The biggest story in medicine this year is the coronavirus 2019 (COVID-19) pandemic. This disease affects people with diabetes out of proportion to how it affects the general population, as evidenced by higher admissions rates to hospitals among diabetes patients out of proposition.1 Furthermore, hospitalized patients are at greater risk of morbidity and mortality than the general population.2 The angiotensin converting enzyme 2 (ACE2) is the critical receptor for severe acute respiratory syndrome coronavirus and severe acute respiratory syndrome coronavirus 2, also known as COVID-19.3 The localization of ACE2 expression in the endocrine part of the pancreas suggests that COVID-19 also enters islets using ACE2 as its receptor and damages islets causing acute diabetes.4 Because of international shelter-in-place policies due to the COVID-19 pandemic, many people, including patients with diabetes and healthcare professionals, have been staying home most of the time this spring. Accordingly, the pandemic has resulted in a major reorganization throughout the world in how diabetes care is delivered to outpatients.5
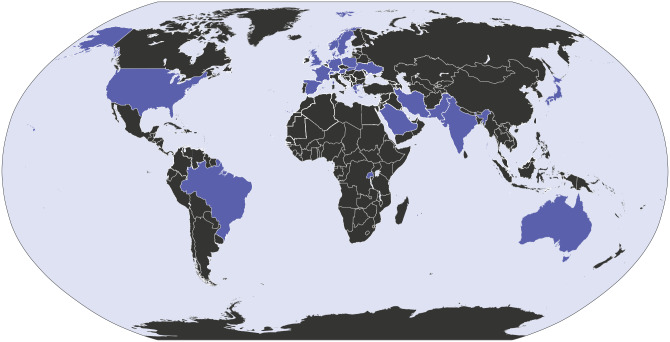
For this issue, Journal of Diabetes Science and Technology (JDST) reached out to 48 diabetes clinicians, scientists, and business people and asked them to write a commentary article on what they have learned from the COVID-19 pandemic and based on this new information, what do they predict for the future. Our authors hail from 23 countries in the six inhabited continents, including North America, South America, Europe, Africa, Asia, and Australia (Figure 1). Their stories and their discussions of what they have learned from the COVID-19 pandemic reflect the common priorities and reactions to social isolation that diabetes clinicians and other experts all over the world have faced this year.
Figure 1.
Countries represented (purple) in the JDST special section on COVID-19 and diabetes.
Ten themes were mentioned repeatedly as predictions for the future triggered by the COVID-19 pandemic. These themes are summarized in Table 1 and are listed here: (1) telemedicine, by way of video or texting software, which has replaced in-person visits in essentially all parts of the word, will continue to be an important tool for care delivery after the pandemic is over and care through virtual diabetes clinics will become routine; (2) insurance coverage policies and regulations that have held back adoption of widespread telemedicine are currently amended and after the pandemic will remain favorable when the state of emergency is over; (3) remote sensors for monitoring glucose, vital signs, geographic location, and specific physiological measurements (eg, foot wound size, physical activity, sleep, and food intake) will become much more widely used to supplement direct visual observations from telemedicine; (4) multiplatform systems to review smart sensor data will be increasingly used and the sensor data will be routinely integrated into the electronic health record; (5) mobile phones and mobile phone apps based on sensor information, providing aggregated data and decision support treatment recommendations, will become even more widely used; (6) many aspects of clinical diabetes research will migrate from being conducted during in-person visits to remote visits via telemedicine; (7) continuous glucose monitoring will become a widely used tool for hospitalized diabetes patients when it is time to perform assisted monitoring of blood glucose even after it is no longer advantageous to decrease nurse contact with patients to minimize use of personal protective equipment and exposure to viruses; (8) public health agencies will be better prepared for the next pandemic than they were for the current one with more available supplies and better plans for sampling and for assaying microbe-associated laboratory tests; (9) remote learning by healthcare professionals and students will become more established, and remote teaching by diabetes educators will become more widely practiced; (10) international cooperation to identify best practices and treatments for our patients will continue or become even more widespread.
Table 1.
Future Predictions in the COVID-19 Special Section on COVID-19 and Diabetes.
| 1. Telemedicine will continue to be important 2. Coverage and regulations will facilitate telemedicine 3. Remote sensors will be used more often 4. Multisensor platforms will be used more often 5. Mobile phones and mobile apps will be used more often 6. Clinical research will become more remote 7. Continuous glucose monitoring in the hospital will become established 8. Public health agencies will be better prepared 9. Remote learning and teaching will become used more often 10. International cooperation will continue |
COVID-19, coronavirus 2019.
This type of issue emphasizing commentaries about a single aspect of diabetes (ie, its relationship to the COVID-19 disease) is a first for JDST. We hope our readers find the personal stories instructive and the future predictions stimulating. We also hope that there will be no reason to publish another such issue in the future related to such a public health crisis as the COVID-19 pandemic.
Footnotes
Abbreviations: ACE2, Angiotensin converting enzyme 2; COVID-19, coronavirus 2019; SARS-CoV, severe acute respiratory syndrome coronavirus; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Declaration of Conflicting Interests: The author declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Riddle MC, Buse JB, Franks PW, et al. COVID-19 in people with diabetes: urgently needed lessons from early reports [published online ahead of print May 14, 2020]. Diabetes Care. doi: 10.2337/dci20-0024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bode B, Garrett V, Messler J, et al. Glycemic characteristics and clinical outcomes of COVID-19 patients hospitalized in the United States. J Diabetes Sci Technol. Diabetes Sci Technol. 92020; 14(4):813-821. doi: 10.1177/193229682092446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Monteil V, Kwon H, Prado P, et al. Inhibition of SARS-CoV-2 infections in engineered human tissues using clinical-grade soluble human ACE2. Cell. 2020;181(4):905-913.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Yang JK, Lin SS, Ji XJ, Guo LM. Binding of SARS coronavirus to its receptor damages islets and causes acute diabetes. Acta Diabetol. 2010;47(3):193-199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382(18):1679-1681. [DOI] [PubMed] [Google Scholar]