Abstract
Background
Recent advances in treatment for stroke give new possibilities for optimizing outcomes. To deliver these prehospital care needs to become more efficient.
Aim
To develop a framework to support improved delivery of prehospital care. The recommendations are aimed at clinicians involved in prehospital and emergency health systems who will often not be stroke specialists but need clear guidance as to how to develop and deliver safe and effective care for acute stroke patients.
Methods
Building on the successful implementation program from the Global Resuscitation Alliance and the Resuscitation Academy, the Utstein methodology was used to define a generic chain of survival for Emergency Stroke Care by assembling international expertise in Stroke and Emergency Medical Services (EMS). Ten programs were identified for Acute Stroke Care to improve survival and outcomes, with recommendations for implementation of best practice.
Conclusions
Efficient prehospital systems for acute stroke will be improved through public awareness, optimized prehospital triage and timely diagnostics, and quick and equitable access to acute treatments. Documentation, use of metrics and transparency will help to build a culture of excellence and accountability.
Keywords: Stroke, emergency medical services, prehospital care
Background
Stroke is a major cause of death and disability worldwide with an estimated 15.2 million strokes causing 7 million deaths per year globally.1 Over half of stroke survivors will have some degree of disability and for most individuals and their families, it is a life-changing experience. Changes in demography will lead to a predicted 45% increase in stroke incidence in Europe over the next 20 years with similar increases predicted in other parts of the world.2 Rapid recognition of stroke symptoms and delivery of evidence-based acute care, including thrombolytics and endovascular thrombectomy (EVT), blood pressure control for primary intracerebral hemorrhage and stroke unit management have all been shown to significantly improve outcomes.3,4 These treatments are time dependent and require rapid access to definitive care in hospital.
Many people consider stroke as an untreatable disease. The public lacks awareness of the signs and symptoms of stroke and the need for urgent medical attention. Less than 50% of individuals with acute stroke recognize the nature of their own symptoms.5 In some countries, individuals with stroke are more likely to call a general practitioner rather than the Emergency Medical Services (EMS) and in many low- and middle-income countries, EMS systems are scarce or non-existent.6 Compounded by lack of knowledge, inefficient and inadequate acute care pathways and facilities, seen in both high and low resource countries, many people face death and disability after stroke that is potentially preventable.
Recent advances in acute ischemic stroke care have expanded the pool of patients who may benefit from acute therapy, demonstrating benefit of EVT up to 24 h after symptom onset in selected patients,7 as well as benefit for acute therapy in patients without a witnessed time of onset.8 However, the best outcomes are associated with the shortest treatment times.9,10 Optimizing the organization of stroke systems of care is essential.
This article presents a “Chain of Survival” for emergency stroke care and sets out the recommendations for health systems to strive for worldwide. While none of the individual components will be unknown to professionals involved in the area, we believe unifying them into a single program, calling for global action and asking EMS to work in a unified way with hospitals will be of great benefit for health systems trying to improve prehospital and emergency care. Such a system has proved hugely beneficial in cardiac arrest and acute myocardial infarction.11 This study in South Korea shows a doubling of the percentage survival rate and survival with good neurological function after implementation of the Utstein recommendations. While some of the components require well-resourced services, many are applicable to low- and middle-income countries and can be delivered by improving the organization of existing services and close collaboration between stroke specialists in hospitals and the EMS composed in most cases of non-specialists. These interventions in emergency stroke care management will reduce stroke mortality and disability.
Methodology
The first Utstein Meeting was held in 1990 at Utstein Abbey, Stavanger, Norway. Researchers and experts produced a consensus recommendation on how to report cardiac arrest survival data.12 This process of defining the essential elements of complex medical challenges within emergency care came to be known as the Utstein methodology or merely Utstein. The Utstein terminology for cardiac arrest is the international standard for reporting data and science.13,14 The method of reporting cardiac arrest has been updated and remains the universal standard. The methodology has since been used for numerous recommendations primarily for cardiac arrest but also within various other emergency areas.
In 2015, an Utstein meeting resulted in a call for establishing a Global Resuscitation Alliance (GRA) in order to best implement successful strategies in managing cardiac arrest and to disseminate best practice.15 This aimed to update and expand the reach and utilization of the concept of 10 programs to improve survival from out-of-hospital cardiac arrest including the Resuscitation Academy concept of “measure and improve”, developed in EMS Seattle and King County USA.16 This concept was successfully disseminated worldwide and is acknowledged as an implementation plan for best practice in cardiac arrest management for EMS.
The purpose of this Utstein article on emergency stroke care is to employ the Utstein methodology to transfer the experience from the area of out-of-hospital cardiac arrest into the field of emergency stroke care. It seeks to adapt concept recommendations from the GRA to produce 10 programs to improve outcome and survival for stroke patients. It aims to target clinicians delivering stroke care particularly in the prehospital stage who may not be experts in stroke in all countries rich and poor, urban and rural to provide a framework which can be used to progressively improve care and consequently outcomes.
An international group (supplementary Appendix A) representing expertise from EMS, emergency medicine neurology, stroke and quality improvement, including representatives from organizations and foundations working with stroke care, was brought together to formulate recommendations in 10 predefined areas of the acute stroke systems of care. The meeting took place on 5–6 June 2018 at the Utstein Abbey in Norway. Preparations before the meeting included identifying and reviewing guidelines, consensus articles and scientific data on emergency stroke care and considering how to apply the 10 programs for out-of-hospital cardiac arrest to emergency stroke care. According to the Utstein methodology, six major issues were defined, including sub-questions for discussions. Prior to the meeting, two chairs were identified to facilitate the discussion of the topics. The participants were divided into six groups and rotated between the six topics to discuss and refine the solutions. At the end of day two, the results were presented by the chairs for debate and new questions were discussed in plenary followed by an immediate summary. After the meeting, the chairs had teleconferences to finalize the final recommendations and prepare this document. The final document was further discussed and approved by the full Utstein group. The recommendations are founded on existing guidelines, evidence-based practice and experts’ knowledge from both cardiac arrest and stroke care. Furthermore, examples of best practices have been identified to be used to inspire implementation.
Results
Ten programs to improve survival and outcome after stroke
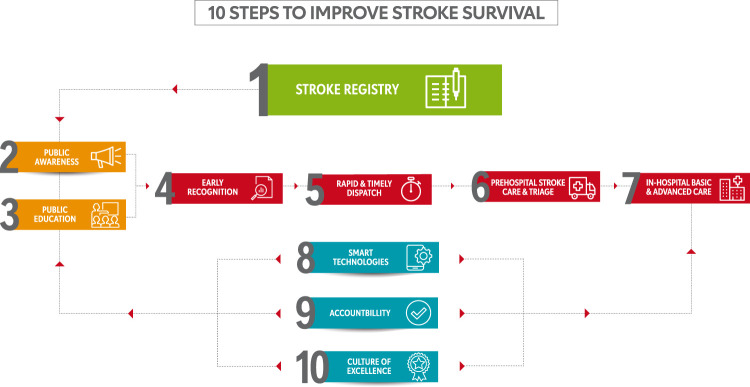
Figure 1 summarizes the 10 programs and Figure 2 shows the key recommendations.
Figure 1.
Ten programs to improve stroke survival.
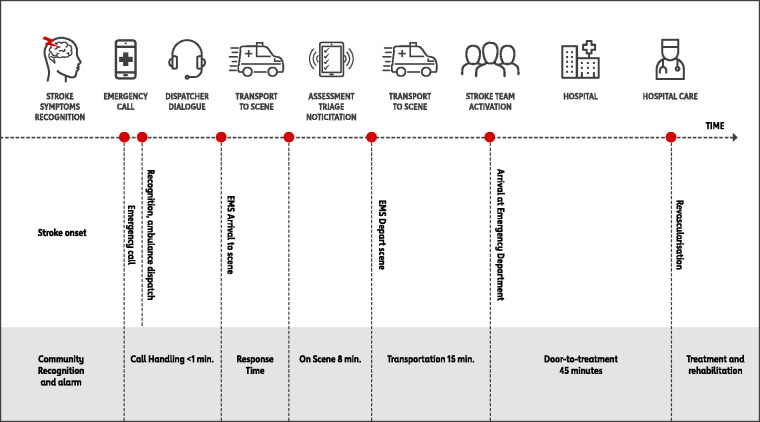
Figure 2.
Chain of survival for emergency stroke care.
(1) Establish a Stroke Registry
Data are essential to improve care and outcomes. You cannot improve what you do not measure; therefore a stroke registry is essential to identify current performance, areas for improvement and the effects of quality improvement programs. Registries should be population-based, encompassing prehospital care, in-hospital care and survival, function and quality of life. A registry should measure clinical outcomes such as mortality and essential processes of stroke care. Only essential data that are easily measurable should be collected and where possible the data should be extracted from routine data sets. Examples of possible data elements are given in Table 1 (supplementary Appendix C). Stroke registries may encompass local, regional, state or national levels but function best where performance can be compared to earlier results and between services. Registries require appropriate resource allocation from hospitals, EMS and preferably government funding. Stroke should be a mandatory reportable disease in society. Global collaboration is needed to further develop and implement stroke registries, including enhancing comparability and ensuring data quality. Table 1 (supplementary Appendix C) suggests data items for an acute stroke care registry.
(2) Create public awareness
Two major barriers to timely stroke intervention are late recognition by the public and lack of activation of EMS. Both are crucial for successful early treatment, yet the latter is dependent upon the first. Increasing public awareness of stroke requires improving knowledge of its acute presentation. In a summary of 22 studies that surveyed such knowledge, only a few participants could name more than two risk factors in most studies. Knowledge of stroke warning signs varied widely, with a substantial proportion not knowing a single sign of stroke.17 For awareness of stroke warning signs, most studies identified greater knowledge in women compared with men. Individuals with pre-existing conditions tended to know more about risk factors and warning signs than people without such history and most the studies reported better knowledge in older participants. Lower socio-economic groups and people with less education were less knowledgeable than higher socio-economic groups and people with higher education. Although stroke knowledge improved recently, the public’s recognition of these warning signs still remains unsatisfactory.18
Accompanying this challenge is the added need for the public to recognize stroke as a treatable and time-dependent condition and therefore immediately activate EMS. Help-seeking behavior after acute stroke is a complex and not well-understood process, requiring not only knowledge of stroke symptoms but also their correct recognition by the patient or bystander, and an understanding of how to activate the process of acute stroke care. Studies have shown that patients brought to the hospital by EMS arrive sooner after onset of their symptoms than those transported by other means and receive more rapid evaluation and treatment.19 In countries with well-developed EMS systems, people with stroke use EMS about 60 % of the time for transportation to the hospital.20 Individuals showing signs of major stroke such as paresis, aphasia, or altered level of consciousness are more likely to use EMS than those with symptoms such as vision disturbance, ataxia, or vertigo.21,22 Patients transported by EMS receive more sophisticated prehospital care and evaluation22 and are treated more quickly at the stroke center.23 Thus, promoting early recognition and triggering an EMS-focused response are paramount priorities for public stroke education.
(3) Start public education
Educational efforts should be broad-based and built upon advertising success in other domains. These can include mass media campaigns, targeted programs in schools, ambassadors and social media. An important part of public education is dispelling fatalistic attitudes about stroke using success stories that highlight the potential for excellent functional outcomes, with the best likelihood for optimal recovery when identified readily and treated rapidly. Studies have shown that when aimed at potential patients and bystanders, such knowledge can incentivize learning, remembering, and implementing a stroke recognition and action plan, resulting in more rapid hospital presentation and intervention.24 Regardless of approach, one challenge is maintaining the durability of the education initiative and this may require repeat messaging in various media formats and recurring reminders using testimonials of success. The ultimate goal is to foster an ongoing partnership between the public, EMS, the hospitals and community that results in more rapid programs to intervene in a potentially devastating but potentially reversible condition. Stroke education and campaigning should be directed both to the public and to the medical services and in-hospital personnel involved in stroke triage and treatment.
(4) Improve early recognition by first responders
Early recognition of potential stroke symptoms by emergency dispatchers is critical to activating emergency stroke care. Once a call to an emergency center occurs, the call-taker needs to differentiate the 1–2% of patients with stroke from the range of other emergency conditions. As patients often do not recognize their symptoms as being due to stroke, their description of symptoms may be unclear. Emergency call centers often use a predefined guideline for prioritizing stroke as part of their computer aided dispatch system. Some identification strategies are insensitive, detecting between 40 % and 65 % of acute strokes with variable specificity.25–27 There is no evidence favoring any one particular diagnostic scale or strategy by emergency call takers to identify stroke.28 However, using a tool to facilitate rapid recognition seems obvious and recently the American Heart Association/American Stroke Association has recommended new time process indicators for emergency call-taking and dispatch.3 Many stroke patients and relatives contact non-acute health services, such as general practitioners or various help lines. These should also be able to identify potential stroke patients and to directly activate the emergency call center.
(5) Practice rapid and timely dispatch
Accurate recognition by dispatchers is key to rapid treatment. In a Norwegian study,29 when the emergency call-taker suspected a diagnosis of stroke, ambulance services were dispatched as high priority response to 92% of patients. But if the call-taker missed the diagnosis, the ambulance was dispatched as high priority response in only about 55% of cases. Based on the initial dialogue, the presence of key symptoms (for instance Face-Arm-Speech-Time questions) should lead to an immediate high priority response. Even patients with transient stroke symptoms should have an acute EMS response. Once an initial response is sent, additional questions may clarify the diagnosis and allow dispatch of additional specialist resources, such as a mobile stroke unit. When acute stroke is suspected, call-takers should ask additional questions, e.g. contact information for caregiver, time last known well, and communicate the results to the EMS team to assist in choosing the appropriate receiving hospital.
(6) Optimize prehospital stroke care and triage
There are three phases of a prehospital stroke care program: field screening and assessment, treatment in the field and in transit, and notification of the receiving hospital. During the screening phase, emergency personnel should use validated stroke identification tools.30,31 Once stroke is suspected, other tools may be employed aiming to identify strokes due to large vessel occlusion (LVO),32,33 although all current existing prehospital LVO detection tools have low specificity and currently should not be used to triage patients for thrombectomy although pending further studies may be useful for triaging patients to stroke centers with interventional capabilities, though not necessarily requiring thrombectomy. Essential vital sign assessment should include heart rate, blood pressure, blood glucose, and pulse oximetry measurements.34,35 The pre-arrival notification phase is the critical link between prehospital and hospital care to shorten the time interval from hospital arrival to treatment initiation. In addition to notifying that a suspected stroke patient is enroute, provision of key information will allow the hospital to prepare for appropriate prompt assessment and treatment.36,37 There is an important balance between adequate assessment and treatment in the prehospital environment and rapid transport to definitive hospital care. The patient should be triaged to a pre-defined facility for intravenous thrombolysis and potential EVT based on the local stroke system of care. It is key for effective acute stroke services to have regional planning of a stroke system of care and clear pathways to minimize delays in therapeutic decision-making and delivery of care. This requires transportation to a center that will minimize treatment time. Optimizing these transport decisions requires modelling based on factors such as population density, stroke incidence, hospital capabilities and performance metrics and transport times. An ideal acute stroke service is one that is reached quickly, with immediate access to stroke specialist care either on site or via telemedicine, capable of emergent brain imaging including angiography and perfusion with a dedicated stroke unit, expertise in intravenous thrombolysis and EVT, and all organized to provide expert care with minimal delay.38 For the provision of EVT air transport providers should work together to identify the most efficient transport option both pre- and inter-hospital. This should include immediate availability and back-up systems. A cross sector collaborative approach will be more effective than identifying a single preferred provider.
(7) Optimize In-hospital triage and acute care
Expert guidelines for the management of stroke in the emergency department have been produced3,4 and will not be repeated here. There is good evidence to show that rapid treatment of both ischemic and hemorrhagic stroke39 can improve outcomes and often neglected is the need for early rehabilitation. However, achieving this requires high levels of coordination and ongoing staff training involving EMS staff, radiology and the stroke team. Up-to-date evidence-based protocols are needed to cover the acute management of ischemic and hemorrhagic stroke, and transient ischemic attack (TIA)3,39 and there needs to be regular review of performance against these protocols. It is unacceptable that some units have average door to needle times of 1 h when others can achieve it in 20 min.40,41 While not all admitting units will have access to interventional neuroradiology, protocols are needed to ensure rapid “door in, door out” times, with immediate transfer of medical records and imaging to the thrombectomy center.
(8) Use smart technologies
New technologies are emerging and have been successful in other areas of emergency care and may assist with recognition and early treatment of stroke. Linguists and computer scientists may be able to develop new solutions. Machine learning and artificial intelligence should be evaluated to assist dispatchers in recognizing possible cases of stroke and are already used to aid in interpretation of neuroimaging. New video-assisted dispatch systems might enable dispatchers to better assess calls and be able to identify potential strokes. Smartphones are available in most communities, including low resource countries, and provide a cost effective means for public education in awareness of stroke symptoms and the importance of timely activation of emergency services, as well as activating the emergency medical response.42 Telemedicine is invaluable in providing expert advice in the acute setting, particularly in hospitals in rural areas where 24/7 on site specialists availability is not feasible.43 The use of telemedicine in the ambulance service is less well developed but has been shown to be practicable.44 Mobile stroke units have been shown to shorten assessment and treatment times compared to conventional hospital care but have not yet been shown to improve outcomes or to be cost-effective.45
(9) Demonstrate accountability
Transparency is essential when reporting performance of an emergency response and treatment system for acute stroke. It allows the community and stakeholders to gauge a system’s progress as well as its opportunities for improvement. One of the hallmarks of excellent stroke care is an ongoing quality improvement program with transparent public reporting of data. Regular monitoring of the metrics allows the public to identify the best-performing centers while motivating improvement among hospitals at the lower end of the performance spectrum to improve.46 Those involved in developing and optimizing the system are accountable to the public, to administrators and funding bodies, and to each other. Metrics describing a system’s performance may vary depending on the intended audience. Potential choices for primary performance metrics may also vary given the robustness of the available medical and emergency response systems. For example, systems within low- or middle-income countries may require different performance metrics than those in higher income nations. Feasible reporting of results will need to begin with data elements that can be collected locally and simply, and in a well-defined setting. Some systems may share data highlighting relevant challenges or best practices through scientific publications or other publicly accessible platforms. Demonstrating accountability might be for a well-defined portion of the stroke pathway or it might be for the entire patient journey, depending on responsibilities. Reporting should be linked to incentives for performance, annual accountability to stakeholders, and making decisions related to systems of care.
(10) Create a culture of excellence
The secret of moving a system from its current performance level to a “Culture of Excellence” requires an environment that empowers, focuses and engages staff, and equips teams with the right mindset and skills necessary to achieve the best results. A culture of excellence has a system and staff that use a combination of best practice evidence and performance data to continually review their practices and identify opportunities to improve patient care. They must focus on creating a system that exudes excellence, breaking records, and achieving extraordinary results. As has been witnessed from the work of the GRA in out-of-hospital cardiac arrest, we need to identify the “best of breed” and seek to emulate their performance.47 A system that sets the benchmark for excellence is not necessarily the best resourced service or the most advanced, but the one that integrates, and recognizes the importance of, the whole system in achieving the best possible outcomes for patients. To create a culture of excellence takes time and it starts with you!
To achieve a culture of excellence, every staff member must understand not only the organization’s vision, but also know their own roles, responsibilities, and the specific actions they need to implement to achieve this vision. In a culture of excellence, staff feel that their contribution is meaningful, significant, and purposeful. Staff need to be inspired by the common purpose which becomes the driving force behind everything that they do. Organizations focused on achieving a culture of excellence must set an expectation of high performance. Every staff member must be supported and encouraged to become a master in their role and area of expertise.
Up-to-date evidence-based protocols should be in place to cover the acute management of ischemic stroke, hemorrhagic stroke and TIA. Many services already have in place quality improvement programs. For example, in the US and globally, The Institute for Healthcare Improvement Triple Aims framework.48 In Australia, The National Safety and Quality Health Service Standards49 and in the UK, the Sentinel Stroke National Audit Programme.40
The chain of survival for emergency stroke care and patient journey
To promote awareness, educate, and create a framework for accountability and excellence, the Utstein meeting resulted in an additional illustration of the Chain of Survival for emergency stroke care (Figure 2) and a stroke patient journey pathway illustration (Figure 3).
Figure 4.
Summarizing best practice programs and actions.
Figure 3.
Stroke patient journey.
Stroke is a time-sensitive emergency. Many initiatives have focused on the reduction in door-to-treatment times (both with intravenous thrombolysis and endovascular therapy) and have achieved positive results in reducing times and improving patient outcomes.50–52 Other time-sensitive emergencies, notably myocardial infarction, have focused on reducing door-to-treatment times with success in reducing times.53 In understanding the primary importance of symptom onset to treatment in overall outcomes, efforts have logically evolved to extend beyond hospital treatment times, focusing on systems of care that include the public, partnership with EMS and referral hospitals to reduce prehospital times and improve the efficiency of the entire system. Stroke has similarly evolved, with efforts to focus on systems of care, including partnerships with EMS, telestroke, and multi-tiered stroke center designation. Recently, the positive results of endovascular trials have highlighted the need for stroke systems of care that direct patients to the most appropriate facility for treatment and as quickly as possible. Even in countries with highly developed stroke systems of care, prehospital severity screening to try to identify LVO and destination algorithms are challenging to implement uniformly, as access to primary and comprehensive stroke centers varies by geography and regional resources, as does access to EMS and EMS training in severity scores. In low- and middle-income countries, the primary challenges are often related to the lack of well-developed EMS systems. These factors highlight the need for international collaboration and recommendations for a stroke chain of survival that addresses the most critical components of acute stroke care from onset to intervention with the ability to be implemented in a variety of settings. The Utstein meeting developed a comprehensive chain of survival to facilitate worldwide improvements in stroke care.
Supplementary material of best practice of the 10 programs from international organizations is available as attachment (supplementary Appendix C). Further references are available in supplementary Appendix D.
Conclusion
Current outcome and survival from stroke can be improved by optimizing each part of the Chain of Survival of Stroke, improving the survival and outcome for individuals with stroke and the community. Key elements from the “Chain of Survival” for cardiac arrest can be translated into 10 programs for improving the survival and outcome after acute stroke. The 10 programs promote best practices and offer help with implementation, enabling communities to improve the stroke survival and outcome rates (Figure 4).
Supplemental Material
Supplemental material, WSO915135 Supplemental Material for Utstein recommendation for emergency stroke care by AG Rudd, C Bladin, P Carli, DA De Silva, TS Field, EC Jauch, P Kudenchuk, MW Kurz, T Lærdal, MEH Ong, P Panagos, A Ranta, C Rutan, MR Sayre, L Schonau, SD Shin, D Waters and F Lippert on behalf of the Utstein Stroke working group in International Journal of Stroke
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
AG Rudd https://orcid.org/0000-0002-5738-2703
TS Field https://orcid.org/0000-0002-1176-0633
Supplemental material
Supplemental material for this article is available online.
References
- 1.Benjamin EJ, Muntner P, Bittencourt MS. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation 2019; 139: e56–e528. [DOI] [PubMed] [Google Scholar]
- 2.Stevens E, Emmett E, Wang Y, McKevitt C and Wolfe CDA. The Burden of Stroke in Europe, https://www.stroke.org.uk/sites/default/files/theburdenofstrokeineuropereport.pdf (2015, accessed 18 March 2020).
- 3.Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2018; 49: e46–e99. [DOI] [PubMed] [Google Scholar]
- 4.Intercollegiate Stroke Working Party. National Clinical Guidelines for Stroke 5th Edition 2016 Royal College of Physicians, London, https://www.rcplondon.ac.uk/guidelines-policy/stroke-guidelines (accessed 18 March 2020).
- 5.Lecouturier J, Murtagh MJ, Thomson RG, et al. Response to symptoms of stroke in the UK: a systematic review. BMC Health Serv Res 2010; 10: 157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Suryanto M, Plummer V, Boyle M. EMS systems in lower-middle income countries: a literature review. Prehosp Disaster Med 2017; 32: 64–70. [DOI] [PubMed] [Google Scholar]
- 7.Robinson T. Reperfusion in the brain: is time important? The DAWN and DEFUSE-3 trials. Cardiovasc Res 2018; 114: e9–e28. [DOI] [PubMed] [Google Scholar]
- 8.Thomalla G, Boutitie F, Fiebach JB, et al. Stroke with unknown time of symptom onset: baseline clinical and magnetic resonance imaging data of the first thousand patients in WAKE-UP (efficacy and safety of MRI-based thrombolysis in wake-up stroke: a randomized, doubleblind, placebo-controlled trial). Stroke 2017; 48: 770–773. [DOI] [PubMed] [Google Scholar]
- 9.Khatri P, Yeatts SD, Mazighi M, et al. Time to angiographic reperfusion and clinical outcome after acute ischaemic stroke: an analysis of data from the Interventional Management of Stroke (IMS III) phase 3 trial. Lancet Neurol 2014; 13: 567–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Emberson J, Lees KR, Lyden P, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet 2014; 384: 1929–1935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim YT, Shin SD, Hong SO, et al. Effect of national implementation of Utstein recommendation from the global resuscitation alliance on ten steps to improve outcomes from Out-of-Hospital cardiac arrest: a ten-year observational study in Korea. BMJ Open 2017; 7: e016925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cummins RO, Chamberlain DA, Abramson NS, et al. Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: the Utstein Style. A statement for health professionals from a task force of the American Heart Association, the European Resuscitation Council, the Heart and Stroke Foundation of Canada, and the Australian Resuscitation Council. Circulation 1991; 84: 960–975. [DOI] [PubMed] [Google Scholar]
- 13.Cummins RO, Chamberlain D, Hazinski MF, et al. Recommended guidelines for reviewing, reporting, and conducting research on in-hospital resuscitation: the in-hospital “Utstein style”. Ann Emerg Med 1997; 29: 650–679. [DOI] [PubMed] [Google Scholar]
- 14.Perkins G, Jacobs I, Nadkarni V, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein resuscitation registry templates for out-of-hospital cardiac arrest. Resuscitation 2015; 96: 328–340. [DOI] [PubMed] [Google Scholar]
- 15.Nadarajan GD, Tiah L, Ho AFW, Azazh A et al. Global resuscitation alliance utstein recommendations for developing emergency care systems to improve cardiac arrest survival. Resuscitation 2018; 132: 85–89. [DOI] [PubMed]
- 16.Alliance GR. Resuscitation Academy, http://www.resuscitationacademy.org/global-resuscitation-alliance/ (accessed 18 March 2020).
- 17.Stroebele N, Müller-Riemenschneider F, Nolte CH, Müller-Nordhorn J, Bockelbrink A, Willich SN. Knowledge of risk factors, and warning signs of stroke: a systematic review from a gender perspective. Int J Stroke 2011; 6: 60–66. [DOI] [PubMed] [Google Scholar]
- 18.Oh G-J, Moon J, Lee Y-M, et al. Public awareness of stroke and its predicting factors in Korea: a national public telephone survey, 2012 and 2014. J Korean Med Sci 2016; 31: 1703–1710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ekundayo OJ, Saver JL, Fonarow GC, et al. Patterns of emergency medical services use and its association with timely stroke treatment: findings from Get With the Guidelines-Stroke. Circulation Cardiovasc Qual Outcomes 2013; 6: 262–269. [DOI] [PubMed] [Google Scholar]
- 20.Mochari-Greenberger H, Xian Y, Hellkamp AS, et al. Racial/ethnic and sex differences in emergency medical services transport among hospitalized US stroke patients: analysis of the National Get With The Guidelines–Stroke Registry. J Am Heart Assoc 2015; 4: e002099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kleindorfer D, Lindsell CJ, Moomaw CJ, et al. Which stroke symptoms prompt a 911 call? A population-based study. Am J Emerg Med 2010; 28: 607–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oostema JA, Chassee T, Reeves M. Emergency dispatcher stroke recognition: associations with downstream care. Prehosp Emerg Care 2018; 22(4): 466–471. [DOI] [PubMed] [Google Scholar]
- 23.Caceres JA, Adil MM, Jadhav V, et al. Diagnosis of stroke by emergency medical dispatchers and its impact on the prehospital care of patients. J Stroke Cerebrovasc Dis 2013; 22: e610–e614. [DOI] [PubMed] [Google Scholar]
- 24.Wolters FJ, Paul NL, Li L, Rothwell PM. Sustained impact of UK FAST-test public education on response to stroke: a population-based time-series study. Int J Stroke 2015; 10: 1108–1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mould-Millman N-K, Meese H, Alattas I, et al. Accuracy of prehospital identification of stroke in a large stroke belt municipality. Prehosp Emerg Care 2018; 22(6): 734–742. [DOI] [PubMed] [Google Scholar]
- 26.Richards CT, Wang B, Markul E, et al. Identifying key words in 9-1-1 calls for stroke: a mixed methods approach. Prehosp Emerg Care 2017; 21: 761–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yvonne T, Michael B. Stroke education: discrepancies among factors influencing prehospital delay and stroke knowledge. Int J Stroke 2010; 5: 187–208. [DOI] [PubMed] [Google Scholar]
- 28.Rudd M, Buck D, Ford GA, Price CI. A systematic review of stroke recognition instruments in hospital and prehospital settings. Emerg Med J 2016; 33: 818–822. [DOI] [PubMed] [Google Scholar]
- 29.Viereck S, Møller TP, Iversen HK, Christensen H, Lippert F. Medical dispatchers recognise substantial amount of acute stroke during emergency calls. Scand J Trauma Resusc Emerg Med 2016; 24: 89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kidwell CS, Starkman S, Eckstein M, Weems K, Saver JL. Identifying stroke in the field: prospective validation of the Los Angeles Prehospital Stroke Screen (LAPSS). Stroke 2000; 31: 71–76. [DOI] [PubMed] [Google Scholar]
- 31.Bray JE, Martin J, Cooper G, Barger B, Bernard S, Bladin C. Paramedic identification of stroke: community validation of the Melbourne ambulance stroke screen. Cerebrovasc Dis 2005; 20: 28–33. [DOI] [PubMed] [Google Scholar]
- 32.Richards CT, Huebinger R, Tataris KL, et al. Cincinnati prehospital stroke scale can identify large vessel occlusion stroke. Prehosp Emerg Care 2018; 22: 312–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Perez de la Ossa N, Carrera D, Gorchs M, et al. Design and validation of a prehospital stroke scale to predict large arterial occlusion the rapid arterial occlusion evaluation scale. Stroke 2014; 45: 87–91. [DOI] [PubMed] [Google Scholar]
- 34.Jauch EC, Saver JL, Adams HP, Jr, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013; 44: 870–947. [DOI] [PubMed] [Google Scholar]
- 35.Slavin SJ, Sucharew H, Alwell K, et al. Prehospital neurological deterioration in stroke. Emerg Med J 2018; 35: 507–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hsieh M-J, Tang S-C, Chiang W-C, Tsai L-K, Jeng J-S, Ma MH-M. Effect of prehospital notification on acute stroke care: a multicenter study. Scand J Trauma Resusc Emerg Med 2016; 24: 57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Higashida R, Alberts MJ, Alexander DN, et al. Interactions within stroke systems of care: a policy statement from the American Heart Association/American Stroke Association. Stroke 2013; 44: 2961–2984. [DOI] [PubMed] [Google Scholar]
- 38.Norrving B, Barrick J, Davalos A, et al. Action plan for Stroke in Europe 2018–2030. Eur Stroke J 2018; 3: 309–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Parry-Jones A. Cutting delays in reversing anticoagulation after intracerebral haemorrhage: three key changes at a UK comprehensive stroke centre. BMJ Qual Improv Rep 2015; 4: u208763.w3521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sentinel Stroke National Audit Programme (SSNAP), www.strokeaudit.org (accessed 18 March 2020).
- 41.Meretoja A, Strbian D, Mustanoja S, Tatlisumak T, Lindsberg PJ, Kaste M. Reducing in-hospital delay to 20 minutes in stroke thrombolysis. Neurology 2012; 79: 306–313. [DOI] [PubMed] [Google Scholar]
- 42.Nogueira RG, Silva GS, Lima FO, et al. The FAST-ED App: a smartphone platform for the field triage of patients with stroke. Stroke 2017; 48: 1278–1284. [DOI] [PubMed] [Google Scholar]
- 43.Wechsler LR, Demaerschalk BM, Schwamm LH, et al. American Heart Association Stroke Council; Council on Epidemiology and Prevention; Council on Quality of Care and Outcomes Research. Telemedicine quality and outcomes in stroke: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2017; 48: e3–e25. [DOI] [PubMed] [Google Scholar]
- 44.Lippman JM, Smith SNC, McMurry TL, et al. Mobile telestroke during ambulance transport is feasible in a rural EMS setting: the iTREAT Study. Telemed e-Health 2016; 22: 507–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tsivgoulis G, Geisler F, Katsanos AH, et al. Ultraearly intravenous thrombolysis for acute ischemic stroke in mobile stroke unit and hospital settings: a comparative analysis. Stroke 2018; 49: 1996–1999. [DOI] [PubMed] [Google Scholar]
- 46.Machline-Carrion MJ, Santucci EV, Damiani LP, et al. An international cluster randomized quality-improvement trial to increase the adherence to evidence-based therapies for acute ischemic stroke and transient ischemic attack patients: rationale and design of the BRIDGE STROKE trial. Am Heart J 2019; 207: 49–57. [DOI] [PubMed] [Google Scholar]
- 47.Resuscitation Alliance. Improving survival from out-of-hospital cardiac arrest acting on the call, 2018 update from the global resuscitation alliance including 27 case reports, 2018, https://www.globalresuscitationalliance.org/wp-content/pdf/acting_on_the_call.pdf (accessed 18 March 2020).
- 48.Improvement IfH. Triple Aim for Populations, http://www.ihi.org/Topics/TripleAim/Pages/default.aspx (accessed 18 March 2020).
- 49.Care ACoSaQiH. Assessment to the NSQHS Standards, https://www.safetyandquality.gov.au/our-work/assessment-to-the-nsqhs-standards/ (accessed 18 March 2020).
- 50.Ford AL, Williams JA, Spencer M, et al. Reducing door-to-needle times using Toyota’s lean manufacturing principles and value stream analysis. Stroke 2012; 43: 3395–3398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fonarow GC, Smith EE, Saver JL, et al. Improving door-to-needle times in acute ischemic stroke: the design and rationale for the American Heart Association/American Stroke Association's Target: Stroke initiative. Stroke 2011; 42: 2983–2989. [DOI] [PubMed] [Google Scholar]
- 52.Kansagra AP, Wallace AN, Curfman DR, et al. Streamlined triage and transfer protocols improve door-to-puncture time for endovascular thrombectomy in acute ischemic stroke. Clin Neurol Neurosurg 2018; 166: 71–75. [DOI] [PubMed] [Google Scholar]
- 53.Krumholz HM, Herrin J, Miller LE, et al. Improvements in door-to-balloon time in the United States, 2005 to 2010. Circulation 2011; 124: 1038–1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, WSO915135 Supplemental Material for Utstein recommendation for emergency stroke care by AG Rudd, C Bladin, P Carli, DA De Silva, TS Field, EC Jauch, P Kudenchuk, MW Kurz, T Lærdal, MEH Ong, P Panagos, A Ranta, C Rutan, MR Sayre, L Schonau, SD Shin, D Waters and F Lippert on behalf of the Utstein Stroke working group in International Journal of Stroke