Abstract
Initial studies on renal denervation (RDN) for the treatment of non-controlled arterial hypertension (HTN) through radiofrequency ablation of renal arteries demonstrated that RDN is an effective therapeutic strategy to reduce arterial blood pressure (BP). Nonetheless, the first randomized study, SYMPLICITY-HTN-3, failed to demonstrate a clear benefit for RND over the control group. Technologic evolution, with the introduction of new second generation multi-electrode devices, allowed deep energy delivery along the full circumference of the vessel. Two recent randomized studies involving patients assuming (SPYRAL HTN-ON MED) or not (SPYRAL HTN-OFF MED) antihypertensive pharmacologic treatment, demonstrated the efficacy and safety of RDN using second generation systems for radiofrequency ablation. Another recent randomized study demonstrated that RDN with ultrasounds (RADIANCE-HTN SOLO) of the main renal arteries led to a significant BP reduction compared to the control group. These studies have once again raised the interest of the scientific community towards attempting to define the appropriate role of RDN in the treatment of hypertension. Nonetheless, larger and longer clinical trials will be necessary to draw further conclusions.
Keywords: Arterial hypertension, Renal arteries, Sympathetic nervous system
Introduction
Over 1 billion people worldwide suffer from hypertension (HTN); of these, ∼150 million in Europe and the number is constantly growing. By 2025, an increase of 15–20% is expected with almost 1.5 billion hypertensive people worldwide. This high prevalence is constant, regardless of social status, income, and geographic location. Hypertension becomes progressively more common with advancing age. In fact, the prevalence in adults reaches around 30–45% and becomes greater than 60% in people over the age of 60. It is also estimated that over 9 million people die each year from complications related to hypertension, such as myocardial infarction, stroke, and kidney failure.2 These impressive epidemiological data underline the need for new therapeutic options to control arterial blood pressure (BP), considering that the reduction of even a few millimetres of mercury of pressure is associated with significant reductions in cardiovascular events.1 With this aim, the recent guidelines of the American College of Cardiology/American Heart Association (2017) and of the European Society of Cardiology (2018) have redefined the criteria for HTN and the indications to drug treatment initiation, which is now recommended for lower BP thresholds than in the past, particularly in patients at higher cardiovascular risk.2,3
The sympathetic nervous system and arterial pressure: rationale for treatment with renal denervation
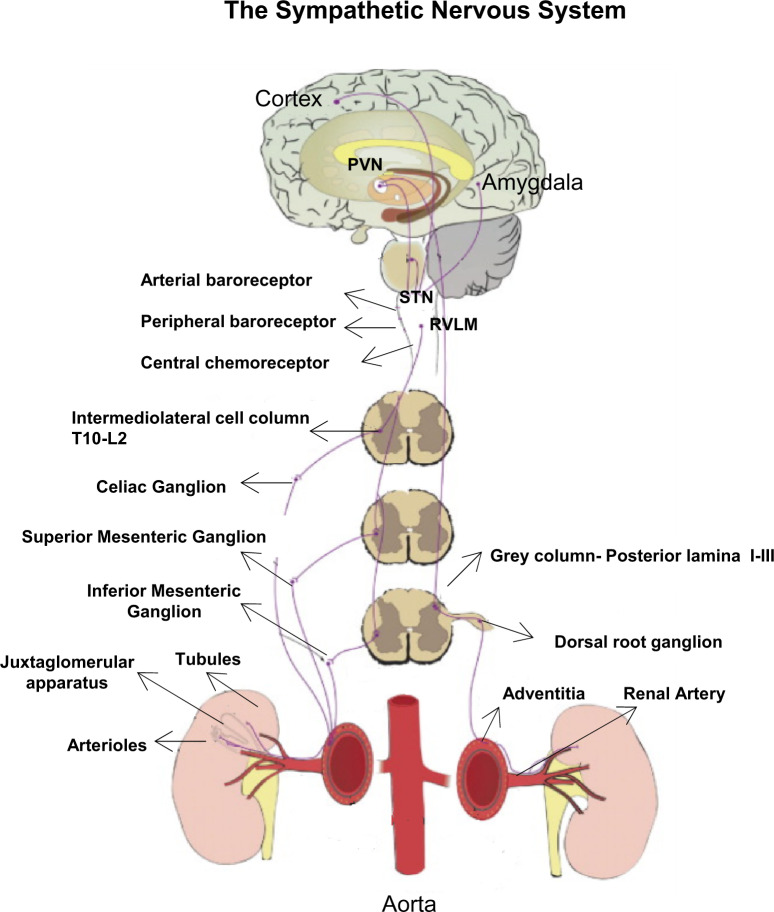
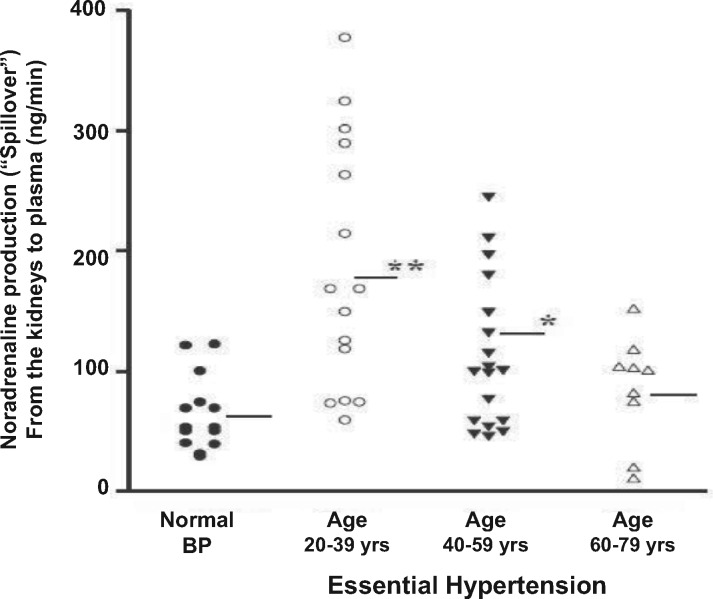
Blood pressure is regulated by many neurogenic and humoral factors that condition the functional and structural state of microcirculation by regulating peripheral vascular resistance (Figure 1). The sympathetic nervous system (SNS) has a well-defined role in regulating pressure in both acute and chronic conditions. Sympathetic nerve activity is increased in all forms of hypertension when measured as muscular sympathetic nerve activity (MSNA). Renal norepinephrine production is on average two to three times higher in patients with essential hypertension or secondary to obesity (Figure 2). This observation highlights the role of the SNS in regulating pressure and its activity increases early in hypertensive patients. It is interesting to note that the reactivity of the sympathetic system is increased in normotensive children of hypertensive parents compared to the offspring of normotensive parents. This aspect underlines the different phenotypic expression of the responsiveness of the SNS based on familiarity.4
Figure 1.
The kidney plays a key role in the regulation of cardiovascular function and in pressure homeostasis. Two main functions of the kidney are involved in cardiovascular control: the production and release of renin with consequent production of angiotensin II, a powerful vasoconstrictor agent, and the urinary excretion of Na which affects the fluid balance. Both of these effects are influenced by adrenergic nerve factors that play a key role in controlling renin release and saline balance through both direct and indirect mechanisms. In particular, the sympathetic nervous system has a key role in the regulation of perfusion and renal function through afferent and efferent fibres that reach the kidneys from the aorta with fibres located in the adventitia of the renal arteries.
Figure 2.
Renal norepinephrine production is on average two to three times higher in patients with essential hypertension or secondary to obesity. This observation highlights the role of the sympathetic nervous system in regulating pressure and its activity increases early in hypertensive patients.
The kidney plays a key role in the regulation of cardiovascular function and in BP homoeostasis. Two main functions of the kidney are involved in cardiovascular control: the production and release of renin with consequent production of angiotensin II, a powerful vasoconstrictor agent, and the urinary excretion of sodium which affects the fluid balance. Both of these effects are influenced by adrenergic nerve factors that play an essential role in controlling renin release and saline balance through both direct and indirect mechanisms. Specifically, the SNS regulates perfusion and renal function through afferent and efferent fibres that reach the kidneys from the aorta with fibres located in the adventitia of the renal arteries.5
Cannon was the first to describe the effects of sympathectomy on BP in 1931. In the 1950s, surgical sympathectomy became a technique capable of controlling BP levels, reducing the mortality of patients with malignant hypertension. Unfortunately, this technique, although effective, was burdened by a high morbidity and was inevitably abandoned with the discovery of antihypertensive drugs and diuretics.
Radiofrequency denervation
Based on the results of experimental studies that underlined the role of the sympathetic nerve fibres of the kidney in BP control, a selective sympathectomy technique was developed, inspired by the procedures used in electrophysiology for rhythm disorders ablation. Thus, the first Symplicity catheter was developed by Ardian Inc. (Paolo Alto, CA, USA), a device capable of selectively destroying the sympathetic fibres of the renal arteries with radiofrequency energy via a percutaneous approach. Through the use of this system, it was possible to demonstrate, at first on an animal model and subsequently in humans, that this procedure was able to reduce the production of norepinephrine, MSNA, and systemic BP values.
The Symplicity HTN-1, HTN-2, and HTN-3 studies
In 2009, Schlaich et al.6 published the results of the first case of denervation by radiofrequency ablation in a patient with five drug-resistant hypertension (RHTN). A significant reduction in systolic and diastolic values was described from the first month with a significant reduction in the spill-over of norepinephrine, plasma renin, an improvement of renal blood flow, and a reduction of left ventricular mass.
These results were confirmed by an observational register including a higher number of patients (Symplicity-HTN1) and subsequently by the first randomized study vs. medical therapy (Symplicity-HTN2).7 These data generated considerable enthusiasm in the scientific community: an expert consensus for the treatment of patients with hypertension published in 2013, included for the first time the ablation of the sympathetic pathways as a therapeutic strategy for RHTN.8
The epidemiology of hypertension in its drug-resistant form and the preliminary results of denervation yielded a major technological boost. The industries of the sector in a few months produced more than twenty new devices which could be used for this strategy through different energy sources.
Nonetheless, this remarkable interest encountered a setback with the presentation of the Symplicity-HTN3 trial results. While the main objective regarding safety (adverse events and renal and vascular complications) was achieved, the renal denervation (RDN) performed by using the Symplicity Flex catheter did not reach the efficacy endpoint with regards to the reduction of systolic BP.
Analysis of the failure of Symplicity HTN-3
There is no doubt that the design of the S-HTN3 study was very rigorous. The interest generated by the results was truly remarkable and put the approval of the radio frequency denervation system by the American FDA at stake, as well as the diffusion of the procedure worldwide. However, a careful evaluation of the study results highlights numerous elements that may have influenced the failure to reach the set end-points. Specifically, in order to address these factors, we must focus on three fundamental aspects of the study design including the selected population, the drug therapy and the technical-procedural characteristics of the procedure itself.
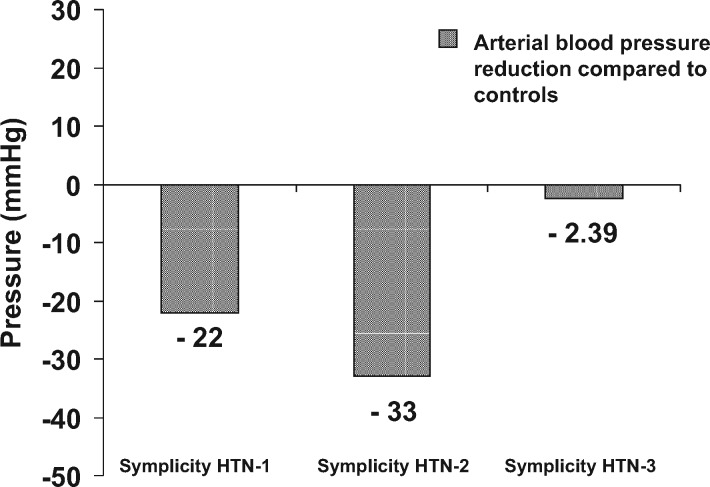
Study population
The comparison of the 6-month BP data of HTN-3 with those of the HTN-1 and HTN-2 studies is surprising (Figure 3). The evident effect of RDN on BP values obtained in the HTN1 and HTN-2 studies could be linked to the phenomenon of ‘regression from the average’, a typical bias of registers and observational studies, with very high standard deviation. Having ‘overestimated’ the effectiveness of the procedure in previous studies may have led to an error in the calculation of the sample size (calculation of power) of patients to be recruited in HTN-3. The standard deviation of the pressure variations compared to the baseline values obtained by HTN-3 underlines the considerable variability of the response after RDN, suggesting that the procedure may be effective in particular groups of patients such as those of non-African American race, patients <65 years of age, and those with normal renal function (≥60 mL/min/1.73 m2).
Figure 3.
The comparison of the six-month blood pressure data of HTN-3 with those of the HTN-1 and HTN-2 studies is truly surprising. The evident effect of renal denervation on blood pressure values obtained in the HTN1 and HTN-2 studies could be linked to the phenomenon of ‘regression from the average’: typical bias of registers and observational studies, with very high standard deviation. Having ‘overestimated’ the effectiveness of the procedure in previous studies may have led to an error in the calculation of the sample size (calculation of power) of patients to be recruited in HTN-3.
Pharmacological therapy and technical-procedural aspects
The lack of an adequate stabilization period led to the variation of at least one drug in about 40% of patients after randomization, due to the presence of side effects, creating a further confounding element. Among the least convincing points from a methodological point of view, we must cite those relating to technical-procedural aspects of the RDN procedure. In fact, on average, each operator performed only three procedures during the study (one-third of the operators only one procedure) with the learning curve achieved during the trial.
Second generation systems
The second generation denervation systems were born to improve the safety9–11 and the effectiveness of RDN procedures.12,13 The design of these devices was linked to the concept that the radial distribution of the lesions created during RDN over the entire circumference of the vessel represented a crucial aspect for success, making the procedure less operator dependent.
However, after the neutral results of the Symplicity HTN-3 study, most of the investment in developing new clinical trials on second generation RDN systems was discontinued and many of the studies abandoned.
Among the new devices subject to important investments by the manufacturers and of considerable clinical attention is the Symplicity Spyral system (Medtronic) developed through the use of a flexible system with four electrodes mounted on a 4-Fr catheter to determine during energy delivery four simultaneous lesions with a helical distribution. The RDN performed through this system provided for ablations carried out both at the level of the main renal artery and its branches. The theoretical verifications were evaluated in two trials (SPYRAL HTN-OFF MED and SPYRAL HTN-ON MED).14,15 These multicentre studies, conducted in single-blind, randomized against a group in which the procedure was simulated (‘Sham’ group) enrolled patients with systolic and diastolic hypertension. All operators were adequately trained and the RDN procedure was standardized by performing multiple RDNs also in the divisional branches of the renal arteries and in the accessory renal arteries. The inclusion criteria of the HTN-OFF MED study included patients with medium/moderate hypertension in the absence of medical treatment. The analysis of the results of the first 80 patients showed a significant reduction in BP values at 3 months for patients treated with RDN compared to the control group, without any adverse effects related to the procedure.
The SPYRAL HTN-ON MED study randomized 80 patients with elevated systolic and diastolic ambulatory BP values despite the administration of antihypertensive therapy (one to three drugs). The results of the study showed a significant reduction in ambulatory BP at 6 months in patients treated with RDN and a significant reduction in systolic pressure both at night and during the day.
An additional second generation device for the treatment of hypertension (Peregrine System Infusion Catheter, Ablative Solutions) consists of the injection of ethanol into the peri-adventitial space through the arterial wall via three needles that protrude perpendicularly from a device. The efficacy and safety of this device are currently being assessed by means of a randomized, double-blind, group-controlled study in which the procedure is simulated.
A further technique that has shown remarkable efficacy in animal studies, currently being evaluated by randomized clinical trials, involves the use of ultrasound to carry out denervation.16 Ultrasound is emitted circumferentially from a piezoelectric crystal placed in the final portion of a catheter balloon (Paradise Ultrasound System; ReCor Medical). In a recent multicentre, randomized, single-blind study, comparing non medically treated hypertensive patients randomized to either ultrasound ablation or to a sham procedure consisting of renal angiography only (RADIANCE-HTN SOLO) a significant reduction in daytime ambulatory systolic BP was achieved in the group treated with the Radiofrequency ablation two months post-procedure. Two further studies carried out using ultrasound (RADIANCE-HTN TRIO conducted in the USA and Europe and REQUIRE conducted in Japan and Korea) designed to evaluate the efficacy and safety of ultrasound denervation in hypertensive patients receiving multiple drugs are currently underway.17 A recent randomized comparison study (RADIOSOUND-HTN) between radiofrequency RDN (of the main renal artery only or ‘extensive’ including also side branches and accessories) and ultrasound RDN, involving patients with uncontrolled hypertension (i.e. patients assuming at least three classes of antihypertensive drugs), has shown a significant reduction in daily systolic BP values in the ultrasound group if compared to the radiofrequency RDN of the main renal artery group at 3 months post-procedure; no statistically significant reduction between ultrasound RDN and ‘extensive’ radiofrequency RDN of the main arteries, side branches, and accessories was found. These data support the results of studies conducted on animal models that have highlighted how ultrasound RDN achieves deeper lesions compared to radio frequency RDN, allowing for equal efficacy without the need to treat the divisional branches of the renal arteries.
The future of RDN
The SYMPLICITY HTN-3 study, although controversial, had the advantage of focusing on the considerable therapeutic potential of RDN when the procedure is preceded by adequate planning that involves a strict selection of patients, of devices, and of techniques. The effects of RDN through the use of second generation systems are summarized in Figure 4. Although these studies have shown a significant reduction in arterial BP values after RDN, it is necessary to analyse these results with caution taking into account the limits related to the small sample size and the short-term follow-up still. Larger trials, with a greater number of recruited patients and longer follow-ups, are required to better define the role of this procedure in controlling arterial BP values and in reducing the number of antihypertensive drugs and their adequate dose for long-term control of BP.
Figure 4.
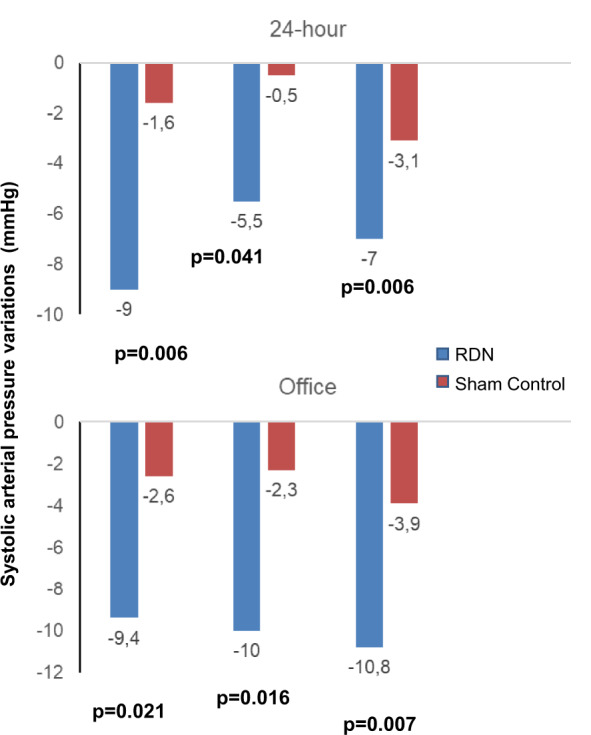
Average changes in systolic blood pressure compared to baseline during 24-h outpatient recording and assessment of blood pressure values in three outpatient randomized denervation studies of renal arteries using second generation devices compared to groups in which the procedure was simulated (‘Sham’ group): all trials show a significant reduction in the mean 24-h pressure of the outpatient pressure and the systolic pressure in the renal denervation group compared with the follow-up control group.
Conflict of interest: none declared.
References
- 1. Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, Chalmers J, Rodgers A, Rahimi K. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and metaanalysis. Lancet 2016;387:957–967. [DOI] [PubMed] [Google Scholar]
- 2. Whelton PK, Carey RM, Aronow WS et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2018;71:e127. [DOI] [PubMed] [Google Scholar]
- 3. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K; ESC Scientific Document Group. 2018 ESC/ESH Guidelines for the management of arterial hypertension. I. ESC Scientific Document Group. Eur Heart J 2018;39:3021–3104. [DOI] [PubMed] [Google Scholar]
- 4. Bertog SC, Sobotka PA, Sievert H. Renal denervation for hypertension. J Am Coll Cardiol Cardiovasc Interv 2012;5:249–258. [DOI] [PubMed] [Google Scholar]
- 5. Chinushi M, Izumi D, Iijima K, Suzuki K, Furushima H, Saitoh O, Furuta Y, Aizawa Y, Iwafuchi M. Blood pressure and autonomic responses to electrical stimulation of the renal arterial nerves before and after ablation of the renal artery. Hypertens 2013;61:450–456. [DOI] [PubMed] [Google Scholar]
- 6. Schlaich MP, Sobotka PA, Krum H, Lambert E, Esler MD. Renal sympathetic-nerve ablation for uncontrolled hypertension. N Engl J Med 2009;361:932–934. [DOI] [PubMed] [Google Scholar]
- 7.Symplicity HTN-1 Investigators. Catheter-based renal sympathetic denervation for resistant hypertension: durability of BP reduction out to 24 months. Hypertens 2011;57:911–917. [DOI] [PubMed] [Google Scholar]
- 8.Symplicity HTN-2 Investigators, Esler MD, Krum H, Sobotka PA, Schlaich MP, Schmieder RE, Böhm M. Renal sympathetic denervation in patients with treatment-resistant hypertension (The Symplicity HTN-2 Trial): a randomised controlled trial. Lancet 2010;376:1903–1909. [DOI] [PubMed] [Google Scholar]
- 9. Versaci F, Trivisonno A, Olivieri C, Caranci F, Brunese L, Prati F. Vascular response after percutaneous sympathectomy: not all devices are equal. Int J Cardiol 2014;174:406–407. [DOI] [PubMed] [Google Scholar]
- 10. Versaci F, Trivisonno A, Olivieri C, Magri G, Caranci F, Prati F. Is an abnormal vascular response after renal sympathetic denervation predictive of permanent damage? A case report of a late renal artery stenosis after energy delivery. J Endovasc Ther 2014;21:191–196. [DOI] [PubMed] [Google Scholar]
- 11. Versaci F, Trivisonno A, Olivieri C, Caranci F, Brunese L, Prati F. Late renal artery stenosis after renal denervation: is the tip of the iceberg? Int J Cardiol 2014;172:e507–e508. [DOI] [PubMed] [Google Scholar]
- 12. Versaci F, Nardi S, Trivisonno A, Olivieri C, Caranci F, Prati F. 3D-sympathetic renal denervation increases procedural efficacy in non-responders after percutaneous renal denervation: dream or reality with second generation of devices. Int J Cardiol 2014;175:370–371. [DOI] [PubMed] [Google Scholar]
- 13. Versaci F, Trivisonno A, Brunese L, Prati F. Acute treatment with renal denervation in a patient with resistant hypertension and hemorrhagic stroke. Int J Neurol Neurother 2015;2:030. [Google Scholar]
- 14. Townsend RR, Mahfoud F, Kandzari DE, Kario K, Pocock S, Weber MA, Ewen S, Tsioufis K, Tousoulis D, Sharp ASP, Watkinson AF, Schmieder RE, Schmid A, Choi JW, East C, Walton A, Hopper I, Cohen DL, Wilensky R, Lee DP, Ma A, Devireddy CM, Lea JP, Lurz PC, Fengler K, Davies J, Chapman N, Cohen SA, DeBruin V, Fahy M, Jones DE, Rothman M, Böhm M, Aoki J, Batson B, Böhm M, Choi JW, Cohen DL, Dangas G, David S, Davies J, Devireddy CM, Kandzari D, Kario K, Lee DP, Lurz PC, Patel M, Patel K, Schmieder RE, Sharp ASP, Singh J, Tsioufis K, Walton A, Weber T, Weil J, Zeller T, Ziada K, Tanabe K, Wilkins R, Mahfoud F, East C, Wilensky R, Contreras J, Steigerwalt S, Chapman N, Lea JP, Reedus D, Hoshide S, Ma A, Fengler K, Svetkey L, Rao A, Schmid A, Watkinson AF, Brown A, Tousoulis D, Hopper I, Suppan M, Agdirlioglu T, Noory E, Chasen C. Catheter-based renal denervation in patients withuncontrolled hypertension in the absence of antihypertensivemedications (SPYRAL HTN-OFFMED): a randomised, sham-controlled, proof-of-concept trial. Lancet 2017;390:2160–2170. [DOI] [PubMed] [Google Scholar]
- 15. Kandzari DE, Böhm M, Mahfoud F, Townsend RR, Weber MA, Pocock S, Tsioufis K, Tousoulis D, Choi JW, East C, Brar S, Cohen SA, Fahy M, Pilcher G, Kario K, Aoki J, Batson B, Böhm M, Choi JW, Cohen DL, Dangas G, David S, Davies J, Devireddy CM, Kandzari D, Kario K, Lee DP, Lurz PC, Papademetriou V, Patel M, Patel K, Schmieder RE, Sharp ASP, Singh J, Tsioufis K, Walton A, Weber T, Weil J, Zeller T, Ziada K, Tanabe K, Wilkins R, Mahfoud F, East C, Wilensky R, Contreras J, Steigerwalt S, Chapman N, Lea JP, Reedus D, Hoshide S, Ma A, Fengler K, Li P, Svetkey L, Rao A, Schmid A, Watkinson AF, Brown A, Tousoulis D, Hopper I, Suppan M, Agdirlioglu T, Noory E, Chasen C. Effect of renal denervation on blood pressure in the presence of antihypertensive drugs: 6-month efficacy and safety results from the SPYRAL HTN-ON MED proof-of-concept randomised trial. Lancet 2018;391:2346–2355. [DOI] [PubMed] [Google Scholar]
- 16. Azizi M, Schmieder RE, Mahfoud F, Weber MA, Daemen J, Davies J, Basile J, Kirtane AJ, Wang Y, Lobo MD, Saxena M, Feyz L, Rader F, Lurz P, Sayer J, Sapoval M, Levy T, Sanghvi K, Abraham J, Sharp ASP, Fisher NDL, Bloch MJ, Reeve-Stoffer H, Coleman L, Mullin C, Mauri L; on behalf of the RADIANCE-HTN Investigators. Endovascular ultrasound renal denervation to treat HTN (RADIANCE-HTN SOLO): a multicentre, international, single-blind, randomised, shamcontrolled trial. Lancet 2018;391:2335–2345. [DOI] [PubMed] [Google Scholar]
- 17. Mauri L, Kario K, Basile J, Daemen J, Davies J, Kirtane AJ, Mahfoud F, Schmieder RE, Weber M, Nanto S, Azizi M. A multinational clinical approach to assessing the effectiveness of catheter-based ultrasound renal denervation: the RADIANCE-HTN and REQUIRE clinical study designs. Am Heart J 2018;195:115–129. [DOI] [PubMed] [Google Scholar]