.
As Table 1 shows, regarding to diagnosis, a decrease in absolute terms is observed for all the diagnostic categories. When the percentages of each diagnostic category are compared between the two studied periods, changes are also observed. Strikingly, an increase in the percentage of patients with schizo psychotic disorders during the COVID-19 period was observed compared with the previous year, rising from 24.3% to 34.3%, as well as a decrease in the percentage of patients diagnosed with anxiety/adaptive disorders during the COVID-19 period compared with the previous year, falling from 35.4% to 25.4%. A trend towards statistical significance differences is detected in diagnostic categories (χ2 (7) = 13.124, p = .069). In the group of people with schizo psychotic disorders, during the 2020's time frame, 74.0% had been conducted involuntarily to the emergency area, while in the same period in 2019, involuntarily attendance was just 50.6% (χ2 (1) = 9.248, p = .002). Regarding the attendance clinical reason in this group of patients, in the 2020 period, 76.7% went to the emergency department because of an exacerbation of psychotic symptoms, while in the 2019 period 74.2% of schizo phychotic patients were attended due to the same clinical reason (χ2 (1) = 0.140, p = .707).
Table 1.
Total number of attentions in psychiatric emergencies and percentage of total care by diagnostic categories from March 14 to May 1, during 2019 and 2020.
| 2019 | 2020 | |
|---|---|---|
| Schizopsychotic disorders | 89 (24.3%) | 73 (34.3%) |
| Bipolar disorders | 23 (6.3%) | 11 (5.2%) |
| Depressive disorders | 13 (3.5%) | 5 (2.3%) |
| Degenerative disorders | 13 (3.5%) | 12 (5.6%) |
| Substance use disorders | 23 (6.3%) | 19 (8.9%) |
| Anxiety/adaptive disorders | 130 (35.4%) | 54 (25.4%) |
| Personality disorders | 74 (20.2%) | 38 (17.8%) |
| Other disorders | 2 (0.5%) | 1 (0.5%) |
Table 2 shows the different ratios calculated through dividing the number of cases of each possibility of outcome (discharge, admission, referral) by the total of emergency day visits. The discharge / emergency care day ratio was significantly lower during the COVID-19 studied period compared with the same time frame in 2019 (t (48)= 4.8, p< .001). When considering the psychiatric hospitalization admissions / emergency care day ratio, a trend towards a statistically significant difference was found, suggesting an increased need for hospitalization during the outbreak of COVID-19 studied period compared to 2019 (t (48)= -1.88, p= .066). The referral ratios of patients already evaluated by a psychiatrist to Internal Medicine Services / emergency care days were statistically different between both periods, indicating a greater referral to medical services during the pandemic time frame compared to the same period in 2019 (t (48)= -5.09, p< .001). Finally, in the referral ratios to other different hospitals, no significant differences were found between both periods (t(48)= -0.66, p= .52). Regarding the PCR assessment, from March 14 to April 10, PCR was performed prior to admission in 10 of the 30 patients who were to be hospitalized (due to compatible symptoms or clinical suspicion), with 1 being positive (with a diagnosis of schizo psychotic disorder). And, since April 11, PCR had been performed systematically on all patients prior to admission in the psychiatric hospitalization department (regardless of clinical suspicion). During this second period, all PCRs performed in the 44 patients admitted have been negative.
Table 2.
Ratio [M (SD)] of referrals after assessment by the psychiatric emergency service from March 14 to May 1, during 2019 and 2020.
| 2019 | 2020 | |
|---|---|---|
| Discharges | 63.43 (17.64) | 42.17 (26.94) |
| Psychiatry Hospitalization | 20.06 (14.25) | 27.89 (24.54) |
| Internal Medicine Department | 3.32 (6.63) | 20.55 (22.16) |
| Referrals to other hospitals | 7.56 (10.43) | 9.39 (15.01) |
4. Discussion
The main objective of this study was to quantitatively and qualitatively compare assistance to the psychiatric emergency department in one of the largest hospitals located in Madrid, during the period of the greatest social alarm due to the spread of the SARS-CoV-2, the declared state of emergency and the situation of imposed confinement for the general population.
The first interesting finding is the significant reduction in emergency room visits per day, which has been decreased almost by a half compared to the previous year's rate and, although it is not the object of the present study, also in relation to historical data, amounting to 362 emergency room visits per day in 2018, 358 in 2017, and 340 in 2016. This result is surprising, bearing in mind that the research points to the exacerbation of existing mental health conditions and to the development of new ones (Druss, 2020; Yao et al., 2020) which would be logically accompanied by a substantial increase in the need for psychiatric emergency care. Hence, this striking decrease may have to do with both the mass fear of contagion in the hospital environment or “coronaphobia” (Dubey et al., 2020), and the certainty of finding a surpassed the emergency service daily reported by the media. The observed trend towards a progressive increase in the number of emergency attention as the end of the study period is reached supports this hypothesis. To date, we are only aware of a study published in Europe that found a decrease in the number of psychiatric emergencies attended at the Central Institute of Mental Health, Mannheim, Germany, during the ourtbreak of COVID-19 (Hoyer et al., 2020), similarly to the study presented.
The second important finding of the present study has to do with the type of pathology attended. Although the differences only show a trend towards statistical significance, an increase of about 10% in schizo psychotic disorders, as well as a decrease around 10% in anxiety and adaptive disorders have been definitely observed. These results seem to point to a more serious patient profile in those attending emergency room services during the COVID-19 outbreak in 2020 compared to the same period in the previous year. In the case of patients with a schizo psychotic diagnosis, the results obtained indicate that the percentage of patients attended in psychiatric emergencies due to an exacerbation of psychotic symptoms is similar in both periods, however, the percentage of patients taken to the emergency room against their will is higher during the COVID-19 outbreak period in 2020 when compared to 2019. These results could indicate that patients with a schizo psychotic diagnosis do also show a certain reluctance to go to the emergency room due to what has been mentioned previously (the mass fear of contagion in the hospital environment and the surpassed emergency service daily reported by the media), but their clinical situation makes it necessary for them to be taken to the emergency room involuntarily.
Furthermore, the results obtained related to the referral after the psychiatric emergency room visit acquire special importance. Thus, the ratio of daily discharges following emergency visits during the 2020 outbreak is significantly lower than the same rate in the 2019 comparison period. In this line, a statistical trend was found towards a higher ratio of daily hospital admissions following emergency visits in the outbreak period compared to that of 2019. These results would also support the hypothesis that a more severe patient profile has been assisted in the psychiatric emergency services during the outbreak COVID-19 studied period. In addition, the finding of a substantially higher rate of referrals to the Internal Medicine Department, once the psychiatric assessment has been carried out, in patients seeking for psychiatric emergency care during the outbreak could be related to the systematic evaluation by psychiatrists of possible suspicious symptoms of COVID-19 (fever, cough and sneezing), and the need to guarantee the absence of COVID-19 even in patients consulting for mental health symptoms. Finally, in the early stages of the outbreak coinciding with the beginning of this study, PCR for SARS-CoV-2 was only performed prior to admission in patients showing a clinical suspicion, later on, PCR has been carried out systematically in order to detect possible asymptomatic carriers.
The strengths of this study include the collection of data during the period of the greatest health crisis within the COVID-19 outbreak in Spain, together with the provenance of the sample from a large hospital in a geographical area severely punished by the pandemic. However, some limitations must also be pointed out, first, the diagnoses were based on the regular clinical interview and there was no application of structured diagnostic instruments and to end, the final destination, admitted or discharged, of patients who have been referred to other hospitals remains unknown.
To date, we are not aware of any published study that had assessed the impact of the outbreak of the COVID-19 pandemic in Spain during the current health and social crisis, measuring psychiatric emergency care in a large hospital in an area especially affected by the pandemic. The results obtained indicate that there has been a clear decrease in the number of patients seeking psychiatric emergency care, which seems to normalize as containment measures are relaxed. On the other hand, the results seem to point that during the COVID-19 outbreak a profile of patient of greater clinical severity, with less probability of returning home after emergency care, has sought for care in the psychiatric emergency department. These data emphasize the attitudinal changes that the current social and health crisis has posed for people with mental illness, one of the most vulnerable population groups (Yao et al., 2020). In future clinical emergency situations, it seems clear that there is a need to develop strategies to avoid the collapse of emergencies and thus, to ensure accessibility to psychiatric care for people with mental disorders, as well as to implement triage systems in the emergency that allow establishing separate circuits for contagious patients and virus-free patients, in order to reduce the fear of contagion in people who need to go to the emergency room due to any clinical situation.
Authors' contribution
RRJ and DR were in charge of the conceptualization and data collection. VRF took data curation and formal analysis. RRJ and LGF wrote, reviewed and edited the manuscript. All authors have approved the final document.
Role of the funding source
This research was supported in part by the by the Instituto de Salud Carlos III (grants PI16/00359, PI19/00766; Fondo de Investigaciones Sanitarias/FEDER), by the European Development Regional Fund ‘‘A way to achieve Europe’’ (ERDF), by Madrid Regional Government (R&D activities in Biomedicine S2017/BMD-3740 (AGES-CM 2-CM)) and Structural Funds of the European Union.
Declaration of Competing Interest
Dr. R. Rodriguez-Jimenez has been a consultant for, spoken in activities of, or received grants from: Instituto de Salud Carlos III, Fondo de Investigación Sanitaria (FIS), Centro de Investigación Biomédica en Red de Salud Mental (CIBERSAM), Madrid Regional Government (S2010/ BMD-2422 AGES; S2017/BMD-3740), JanssenCilag, Lundbeck, Otsuka, Pfizer, Ferrer, Juste, Takeda, Exeltis, Angelini, Casen-Recordati. All other authors declare that they have no conflict of interest.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.psychres.2020.113581.
Appendix. Supplementary materials
References
- BOE “Real Decreto 463/2020, de 14 de marzo, por el que se declara el estado de alarma para la gestión de la situación de crisis sanitaria ocasionada por el COVID-19”. Boletín Oficial del Estado. 2020;67:25390–25400. [Google Scholar]
- Brooks S.K., Webster R, K Smith, L E, Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. Lancet Publishing Group. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campion J., Javed A., Sartorius N., Marmot M. Addressing the public mental health challenge of COVID-19. Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30240-6. Elsevier. 0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Druss B.G. Addressing the COVID-19 pandemic in populations with serious mental illness. JAMA Psychiatry. 2020 doi: 10.1001/jamapsychiatry.2020.0894. American Medical Association. [DOI] [PubMed] [Google Scholar]
- Dubey S., Biswas P., Ghosh R., Chatterjee S., Dubey M.J., Chatterjee S., Lahiri D., Lavie C.J. Psychosocial impact of COVID-19. Diabetes Metabolic Syndrome. 2020;14:779–788. doi: 10.1016/j.dsx.2020.05.035. Elsevier Ltd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O’Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A., Worthman C.M., Yardley L., Cowan K., Cope C., Hotopf M., Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. Elsevier Ltd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyer C., Ebert A., Szabo K., Platten M., Meyer-Lindenberg A., Kranaster L. Decreased utilization of mental health emergency service during the COVID-19 pandemic. Eur. Arch. Psychiatry Clin. Neurosci. 2020;1:1–3. doi: 10.1007/s00406-020-01151-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112954. Elsevier Ireland Ltd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iasevoli F., Fornaro M., D’Urso G., Galletta D., Casella C., Paternoster M., Buccelli C., De Bartolomeis A. Psychological distress in serious mental illness patients during the COVID-19 outbreak and one-month mass quarantine in Italy. Psychol. Med. 2020:1–3. doi: 10.1017/S0033291720001841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ISCIII, 2020. Informe sobre la situación de COVID-19 en España. Informe n° 27. Equipo COVID-19. RENAVE. CNE. CNM (ISCIII).
- ISCIII, 2020. Informe sobre la situación de COVID-19 en España. Informe N° 9. COVID-19 en España. CNE. SiVies. CNM (ISCIII).
- ISCIII, 2020. Informe sobre la situación de COVID-19 en España. Informe N° 10. COVID-19 en España. CNE. SiVies. CNM (ISCIII).
- World Health Organization . Vol. 12. World Health Organization; 2019. (Global Influenza Strategy 2019-2030. Weekly Epidemiology Monitor). [Google Scholar]
- Wu F., Zhao S., Yu B., Chen Y.M., Wang W., Song Z.G., Hu Y., Tao Z.W., Tian J.H., Pei Y.Y., Yuan M.L., Zhang Y.L., Dai F.H., Liu Y., Wang Q.M., Zheng J.J., Xu L., Holmes E.C., Zhang Y.Z. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579:265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu J.T., Leung K., Bushman M., Kishore N., Niehus R., de Salazar P.M., Cowling B.J., Lipsitch M., Leung G.M. Estimating clinical severity of COVID-19 from the transmission dynamics in Wuhan, China. Nat. Med. 2020;26:506–510. doi: 10.1038/s41591-020-0822-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu J.T., Leung K., Leung G.M. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet. 2020;395:689–697. doi: 10.1016/S0140-6736(20)30260-9. Lancet Publishing Group. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao H., Chen J.H., Xu Y.F. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry. 2020;7:e21. doi: 10.1016/S2215-0366(20)30090-0. Elsevier Ltd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou P., Yang X.L., Wang X.G., Hu B., Zhang L., Zhang W., Si H.R., Zhu Y., Li B., Huang C.L. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., Zhao X., Huang B., Shi W., Lu R., Niu P., Zhan F., Ma X., Wang D., Xu W., Wu G., Gao G.F., Tan W. A novel coronavirus from patients with pneumonia in China, 2019. New Engl. J. Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. Massachussetts Medical Society. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.