Abstract
There is mounting evidence that only a small fraction of early-onset Alzheimer disease cases (onset <65 years) are explained by known mutations. Even multiplex families with early onset often also have late-onset cases, suggesting that the commonly applied categorization of Alzheimer disease into early- and late-onset forms may not reflect distinct underlying etiology. Nevertheless, this categorization continues to govern today's research and the design of clinical trials. The aim of this review is to evaluate this categorization by providing a comprehensive, critical review of reported clinical, neuropathologic, and genomic characteristics of both onset-based subtypes and explore potential overlap between both categories. The article will lay out the need to comprehensively assess the phenotypic, neuropathologic, and molecular variability in Alzheimer disease and identify factors explaining the observed significant variation in onset age in persons with and without known mutations. The article will critically review ongoing large-scale genomic efforts in Alzheimer disease research (e.g., Alzheimer Disease Sequencing Project, Dominantly Inherited Alzheimer Network, Alzheimer Disease Neuroimaging Initiative) and their shortcomings to disentangle the delineation of unexplained nonmendelian early-onset from late-onset and mendelian forms of Alzheimer disease. In addition, it will outline specific approaches including epigenetic research through which a comprehensive characterization of this delineation can be achieved.
Alzheimer disease (AD) is the most common form of dementia accounting for 50%–75% of dementia cases.1 To date, an estimated 5.4 million Americans have AD; this number is projected to quadruple by midcentury, largely driven by population aging. By 2050, it is projected that a new case of AD will develop every 33 seconds on average, resulting in nearly a million new cases each year.1 Overall, the incidence of AD increases exponentially with age, doubling every 5 years after age 65 years, although some individuals, even in multiplex AD families, successfully age without cognitive decline.2,3 Currently, 1 in 9 people aged 65 years and older and 1 in 3 people older than 85 years have the disease. There are no substantially effective therapeutic interventions for AD available.1 Although deaths resulting from heart disease, prostate cancer, and stroke have decreased over the past decade, deaths from AD have increased by 145%, making AD the sixth leading cause of mortality in the United States.1 Total costs for health care, long-term care, and hospice services for people with dementia are expected to increase from approximately $290 billion to date to more than $1.1 trillion by the year 2050. Not accounted for in these numbers are the billions of hours of care provided by unpaid caregivers estimated to be equivalent to nearly $234 billion annually.1
Categorization into early- and late-onset forms of AD
AD is commonly categorized as either early onset (EOAD) or late onset (LOAD) based on an age cutoff, typically 65 years.4,5 This threshold, however, is arbitrary, and a cutoff of 60 years is also commonly used. Of all patients with AD, 5%–10% (corresponding to 220,000–640,000 Americans)6 are attributed to EOAD. Specifically, the 45–64 years age group has a reported annual incidence of 6.3/100,000 and prevalence of 24.2/100,000, with both rates rising exponentially as individuals approach age 65 years.7,8 However, unlike LOAD for which an extensive number of representative data on prevalence and incidence are available, these estimates for EOAD are derived from significantly less data from nationally (and internationally) representative samples, with a paucity of data both within and across ethnic groups. It is possible that the true prevalence and incidence rates for EOAD are higher, in particular for sporadic cases and nonmendelian familial EOAD cases. A substantial portion of those who would meet the diagnostic criteria for AD are not diagnosed by a physician and so underreported.
In general, there are 2 types of inheritance patterns observed in EOAD: mendelian (mEOAD) and nonmendelian (nmEOAD) patterns. mEOAD forms are typically fully penetrant with an autosomal dominant inheritance pattern, most often caused by mutations in APP, PSEN1, and PSEN2 (see Genetics of mEOAD section). Conversely, nmEOAD is often sporadic or with inconsistent inheritance patterns (i.e., inheritance patterns that are not obviously autosomal dominant, or with highly variable age at onset, including LOAD). Although the etiology and genetic basis of nmEOAD are largely unknown, it is generally considered to be multifactorial, with polygenic effects.
Among the scientific literature, the terminology used to describe EOAD and its subtypes is inconsistent. For many EOAD is synonymous with mEOAD, although mEOAD accounts only for approximately 10% of EOAD cases.4,5 Some use the terms familial EOAD or autosomal dominant EOAD to refer to mEOAD. Still others use familial EOAD to refer to any EOAD case with a positive family history (whether autosomal dominant) and sporadic EOAD for cases without a family history. This inconsistency in terminology reflects a lack of understanding of the molecular etiology of EOAD, EOAD subtypes, and their delineation from LOAD. Although there is a general consensus that mEOAD represents a genetic etiology distinct from LOAD, it is less clear if and how nmEOAD is distinct from LOAD. As indicated above, it is generally held that most nmEOAD, both with and without a family history, is predominantly polygenic. Many hypothesize that nmEOAD is simply an extreme phenotype of LOAD that results from an accumulation of variants typically associated with LOAD or the presence of additional genetic or environmental modifying factors lowering onset age (e.g., cerebrovascular disease).4,5 However, there has been little work performed to actually test and verify this hypothesis, posing a critical gap in AD research and our understanding of AD etiology. Clarifying to what extend nmEOAD is clinically and etiologically distinct from mEOAD and LOAD is vital for understanding the molecular mechanisms leading to AD, determining accurate population burden, predicting an individuals' risk, applying appropriate study designs from basic research to clinical trials, and developing personalized and effective targets for prevention and treatment. The purpose of this review is to address this critical gap of knowledge by assessing and summarizing the evidence for differences in etiology between the various presentations of AD and identifying the void that remains in our understanding of these presentations.
Clinical characteristics of EOAD and LOAD
The typical clinical presentation of AD is characterized by predominant impairment of anterograde episodic memory that, as the disease progresses, is accompanied by dysfunction in additional cognitive domains such as visuospatial, language, and executive function, eventually resulting in global cognitive decline, complete dependency, and death. This typical memory-predominant phenotype is observed in most LOAD cases and a large subset of EOAD cases.9 However, roughly 25% of all subjects with EOAD show an atypical clinical presentation that is characterized by preserved episodic memory but focal cortical symptoms, in particular apraxia, visual dysfunction, aphasia, or executive dysfunction.10–12
The clinical characteristics of mEOAD have been researched through projects such as the Dominantly Inherited Alzheimer Network observational study (DIAN-OBS) and other studies.2,13–17 Data from these initiatives suggest that in mEOAD, cognitive symptoms overlap substantially with typical sporadic LOAD symptoms, but usually with a more aggressive disease course with shorter relative survival time.11 Noncognitive clinical manifestations affect a subset of participants with mild to moderate mEOAD.16 The most prevalent nonamnestic cognitive manifestations in participants in the DIAN-OBS cohort are those typical of mild to moderate AD, including visual agnosia (55.1%), aphasia (57.9%), and behavioral changes (61.7%), whereas the prevalence of noncognitive neurologic manifestations was reported to be lower: myoclonus and spasticity (9.3%), seizures (2.8%), and parkinsonism (11.2%). Analyses of published data on subjects with mEOAD yielded a higher prevalence for myoclonus (19.4%), spasticity (15.0%), parkinsonism (12.5%), and seizures (20.3%) but a lower prevalence for nonamnestic cognitive manifestations (e.g., visual agnosia [5.6%], aphasia [23.0%], and behavioral changes [31.7%]).16 Such discrepancies could be due to differences in disease stage, phenotyping, and/or ascertainment protocols between studies. A recent larger prospective cohort study reported that a significant minority (16%) of subjects with mEOAD had nonamnestic cognitive phenotypes, and about 25% had atypical neurologic symptoms in addition to the amnestic phenotype.18 Analyses of clinical presentation based on genetic background suggest that compared with APP carriers, PSEN1 carriers are more likely to exhibit additional neurologic features such as myoclonus, corticobulbar deficits, aphasia, and spasticity but less often ischemic stroke and hemorrhage.16,18 Also, mutation location within the gene could affect the clinical phenotype.18 For instance, most of the APP substitutions at the Aβ sequence lead to mEOAD, whereas the Ala673Thr APP protects against of AD.19
There is a lack of studies assessing the clinical characteristics of nmEOAD as a specific disease entity separate from mEOAD and LOAD. The reported studies were heterogeneous in their design, applied a variety of diagnostic criteria, often did not consider biomarkers, and typically assessed all types of dementia without excluding mEOAD, hindering informed conclusions to be drawn about this form of AD.7 Like mEOAD and LOAD, nmEOAD is typically memory predominant, with nonamnestic symptoms in a subset of the patients. However, data beyond this are limited. It is not clear whether the neuropsychological profile within the memory domain differs from that of mEOAD and LOAD. In addition, the true prevalence of atypical presentations within the nmEOAD category remains unclear, as does the true onset age distribution of both sporadic and familial nmEOAD cases.
Neuropathologic distinction between EOAD and LOAD
AD is neuropathologically characterized by extracellular accumulation of diffuse and neuritic amyloid plaques composed of abnormally folded Aβ40 and Aβ42 generated by cleavage of APP, and intraneuronal accumulation of neurofibrillary tangles (NFTs) composed of hyperphosphorylated tau protein (p-tau). These pathologic features are often accompanied by neuropil threads, dystrophic neurites, associated astrogliosis, microglial activation, and cerebral amyloid angiopathy.20 Furthermore, 50% of patients with AD exhibit concurrent α-synuclein (αSyn) pathology.21,22 Although amyloid deposition does not always follow a fixed pattern of progression, it usually develops in the isocortex and affects subcortical structures later in the disease process. In contrast, tau pathology begins typically in the allocortex of the medial temporal lobe involving the entorhinal cortex and hippocampus.23 In general, Aβ pathology reaches a plateau in the early symptomatic phase of the disease,24 whereas NFT pathology correlates more closely with clinical features, severity, and progression of AD.20 There is, however, a certain degree of disconnect between these neuropathologic changes and clinical symptoms; individuals with a high burden of AD pathology are sometimes without clinical symptoms, and individuals with a significant degree of cognitive impairment sometimes exhibit limited AD pathology.23
To what extent the neuropathology of nmEOAD, mEOAD, and LOAD overlap remains unclear. Compared with older people who often show multiple comorbid pathologies other than AD (e.g., Lewy bodies, TDP-43, or vascular pathology), AD at a younger age tends to be associated with more pure AD pathology.25–27 In line with this notion, a number of studies using MRI and PET scans have reported a larger burden and more widespread pathology with neocortical and subcortical involvement in younger cases, see the section entitled “Brain imaging and biofluid biomarkers” below.10,28–32 The brain pathology of some variant AD cases is characterized by diffuse cotton wool Aβ-plaques without neuritic pathology or neuroinflammation.33 Most of the variant AD cases are PSEN1 carriers often affected by spastic paraparesis.34 However, the cotton wool plaques were also reported in a few LOAD cases, suggesting that this brain pathology is not entirely specific for mEOAD.35 Cotton wool Aβ-plaques might result from an inhibited nucleation stage of fibrillogenesis in the presence of a particular genetic background. Furthermore, there is evidence that different fibril structures of Aβ peptides might underlie different courses and time frames of disease progression.36
A critical shortcoming of most neuropathology studies is the lack of genetic information to distinguish between carriers and noncarriers of causal/risk variants and patterns of inheritance (e.g., mEOAD vs nmEOAD). Recognizing the urgency to better define the pathologic distinction between mEOAD and LOAD, the Alzheimer Disease Neuroimaging Initiative (ADNI)/DIAN Neuropathology Core (NPC) has recently implemented a uniform assessment protocol to evaluate the neuropathologic overlap between these 2 forms.37 As part of this protocol, multiple histologic stains are performed on all brains that include hematoxylin and eosin, a modified Bielschowsky silver impregnation, and immunohistochemistry using the following primary antibodies: phosphorylated tau (PHF1), β-amyloid (10D5; Eli Lilly, Indianapolis, IN), phosphorylated αSyn (Cell Applications, San Diego, CA), and phosphorylated TDP-43 (Cosmo Bio, Carlsbad, CA). NACC operational criteria for the classification of AD and other pathologies are applied, which include diagnosis of AD by several sets of criteria (Khachaturian, CERAD, NIA-Reagan, and the NIA-AA38–40). However, there is no coordinated research effort to evaluate the overlap with nmEOAD.
Brain imaging and biofluid biomarkers
Data on mEOAD from the DIAN study suggest that compared with noncarriers, carriers of causal mutations show reduced cortical glucose metabolism and cortical thinning in the medial and lateral parietal lobes 5–10 years before the estimated age at onset and widely distributed elevated Pittsburgh compound B (PiB) levels in nearly every cortical region approximately 15 years before estimated onset.41 Subcortical regions seem to show a disparate pattern, with all subcortical gray matter regions exhibiting elevated PiB uptake, but reduced glucose metabolism being apparent only in the hippocampus.41 Atrophy in mEOAD is observed early, both in areas commonly associated with sporadic LOAD and additional areas including the putamen and thalamus, which are associated with early amyloid deposition in mEOAD.42 Tau tracer binding in the neocortex is also increased in symptomatic mutation carriers compared with sporadic LOAD43; however, it remains to be clarified which component of tauopathy (e.g., NFT, neuritic plaques, or neuropil threads) is reflected by this increased PET-tau signal.
Longitudinal analyses in the DIAN study17 aim to pinpoint onset, sequence, and rate of progression of biomarker and clinical measures across the spectrum of mEOAD. The results from this study suggest that β-amyloid measured in CSF change first, decades before estimated symptom onset, followed by declines in measures of cortical metabolism approximately 7–10 years later, then cognition and hippocampal atrophy (approximately 2 decades after changes in β-amyloid). CSF p-tau181 showed a marked decline near symptom onset; this is in contrast with previous observations from cross-sectional analyses, which suggested a continued elevation of CSF p-tau181. There is also evidence that CSF αSyn levels are linked to onset of cognitive symptoms in both sporadic LOAD and mEOAD22 and that CSF progranulin, encoded by GRN, increases over the course of disease and is associated with sTREM2, neurodegeneration, and cognitive decline.44
Studies in subjects with nmEOAD without AD family history have also shown more atrophy,45 more prominent neocortical glucose hypometabolism,46 and increased tau PET uptake47,48 relative to LOAD. This is in line with findings at brain autopsy, indicating that neurodegeneration and tauopathy are more aggressive at a younger onset, but the number of studies is limited. Even more limited is the availability of longitudinal imaging and biomarker data sets of nmEOAD multiplex families and direct comparison with the mendelian form of EOAD. Analyses of the ADNI data set (unrelated ≥65-year-old subjects) applying linear mixed-effects models also demonstrate that LOAD defined by MRI and biofluid-based biomarkers proceeds more aggressively among younger than older elderly individuals.49 Specifically, this study suggests that brain atrophy rates in AD (and mild cognitive impairment) are stronger with younger baseline age. Conversely, atrophy rates for clinically normal older individuals remain constant or exhibit a slight increase with age (slopes [% atrophy/year2] ranged from −0.04 to 0.006 and was only significant for the hippocampus [slope: −0.04; p = 0.004]).49 Similarly, younger individuals with AD or mild cognitive impairment exhibit a greater CSF biomarker burden, whereas among healthy controls, biomarker burden increases with age. In addition, AD cases show reduced rates of cognitive decline with increasing baseline age.49 Together, these data support the notion of a disease continuum across the age range in LOAD, up to a blurring of the distinction between AD and healthy controls older than 85 years.49 However, whether this continuum truly extends to the younger age range and nmEOAD remains to be assessed.
Efforts to develop reliable, sensitive, and specific biomarkers of blood-based biomarkers for AD (e.g., plasma or serum) have been hampered by various challenges, in particular much lower amounts of molecules of interest in the bloodstream compared with the CSF and high levels of other proteins from peripheral organs in the blood and presence of proteases that degrade brain proteins. However, in recent years, there have been significant advances in the development of highly sensitive assays to assess plasma levels of molecules that could serve as biomarkers of AD and other types of neurodegeneration for diagnosis, prognosis, and disease progression monitoring.50,51 Various studies have shown that the ratio of plasma Aβ42/40 measured by these ultrasensitive assays such as the single-molecule array method provides a sensitive and reliable measure of amyloid status that predicts future conversion to positive amyloid PET independent of the time of day and correlates with CSF Aβ42/40 in both mEOAD and LOAD.52–55 In addition, neurofilament light chain (NFL), an intraneuronal component of the axonal cytoskeleton reflecting neuronal damage and degeneration, increases in the CSF in early stages of the disease. Also, NFL increases over time as cognition declines and atrophy and white matter changes increase. NFL has diagnostic accuracy for AD dementia similar to that of CSF biomarkers in subjects with both forms of disease,56,57 and studies in individuals with mEOAD, including the DIAN study, suggest that plasma NFL increases several years before symptom onset, indicating its utility as a screening tool in this type of AD.58–60 However, there is a lack of data specifically assessing NFL association in nmEOAD. Current data are less supportive of the use of plasma tau as a useful biomarker for AD, although p-tau181 levels are elevated in AD dementia and show associations with both Aβ and tau PET, suggesting greater specificity for AD pathology than other tau species.e-1
Genetics of mEOAD
Heritability
Although LOAD is a complex disorder with a strong genetic component (heritability of 70%–80%),4,e-2 EOAD in general has an even stronger heritability estimated between 92% and 100%.4 This is in line with the observation that up to 60% of patients with EOAD have at least 1 affected first-degree relative.e-3,e-4
Genetics of mEOAD
Known mEOAD results from 1 copy of a mutant allele in APP,e-5 PSEN1,e-6 or PSEN2e-7,e-8; in total, ∼330 mutations in these genes have been reported (alzforum.org/alzgene), accounting for 10%–15%, 30%–70%, and <5% of mEOAD cases, respectively.e-9 However, overall variation in these genes explains only 10%–15% of all patients with familial EOAD.e-4 Mutations in APP, PSEN1, and PSEN2 affect the amyloidogenic pathway leading to increased generation/aggregation of Aβ.e-10,e-11 APP undergoes cleavage by β- and subsequently γ-secretase generating Aβ peptides; and PSEN1 or PSEN2 are components of the γ-secretase complex.e-12 Known pathogenic APP missense substitutions are clustered at the Aβ sequence and linked to higher Aβ production or aggregation, similar to APP duplications.e-13 In contrast, the protective Icelandic APP substitution (Ala673Thr) decreases Aβ levels by 40%.19 Notably, a mutation at the same codon (Ala673Val) causes AD, but only in a recessive mode.e-14 The brain pathology of APP carriers is often accompanied by a significant level of cerebral amyloid angiopathy, which can lead to cerebral hemorrhage and stroke in carriers of APP duplicationse-15,e-16 or some substitutions (e.g., Glu693Glne-5 and Glu693Lyse-17). However, some of the APP mutations (e.g., Glu693Glye-18) were reported in patients without the severe amyloid angiopathy.
In contrast to APP, mutations in PSEN1 or PSEN2 are broadly distributed throughout the gene (alzforum.org/alzgene). Most of them are missense variants with a few in-frame deletions/insertions.33,e-19,e-20 Despite considerable sequence, structural, and functional similarities, many more pathogenic mutations were reported in PSEN1 (n = 263) than PSEN2 (n = 12). PSEN1-related disease is also more severe with onset as early as the third decade (e.g., in Ser170Phe carriers),e-21 whereas some PSEN2 mutations cause LOAD (e.g., Val148Ile).e-22 This discrepancy might be explained by the fact that brain expression of PSEN2 is up to 10 times lower than PSEN1 (FANTOM5 data set; proteinatlas.org/).
Phenotypic variability in PSEN1 patients includes frontotemporal dementia (FTD), Pick-type tauopathy,e-23,e-24 primary progressive aphasia, spinocerebellar ataxia,e-25,e-26 Lewy body dementia,e-27 and variant AD accompanied by spastic paraparesis.34 Even within a family, phenotypes of PSEN1 carriers can appear as variant AD, pure EOAD, or pure spastic paraparesis,e-28 suggesting the action of genetic modifier(s).
Genes modifying age at onset in mEOAD
In general, age at onset of AD is a substantially heritable trait; however, with increasing age at onset, the heritability of AD declines, implying an increased environmental contribution to AD at older ages.4 Even within families, carriers of the same APP, PSEN1, or PSEN2 variant can present with significant variability in age at onset and disease course. A meta-analysis of 387 mEOAD pedigrees showed that the observed variance could only be partially explained by family history, the mutated genes, and the mutation type.e-29
The APOE ε4 allele, the major genetic risk factor identified for LOAD, decreases age at onset of AD in a dose-dependent manner.e-30 In contrast to fully penetrant mEOAD mutations, the APOE ε4 allele is neither necessary nor sufficient to cause AD. However, a more recent study suggested that the effect of APOE on AD risk is consistent with semidominant inheritance of a moderately penetrant gene.e-31 Furthermore, several studies showed that APOE has an age at onset–modifying effect in carriers of some causal mutations (e.g., APP Val717Ile,e-32 PSEN1 Glu280Ala,e-33,e-34 PSEN1 Glu318Gly,e-35 and PSEN2 Asn141Ilee-36).
However, the wide range of onset age in carriers of the PSEN1 Glu206Ala mutation (found in 42% of EOAD families of Caribbean Hispanic origine-37) is not explained by the APOE ε4 allelee-29 nor any antecedent environmental, health-related, or social factors.e-38 Investigation of Glu206Ala carriers and other common founder mutations (e.g., PSEN1 Ala431Glu in Mexicans) can facilitate the search of novel age at onset modifiers.e-39,e-40 For instance, genome-wide linkage analyses of Volga German families segregating the PSEN2 Asn141Ile mutation identified 3 genetic loci (1q23.3, 17p13.2, and 7q33)e-41 potentially harboring onset-modifying genes. Whole-genome sequencing analyses of a large Colombian kindred with the PSEN1 Glu280Ala mutation identified a protective haplotype spanning several cytokine genes on chromosome 17 that delayed AD onset by approximately 10 years.e-42 Intriguingly, a separate study in this kindred identified a carrier of the Glu280Ala variant who developed mild cognitive impairment only in the seventh decade, which is ∼30 years later than the median age at onset in the kindred.e-43 The patient had very high brain amyloid, but limited neurodegeneration and tau pathology. Whole-exome sequencing identified a homozygous Arg136Ser mutation in APOE that was previously associated with hyperlipoproteinemia type III, suggesting that this rare APOE variant is protective and in a homozygous state may reduce tau pathology and neurodegeneration.e-43
Genetics of LOAD
Over the past decade, large-scale genome-wide association study (GWAS) and whole-genome/exome sequencing have identified over 30 genome-wide significant common variant signals in addition to APOE that influence risk for LOAD.e-44–e-51 These variants mostly point to specific pathways (e.g., lipid metabolism, endocytosis/intracellular trafficking, inflammation, immune response, synaptic function, and transcription) indicating a major role for these pathways in the development of LOAD. Although risk variants in genes involved in tau and APP metabolism (PSEN1, PSEN2, APP, ADAM10, ADAMTS1, MAPT),e-52–e-54 as well as in genes of other dementing disorders (e.g., GRN, ARSA, CSF1R) were also implicated.e-55 Taken together with the fact that some families carrying APP, PSEN1, or PSEN2 mutations present with LOADe-52 strongly corroborates the notion that these pathways are not restricted to mEOAD and that there is etiologic overlap between the forms commonly classified as EOAD and LOAD.
In addition, some of the known LOAD loci might be age at onset modifiers in EOAD. For instance, analysis of the ABCA7 coding sequence showed a 5-fold enrichment of premature termination codon mutations in patients with EOAD (n = 928) vs controls (n = 980). Of 17 observed mutations, 10 were novel and only observed in patients.e-56 Furthermore, although common variants in SORL1 were first linked to LOAD with an odds ratio of ∼1.2,e-57,e-58 rare truncating SORL1 mutations with odds ratios up to 12 are seen in EOAD cases and might need to be considered in clinical practice in addition to PSEN1, PSEN2, and APP.e-59 Overall, the risk variants identified to date account for ∼31% of the genetic variance of LOAD,e-44 leaving the majority of genetic risk as yet uncharacterized.
Genetics of nmEOAD
Considering that (1) EOAD is almost entirely genetically determined4; (2) 35%–60% of patients with EOAD have at least 1 affected first-degree relativee-3,e-4,e-60; and (3) known causal mutations account for less than 10% of EOAD cases, it is clear that there are unidentified genetic variation(s) with a substantial effect on nmEOAD risk and/or age at onset. The fact that the concordance between the parent and the offspring in nmEOAD cases is lower than 50% but higher than 2.5%4 indicates that this form of EOAD rather represents a complex disease with the genetic component made up of a significant number of both rare and common variants. In addition, part of the missing heritability of nmEOAD can be hidden within poorly investigated mutation types, such as copy number variations (CNVs). In general, only a limited number of AD studies have investigated the role of CNVs and other structural variants.e-61 An 18-kb insertion in CR1 (responsible for the CR1-S isoform with an allelic frequency of 15% resulting in an extra set of C3b/C4b binding sites) increases AD risk 2-fold and explains the GWAS signals at the CR1 locus.e-62 A 44-base pair frameshift deletion in ABCA7 increases AD risk in African Americans and Caribbean Hispanics.e-49
A study of 261 nonmendelian families with at least 1 EOAD case revealed 5 deletions and 5 duplications that segregated with dementia,e-63 with 2 CNVs encompassing FTD genes (deletion of CHMP2B and duplication of MAPT). A recent analysis of Caribbean Hispanic families multiplex for EOAD not explained by APP, PSEN1, or PSEN2 mutations,e-64 identified 8 regions previously associated with the late-onset form, and several novel linkage regions previously not reported in LOAD subjects (2p15, 5q14.1, 11p15.1, 13q21.22, 13q33.1, 16p12.1, 20p12.1, and 20q11.21). This is in line with the notion that the genetic architectures of nmEOAD and LOAD overlap partially, but not fully.
Role of epigenetic changes
The role of epigenetic modifiers in AD is largely unknown; however, both environmental and genetic age at onset modifiers could act through epigenetic changes, such as DNA methylation (DNAm) at specific cytosine-phosphate-guanine (CpG) sites, one of the key epigenetic modifications. The Exome Aggregation Consortium revealed that CpGs are the most highly mutable sites in the human genome, likely because methyl-C can spontaneously deaminate to T, leading to C>T or G>A transitions on sense or antisense DNA strands.e-65 As a result, the frequency of CpGs in the genome is 25% less than expected and 35% of all coding mutations occur at CpG sites. The fact that DNAm levels are under strong genetic control is evident by very similar genome-wide DNAm profiles in identical twins or triplets vs fraternal siblings.e-66,e-67 Hence, studies of crosstalk between genetic and epigenetic markers are of significant value. For instance, the analysis of genetic variations controlling the gain or loss of CpG sites could reveal the functional disease–related CpG single nucleotide polymorphisms responsible for DNAm changes. Such a study design reduces the likelihood of false-negative results due to excessive correction for multiple testing used in classic GWAS.e-68
Aging, the strongest risk factor for AD, is closely linked to DNAm. It is clear that aging processes are not sufficiently represented by chronological aging. In contrast to the steady pace of chronological age, the pace of biological age varies among individuals and may be linked with different aspects of aging via age-related CpGs. In the genomic research field, both the number of different DNAm clocks (based on specific GpG sets) and the methodological approaches to assess these clocks are rising due to their potential in predicting health span.e-69 It would be important to establish the age-related expression pattern of genes corresponding to clock-building CpGs. The CpGs of the reported DNAm clocks are mapped to 1,633 different genes, including 106 of that are genetically associated with neurodegenerative diseases, as well as 32 genes involved in the amyloid biological network (e.g., BACE1 and PSEN1).e-69
The Horvath's DNAm clock outperforms others based on its multitissue applicability and may reflect biological aging.e-70 It is an accurate age predictor across different tissues (r = 0.96), including blood and brain, and is based on cumulative assessment ∼350 CpGs (available on genome-wide DNAm arrays), which are hyper- or hypomethylated with age and mainly mapped to genes involved in development, cell death, and survival.e-70
DNAm-age acceleration (DNAm-age minus chronological age) has been found to be significantly associated with several neurodegenerative diseases including Parkinson disease,e-71 Huntington disease,e-72 and amyotrophic lateral sclerosis with or without symptoms of FTD.e-73,e-74 The limited data on DNAm-age in AD suggest that DNAm-age acceleration is a significant predictor of dementiae-75 and correlates with degree of amyloid pathology in AD.e-76 We recently investigated a unique Ashkenazi Jewish family with monozygotic triplets affected by LOAD, whereas one of their offspring developed EOAD at age 50 years. Notably, DNAm-age of the triplets was 6–10 years younger than chronological age, but it was 9 years older in the offspring with EOAD, suggesting accelerated aging.e-66 It is not clear whether DNAm-age reacts to aging or causes aging; however, the longitudinal study of identical twins revealed that the asymptomatic twins had aged slower than the affected twins, supporting the latter notion.e-67 Comprehensive characterization of the association of DNAm-age acceleration with AD onset can provide critical information on the distinction between nmEOAD, mEOAD, and LOAD.
What is lacking in our understanding of the clinical, neuropathologic, and genetic delineation of nmEOAD from mEOAD and LOAD?
There remain critical gaps that need to be addressed to disentangle the etiologic and clinical delineations between nmEOAD, mEOAD, and LOAD. Foremostly, there has been a critical lack of longitudinal well-phenotyped data sets of nmEOAD cases and multiplex families, with standardized definition and methodology, in different disease stages, and of different ancestries with clinical, biofluid, neuropathologic, and genomic information. Although some existing EOAD cohorts might harbor nmEOAD cases, emphasis has mostly been put on individuals screening positive for genetic variants. For many data sets, it remains unclear if and how many subjects without known mutations there are and what their clinical biomarker and neuropathologic expression is. Studies specifically sampling nmEOAD cases would allow comprehensive examination of population risk across ethnic groups, longitudinal changes in biomarkers/neuropathology over the disease course, prevalence of atypical nonamnestic and neurologic manifestations, and tease apart clinical, neuropathologic, and genetic overlap with mEOAD and LOAD, and among sporadic and familial forms.
Second, pinpointing the significant proportion of missing heritability will require large sets of well-phenotyped family-based and case-control studies of nmEOAD cases with sufficient statistical power. Investigation of all types of genetic variation including structural, synonymous, and rare variations, examination of all possible inheritance modes, and comprehensive study of epigenetic changes is needed. Integration of sequencing with data derived from other -omics approaches (e.g., transcriptomics, epigenomics, proteomics, and metabolomics) coupled with advanced bioinformatics will be critical to pinpoint the functional allelic effectors of identified loci, define and understand the cellular expression of disease, characterize determinants and mechanisms of disease progression, and clarify the distinction of disease subtypes.
In-depth genetic studies in additional mEOAD and nmEOAD kindreds displaying a marked discrepancy in age at onset between family members will also be highly valuable to disentangle the etiology of differences in age at onset. It has become clear that the location of pathogenic variants within causal genes can affect pathophysiology and age at onset, as has been established for variation in PSEN1 pre- and postcodon 200.16,e-77 However, there are limited data of differential effects of variant location within any other AD genes on age at onset and phenotypic variability, incomplete understanding of the biochemical features of the AD-associated gene domains, and a lack of knowledge on local genetic ancestry at these loci. As has been recently demonstrated for the APOE locus, examination of local ancestry can identify novel ancestry-specific disease loci and help disentangle the factors underlying observed differential genome-phenome associations including variability in age at onset.e-78
For both mEOAD and nmEOAD, there is a lack of data comprehensively assessing the effect of APOE and other established AD variants on age at onset and clinical variability in mutation carriers, and a lack of data incorporating genomic information and neuropathologic features, changes in biomarker sequence and progression of symptoms. Assessing neuropathologic, biofluid, and brain imaging measures across the disease course informed by genetic background is critical to disentangle the clinical delineation of AD subtypes associated with specific variants. As described above, the ADNI/DIAN NPC has implemented a uniform assessment protocol to evaluate the neuropathologic overlap between mEOAD and LOAD.37 Similar collections of nmEOAD brain tissue with standardized neuropathologic assessment are needed to comprehensively delineate neuropathologic overlap of both these forms with sporadic and familial nmEOAD informed by genetic background, acknowledging that—given that pathology is confounded with disease onset, progress, and age at death—differentiation of mEOAD, nmEOAD, and LOAD based on neuropathologic profile is inherently limited.
Conclusions
Facilitated by substantial advances in genomic technologies and bioinformatics, the past decade has brought significant breakthroughs in our understanding of the genetic etiology and molecular mechanisms underlying AD. In addition to the known EOAD genes and APOE, we have now identified over 30 loci that modify disease susceptibility. These loci robustly implicate specific molecular pathways (e.g., immune response, lipid metabolism, and endocytosis) and have advanced our understanding of the disease mechanisms at play. However, significantly lacking is the understanding of genetic, clinical, and neuropathologic delineation of nmEOAD from mEOAD and LOAD. In-depth characterization of the distinction between these forms is critical to fully understand the etiology of AD, risk factors, and clinical determinants of age at onset, inform clinical trials aiming to reposition existing drugs, and develop more effective novel preventive and therapeutic measures advancing the field toward our vision of personalized medicine.
It is possible to fill the research gaps in our understanding of nmEOAD. Although nmEOAD is less common than LOAD, collection and assessment of participants with nmEOAD is quite feasible. Given the severity of the disease, patients are often enthusiastic to participate in clinical research studies. Such participants present at Alzheimer Disease Centers and other memory clinics with regularity, although follow-up and participation in biomarker and genetic studies are inconsistent. Indeed, there are now novel ongoing efforts to address these issues. Two such studies include efforts out of the Alzheimer Disease Genetics Consortium (ADGC) and the Resource for Early-onset Alzheimer Disease Research (READR). The ADGC and READR have novel whole-genome sequencing studies of well-phenotyped EOAD participants lacking known mutation (ADGC focusing on singleton/sporadic and READR focusing on families). It is expected that these studies will identify novel variants and molecular pathways associated with nmEOAD in different ethnic groups and help delineate the etiology of this form of AD from mEOAD and LOAD genetically and clinically.
Glossary
- αSyn
α-synuclein
- AD
Alzheimer disease
- ADGC
Alzheimer Disease Genetics Consortium
- ADNI
Alzheimer Disease Neuroimaging Initiative
- CNV
copy number variation
- CpG
cytosine-phosphate-guanine
- DIAN-OBS
Dominantly Inherited Alzheimer Network observational study
- DNAm
DNA methylation
- EOAD
early-onset AD
- FTD
frontotemporal dementia
- GWAS
genome-wide association study
- LOAD
late-onset AD
- mEOAD
mendelian EOAD
- NFL
neurofilament light chain
- NFT
neurofibrillary tangle
- nmEOD
nonmendelian EOAD
- NPC
Neuropathology Core
- PiB
Pittsburgh compound B
- READR
Resource for Early-onset Alzheimer Disease Research
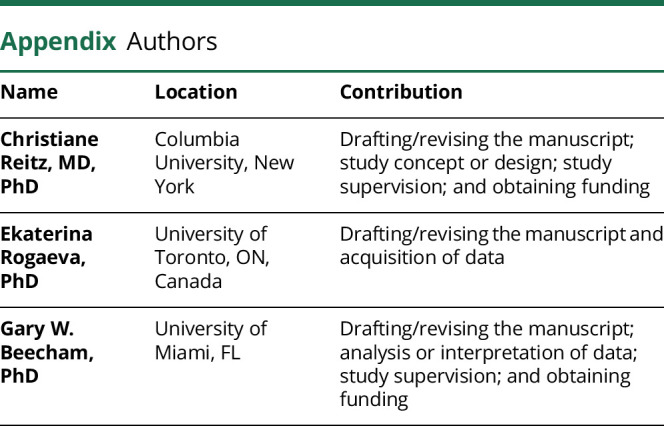
Appendix. Authors
Study funding
This work was in part supported by NIH grants RF1AG054080 (C.R., G.W.B., E.R.), R01AG064614 (C.R., G.W.B.), U01AG052410 (C.R.), P50AG008702 (C.R.), U01AG052410 (G.W.B.), and RF1AG054074 (G.W.B.). E. Rogaeva was further supported by the Canadian Consortium on Neurodegeneration in Aging.
Disclosure
The authors report no disclosures relevant to the manuscript. Go to Neurology.org/NG for full disclosures.
References
- 1.Alzheimer's Association. 2019 Alzheimer's disease facts and figures. Alzheimers Dement 2019;15:321–387. [Google Scholar]
- 2.Bateman RJ, Xiong C, Benzinger TL, et al. Clinical and biomarker changes in dominantly inherited Alzheimer's disease. N Engl J Med 2012;367:795–804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kukull WA, Higdon R, Bowen JD, et al. Dementia and Alzheimer disease incidence: a prospective cohort study. Arch Neurol 2002;59:1737–1746. [DOI] [PubMed] [Google Scholar]
- 4.Wingo TS, Lah JJ, Levey AI, Cutler DJ. Autosomal recessive causes likely in early-onset Alzheimer disease. Arch Neurol 2012;69:59–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barber IS, Braae A, Clement N, et al. Mutation analysis of sporadic early-onset Alzheimer's disease using the NeuroX array. Neurobiol Aging 2017;49:215.e211–215.e218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alzheimer's A. Early-Onset Dementia: A National Challenge, a Future Crisis. Washington, DC: Alzheimer's Association; 2006. [Google Scholar]
- 7.Lambert MA, Bickel H, Prince M, et al. Estimating the burden of early onset dementia; systematic review of disease prevalence. Eur J Neurol 2014;21:563–569. [DOI] [PubMed] [Google Scholar]
- 8.Renvoize E, Hanson M, Dale M. Prevalence and causes of young onset dementia in an English health district. Int J Geriatr Psychiatry 2011;26:106–107. [DOI] [PubMed] [Google Scholar]
- 9.Dubois B, Feldman HH, Jacova C, et al. Advancing research diagnostic criteria for Alzheimer's disease: the IWG-2 criteria. Lancet Neurol 2014;13:614–629. [DOI] [PubMed] [Google Scholar]
- 10.van der Flier WM, Pijnenburg YA, Fox NC, Scheltens P. Early-onset versus late-onset Alzheimer's disease: the case of the missing APOE varepsilon4 allele. Lancet Neurol 2011;10:280–288. [DOI] [PubMed] [Google Scholar]
- 11.Bateman RJ, Aisen PS, De Strooper B, et al. Autosomal-dominant Alzheimer's disease: a review and proposal for the prevention of Alzheimer's disease. Alzheimers Res Ther 2011;3:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ryan NS, Rossor MN. Correlating familial Alzheimer's disease gene mutations with clinical phenotype. Biomark Med 2010;4:99–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wattmo C, Wallin AK. Early- versus late-onset Alzheimer's disease in clinical practice: cognitive and global outcomes over 3 years. Alzheimers Res Ther 2017;9:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koedam EL, Pijnenburg YA, Deeg DJ, et al. Early-onset dementia is associated with higher mortality. Dement Geriatr Cogn Disord 2008;26:147–152. [DOI] [PubMed] [Google Scholar]
- 15.Stanley K, Walker Z. Do patients with young onset Alzheimer's disease deteriorate faster than those with late onset Alzheimer's disease? A review of the literature. Int Psychogeriatr 2014;26:1945–1953. [DOI] [PubMed] [Google Scholar]
- 16.Tang M, Ryman DC, McDade E, et al. Neurological manifestations of autosomal dominant familial Alzheimer's disease: a comparison of the published literature with the Dominantly Inherited Alzheimer Network observational study (DIAN-OBS). Lancet Neurol 2016;15:1317–1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McDade E, Wang G, Gordon BA, et al. Longitudinal cognitive and biomarker changes in dominantly inherited Alzheimer disease. Neurology 2018;91:e1295-e1306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ryan NS, Nicholas JM, Weston PSJ, et al. Clinical phenotype and genetic associations in autosomal dominant familial Alzheimer's disease: a case series. Lancet Neurol 2016;15:1326–1335. [DOI] [PubMed] [Google Scholar]
- 19.Jonsson T, Atwal JK, Steinberg S, et al. A mutation in APP protects against Alzheimer's disease and age-related cognitive decline. Nature 2012;488:96–99. [DOI] [PubMed] [Google Scholar]
- 20.Serrano-Pozo A, Frosch MP, Masliah E, Hyman BT. Neuropathological alterations in Alzheimer disease. Cold Spring Harb Perspect Med 2011;1:a006189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Arai Y, Yamazaki M, Mori O, Muramatsu H, Asano G, Katayama Y. Alpha-synuclein-positive structures in cases with sporadic Alzheimer's disease: morphology and its relationship to tau aggregation. Brain Res 2001;888:287–296. [DOI] [PubMed] [Google Scholar]
- 22.Twohig D, Rodriguez-Vieitez E, Sando SB, et al. The relevance of cerebrospinal fluid alpha-synuclein levels to sporadic and familial Alzheimer's disease. Acta Neuropathol Commun 2018;6:130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hyman BT, Phelps CH, Beach TG, et al. National Institute on Aging-Alzheimer's Association guidelines for the neuropathologic assessment of Alzheimer's disease. Alzheimers Dement 2012;8:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ingelsson M, Fukumoto H, Newell KL, et al. Early Abeta accumulation and progressive synaptic loss, gliosis, and tangle formation in AD brain. Neurology 2004;62:925–931. [DOI] [PubMed] [Google Scholar]
- 25.Savva GM, Wharton SB, Ince PG, et al. Age, neuropathology, and dementia. N Engl J Med 2009;360:2302–2309. [DOI] [PubMed] [Google Scholar]
- 26.Middleton LE, Grinberg LT, Miller B, Kawas C, Yaffe K. Neuropathologic features associated with Alzheimer disease diagnosis: age matters. Neurology 2011;77:1737–1744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Haroutunian V, Schnaider-Beeri M, Schmeidler J, et al. Role of the neuropathology of Alzheimer disease in dementia in the oldest-old. Arch Neurol 2008;65:1211–1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marshall GA, Fairbanks LA, Tekin S, Vinters HV, Cummings JL. Early-onset Alzheimer's disease is associated with greater pathologic burden. J Geriatr Psychiatry Neurol 2007;20:29–33. [DOI] [PubMed] [Google Scholar]
- 29.Scholl M, Ossenkoppele R, Strandberg O, et al. Distinct 18F-AV-1451 tau PET retention patterns in early- and late-onset Alzheimer's disease. Brain 2017;140:2286–2294. [DOI] [PubMed] [Google Scholar]
- 30.Youn YC, Jang JW, Han SH, et al. (11)C-PIB PET imaging reveals that amyloid deposition in cases with early-onset Alzheimer's disease in the absence of known mutations retains higher levels of PIB in the basal ganglia. Clin Interv Aging 2017;12:1041–1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hirano S, Shinotoh H, Shimada H, et al. Voxel-based acetylcholinesterase PET study in early and late onset Alzheimer's disease. J Alzheimers Dis 2018;62:1539–1548. [DOI] [PubMed] [Google Scholar]
- 32.Lowe VJ, Wiste HJ, Senjem ML, et al. Widespread brain tau and its association with ageing, Braak stage and Alzheimer's dementia. Brain 2018;141:271–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Crook R, Verkkoniemi A, Perez-Tur J, et al. A variant of Alzheimer's disease with spastic paraparesis and unusual plaques due to deletion of exon 9 of presenilin 1. Nat Med 1998;4:452–455. [DOI] [PubMed] [Google Scholar]
- 34.Rogaeva E. The solved and unsolved mysteries of the genetics of early-onset Alzheimer's disease. Neuromolecular Med 2002;2:1–10. [DOI] [PubMed] [Google Scholar]
- 35.Le TV, Crook R, Hardy J, Dickson DW. Cotton wool plaques in non-familial late-onset Alzheimer disease. J Neuropathol Exp Neurol 2001;60:1051–1061. [DOI] [PubMed] [Google Scholar]
- 36.Qiang W, Yau WM, Lu JX, Collinge J, Tycko R. Structural variation in amyloid-beta fibrils from Alzheimer's disease clinical subtypes. Nature 2017;541:217–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cairns NJ, Perrin RJ, Franklin EE, et al. Neuropathologic assessment of participants in two multi-center longitudinal observational studies: the Alzheimer Disease Neuroimaging Initiative (ADNI) and the Dominantly Inherited Alzheimer Network (DIAN). Neuropathology 2015;35:390–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Consensus recommendations for the postmortem diagnosis of Alzheimer's disease. The National Institute on Aging, and Reagan Institute Working Group on diagnostic criteria for the neuropathological assessment of Alzheimer's disease. Neurobiol Aging 1997;18:S1–S2. [PubMed] [Google Scholar]
- 39.Mirra SS. The CERAD neuropathology protocol and consensus recommendations for the postmortem diagnosis of Alzheimer's disease: a commentary. Neurobiol Aging 1997;18:S91–S94. [DOI] [PubMed] [Google Scholar]
- 40.Khachaturian ZS. Diagnosis of Alzheimer's disease. Arch Neurol 1985;42:1097–1105. [DOI] [PubMed] [Google Scholar]
- 41.Benzinger TL, Blazey T, Jack CR Jr, et al. Regional variability of imaging biomarkers in autosomal dominant Alzheimer's disease. Proc Natl Acad Sci USA 2013;110:E4502–E4509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Knight WD, Okello AA, Ryan NS, et al. Carbon-11-Pittsburgh compound B positron emission tomography imaging of amyloid deposition in presenilin 1 mutation carriers. Brain 2011;134:293–300. [DOI] [PubMed] [Google Scholar]
- 43.Gordon BA, Blazey TM, Christensen J, et al. Tau PET in autosomal dominant Alzheimer's disease: relationship with cognition, dementia and other biomarkers. Brain 2019;142:1063–1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Suarez-Calvet M, Capell A, Araque Caballero MA, et al. CSF progranulin increases in the course of Alzheimer's disease and is associated with sTREM2, neurodegeneration and cognitive decline. EMBO Mol Med 2018;10:e9712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Moller C, Vrenken H, Jiskoot L, et al. Different patterns of gray matter atrophy in early- and late-onset Alzheimer's disease. Neurobiol Aging 2013;34:2014–2022. [DOI] [PubMed] [Google Scholar]
- 46.Rabinovici GD, Furst AJ, Alkalay A, et al. Increased metabolic vulnerability in early-onset Alzheimer's disease is not related to amyloid burden. Brain 2010;133:512–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cho H, Choi JY, Lee SH, et al. Excessive tau accumulation in the parieto-occipital cortex characterizes early-onset Alzheimer's disease. Neurobiol Aging 2017;53:103–111. [DOI] [PubMed] [Google Scholar]
- 48.Schöll M, Ossenkoppele R, Strandberg O, et al. Distinct 18F-AV-1451 tau PET retention patterns in early- and late-onset Alzheimer's disease. Brain 2017;140:2286–2294. [DOI] [PubMed] [Google Scholar]
- 49.Holland D, Desikan RS, Dale AM, McEvoy LK; Alzheimer's Disease Neuroimaging Initiative. Rates of decline in Alzheimer disease decrease with age. PLoS One 2012;7:e42325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Shi L, Baird AL, Westwood S, et al. A decade of blood biomarkers for Alzheimer's disease research: an evolving field, improving study designs, and the challenge of replication. J Alzheimers Dis 2018;62:1181–1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hampel H, Vergallo A, Afshar M, et al. Blood-based systems biology biomarkers for next-generation clinical trials in Alzheimer's disease. Dialogues Clin Neurosci 2019;21:177–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ovod V, Ramsey KN, Mawuenyega KG, et al. Amyloid beta concentrations and stable isotope labeling kinetics of human plasma specific to central nervous system amyloidosis. Alzheimers Dement 2017;13:841–849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Nabers A, Perna L, Lange J, et al. Amyloid blood biomarker detects Alzheimer's disease. EMBO Mol Med 2018;10:e8763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Palmqvist S, Janelidze S, Stomrud E, et al. Performance of fully automated plasma assays as screening tests for Alzheimer disease-related beta-amyloid status. JAMA Neurol 2019;76:1060–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kaneko N, Nakamura A, Washimi Y, et al. Novel plasma biomarker surrogating cerebral amyloid deposition. Proc Jpn Acad Ser B Phys Biol Sci 2014;90:353–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Janelidze S, Stomrud E, Palmqvist S, et al. Plasma beta-amyloid in Alzheimer's disease and vascular disease. Sci Rep 2016;6:26801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mattsson N, Andreasson U, Zetterberg H, Blennow K; Alzheimer's Disease Neuroimaging Initiative. Association of plasma neurofilament light with neurodegeneration in patients with Alzheimer disease. JAMA Neurol 2017;74:557–566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Weston PSJ, Poole T, Ryan NS, et al. Serum neurofilament light in familial Alzheimer disease: a marker of early neurodegeneration. Neurology 2017;89:2167–2175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Preische O, Schultz SA, Apel A, et al. Serum neurofilament dynamics predicts neurodegeneration and clinical progression in presymptomatic Alzheimer's disease. Nat Med 2019;25:277–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bridel C, van Wieringen WN, Zetterberg H, et al. Diagnostic value of cerebrospinal fluid neurofilament light protein in neurology: a systematic review and meta-analysis. JAMA Neurol 2019;76:1035–1048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Additional references (e-1 to e-78) to this article are listed at links.lww.com/NXG/A320


