Abstract
Background:
Racial and ethnic disparities in healthcare are well documented in the United States, although evidence of disparities in pediatric anesthesia is limited. We sought to determine if there is an association between race and ethnicity and the use of intraoperative regional anesthesia at a single academic children’s hospital.
Methods:
We performed a retrospective review of all anesthetics at an academic tertiary children’s hospital between May 4th, 2014 and May 31st, 2018. The primary outcome was delivery of regional anesthesia, defined as a neuraxial or peripheral nerve block. The association between patient race and ethnicity (white non-Hispanic or minority) and receipt of regional anesthesia was assessed using multivariable logistic regression. Sensitivity analyses were performed comparing white non-Hispanic to an expansion of the single minority group to individual racial and ethnic groups and on patients undergoing surgeries most likely to receive regional anesthesia (orthopedic and urology patients).
Results:
Of 33,713 patient cases eligible for inclusion, 25,664 met criteria for analysis. 3,189 patients (12.4%) received regional anesthesia. 1,186 (13.3%) of 8,884 white non-Hispanic patients and 2,003 (11.9%) of 16,780 minority patients received regional anesthesia. After multivariable adjustment for confounding, race and ethnicity were not found to be significantly associated with receiving intraoperative regional anesthesia (adjusted odds ratio 0.95, 95% confidence interval: 0.86–1.06; p=0.36). Sensitivity analyses did not find significant differences between the white non-Hispanic group and individual races and ethnicities, nor did they find significant differences when analyzing only orthopedic and urology patients, despite observing some meaningful clinical differences.
Conclusions:
In an analysis of patients undergoing surgical anesthesia at a single academic children’s hospital, race and ethnicity were not significantly associated with the adjusted odds of receiving intraoperative regional anesthesia. This finding contrasts with much of the existing health care disparities literature and warrants further study with additional datasets to understand the mechanisms involved.
Introduction:
Racial and ethnic disparities in health services in the United States have been well-documented for many years across multiple specialties.1–2 In pediatrics, these disparities have appeared in the emergency department,3–5 in mental health clinics,6 and in the operating room.7 Such racial and ethnic disparities in health services have been shown to impact health outcomes in a variety of settings and disease states.8
Investigations on racial and ethnic disparities in pediatric perioperative anesthesiology are currently limited and inconclusive. Available studies on perioperative pharmacologic treatment in pediatric anesthesia have demonstrated reduced opioid receipt to Latino tonsillectomy and adenoidectomy patients compared to Caucasian patients in the post-anesthesia care unit (PACU),9 increased PACU opioid administration to African-American children after tonsillectomy as compared to Caucasian children,10 a lack of association with race in preoperative and intraoperative medication administration in appendectomy patients,11 and increased likelihood of PACU opioid treatment in minority children undergoing elective outpatient surgery compared to Caucasian children.12 Although adult studies have consistently demonstrated differences in the use of regional anesthesia in the perioperative13–14 and obstetric15–16 settings by race and ethnicity, to our knowledge no studies have focused on associations with race or ethnicity in the use of pre-operative and intraoperative regional anesthesia for children undergoing surgical procedures.
Large, multicenter trials have demonstrated that pediatric peripheral nerve and neuraxial blocks are safe,17–18 and several professional societies recommend the use of these anesthetic techniques for postoperative pain control.19 As the use of regional anesthesia for children undergoing surgery represents a common practice, we sought to determine if racial or ethnic associations exist in the rate of utilization of intraoperative regional anesthesia at a single, academic children’s hospital. With evidence of racial and ethnic disparities in medical and anesthesia (although not to date in pediatric anesthesia) health services,1,3–7 the primary hypothesis was that white non-Hispanic children would be more likely to receive regional anesthesia than racial or ethnic minority children.
Methods:
Study design:
This report is a retrospective cohort study that is part of an ongoing quality improvement project investigating if racial or ethnic associations exist in the perioperative care of children undergoing anesthesia at the Lucile Packard Children’s Hospital at Stanford University (Stanford, CA). As such, the requirement for written informed consent for this project was granted a waiver by the Stanford University Institutional Review Board.
Study Population:
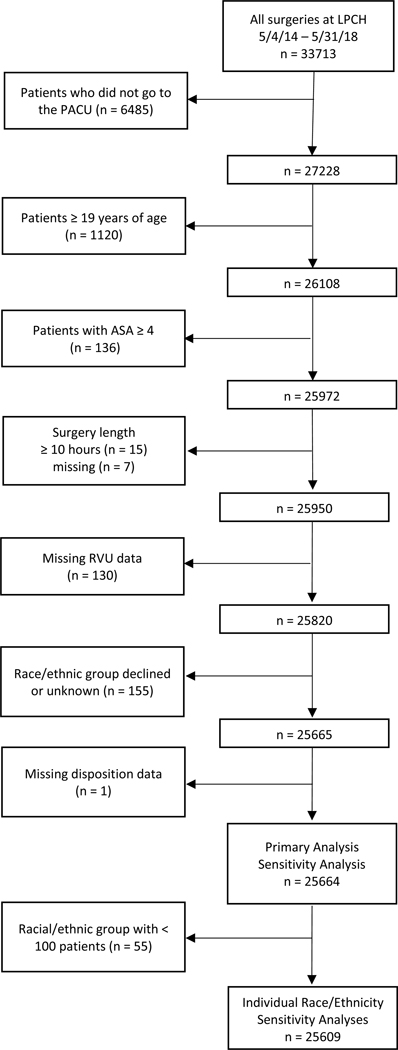
All anesthetics taking place at a single, academic children’s hospital between May 4th, 2014 and May 31st, 2018 were retrospectively reviewed. We used SAP Business Objects BI Platform 4.2 (Version: 14.2.5.2618), a reporting and analytics platform, which runs structured query language (SQL) queries off a SAP Business Objects Universe (our enterprise data warehouse incorporating data from Epic Clarity tables) to create a patient dataset from the hospital’s electronic medical record system (Epic Systems, Verona, WI). In order to exclude anesthetics for diagnostic imaging procedures (which do not, as a rule, involve regional anesthesia), eligible procedures were identified by 1) the presence of an anesthetic start time, 2) a procedure location in the main and ambulatory operating areas and 3) a PACU arrival time. Patients were excluded if they were greater than or equal to 19 years of age, American Society of Anesthesiologists physical status classification (ASA class) of 4 or greater, or in surgery for greater than or equal to 10 hours because the severity of illness may have created a complicated clinical picture that is difficult to capture in retrospective analysis. Patients who declined to state racial or ethnic groups or whose racial or ethnic group was unknown were excluded. Patients whose case complexity, surgery length, or disposition was missing were excluded from analysis because these variables were considered potential confounders. Figure 1 details the number of patients in each exclusion group. There were no other missing data.
Figure 1:
Flow diagram of study population selection. LPCH – Lucile Packard Children’s Hospital Stanford; ASA – American Society of Anesthesiologists; RVUs – Relative Value Units
Outcome and exposure:
The primary outcome was defined as receipt of any regional anesthesia as part of the intraoperative anesthetic. We defined regional anesthesia as neuraxial anesthesia, head and neck peripheral nerve blocks, truncal peripheral nerve blocks, and limb peripheral nerve blocks. The use of regional anesthesia was identified by the presence of documentation of block placement, block start and block end times in the anesthetic record and/or the route of medication administration (peripheral nerve block, epidural, caudal, continuous epidural, or intrathecal). The primary exposure was defined as racial and ethnic group: white non-Hispanic and minority, composed of black/African-American, Asian, Pacific Islander, other non-Hispanic, Hispanic, and American Indian/Alaska Native. We elected to aggregate minority groups in our primary analysis given small sample sizes of certain groups. Race and ethnicity are self-identified by patients and patients’ care givers during hospital or clinic registration. A sensitivity analysis was performed comparing white non-Hispanic to an expansion of minority to individual racial and ethnic groups: black/African-American, Asian, Pacific Islander, other non-Hispanic, and Hispanic. Racial or ethnic groups with fewer than 100 patients (American Indian/Alaska Native) were excluded from this sensitivity analysis given insufficient numbers. In order to focus on the patients most likely to receive regional anesthesia, a sensitivity analysis was also performed on cases in orthopedics or urology services, the services with the highest percentage of block utilization at the institution.
Statistical analysis:
Statistical analyses were planned a priori. Baseline participant demographics and characteristics were reported as frequency count by racial or ethnic group. A multivariable logistic regression model was fitted to estimate the relationship between race and ethnicity and the use of regional anesthesia. To choose variables for which to control in the model, potential confounders were identified by clinical knowledge and existing literature11–12,20 and the significance of their association with exposure and outcome was assessed: length of surgery, surgical/procedural service, case year (as the dedicated pediatric regional anesthesia team underwent changes in leadership, staffing, and was restructured in January 2018), case complexity (categorized based upon the sum of Relative Value Units for all procedures in the case: <10 minor, between 11 and 17 moderate, >17 major, as described previously21–22), sex, age, pre-/post-operative disposition (outpatient surgery, inpatient, radiation oncology, or surgery admit), ASA class, primary anesthesiologist, and need for interpreter. Variables that were significantly associated with both exposure and outcome were considered confounders and included in the multivariable model (see supplemental table 1).
Results are presented as adjusted odds ratios (ORs) with 95% confidence intervals (CIs). P-values are reported as two-tailed and p < 0.05 was considered significant. Adjustment for multiple comparisons was planned if statistically significant differences were found, but were not planned in the case of negative findings in order to reduce the risk of a false negative result. Analyses were performed using R (R Core Team, Vienna, Austria) and Stata 15 (StataCorp LLC, College Station, TX).
All available data that met inclusion criteria were analyzed. The observed sample size and probability of white non-Hispanic patients receiving a block gave this analysis 87% power to detect an odds ratio of 0.75 for the primary outcome for minority patients (effect size chosen based on prior reports)13–14 for a two-tailed test at significance level 0.05 when conservatively assuming that covariates are highly associated to race (R2=0.81).23
Results:
A total of 33,713 patients underwent surgical procedures between May 4th, 2014 and May 31st, 2018 at the Lucile Packard Children’s Hospital at Stanford University (Palo Alto, CA). One hundred and fifty-five patients declined to state racial or ethnic groups or reported unknown racial or ethnic group and were thus excluded from analysis. After all exclusions (8,048 patients, see Figure 1), 25,664 patients met criteria for the study and were included in the primary analysis of white non-Hispanic or minority race and ethnicity. Characteristics of included patients are listed in Table 1. A total of 3,189 patients (12.4%) received regional anesthesia, with 1,186 (13.3%) of 8,884 white non-Hispanic patients and 2,003 (11.9%) of 16,780 minority patients receiving regional anesthesia. Regional anesthesia included neuraxial anesthesia, head and neck peripheral nerve blocks, truncal peripheral nerve blocks, and extremity peripheral nerve blocks. Before adjusting for covariates, white non-Hispanic patients were significantly more likely than minority racial or ethnicity patients to receive intraoperative regional anesthesia (p=0.001 for Chi-squared analysis).
Table 1.
Characteristics of Study Patients
| White non-Hispanic | Minority Racial/Ethnic Group | Total | p | |||||
|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |||
| Age (years) | 0 to 2 | 1661 | 18.7 | 3568 | 21.3 | 5229 | 20.4 | <0.001 |
| 3 to 5 | 1792 | 20.2 | 3543 | 21.1 | 5335 | 20.8 | ||
| 6 to 11 | 2581 | 29.1 | 5098 | 30.4 | 7679 | 29.9 | ||
| 12 to 18 | 2850 | 32.1 | 4571 | 27.2 | 7421 | 28.9 | ||
| Sex | Female | 3723 | 41.9 | 7009 | 41.8 | 10732 | 41.8 | 0.833 |
| Male | 5161 | 58.1 | 9771 | 58.2 | 14932 | 58.2 | ||
| ASA rating | 1 | 3060 | 34.4 | 5521 | 32.9 | 8581 | 33.4 | 0.001 |
| 2 | 3822 | 43.0 | 7128 | 42.5 | 10950 | 42.7 | ||
| 3 | 2002 | 22.5 | 4131 | 24.6 | 6133 | 23.9 | ||
| Case complexity | Minor | 5347 | 60.2 | 10057 | 59.9 | 15404 | 60.0 | 0.05 |
| Moderate | 1578 | 17.8 | 3165 | 18.9 | 4743 | 18.5 | ||
| Major | 1959 | 22.1 | 3558 | 21.2 | 5517 | 21.5 | ||
| Year of surgery | 2014 | 1417 | 16.0 | 2399 | 14.3 | 3816 | 14.9 | <0.001 |
| 2015 | 2357 | 26.5 | 3906 | 23.3 | 6263 | 24.4 | ||
| 2016 | 2118 | 23.8 | 4067 | 24.2 | 6185 | 24.1 | ||
| 2017 | 2133 | 24.0 | 4589 | 27.3 | 6722 | 26.2 | ||
| 2018 | 859 | 9.7 | 1819 | 10.8 | 2678 | 10.4 | ||
| Patient disposition | Outpatient Surgery | 6180 | 69.6 | 11325 | 67.5 | 17505 | 68.2 | <0.001 |
| Inpatient | 922 | 10.4 | 1962 | 11.7 | 2884 | 11.2 | ||
| Radiation Oncology | 151 | 1.7 | 460 | 2.7 | 611 | 2.4 | ||
| Surgery Admit | 1631 | 18.4 | 3033 | 18.1 | 4664 | 18.2 | ||
| Service | Other | 2181 | 24.5 | 4761 | 28.4 | 6942 | 27.0 | <0.001 |
| Gastroenterology | 872 | 9.8 | 1082 | 6.4 | 1954 | 7.6 | ||
| General | 1300 | 14.6 | 2561 | 15.3 | 3861 | 15.0 | ||
| Orthopedics | 1354 | 15.2 | 2393 | 14.3 | 3747 | 14.6 | ||
| Otolaryngology | 2166 | 24.4 | 4281 | 25.5 | 6447 | 25.1 | ||
| Urology | 1011 | 11.4 | 1702 | 10.1 | 2713 | 10.6 | ||
| Interpreter Needed | No | 8803 | 99.1 | 11967 | 71.3 | 20770 | 80.9 | <0.001 |
| Yes | 81 | 0.9 | 4813 | 28.7 | 4894 | 19.1 | ||
| Surgery length (hours) | Median (interquartile range) | 0.62 | (0.32, 1.18) | 0.62 | (0.32, 1.25) | 0.62 | (0.32, 1.23) | 0.24 |
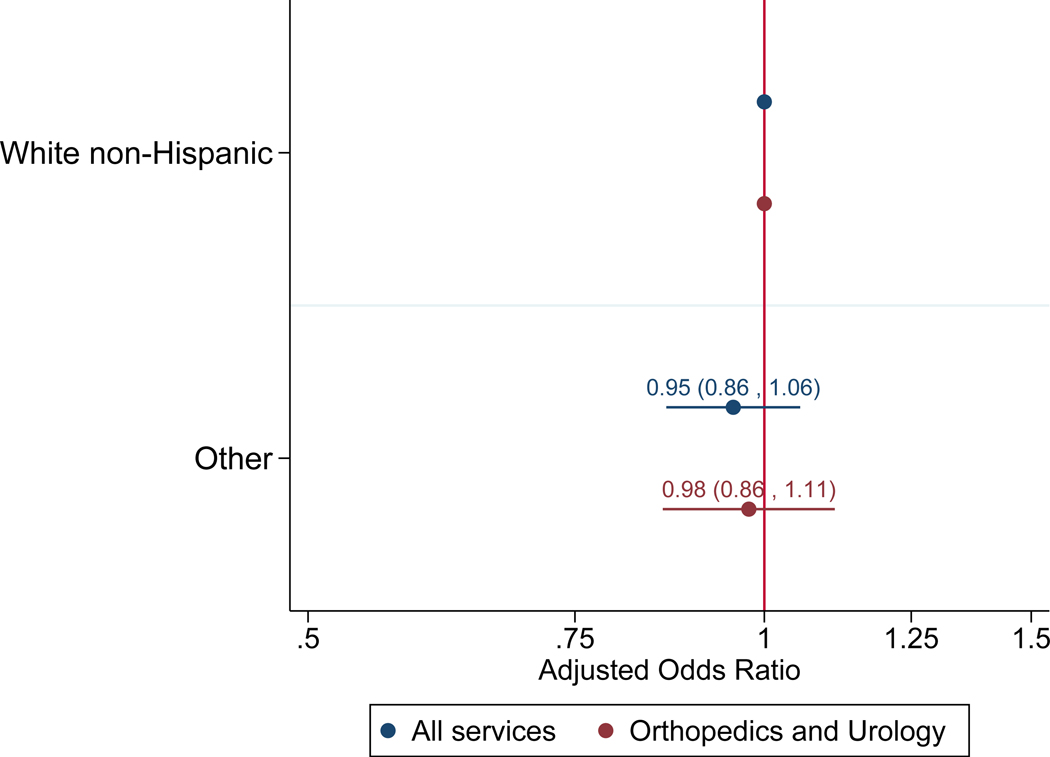
The following variables were each significantly associated with race (white non-Hispanic or minority) and with regional anesthesia and were therefore included in the multivariable regression model to control for confounding: age, patient disposition, year, ASA class, surgical/procedural service, need for interpreter, case complexity, and anesthesiologist. Results for adjusted odds of receiving regional anesthesia by race and ethnicity are shown in Figure 2. Overall, race and ethnicity were not estimated to be significantly associated with receiving regional anesthesia in the multivariable model (adjusted odds ratio 0.95 [95% CI: 0.86–1.06; p=0.36]).
Figure 2:
Adjusted odds ratios of receiving intraoperative regional anesthesia for minority race and ethnic groups for all services in the main analysis (blue) and orthopedics and urology in sensitivity analysis (red). The white non-Hispanic group serves as the reference group. The numbers represent the adjusted odds ratios with lower and upper bounds of the 95% confidence intervals in parentheses.
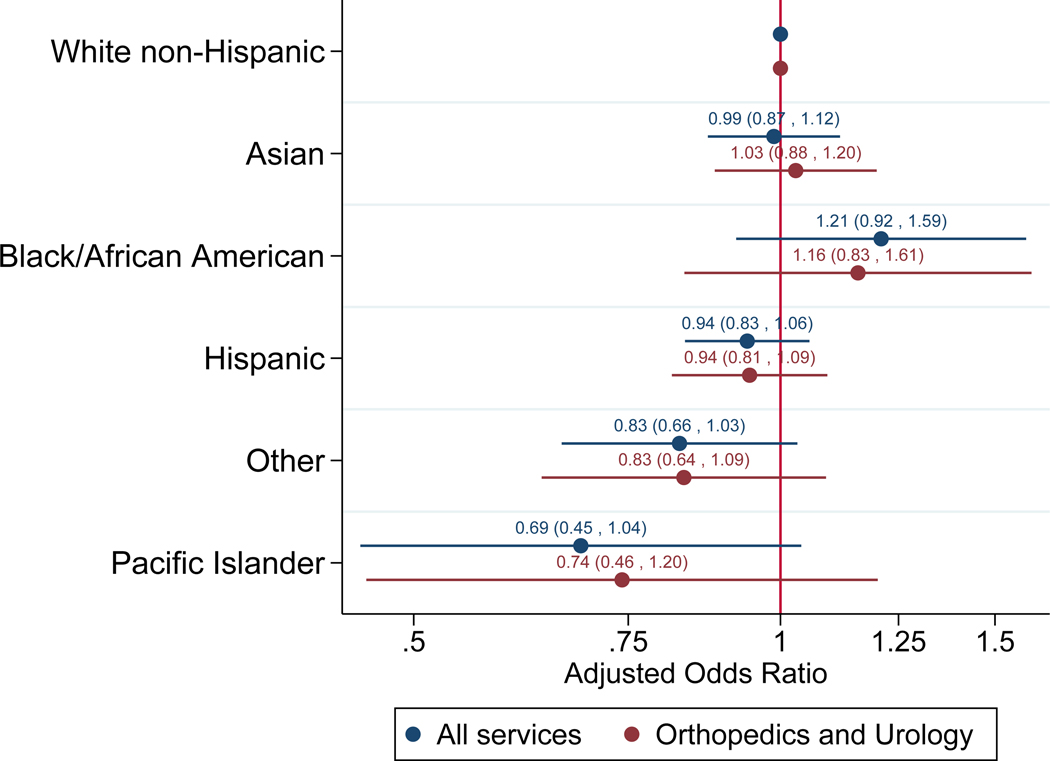
For the sensitivity analysis of expanded non-white race and ethnicity groups, fifty-five patients who belonged to a racial or ethnic group with less than 100 patients (American Indian/Alaskan Native) were excluded from analysis (25,609 patients included in sensitivity analysis). A total of 94 (16.8%) of 558 black/African-American patients, 608 (12.6%) of 4,807 Asian-American patients, 1,124 (11.4%) of 9,877 Hispanic patients, 137 (12.1%) of 1,133 other non-Hispanic patients, and 33 (9.4%) of 350 Pacific Islander patients received regional anesthesia (p < 0.001 for Chi-squared analysis). The following variables were each significantly associated with race and regional anesthesia and were therefore included in the multivariable regression model: age, patient disposition, year, ASA class, service, interpreter, gender, and anesthesiologist. None of the comparisons between individual races or ethnicities and the reference group of white/Non-Hispanic patients resulted in a significant adjusted odds ratio (Figure 3), and there was no significant evidence that including race improved the fit of the model (likelihood ratio test p=0.11). The adjusted odds ratios ranged from 1.21 (95% CI: 0.92–1.59) for black/African-American patients to 0.69 (95% CI: 0.45–1.04) for Pacific Islander patients.
Figure 3:
Adjusted odds ratios of receiving intraoperative regional anesthesia for individual minority race and ethnic group sensitivity analyses for all services (blue) and orthopedics and urology (red). The numbers represent the adjusted odds ratios with lower and upper bounds of the 95% confidence intervals in parentheses.
The surgical/procedural services with the highest rates of patient regional anesthetic receipt were orthopedics (39.6%) and urology (37.3%). Results of the sensitivity analysis performed on orthopedic and urologic procedures are also shown in Figure 2. Race and ethnicity were not estimated to be significantly associated with receiving regional anesthesia (p=0.72). For separate non-white racial or ethnicity groups undergoing orthopedic and urologic procedures, none of the comparisons between individual races or ethnicities and the base group of white/Non-Hispanic patients resulted in a significant adjusted odds ratio; individual racial or ethnic group adjusted odds ratios ranged from 1.16 (95% CI: 0.83–1.61) for black/African-American patients to 0.74 (95% CI: 0.46–1.20) for Pacific Islander patients (Figure 3).
Discussion:
Our study did not find a significant difference in the odds of white/non-Hispanic pediatric patients and pediatric patients of minority racial or ethnic groups receiving intraoperative regional anesthesia after adjusting for confounders. When considering minority racial and ethnic groups separately, none were estimated to have significantly different odds of receiving a regional anesthetic than the white/non-Hispanic reference group, and the direction of the adjusted association differed across racial and ethnic groups.
We hypothesized that white non-Hispanic children would be more likely to receive intraoperative regional anesthesia based on studies on regional anesthesia for adults. Prior work has demonstrated lower percentages of minority patients receiving epidural analgesia during labor15–16 and neuraxial anesthesia for inguinal hernia repair13 and hip or knee arthroplasty,14 although these studies did not specifically address the mechanisms behind these disparities.
We did not find significant differences in the use of intraoperative regional anesthesia among distinct racial and ethnic groups within the pediatric surgical population examined here. Several reasons might explain our finding. It is possible that racial or ethnic health services disparities do not exist in pediatric anesthesia care, despite the evidence of them in adult populations. Indeed, other pediatric studies have suggested the absence of racial and ethnic associations in intraoperative intravenous analgesia.9,11–12 As this study is retrospective and restricted to a single academic children’s hospital, the findings outlined here may have limited generalizability to pediatric anesthesia practice across the United States. Other institutions may, for example, categorize race and ethnicity differently in their records. The large number of patients, and their diverse racial/ethnic make-up are a strength of the study; on the other hand, it may also reveal the limitations of a single-institution study. Anesthesiologists at this institution may be particularly comfortable with care of diverse populations.
Our study also does not identify reasons why regional anesthesia was or was not chosen in different patients undergoing surgery. Reasons for a child not receiving a regional anesthetic include medical concerns, parental refusal, or anesthesiologist or surgeon discretion.24 Although race and ethnicity did not significantly affect the odds of receiving regional anesthesia in our study population, we are unable to determine whether different racial or ethnic groups are offered or refuse regional anesthesia at different rates. Patient refusal may be an important factor in health service delivery: a survey study on acceptance of perioperative epidural analgesia showed African-American race was an independent predictor of refusal of epidural analgesia.25 Higher likelihood of refusal may be related to a history of mistrust in the healthcare system by minority groups, which is well-documented.26 In our subgroup analysis, we observed a non-significant increase in the adjusted odds ratio of black/African-American pediatric patients receiving a regional anesthetic compared to white non-Hispanic patients. It is also possible that our findings are shaped by whether anesthesiologists offered regional anesthesia to each group at similar rates. Identifying ways to improve delivery of regional anesthesia to children has significant clinical implications and is worthy of future study.
The study was adequately powered for the main analysis of white non-Hispanic compared to minority racial and ethnic groups. Comparisons between individual minority racial or ethnic groups had lower power and it is therefore possible that associations exist but have not reached statistical significance in this analysis. We did observe clinically significant signals in individual racial and ethnic groups, most notably an increased adjusted odds of receiving regional anesthesia in black/African-American patients and a decreased adjusted odds in Pacific Islander patients. As such, a future revisiting of this study with another dataset to assess trends over time and with increased power may provide additional insight. Results should be interpreted with caution because of multiple testing. Adjusting for multiple testing would yield even less evidence of statistically significant association.
In order to minimize the number of excluded intraoperative regional anesthetics, we chose to include general anesthetics from all services, including those that infrequently receive regional anesthetics such as gastroenterology and radiation oncology. Although this maximized our total number of regional anesthetics, the technique reduced the overall percentage of patients in the study receiving regional anesthetics. Our sensitivity analyses on urology and orthopedic patients were therefore performed in order to study patients with the highest likelihood of regional anesthetic receipt.
Some data (138 patient cases) were excluded because of missing case Relative Value Unit information, surgery length, or patient disposition. There is no reason to expect missing data on these variables to be related to a patient’s race or ethnicity or to whether they received regional anesthesia, but it is possible bias could be present if it was. One hundred fifty-five cases (15 of which received regional anesthesia) were not analyzed because race and ethnicity were either stated to be unknown or declined to answer. There is potential that this could have introduced bias to the study but given the small numbers the impact should also have been small.
In summary, we present an analysis on the association of race and ethnicity and the utilization of intraoperative regional anesthesia in a dataset of 25,664 pediatric patients at a single, academic children’s hospital. Our results do not demonstrate a significant difference in the adjusted odds of receiving regional anesthesia for white non-Hispanic patients versus other racial and ethnic groups. Further investigation is necessary to determine why differences may be less pronounced in the pediatric than the adult populations, and prospective studies may elucidate whether other factors affect attitudes toward regional anesthesia among healthcare providers, pediatric patients, and parents.
Supplementary Material
Key Points:
Question:
Does race or ethnicity affect the odds of receiving intraoperative regional anesthesia in pediatric patients?
Findings:
In an analysis of 3,189 regional anesthetics in 25,664 surgeries at a single, academic children’s hospital, race and ethnicity affected the probability of receiving intraoperative regional anesthesia, although this association no longer became significant after adjusting for covariates.
Meaning:
While non-significant differences in odds existed for individual groups, our results do not demonstrate a significant difference in the adjusted odds of receiving regional anesthesia for any racial or ethnic group in pediatrics; further study is warranted to consider the possible mechanisms behind our finding, as well as to confirm the findings on a multi-institutional level.
Acknowledgments
Funding Disclosures:
Dr. Rosenbloom’s work was supported by the National Institutes of Health T32 GM007592 grant (Research Training for Anesthetists). All other support was provided from institutional and/or departmental sources.
Prior Presentations: This work was presented in part at the Society for Pediatric Anesthesia-American Academy of Pediatrics Pediatric Anesthesiology meeting in March 2019 in Houston, Texas.
Glossary of Terms
- PACU
post-anesthesia care unit
- SQL
structured query language
- ASA class
American Society of Anesthesiologists physical status classification
- CIs
confidence intervals
- RVUs
Relative Value Units
- ORs
odds ratios
Footnotes
Clinical trial number and registry URL: Not applicable
Conflicts of Interest: All authors declare no competing interests.
Contributor Information
Michael King, Department of Pediatric Anesthesiology, Ann and Robert H. Lurie Children’s Hospital of Chicago and Northwestern University Feinberg School of Medicine, Chicago, IL, United States.
Elizabeth De Souza, Department of Anesthesiology, Perioperative and Pain Medicine, Stanford University School of Medicine, Stanford, CA, United States.
Julia M. Rosenbloom, Department of Anesthesia, Critical Care and Pain Medicine, Massachusetts General Hospital, Harvard Medical School, Boston, MA, United States.
Ellen Wang, Department of Anesthesiology, Perioperative and Pain Medicine, Stanford University School of Medicine, Stanford, CA, United States.
T. Anthony Anderson, Department of Anesthesiology, Perioperative and Pain Medicine, Stanford University School of Medicine, Stanford, CA, United States.
References:
- 1.Smedley BD, Stith AY, Nelson AR, eds. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington DC:NAP; 2003. [PubMed] [Google Scholar]
- 2.National Center for Health Statistics (US). Health, United States, 2015: With Special Feature on Racial and Ethnic Health Disparities. Hyattsville (MD): National Center for Health Statistics (US); 2016 May. [PubMed] [Google Scholar]
- 3.Rasooly IR, Mullins PM, Mazer-Amirshahi M, van den Anker J, Pines JM. The impact of race on analgesia use among pediatric emergency department patients. J Pediatr. 2014;165:618–621. [DOI] [PubMed] [Google Scholar]
- 4.Goyal MK, Kupperman N, Cleary SD, Teach SJ, Chamberlain JM. Racial disparities in pain management of children with appendicitis in emergency rooms. JAMA Pediatr. 2015;169:996–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Johnson TJ, Schultz BR, Guyette FX. Characterizing analgesic use during air medical transport of injured children. Prehosp Emerg Care. 2014;18:531–538. [DOI] [PubMed] [Google Scholar]
- 6.Alegria M, Vallas M, Pumariega AJ. Racial and ethnic disparities in pediatric mental health. Child Adolesc Psychiatr Clin N Am. 2010;19:759–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Squitieri L, Reichert H, Kim HM, Steggerda J, Chung KC. Patterns of surgical care and health disparities of treating pediatric finger amputation injuries in the United States. J Am Coll Surg. 2011;213:475–485. [DOI] [PubMed] [Google Scholar]
- 8.Williams DR and Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32:20–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jimenez N, Seidel K, Martin LD, Rivara FP, Lynn AM. Perioperative analgesic treatment in Latino and non-Latino pediatric patients. J Health Care Poor Underserved. 2010; 21:229–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sadhasivam S, Chidambaran V, Ngamprasertwong P, et al. Race and unequal burden of perioperative pain and opioid related adverse effects in children. Pediatrics. 2012;129:832–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rosenbloom JM, Senthil K, Long AS, et al. A limited evaluation of the association of race and anesthetic medication administration: A single-center experience with appendectomies. Pediatr Anesth. 2017; 27:1142–1147. [DOI] [PubMed] [Google Scholar]
- 12.Nafiu OO, Chimbira WT, Stewart M, Gibbons K, Porter LK, Reynolds PI. Racial differences in the pain management of children recovering from anesthesia. Pediatr Anesth. 2017; 27:760–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Memtsoudis SG, Besculides MC, Swamidoss CP. Do race, gender, and source of payment impact on anesthetic technique for inguinal hernia repair? J Clin Anesth. 2006;18:328–333. [DOI] [PubMed] [Google Scholar]
- 14.Memtsoudis SG, Poeran J, Zubizarreta N, Rasul R, Opperer M, Mazumdar M. Anesthetic care for orthopedic patients: is there a potential for differences in care? Anesthesiology. 2016;124:608–623. [DOI] [PubMed] [Google Scholar]
- 15.Rust G, Nembhard WN, Nichols M, et al. Racial and ethnic disparities in the provision of epidural analgesia to Georgia Medicaid beneficiaries during labor and delivery. Am J Obstet Gynecol. 2004;191:456–462. [DOI] [PubMed] [Google Scholar]
- 16.Glance LG, Wissler R, Glantz C, Osler TM, Mukamel DB, Dick AW. Racial differences in the use of epidural analgesia for labor. Anesthesiology. 2007;106:19–25. [DOI] [PubMed] [Google Scholar]
- 17.Polaner DM, Taenzer AH, Walker BJ, et al. Pediatric Regional Anesthesia Network (PRAN): a multi-institutional study of the use and incidence of complications of pediatric regional anesthesia. Anesth Analg. 2012;115:1353–64. [DOI] [PubMed] [Google Scholar]
- 18.Walker BJ, Long JB, Sathyamoorthy M, et al. Complications in pediatric regional anesthesia: an analysis of more than 100,000 blocks from the pediatric regional anesthesia network. Anesthesiology. 2018;129:721–732. [DOI] [PubMed] [Google Scholar]
- 19.Chou R, Gordon DB, Leon-Casasola OA, et al. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17:131–157. [DOI] [PubMed] [Google Scholar]
- 20.Long DR, Lihn AL, Friedrich S, et al. Association between intraoperative opioid administration and 30-day readmission: a pre-specified analysis of registry data from a healthcare network in New England. Br J Anaesth. 2018;120:1090–1102. [DOI] [PubMed] [Google Scholar]
- 21.Johnson RG, Arozullah AM, Neumayer L, Henderson WG, Hosokawa P, Khuri SF. Multivariable predictors of postoperative respiratory failure after general and vascular surgery: results from the patient safety in surgery study. J Am Coll Surg. 2007;204:1188–1198. [DOI] [PubMed] [Google Scholar]
- 22.Neumayer L, Hosokawa P, Itani K, El-Tamer M, Henderson WG, Khuri SF. Multivariable predictors of postoperative surgical site infection after general and vascular surgery: results from the patient safety in surgery study. J Am Coll Surg. 2007;204:1178–1187. [DOI] [PubMed] [Google Scholar]
- 23.Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav Res Methods. 2009;41:1149–1160. [DOI] [PubMed] [Google Scholar]
- 24.Flack S and Lang RS. Regional anesthesia In: Davis PJ, Cladis FP, eds. Smith’s anesthesia for infants and children, 9th ed. Philadelphia, PA (US): Elsevier Inc.; 2017. p. 461–511. [Google Scholar]
- 25.Ochroch EA, Troxel AB, Frogel JK, Farrar JT. The influence of race and socioeconomic factors on patient acceptance of perioperative epidural analgesia. Anesth Analg. 2007;105:1787–1792. [DOI] [PubMed] [Google Scholar]
- 26.Lillie-Blanton M, Brodie M, Rowland D, Altman D, McIntosh M. Race, ethnicity, and the health care system: public perceptions and experiences. Med Care Res Rev. 2000;57 Suppl 1:218–235. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.