Highlights
-
•
Coronavirus disease 2019 (COVID-19) has emerged as a global health threat.
-
•
Number of suicidal deaths during times of COVID-19 is rising though data is limited.
-
•
Pandemics lead to several risk factors for suicidality like isolation, loneliness, economic fallout, domestic abuse, stigma and fear.
-
•
Biological vulnerabilities (family history of suicide, substance use, etc.) and psychosocial risks (migration, old age, low socio-economic class, etc.) amplify the suicidal risks of pandemics.
-
•
Stress and immune reaction to infections like COVID-19 are hypothesized as possible linking pathways to suicidal risk.
-
•
Suicide-prevention is discussed as an integral part of public health response to pandemics.
Keywords: COVID-19, Coronavirus, Suicide, Biopsychosocial, Pandemic, Suicide prevention
Abstract
The Coronavirus disease 2019 (COVID-19) has emerged as a new global health threat. By increasing the risk of isolation, fear, stigma, abuse and economic fallout, COVID-19 has led to increase in risk of psychiatric disorders, chronic trauma and stress, which eventually increase suicidality and suicidal behavior. There is limited data on association of pandemics and suicides. Cases of suicides have been rising since COVID-19 first emerged in China. The association between suicides and pandemics can possibly be explained through various models like Durkheim's theory, Joiner's interpersonal theory, social stress theory, biological theories, etc. The frontline workers, elderly, migrants, homeless, socio-economically impoverished classes as well as those with pre-existing mental disorders, substance abuse and family history of suicides are at higher risk. Suicides are preventable and need early detection, awareness and socio-culturally tailored interventions. This narrative review draws global perspectives on the association of suicidality and pandemics, the theories and risk factors related to same based on the available evidence. It also hypothesizes neuroimmunity and immune based risk factors as possible links between the psychosocial vulnerabilities and suicide during outbreaks like COVID-19. Proposed strategies of suicide-prevention, as an integral part of public health response to the pandemic are subsequently discussed.
1. Introduction
The last few months have marked an unprecedented impact on the global landscape, courtesy the Coronavirus disease 2019 (COVID-19) pandemic. Originating at Wuhan, China towards the end of last year, the infection took less than two months to evolve into a public health threat, with all nations facing unique challenges (Singhal, 2020). The effect is much beyond just medical concerns. Such large-scale outbreaks might bring about immense psychosocial and economic implications, that long outlast the infection itself. Travel has been restricted, international and national borders have been sealed, economies slashed, and jobs lost, billions isolated at their own homes in order to contain the spread of infection. Social interaction and structured schedules, the two main pillars of human civilization have been distorted leading to major psychological effects. In the absence of an effective biological cure or vaccine against the virus, social distancing and hygiene remain the main strategies to counteract it. This has made various countries enforce lockdown, thus disrupting social structures. The increased incidence of psychosocial problems, exacerbation of pre-existing psychiatric disorders and fear of infection, uncertainty, isolation, unemployment, stress and mass panic have all contributed to one of the most concerning cause of mortality: suicides (World Health Organization, 2020). The risk factors of suicidality converge along with the impact of the pandemic, to create a dual vulnerability. Suicide prevention as an integral part of mental health interventions has been prioritized by the United Nations (U.N.). Pandemics like COVID-19 will not inevitably lead to increase in suicides, but the myriad of socio-economic and psychological factors might lead to a sustained and chronic increase in risk. As the ripple effect of suicide might be related to the increasing spread of COVID-19 and subsequent effect on human lives, this article reviews the rising problem statement, highlights the possible contributing factors and discusses the strategies for suicide prevention during the present pandemic crisis.
2. COVID-19 and suicide: the problem statement
COVID-19, caused by the novel coronavirus SARS-CoV-2, has affected more than 49 million globally and 12,40,000 have succumbed to the infection (Worldometer, as on November 7th, 2020). The case fatality rate is however much lower than its earlier congeners (Severe Acute Respiratory Syndrome, SARS and Middle East Respiratory Syndrome MERS). What makes the infection so contagious and thus so unpredictable is the high human-human transmission and the prolonged viability on various inanimate surfaces (Singhal, 2020). This contributes to the panic and uncertainty related to the virus. Studies in China show the significant impact of the outbreak on mental health, with increase in health anxiety, acute stress reactions, adjustment disorders, depression, panic attacks and insomnia. Cases of severe mental disorders, obsessive compulsive disorder and anxiety disorders are suffering from relapses and increased hospitalization rates (Yao et al., 2020). Both these groups have a high suicide risk. The contributing factors are discussed later. Pandemics and suicides have some association though systematic literature is limited. Most studies have discussed suicidal risk following acute traumatic events like natural calamities. The pandemic being a chronic phenomenon with uncertain and sustained biopsychosocial effects for months to come is different from them, and thus that research cannot be translated to relevance for the current crisis (Devitt, 2020). Suicide rates had increased during the classic ‘pestilences’ of the bubonic plague (Benedictow and Benedictow, 2004). During the Spanish Flu of 1918-19, the United States reported increased deaths due to suicide (Wasserman, 1992). Fatality due to suicides increased in the elderly, women and lower socio-economic class during the SARS outbreak in China (Cheung et al., 2008). The Ebola infection increased self-harm and suicidality in Africa (Bitanihirwe, 2016). Fear, financial crisis and stigma were attributed as the main factors. Vulnerable groups like the frontline workers, elderly, homeless, migrants and daily wage workers have their own unique challenges and thus are at increased risk. A review by Torales et al. (2020) reported increased self-harm thoughts in the medical staff attending to COVID-19 centers. Similar reports have been found in people who have tested COVID-19 positive (Reger et al., 2020). Though the death rate is low, the fear of the outcome and stigma attached to it, often make people distressed, thus leading to impulsive decisions. A recent systematic review studying the impact of COVID-19 on psychosocial wellbeing in the South-Asian countries highlighted the increased sleep disturbances, generalized anxiety, substance use, depression and self-harm behavior among the frontline physicians (Banerjee et al., 2020). In the same paper, the Indian Psychiatric Society (IPS) has mentioned in its advocacy statement about the need for multi-disciplinary action to preserve mental health during the ongoing crisis; suicide prevention, management and research being an integral and important component of the same. It is also important to understand that the pandemic has affected various nations, ethnicities and groups disproportionately and hence the risk and research related to suicides need to be sensitive to these socio-cultural differences (O'Connor et al., 2020). Suicide and suicidal behavior have been conceptualized through various theories. Table 1 summarizes certain such propositions which might explain the propensity for suicidality during pandemics such as COVID-19. The authors would like to highlight that these theories are not listed as causative implications but as constructs which help to theorize the possible increased risk for suicides during large-scale infectious disease outbreaks.
Table 1.
Possible propositions of increased suicidal risk during pandemics based on the theories of suicide.
| Theory | Proposition | Factors in Pandemics |
|---|---|---|
| Durkheim Egoistic |
|
|
|
|
|
|
|
|
|
|
|
| Joiner's Interpersonal theory (Joiner et al., 2009) |
Experience of simultaneous thwarted belongingness (lack of reciprocation) and perceived burdensomeness. Acquired capability |
Hopelessness about future Change in social reciprocation Existential issues (more in elderly) |
| Social stress theory (Rubenstein, 1986) |
Perceived deficiency in social integration | Loneliness Individualism, perceived competition for survival |
|
Klonsky and May (2015) ‘Three-step theory’ |
Ideation (hopelessness and mental ‘pain’) to action (situational factors leading to suicidal behavior) | Distress and panic due to the infection to lockdown, unemployment and uncertainty (situational factors) |
| Biological theories (Decatanzaro, 1980) |
Social exclusion triggers HPA axis and inflammation | Inflammation has mutual relationships with COVID-19 pathogenesis, mental disorders and immunity |
In a given year, roughly 12 per 1,00,000 people die by suicide. For every death due to suicide, there are 15-20 reported suicide attempts. Suicide remains among the top ten causes of death globally (Ferrari et al., 2010). Rates are usually higher in men, in those with psychiatric disorders and past attempts, substance abuse and in developing countries (Vigo et al., 2016). The global burden is increasing, and the World Health Organization (WHO) has called upon for a global action to prevent suicides (Fleischmann and De Leo, 2014). On this background, the COVID-19 crisis is surely a ‘double-hit’ increasing the susceptibility. The pandemic is still spreading its global clutches and systematic studies of suicides are yet to come. However, suicidal deaths have been reported from China, India, Bangladesh, Italy and United States (Mamun and Griffiths, 2020; Thakur and Jain, 2020). Montemurro (2020) reports an increased suicidality to be common offshoot in both the general population and medical staff. Yao et al (2020) while reporting a cluster of 50 COVID-19 inpatients in a psychiatric hospital mentioned mental health disorders and infection as ‘dual-vulnerability’ to suicides. The attributing factors are stated to be increased stigma, lack of medical protective equipment and inadequate access to health care. The medical staff were interviewed in the Second Xiangya Hospital, one of the main COVID-19 centers of Wuhan and self-harm thoughts were related to loneliness, guilt, isolation, burnout and lack of sleep (Chen et al., 2020). Nation-wide surveys have detected high prevalence of depression and anxiety in China and Italy related to COVID-19 which can serve as independent risk factors for suicide (Barari et al., 2020; Qiu et al., 2020). However, the exact number of suicidal deaths are largely unknown. Anecdotal news reports from certain countries have also reported decrease in suicides during the lockdown period. Such data is yet to be scientifically corroborated (Deutsche Welle, 2020; The Guardian, 2020). Under-reporting and medico-legal issues play a role in these cases. The suicide rates in the South-East Asian countries are already high and increasing currently due to fear, misdiagnosis, social perceptions, misinformation and xenophobia (Montemurro, 2020). Added to that is the burden of homelessness and migration, which share neglect and social apathy. Multiple theoretical models have associated increase in suicides with predicted rise in unemployment and financial crisis (Kawohi and Nordt, 2020; Moser et al., 2020). These authors have mentioned a 1% global increase in suicides and used prison incarceration as a proxy measure for the effects of social distancing during the pandemic. Google Trends search patterns have also been used to estimate suicide risk (Knipe et al., 2020), though such methods have been earlier criticized due to the inherent instability and inconsistencies (Tran et al., 2017). The International COVID-19 Suicide Prevention Research Collaboration (ICSPRC) has called for a global representation for risk-assessment, preventive and management responses for suicide. The collaborative network emphasizes on ethical yet systematic research during the early phases of the pandemic, highlighting the need of sharing high-quality suicide research data, designing appropriate assessment tools and platforms, and harmonizing data collection approaches from various settings (International Association for Suicide Prevention, 2020). Niederkrotenthaler et al. (2020) in their recent paper “Suicide Research, Prevention, and COVID-19” stressed on an international response towards suicide prevention and collaborative research during the ongoing pandemic. They mentioned about the urgent need for unbiased and authenticated data from multiple sources to estimate population-based risks and possible pathways of suicide-prevention strategies.
3. Suicide in pandemics
The possible contributing risk factors for suicide during pandemics are summarized in Table 2 . Some of these have been already studied, while the others need to be explored with the progression of COVID-19.
Table 2.
Proposed risk factors and contributors for suicide during pandemics.
| Risk factors for suicide | Contributors |
|---|---|
| Loneliness, isolation and boredom | Social (along with physical) distancing Travel restriction Lack of access to technology Quarantine and confinement |
| Fear and uncertainty | Unknown nature of the infection/lack of biological cure Misinformation / ‘information pollution’ Irresponsible media reporting Competition for health care |
| Marginalization | Social stigma Prejudice Blame and xenophobia Communal sentiments |
| Psychological disorders | Health anxiety Depression Grief/bereavement Acute stress, paranoia Post-traumatic stress disorder Substance abuse |
| Relapse of psychiatric disorders | Limited access to healthcare Lack of medications and supervision (non-compliance) Lack of awareness Stress diathesis directly related to the pandemic |
| Economic fallout | Recession/financial crisis Employment and salary loss Collapse of small-scale industries Guilt Daily-wage workers Uncertainty of future |
| Domestic abuse and Intimate partner violence | Increased contact time between partners (entrapment with abusive partners) Substance abuse Sexism and prejudice against the opposite gender Responsibility for children |
| Increased access | Pesticides, medicines and firearms Lack of administrative vigilance |
| Special vulnerabilities | Adolescent, Elderly (more prone to isolation, loneliness, depression and increased baseline suicidal risk) Frontline health workers (health workers, police, essential service providers, volunteers, delivery personnel, etc.) Migrants and homeless Poverty and lower socio-economic status |
4. Populations at increased risk
4.1. Frontline workers
A significant amount of research has been ongoing in the mental health care of frontline health workers. They are being the backbone of a country's battle against COVID-19 are equally susceptible to its physical and psychosocial risks. Apart from staying in constant fear about the threat of infection, they are guilty about transmitting it to their loved ones. The increased work pressure, witnessing the morbidity, chronic stress and need for self-isolation can contribute to depression, absenteeism, burnout, frustration and eventually suicidality. Studies of psychological wellbeing among medical staff have showed increased hopelessness, decreased self-esteem, guilt and self-blame, and insomnia, all of which can be risk factors for suicide (Chen et al., 2020). Lack of adequate personal protective equipment, lack of flexibility in shifts due to decreased health care resources and inadequate insurance facilities can be additional burden in developing countries (Heymann and Shindo, 2020). Moreover, stigma and discrimination have been prevalent against frontline workers with threats of eviction from their residences, difficulties in cremation and shrinkage of social circle, as they are at increased risk of exposure (Logie and Turan, 2020). This further leads to isolation and social disconnectedness.
4.2. Elderly
Age and ageism are also special concerns at times of COVID-19. Apart from being the single most important risk factor for severity and mortality in the infection, age also predisposes an individual to the psychosocial adversities. Quarantine and isolation can cause profound loneliness, depression and suicidality in the elderly (Armitage and Nellums, 2020). Frailty, cognitive and sensory impairment further contribute to the risk while neglect, abuse, overcrowding and noncompliance to precautionary measures are added troubles in those institutionalized. Autonomy, self-dignity and mobility, the important indicators of their wellbeing can be compromised during such pandemics, when they are not involved in the decision making (Banerjee, 2020). Many of them are stranded alone, with inadequacies of domestic help and basic living amenities due to the lockdown, which makes them isolated and increases self-neglect. Suicidality is often under-reported and more in the seniors and late-life depression can be polymorphic, which leads to higher number of suicidal deaths in older adults (Lindesay, 1991). Existential issues might arise, when ‘suicide’ is considered to shorten the misconstrued fear of infection and over-estimated threat of mortality during the pandemic.
4.3. Homeless and migrants
The world shelters around 1.5 billion homeless, most of them being in the South Asian and African countries (Ortiz-Ospina and Roser, 2017). Besides having physical risks of infection, the principles of ‘social distancing’ are but ironical in their overcrowded and impoverished shelters. Administrative unaccountability and societal apathy lead to poor testing rates and improper awareness in them. Mental disorders and substance abuse are common accompaniments, which together with the perceived vulnerability of the infection increases the risk of suicides. Post lockdown, especially in countries like India, thousands of migrants have been stranded on the streets and stations with no food or money for survival. They often welcome death, suffering from hunger and unable to survive far from homes, when living conditions are a greater threat than the virus itself (Banerjee and Bhattacharya, 2020).
4.4. Victims of abuse and violence
Entrapment of various families during the COVID-19 induced lockdown has led to unprecedented circumstances, when couples cohabit together for extended periods like never before. In families with pre-existing marital discord, interpersonal violence and substance abuse, the problems have exacerbated leading to marked increase in domestic abuse and intimate partner violence during the present times. The United Kingdom Domestic Abuse helpline has been registering an increase in number of complaints, some of whom have expressed death-wishes (World Health Organization, 2020). The national helplines that we are operating in a tertiary mental health care institute in India, receive consistent calls of domestic violence associated with suicidality as an easy escape. Normalization by families, sexism, objectification of women and aggression are known to increase during disasters. Under-reporting, fear of legal hassles, acceptance and underlying untreated depression can lead to suicides, which otherwise could have been prevented.
4.5. Stigmatized groups
Though data is sparse for adolescents, sexual and racial minorities, theoretical risk of depression and suicidality are high among them. Social disconnectedness, unhealthy use of technology, substance abuse and isolation can be high in adolescents as interaction and peer-support form important aspects of their identity. Virtual connections can never be a total replacement of human-human interactions and psychological distress post lockdown has been shown to be complex and chronic for young children and adolescents. Racial and sexual ‘othering’ are common in pandemics and have been sporadically reported during COVID-19. From terming the disease as ‘Kung-flu’ to discriminating against people of mongoloid origin, reports of suicide have been increasing in response to prejudice and xenophobia, with relation to the infection (Coates, 2020). Lack of abused substance, withdrawal symptoms and difficulties in health-care access have shown to increase the suicidal risk in addiction disorders.
4.6. Financial crisis
Lastly, COVID-19 has led to restrictive implementations that had significant impact on the global economy. The unemployment rate has risen sharply, and 2.5 million people have lost their jobs in the United States alone (Buera et al., 2020). The most developed economies have been struck hard, which can lead to a fair assumption as how other countries might fare. This effect is rippling and can have long-term consequences. Many small-scale industries especially those involved in travel, tourism, entertainment, etc. have closed down in the lockdown period, with uncertainty shadowing their futures. In a study on effect of unemployment on suicide based on global data of 63 countries, suicide risk was elevated by 20-30 percent during the 2000-2011 period. The peak was during the 2008 ‘Great Recession’. Data from this period showed that increase in suicides preceded the actual unemployment rate (Nordt et al., 2015). Considering that the International Labor Organization (ILO) predicted a loss of around 25 million jobs due to the COVID-19 pandemic period alone, the aftermath can have prolonged challenges (International Labour Organization, 2020). Based on a model proposed by Kawohl and Nordt (2020) to describe non-linear connection between unemployment and suicide, the worldwide unemployment rate might lead to an increase of suicides by around 6000-9570 per year. The downsized economy coupled with vulnerabilities in society, can lead to a surge in suicidal mortality for many more months to come. The preparedness of health-care facilities at all levels might be vital in its understanding and prevention.
5. Immunity, suicide and COVID19: a linking pathway?
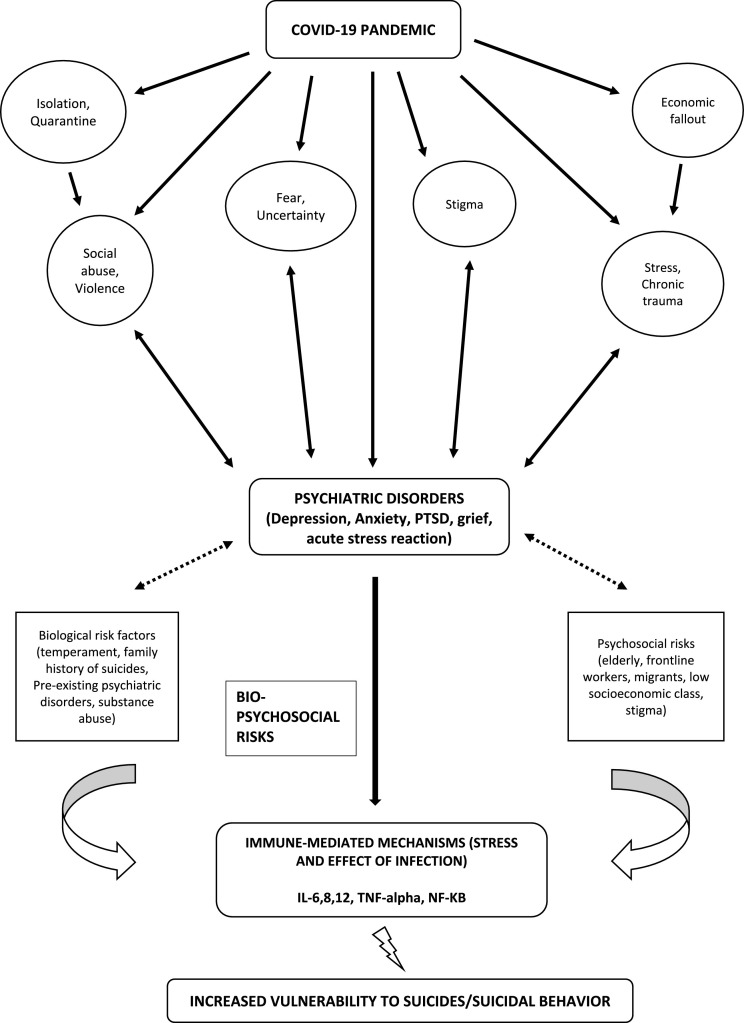
The pneumonia caused by COVID-19 has already been well-known all over the world. The direct neuropsychiatric effects of the virus have been discussed in a recent systematic review (Rogers, 2020). The increased penetration of blood-brain barrier, delirium and acute behavioral effects have been reported in the acute stage. Whereas the authors caution about the possibility of depression, anxiety, fatigue, post-traumatic stress and adjustment disorders in the long run, each of which can contribute to the suicidal risk. Besides, the clinical assessment of COVID-19 infections have indicated mild to severe cytokine storms in symptomtic patients and this has accounted for the death in many such patients. Consequently the focus had also been on the treatment of cytokine storm for treating severe cases. It was found that Interleukin-6 (IL-6) plays a significant role in cytokine release syndrome (CRS) and hypothesized that if the signal transduction pathway of IL-6 is blocked, it helps to develop a new method for the treatment of severe cases. Research has been looking at Tocilizumab, potential blocker of IL-6R, that might effectively block IL-6 signal transduction pathway and potentially help patients to treat with severe manifestations of COVID-19. Further it was reported that IL-6 levels were elevated in the cerebrospinal fluid of suicide attempters and related to symptom severity. This adds a possible new dimension in explaining suicidal symptoms in COVID 19 infected patients associated with IL-6 effects (Zhang et al., 2020). Hence with all the psychosocial and biological risk factors, stress and immune-mediated diathesis for COVID-19 can be hypothesized as a possible linking pathway for increase in suicidality during this pandemic ( Fig. 1 ). Research correlating severity, neuroimmunity blood markers and suicidal risk will help understand the pathogenic effects of COVID-19 and associated comorbidity like suicidal behavior (Lindqvist et al., 2009).
Fig. 1.
Coronavirus disease 2019 (COVID-19) has led to various unique challenges (isolation, loneliness, stigma, fear, uncertainty, economic fallout, etc.), which together with biological risk factors (temperament, family history of suicide, pre-existing mental disorders and substance abuse) and psychosocial vulnerabilities (elderly, migration, homeless, low socioeconomic classes) increase the risk of primary psychiatric symptoms. This in turn combined with the interaction between stress and immunity related to infection can serve as a possible link (increase in inflammatory mediators like IL-6,8,12, Tumor Necrosis Factor-alpha, Toll-like Receptors, NF-KB, etc.) to increase suicidality and suicidal behavior.
There have been established relations between the immune system and suicides (Pandey et al., 2019). One such example is the abnormal change in Toll-like receptors (TLRs) having a significant role in the neuropathogeneis of depression and suicide. The TLRs interact with the pathogen-associated molecular patterns (PAMP), damage-associated molecular patterns (DAMP) and induce cytokines through the activation nuclear factor kappa beta (NF-kB). Earlier studies showed that the protein and mRNA expression of TLR3 and TLR4 in the prefrontal cortex (PFC) of depressed suicidal (DS) subjects were increased when compared to normal control (NC) subjects. These findings provided a valuable insight that very specific TLRs were altered in DS, some of which might be targeted for suicidal treatment in translational psychiatry (Pandey et al., 2019). TLRs have already been studied in the pathogenesis of COVID-19 and extra-pulmonary manifestations, which might again provide a possible biological link for suicide risk.
The frequently asked question is how does SARS-CoV-2 alter the immune system? It is already known that CD4+ and CD8+ have significant antiviral properties. The CD4 + T cells favor the elevation of viral-specific antibodies through T cell-dependent B cells activation. But CD8+ T cells being cytotoxic kill virus infected cells. Actually, CD8+ T cells significantly increase in the pulmonary interstitium in SARS-CoV-2 infection killing coronaviruses in infected cells. Further, the cytokines like IL-17 are involved in the recruitment of monocytes and neutrophils to the infection site. Studies have clearly shown that T cell response relevance to S, M and N proteins is assumed to be persistent and this pathway may be a target for vaccines for SARS-CoV-2, which is currently under research. Also, it was found that the ACE2 protein fused with human immuno-globulin G Fc domain (ACE2-Fc) of SARS-CoV-2 patients may have involved in the traditional neutralizing antibody. Hence there is a need to focus on clinical trials to understand the benefits and side effects of ACE2-Fc treatment. These studies are crucial to understand the complex immune responses to COVID-19 and its effects on the central nervous system. The alterations of psychoneuroimmunity seen in brain and other organs tend to cause multiple other effects of COVID-19 which leads to the unanswered questions on immunity, brain and mental health issues in relevance to this infection (Vellingiri et al., 2020). These might directly or indirectly increase suicide risk, as inflammation and immunity dysregulation have been linked both to the neuropathogenesis of depression and suicides.
6. Suicide prevention during COVID-19: special considerations
The basic premise of any management strategy is that suicide is preventable. A qualitative study of psychological autopsies based on interviews conducted with relatives of 66 suicide victims showed that more than half of them had availed some sort of professional help within past one month of the attempt (Owens et al., 2005). Those who did not were either ‘help-resisters’ or the families were not aware of the suicidal signs, that they acknowledged later on retrospect. The various guidelines like WHO, Centre for Disease Control and Prevention (CDC), The U.S. National Strategy for Suicide prevention, etc. mention certain generic principles. They include strengthening economic supports, enabling access and delivery of suicide care, creating protective environments, promoting connectedness, training public with coping and problem-solving skills, early identification of risk, gatekeeper training at community level and futuristic harm-prevention (Bernert et al., 2014). Besides, prompt treatment of psychiatric disorders, increasing mental health promotion and awareness as well as reducing social risks like poverty are other broader strategies for suicide prevention. While all of these measures are equally important and applicable even to the pandemic situation, certain specific risks during COVID-19 crisis might need special measures at different levels. Few such possible ways are proposed in Table 3 . In the absence of specific evidence on suicide risks during pandemic, these strategies are merely conceptualizations that can be used in interventions and research. Besides, administrative changes in the pandemic acts of countries might need to include suicide prevention programs, crisis management and mental health integration in public health infrastructure.
Table 3.
Proposed suicide prevention strategies during pandemics.
| Problem situation | Interventions |
|---|---|
| Mental disorders | Tele-psychiatry & tele-psychotherapy Active digital follow-up Online medication refill Ensure availability of psychotropics at district levels Psychoeducation of caregivers |
| Psychological distress due to pandemics | Encourage professional help Staying away from the social media Online counseling |
| Suicidal crisis (acute) | Clear assessment and intervention guidelines Online-based crisis interventions Digital resources for coping Flexible crisis helplines (24/7) Volunteer workforce for outreach Training of the local authorities for emergency response |
| Substance abuse | Safe drinking and monitoring messages |
| Domestic abuse | Integrate mental health helplines with women, child and elder services Hassle-free reporting Ensuring safe shelter |
| Isolation and quarantine | Digital connectedness Community support Ensure living amenities Weekly sessions for mental health support |
| Misinformation | Mental health education through social media: IEC activities Community awareness programs (street plays, infographics on print/digital media) Government messages and policies Tele-training of primary health care providers to debunk fake news Media-health sector collaboration Advocating authentic information sources (WHO, CDC) |
| Economic crisis | Financial packages by Government Ensure food, housing, and emergency funds for the unemployed and homeless Ensure safety, awareness and transportation to homes for migrants Long term labor sustenance policies |
| Vulnerable population | For frontline workers (mental health care sessions, peer support, flexible shifts, ensure safety in isolation, adequate rest, debriefing, medical protective equipment) For the elderly and those stranded alone (delivery of food, water, medicines and other essentials) |
IEC Information, Education and Communication, WHO World Health Organization, CDC Center for Disease Prevention and Control
People in suicidal crisis, require enhanced attention and surveillance. Stigma, fear of being discriminated, legal hassles and avoidance of ‘health-care setups’ due to pandemic fear can be potent barriers to health care access. Early identification of the at-risk population, especially those who are quarantined, are suffering from mental disorders, are working on the frontline, are affected with COVID-19 or relatives of the affected, might be helpful. Online mental health services in China used risk detection, community training and weekly sessions to deal with suicidal individuals in isolation (Liu et al., 2020). Community-based programs in Iran, France and the United Kingdom have included training health-care providers dealing with COVID-19 cases in suicide prevention (Fiorillo and Gorwood, 2020; Zandifar and Badrfam, 2020). Banerjee and Nair (2020) have proposed a community-based toolkit for the current pandemic, modeled on the Zika outbreak, to detect mental health issues at grass-root levels and train multi-purpose health workers and ASHA workers in suicide risk detection. Few ways that suicide prevention can be improvised on during pandemics are as follows:
-
1
Increase in mental health helplines, liaising with the COVID-19 information services and integration with the health centers/ambulance facilities for crisis interventions.
-
2
Tele-consultation (digital/call) for those facing psychological distress, active follow-up of registered patients from the various hospitals. Tele-conferences between primary and tertiary care centers for appropriate for mental health services. Digital privacy need to be ensured.
-
3
Gatekeeper training for community and primary care centers (Red flag warnings: excessive fear due to the pandemic [catastrophic thinking], death wishes, expressions of hopelessness, helplessness, panic attacks, grief, difficulty in coping for families of those affected, history of suicide, substance abuse, low social support, staying alone, low self-worth). Behavioral and verbal cue-based assessment of risk are useful.
-
4
Use of media for Information-Education-Communication (IEC) related to suicide prevention: making evidence-based online sources and socio-culturally appropriate infographics in multiple languages.
-
5
Training the lay counselors in brief and solution focused interventions for crisis management. Digital training resources can be used.
-
6
Public health responses and detection of abuse and domestic violence: early sensitization and rapid response by the police/local authorities. Safe drinking messages can be propagated.
-
7
Sale restrictions on pesticides, medications and firearms, especially during the lockdown.
-
8
Community support for those living alone, in isolation, for the elderly, bereaved individuals. The lockdown can aid foster bonds and relationships.
-
9
Ensuring essential services (food, water, medication) delivery is hassle-free for the elderly, disabled and those quarantined.
-
10
Media and health services collaboration to debunk misinformation and bridge the knowledge-attitude-practice (KAP) gap related to COVID-19 and suicide. Suicide is a sensitive topic and the its portrayal in popular media can potentially influence reactions to it. Responsible reporting of suicide is necessary for mitigating stigma, falsification and prejudice towards this important aspect of mental health. Public health agencies like the WHO has clear guidelines for suicide-reporting by the media, especially in sensitive situations (WHO, 2017). Few facets of the same are highlighted in Table 4 . These are however more commonly overlooked than implemented.
Table 4.
Responsible reporting of suicides by media.
| Preferred ways of reporting | Practices to be avoided |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Modified from World Health Organization (2017). Preventing suicide: A resource for media professionals, update.
7. Conclusion: the way forward
Suicide itself is considered to be a pandemic. A large-scale outbreak like COVID-19 can easily overwhelm the available public health resources, needing more workforce on the ground. This review glances at various possible hypotheses linking pandemics, suicides and suicidal behavior and propositions to mitigate the risk, based on the limited evidence available. These conceptualizations are definitely not ‘causal and definitive’ and can be critiqued and debated. However, they might form the basis of epidemiological and interventional research for the current and futuristic crises. Both for the frontline workers and the general public, these are unprecedented times that no amount of preparedness can account for. As mentioned before, suicide prevention by early detection of risks is the main strategy. This is a collective responsibility irrespective of socio-economic status, occupation or class. It is but natural to be stressed during a pandemic, however the differentiation between the ‘acceptable limits’ of panic and ‘over the edge’ psychiatric symptoms that need professional help is vital. All sectors of society need awareness of the same. Suicide prevention responses need to be comprehensive and they need to be backed up by increased surveillance of COVID-19 specific risk factors (Gunnell et al., 2020). Data and systematic research on self-harm behaviors and suicidality can inform further protocols and policies.
As the epidemic is still in its early stages, both cross-sectional and longitudinal community-based studies might help estimate the population level risk, that can help preparedness for such futuristic crises. Rapid dissemination of data and adequate surveillance of national mortality, surveys and published literature will help researchers and policy makers alike. The suggested areas of exploration are the mental health consequences, economic offshoots, mortality burden and grief, the healthcare crisis response as well as workplace and educational effects of the pandemic (International Association for Suicide Prevention, 2020). As mentioned before, the ICSPRC is collaborating with the International Association for Suicide Prevention (IASP) and WHO to formulate a strategic and evidence-based intervention protocol for reducing suicidal deaths during COVID-19. The effectiveness and implementation of these strategies will depend on filling the gaps in understanding of suicides and suicidal behavior during this outbreak (Niederkrotenthaler et al., 2020). Lived experiences of the vulnerable population, mental health care providers and the patients affected with COVID-19 in the months that follow will help in risk estimation and resource allocation. At each level, these approaches need adequate funding and appropriate coordination. Every nation's public health infrastructure, socio-cultural milieu and demographic parameters are unique to deal with the suicide risk. However, it is expected that global collaboration through public health agencies like the WHO or CDC can shape further insights into suicide prevention during such pandemics (Thakur and Jain, 2020). Technology can be harnessed in these times of ‘social distancing’ for staying connected and also providing adequate mental healthcare. Resource-poor settings need more intense surveillance and care. Stigma and misinformation are important contributors to mental distress and need to be mitigated (World Health Organization, 2020). The world stands at a difficult juncture. Mental health implications of this ongoing pandemic might peak much beyond the infection, and suicide might add to the fatality burden. However, the resilience of humankind throughout history during any disaster has been remarkable. Positivism and hope, two salient markers of coping often arise out of collectivism, optimism and mutual support. Global strategies, collaborative research and collective responsibility might hopefully enhance the efforts against the ‘dual pandemic’ of COVID-19 and suicide.
CRediT authorship contribution statement
Debanjan Banerjee: Conceptualization, Visualization, Validation, Writing - original draft, Writing - review & editing. Jagannatha Rao Kosagisharaf: Conceptualization, Validation, Writing - original draft, Writing - review & editing. T.S. Sathyanarayana Rao: Conceptualization, Validation, Writing - review & editing.
Declaration of Competing Interest
None.
Acknowledgement
Nil.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.psychres.2020.113577.
Appendix. Supplementary materials
References
- Armitage, R. and Nellums, L.B., 2020. COVID-19 and the consequences of isolating the elderly. Lancet Public Health. [DOI] [PMC free article] [PubMed]
- Banerjee D., Vaishnav M., Rao T.S., Raju M.S.V.K., Dalal P.K., Javed A., Saha G., Mishra K.K., Kumar V., Jagiwala M.P. Impact of the COVID-19 pandemic on psychosocial health and well-being in South-Asian (World Psychiatric Association zone 16) countries: A systematic and advocacy review from the Indian Psychiatric Society. Indian J. Psychiatry. 2020;62(9):343. doi: 10.4103/psychiatry.IndianJPsychiatry_1002_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerjee, D. and Bhattacharya, P., 2020. The hidden vulnerability of homelessness in the COVID-19 pandemic: perspectives from India. [DOI] [PMC free article] [PubMed]
- Banerjee D., Nair V.S. Handling the COVID-19 pandemic: proposing a community based toolkit for psycho-social management and preparedness. Asian J. Psychiatry. 2020 doi: 10.1016/j.ajp.2020.102152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerjee D. ‘Age and Ageism in COVID-19’: Elderly Mental Health-care Vulnerabilities and Needs. Asian J. Psychiatry. 2020 doi: 10.1016/j.ajp.2020.102154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barari S., Caria S., Davola A., Falco P., Fetzer T., Fiorin S., Hensel L., Ivchenko A., Jachimowicz J., King G., Kraft-Todd G. Evaluating COVID-19 public health messaging in Italy: self-reported compliance and growing mental health concerns. medRxiv. 2020 [Google Scholar]
- Benedictow O.J., Benedictow O.L. Boydell & Brewer; 2004. The Black Death, 1346-1353: The Complete History. [Google Scholar]
- Bernert R.A., Hom M.A., Roberts L.W. A review of multidisciplinary clinical practice guidelines in suicide prevention: toward an emerging standard in suicide risk assessment and management, training and practice. Acad. Psychiatry. 2014;38(5):585–592. doi: 10.1007/s40596-014-0180-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bitanihirwe B.K.Y. Monitoring and managing mental health in the wake of Ebola. Ann. dell'Istituto Super. Sanita. 2016;52(3):320–322. doi: 10.4415/ANN_16_03_02. [DOI] [PubMed] [Google Scholar]
- Buera F., Fattal-Jaef R., Neumeyer A., Shin Y. Unpublished Manuscript. Available at the World Bank Development Policy and COVID-19—eSeminar Series. 2020. The economic ripple effects of COVID-19. [Google Scholar]
- Chen Q., Liang M., Li Y., Guo J., Fei D., Wang L., He L., Sheng C., Cai Y., Li X., Wang J. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7(4):e15–e16. doi: 10.1016/S2215-0366(20)30078-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheung Y.T., Chau P.H., Yip P.S. A revisit on older adults suicides and Severe Acute Respiratory Syndrome (SARS) epidemic in Hong Kong. Int. J. Geriatr. Psychiatry. 2008;23(12):1231–1238. doi: 10.1002/gps.2056. [DOI] [PubMed] [Google Scholar]
- Coates M. Covid-19 and the rise of racism. BMJ. 2020;369 doi: 10.1136/bmj.m1384. [DOI] [PubMed] [Google Scholar]
- DeCatanzaro D. Human suicide: A biological perspective. Behav. Brain Sci. 1980;3(2):265–272. [Google Scholar]
- Deutsche Welle. 2020, June 3. Is social distancing during coronavirus causing more suicides?Retrieved from https://www.dw.com/en/is-social-distancing-during-coronavirus-causing-more-suicides/a-53584282 (accessed on August 10 2020).
- Devitt P. Can we expect an increased suicide rate due to Covid-19? Irish J. Psychol. Med. 2020:1–15. doi: 10.1017/ipm.2020.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiorillo A., Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur. Psychiatry. 2020;63(1) doi: 10.1192/j.eurpsy.2020.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleischmann, A. and De Leo, D., 2014. The World Health Organization's report on suicide: a fundamental step in worldwide suicide prevention. [DOI] [PubMed]
- Gunnell D., Appleby L., Arensman E., Hawton K., John A., Kapur N., Khan M., O'Connor R.C., Pirkis J., Caine E.D., Chan L.F. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30171-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heymann D.L., Shindo N. COVID-19: what is next for public health? Lancet North Am. Ed. 2020;395(10224):542–545. doi: 10.1016/S0140-6736(20)30374-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Association for Suicide Prevention. 2020. International COVID-19 suicide prevention research collaboration. https://www.iasp.info/COVID-19_suicide_research.php (accessed on August 10 2020).
- International Labour Organisation (ILO), 2020. COVID-19 and the world of work: country policy responses.
- Joiner T.E., Jr., Van Orden K.A., Witte T.K., Rudd M.D. American Psychological Association; 2009. The Interpersonal Theory Of Suicide: Guidance For Working With Suicidal Clients. [Google Scholar]
- Kawohl W., Nordt C. COVID-19, unemployment, and suicide. Lancet Psychiatry. 2020;7(5):389–390. doi: 10.1016/S2215-0366(20)30141-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klonsky E.D., May A.M. The three-step theory (3ST): A new theory of suicide rooted in the “ideation-to-action” framework. Int. J. Cognit. Therapy. 2015;8(2):114–129. [Google Scholar]
- Knipe D., Evans H., Marchant A., Gunnell D., John A. Mapping population mental health concerns related to COVID-19 and the consequences of physical distancing: a Google trends analysis. Wellcome Open Res. 2020;5(82):82. doi: 10.12688/wellcomeopenres.15870.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindesay J. Suicide in the elderly. Int. J. Geriat. Psychiatry. 1991 [Google Scholar]
- Lindqvist D., Janelidze S., Hagell P., Erhardt S., Samuelsson M., Minthon L., Hansson O., Björkqvist M., Träskman-Bendz L., Brundin L. Interleukin-6 is elevated in the cerebrospinal fluid of suicide attempters and related to symptom severity. Biol. Psychiatry. 2009;66(3):287–292. doi: 10.1016/j.biopsych.2009.01.030. [DOI] [PubMed] [Google Scholar]
- Liu S., Yang L., Zhang C., Xiang Y.T., Liu Z., Hu S., Zhang B. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7(4):e17–e18. doi: 10.1016/S2215-0366(20)30077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logie C.H., Turan J.M. How do we balance tensions between COVID-19 public health responses and stigma mitigation? Learning from HIV research. AIDS Behav. 2020:1–4. doi: 10.1007/s10461-020-02856-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamun M.A., Griffiths M.D. First COVID-19 suicide case in Bangladesh due to fear of COVID-19 and xenophobia: Possible suicide prevention strategies. Asian J. Psychiatry. 2020;51 doi: 10.1016/j.ajp.2020.102073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montemurro N. The emotional impact of COVID-19: From medical staff to common people. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moser D.A., Glaus J., Frangou S., Schechter D.S. Years of life lost due to the psychosocial consequences of COVID19 mitigation strategies based on Swiss data. Eur. Psychiatry. 2020:1–14. doi: 10.1192/j.eurpsy.2020.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niederkrotenthaler, T., Gunnell, D., Arensman, E., Pirkis, J., Appleby, L., Hawton, K., John, A., Kapur, N., Khan, M., O'Connor, R.C. and Platt, S., 2020. Suicide research, prevention, and COVID-19. [DOI] [PMC free article] [PubMed]
- Nordt C., Warnke I., Seifritz E., Kawohl W. Modelling suicide and unemployment: a longitudinal analysis covering 63 countries, 2000–11. Lancet Psychiatry. 2015;2(3):239–245. doi: 10.1016/S2215-0366(14)00118-7. [DOI] [PubMed] [Google Scholar]
- O'Connor R.C., Hotopf M., Worthman C.M., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Silver R.C., Ford T. Multidisciplinary research priorities for the COVID-19 pandemic–Authors' reply. Lancet Psychiatry. 2020;7(7):e44–e45. doi: 10.1016/S2215-0366(20)30247-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortiz-Ospina E., Roser M. Homelessness. Our World Data. 2017 [Google Scholar]
- Owens C., Lambert H., Donovan J., Lloyd K.R. A qualitative study of help seeking and primary care consultation prior to suicide. Br. J. Gen. Pract. 2005;55(516):503–509. [PMC free article] [PubMed] [Google Scholar]
- Pandey G.N., Rizavi H.S., Bhaumik R., Ren X. Innate immunity in the postmortem brain of depressed and suicide subjects: Role of Toll-like receptors. Brain Behav. Immun. 2019;75:101–111. doi: 10.1016/j.bbi.2018.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. General Psychiatry. 2020;33(2) doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reger M.A., Stanley I.H., Joiner T.E. Suicide mortality and coronavirus disease 2019—a perfect storm? JAMA Psychiatry. 2020 doi: 10.1001/jamapsychiatry.2020.1060. [DOI] [PubMed] [Google Scholar]
- Rubinstein D.H. A stress-diathesis theory of suicide. Suicide Life Threat. Behav. 1986;16(2):182. doi: 10.1111/j.1943-278x.1986.tb00351.x. [DOI] [PubMed] [Google Scholar]
- Singhal T. A review of coronavirus disease-2019 (COVID-19) Indian J. Pediat. 2020:1–6. doi: 10.1007/s12098-020-03263-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S.D. Macmillan International Higher Education; 1982. Durkheim and the Study of Suicide. [Google Scholar]
- Thakur V., Jain A. COVID 2019-suicides: a global psychological pandemic. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.04.062. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- The Guardian. 2020, May 14. Japan suicides decline as COVID-19 lockdown causes shift in stress factors. Retrieved from https://www.theguardian.com/world/2020/may/14/japan-suicides-fall-sharply-as-COVID-19-lockdown-causes-shift-in-stress-factors (accessed on August 10 2020).
- Torales J., O'Higgins M., Castaldelli-Maia J.M., Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatry. 2020 doi: 10.1177/0020764020915212. [DOI] [PubMed] [Google Scholar]
- Tran U.S., Andel R., Niederkrotenthaler T., Till B., Ajdacic-Gross V., Voracek M. Low validity of Google trends for behavioral forecasting of national suicide rates. PLoS One. 2017;12(8) doi: 10.1371/journal.pone.0183149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vellingiri B., Jayaramayya K., Iyer M., Narayanasamy A., Govindasamy V., Giridharan B., Ganesan S., Venugopal A., Venkatesan D., Ganesan H., Rajagopalan K. COVID-19: a promising cure for the global panic. Sci. Total Environ. 2020 doi: 10.1016/j.scitotenv.2020.138277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vigo D., Thornicroft G., Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry. 2016;3(2):171–178. doi: 10.1016/S2215-0366(15)00505-2. [DOI] [PubMed] [Google Scholar]
- Wasserman I.M. The impact of epidemic, war, prohibition and media on suicide: United States, 1910–1920. Suicide Life‐Threat. Behav. 1992;22(2):240–254. [PubMed] [Google Scholar]
- World Health Organization . World Health Organization; Geneva: 2017. Preventing Suicide: A Resource For Media Professionals, Update 2017. Jan 12. [Google Scholar]
- World Health Organization . World Health Organization; 2020. COVID-19 and Violence Against Women: What The Health Sector/System Can Do, 7 April 2020 (No. WHO/SRH/20.04) [Google Scholar]
- Worldometer. https://www.worldometers.info/coronavirus/ [last accessed on November 7th, 2020 ].
- Yao H., Chen J.H., Xu Y.F. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry. 2020;7(4):e21. doi: 10.1016/S2215-0366(20)30090-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zandifar A., Badrfam R. Iranian mental health during the COVID-19 epidemic. Asian J. Psychiatry. 2020;51 doi: 10.1016/j.ajp.2020.101990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang C., Wu Z., Li J.W., Zhao H., Wang G.Q. The cytokine release syndrome (CRS) of severe COVID-19 and Interleukin-6 receptor (IL-6R) antagonist Tocilizumab may be the key to reduce the mortality. Int. J. Antimicrob. Agents. 2020 doi: 10.1016/j.ijantimicag.2020.105954. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.