Supplemental Digital Content is available in the text.
Keywords: COVID-19, heart arrest, hospitalization, pandemics, registries, survival rate
Abstract
Background:
Patients hospitalized for severe coronavirus disease 2019 (COVID-19) infection are at risk for in-hospital cardiac arrest (IHCA). It is unknown whether certain characteristics of cardiac arrest care and outcomes of IHCAs during the COVID-19 pandemic differed compared with a pre-COVID-19 period.
Methods:
All patients who experienced an IHCA at our hospital from March 1, 2020 through May 15, 2020, during the peak of the COVID-19 pandemic, and those who had an IHCA from January 1, 2019 to December 31, 2019 were identified. All patient data were extracted from our hospital’s Get With The Guidelines–Resuscitation registry, a prospective hospital-based archive of IHCA data. Baseline characteristics of patients, interventions, and overall outcomes of IHCAs during the COVID-19 pandemic were compared with IHCAs in 2019, before the COVID-19 pandemic.
Results:
There were 125 IHCAs during a 2.5-month period at our hospital during the peak of the COVID-19 pandemic compared with 117 IHCAs in all of 2019. IHCAs during the COVID-19 pandemic occurred more often on general medicine wards than in intensive care units (46% versus 33%; 19% versus 60% in 2019; P<0.001), were overall shorter in duration (median time of 11 minutes [8.5–26.5] versus 15 minutes [7.0–20.0], P=0.001), led to fewer endotracheal intubations (52% versus 85%, P<0.001), and had overall worse survival rates (3% versus 13%; P=0.007) compared with IHCAs before the COVID-19 pandemic.
Conclusions:
Patients who experienced an IHCA during the COVID-19 pandemic had overall worse survival compared with those who had an IHCA before the COVID-19 pandemic. Our findings highlight important differences between these 2 time periods. Further study is needed on cardiac arrest care in patients with COVID-19.
What Is Known
Advanced cardiac life support and cardiopulmonary resuscitation have become mainstays of treatment for patients who experience an in-hospital cardiac arrest.
Survival of in-hospital cardiac arrests have increased over the past few decades, likely because of improved cardiac arrest care and quality improvement initiatives.
What the Study Adds
In-hospital cardiac arrest care played a major role during the peak of the coronavirus disease 2019 (COVID-19) pandemic in New York City.
Certain aspects of cardiac arrest care differed significantly during the COVID-19 surge compared with a pre-COVID-19 period.
Overall survival of in-hospital cardiac arrests decreased during the peak of the COVID-19 pandemic compared with a pre-COVID-19 period.
Since late December 2019, the world has experienced a severe outbreak of a novel coronavirus disease (COVID-19). The United States, and New York City (NYC) in particular, has emerged as an epicenter of the global pandemic, with thousands of hospitalizations, in-hospital cardiac arrests (IHCAs), and subsequent deaths.1 The clinical syndrome of COVID-19 ranges from mild infection to severe symptoms such as pneumonia, acute respiratory distress syndrome, and possible death.2 Many patients hospitalized for severe COVID-19 infection are at risk for these adverse outcomes including IHCA.3
Roughly, 200 000 IHCAs occur in the United States per year.4 Advanced cardiac life support (ACLS) and cardiopulmonary resuscitation (CPR) have become mainstays during IHCAs as means to improve survival in patients who experience an IHCA. Since 2010, studies have illustrated an ≈20% survival rate in IHCAs, with an increasing survival rate per year.5 Improved survival is probably related to improved efforts in cardiac arrest care, quality improvement initiatives, and continued education among health care workers.6
Many of these established aspects of cardiac arrest care, including ACLS and CPR, continued to play a major role during the COVID-19 pandemic. Yet, data about the efficacy of these maneuvers in patients with COVID-19 who experience an IHCA remain unknown. The rapid respiratory decline along with other severe complications associated with COVID-19 have made the clinical course unpredictable.7 It is unknown if certain risk factors, causes, and outcomes of patients who experience an IHCA during the COVID-19 pandemic are similar to previous periods before the pandemic. As a result, we sought to compare characteristics and outcomes of IHCAs during the COVID-19 pandemic and before the pandemic in a NYC public hospital.
Methods
The data from this study are available from the corresponding author upon reasonable request.
We identified all patients who experienced an IHCA from March 1, 2020 through May 15, 2020 during the COVID-19 pandemic at NYC Health & Hospitals/Jacobi, one of the 11 acute-care hospitals of the largest public health system in the United States. We compared this cohort with patients who experienced an IHCA at Health and Hospitals/Jacobi from January 1, 2019 through December 31, 2019. All patient data were extracted from our hospital’s American Heart Association’s Get With The Guidelines–Resuscitation registry, a prospective hospital-based archive of IHCA data in an attempt to improve quality measures and overall in-hospital survival after IHCAs. All hospitalized patients who experience an IHCA and undergo CPR are registered by specialized trained staff into the registry. All data are compiled using a Patient Management Tool, which is a centralized flow-sheet of all cardiac arrest data.6,8 NYC Health and Hospitals/Jacobi is one of the participating hospitals of the Get With The Guidelines–Resuscitation registry in the United States.
Patients were included in the study if they experienced an IHCA during the 2 respective time periods, as mentioned above, and who underwent CPR and ACLS. Patients <18 years old and who had a Do-Not-Resuscitate order were not included in the study. Patients who experienced an out-of-hospital cardiac arrest and arrived at the hospital with on-going CPR were not included in the study. Collected data included COVID-19 status, demographic data, comorbidities, cardiac arrest start and end time, intubation status pre- and postcardiac arrest, location of cardiac arrest, initial rhythm at the time of the cardiac arrest and specific interventions performed. Patients were labeled as COVID-19 positive if they had a laboratory confirmed positive polymerase chain reaction for severe acute respiratory syndrome coronavirus 2. The BioReference Laboratories polymerase chain reaction (PCR) molecular test was used at our hospital for COVID-19 testing. Patients were designated as COVID-19 negative if they had a negative PCR test. Patients were considered indeterminate if the patient had an IHCA before the completion of the PCR test. Outcomes of the IHCA such as whether return of spontaneous circulation (ROSC) was achieved, time to ROSC, duration of IHCA, and overall survival at discharge were also collected. Patients were divided into 2 cohorts for statistical analysis based on time of IHCA, before the COVID-19 pandemic and during the COVID-19 pandemic. The primary outcome of the study was survival rate at discharge. Secondary outcomes included duration of cardiac arrest, association of in-hospital location and cardiac arrest, rate of achieved ROSC, time to ROSC, and a comparison of specific interventions performed during the cardiac arrest. All investigators had access to the study database and statistical analysis. This study was approved by the Albert Einstein College of Medicine Institutional Review Board.
Categorical data are shown as numbers and percentages. Continuous variables are presented as means with SDs or medians and interquartile ranges. Parametric or nonparametric hypothesis tests were used depending on variable characteristics. Medians were compared using the Kruskal-Wallis test, and proportions were compared using the χ2 test or Fisher exact test. A P of <0.05 was considered statistically significant. Statistical analysis was performed using STATA 16.1.
Results
From March 1, 2020 through May 15, 2020, during the peak of the COVID-19 pandemic in NYC, there were 125 patients who experienced an IHCA at NYC Health and Hospitals/Jacobi from a total of 4470 total hospitalizations. The incidence rate of IHCAs during this time period was 2.8%. Ninety-nine (79%) of these patients had a laboratory confirmed positive PCR test for COVID-19, 12 patients (10%) tested negative, and 14 (11%) were indeterminate as they had an IHCA before a completed COVID-19 PCR test. In comparison, from January 1, 2019 through December 31, 2019, there were 117 IHCAs from a total of 20 181 hospitalizations. The incidence rate of IHCAs during this time period was 0.6%. As shown in Table 1, both cohorts, those who experienced an IHCA during the COVID-19 pandemic and those before the pandemic in 2019, were similar in median age (67 [57–76] versus 66 [56–77], P=0.99), were less often female (34% versus 42%, P=0.18) and had similar rates comorbidities.
Table 1.
Baseline Characteristics of Patients With an In-Hospital Cardiac Arrest Pre-COVID-19 Pandemic vs During the COVID-19 Pandemic
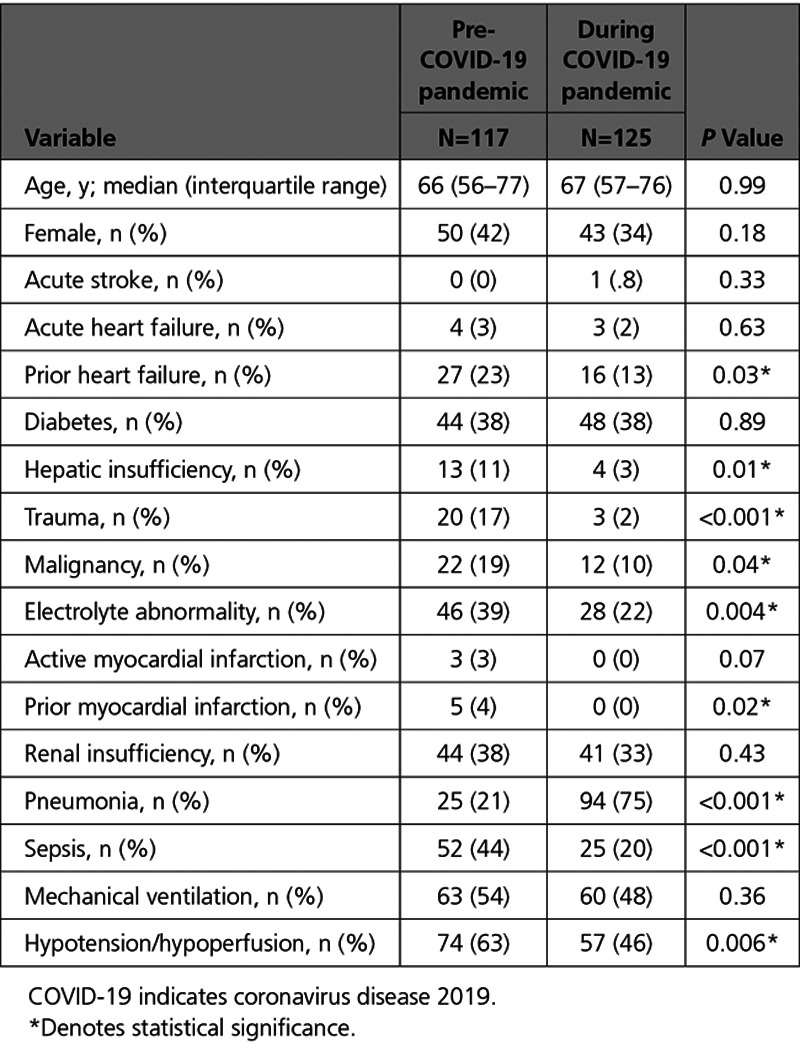
In contrast, those who experienced an IHCA before the COVID-19 pandemic had higher rates of various comorbidities such as: history of prior heart failure (23% versus 13%; P=0.03), acute trauma (17% versus 2%; P<0.001), malignancy (19% versus 10%; P=0.04), sepsis (44% versus 20%; P<0.001), and evidence of hypotension or hypoperfusion (63% versus 46%; P=0.006) compared with patients who had an IHCA during the COVID-19 pandemic (Table 1). In the cohort of patients who had an IHCA during the COVID-19 pandemic, there was more evidence of pneumonia (75% versus 21%; P<0.001) compared with those who had an IHCA in 2019. In addition, a sensitivity analysis was performed comparing IHCAs during the pandemic, from March 1, 2020 through May 15, 2020, to the same time period in 2019 (March 1, 2019 to May 15 2019), which yielded similar findings (Table I in the Data Supplement).
Furthermore, as shown in Figure 1, the majority of IHCAs before the COVID-19 pandemic occurred in an intensive care unit setting as compared with a general inpatient service or the emergency department (60% versus 19% versus 21%, respectively). In contrast, during the peak of the COVID-19 pandemic in NYC, the majority of IHCAs occurred on general inpatient units and not in ICUs (46% versus 33%, 21% in emergency department). These differences about location of IHCAs during the COVID-19 pandemic was statistically significant (P<0.001, see Table 2). There was no statistical difference between the type of initial rhythm at the time of the IHCA between the 2 time periods. Before the COVID-19 pandemic, in 2019, 32% of patients had asystole as the presenting arrest rhythm, 55% had pulseless electrical activity, 9% had ventricular fibrillation/pulseless ventricular tachycardia, and 4% had unknown cardiac rhythms. During the 2.5 months of the COVID-19 pandemic, 37% of patients had asystole, 54% had pulseless electrical activity, 3% had ventricular fibrillation/pulseless ventricular tachycardia, and 6% had unknown cardiac rhythms (P=0.28).
Figure 1.
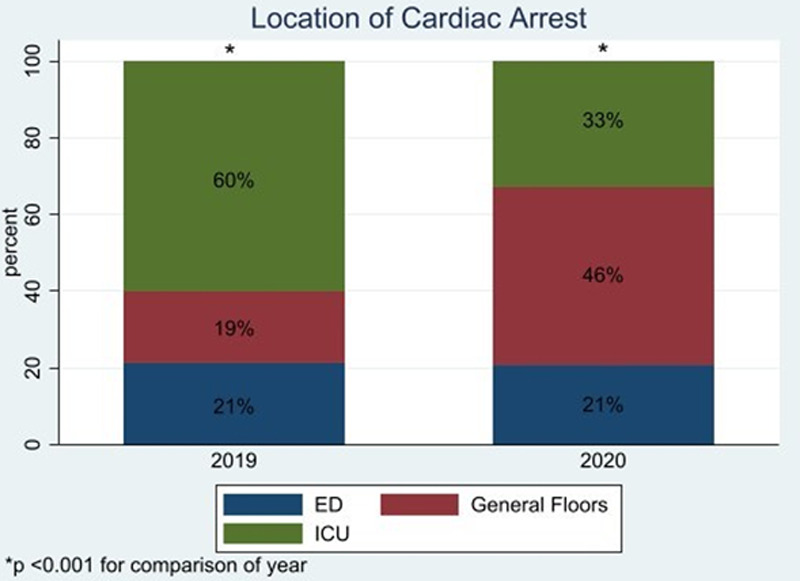
Location of in-hospital cardiac arrests during the coronavirus disease 2019 (COVID-19) pandemic vs before the COVID-19 pandemic. ED indicates emergency department; and ICU, intensive care unit.
Table 2.
Characteristics of In-Hospital Cardiac Arrests During Pre-COVID-19 Pandemic Period vs During the COVID-19 Pandemic
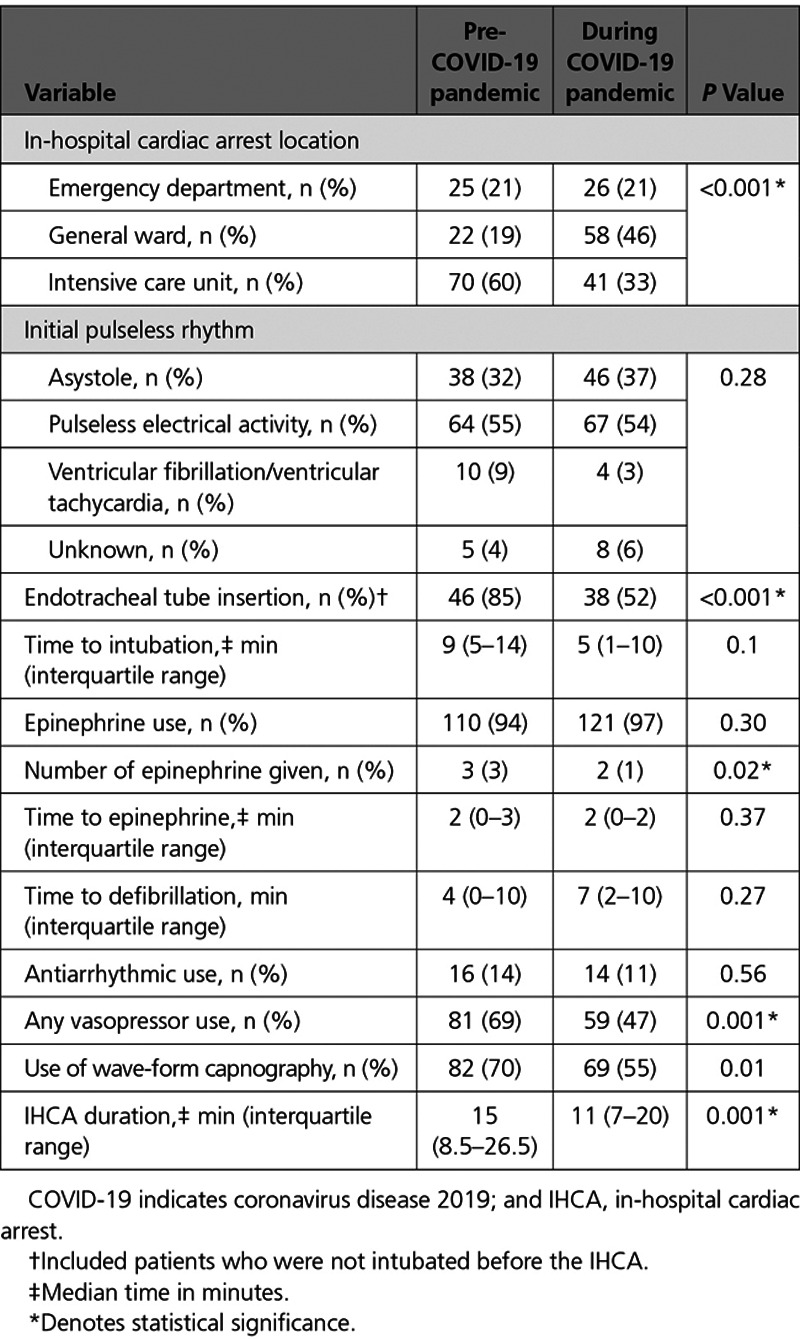
Moreover, as shown in Table 2, the duration of IHCAs was on average shorter during the COVID-19 pandemic compared with 2019 (median time of 11 minute [8.5–26.5] versus 15 minute [7.0–20.0], P=0.001). Similarly, for those not intubated before the IHCA, fewer patients underwent endotracheal tube insertion for mechanical ventilation at the time of IHCA during the COVID-19 pandemic compared with 2019 (52% versus 85%; P≤0.001). There was also a statistical difference between vasopressor use during and after the IHCA between the 2 cohorts, with more vasopressor use before the pandemic compared with during the pandemic (69% versus 47%; P=0.001). Yet, there was no statistical difference between epinephrine use (94% versus 97%; P=0.3), median time to first epinephrine use (2 minute [0–3] versus 2 minute [0–3]; P=0.37), and use of antiarrhythmic medications (14% versus 11%; P=0.56) between the 2 cohorts.
In terms of overall outcomes after initial IHCA, more patients achieved ROSC at the time of initial cardiac arrest in the 2019 cohort compared with during the COVID-19 pandemic (56% versus 36%; P=0.001). For those who achieved ROSC, there was no statistical difference in the median time to ROSC between the 2 cohorts (12 minute [5–19] versus 9 minute [5–16], P=0.86; Table 3). There was also no difference in the number of patients who underwent recurrent CPR for those who achieved ROSC after the initial IHCA during both time periods (36% versus 29%; P=0.41). These findings were similar in patients who were only COVID-19 positive. In addition, there was no significant differences in outcomes in COVID-19 positive/indeterminate patients versus COVID-19 negative patients except for median time to ROSC, which was shorter in COVID-19 negative patients (5.5 minute [2–9] versus 10 minute [5–14]) compared with patients who were positive/indeterminate. Furthermore, as illustrated in Figure 2, overall survival rate at discharge was worse during the COVID-19 pandemic compared with before the pandemic. Only 3% of patients survived an IHCA and were discharged from the hospital during the 2.5 months of the COVID-19 pandemic (compared with 13% in 2019 before the pandemic [P=0.007] or 18.3% survival in 2018). Furthermore, within the COVID-19-positive cohort, only 2% survived to discharge.
Table 3.
Outcomes of In-Hospital Cardiac Arrests During Pre-COVID-19 Period vs During the COVID-19 Pandemic
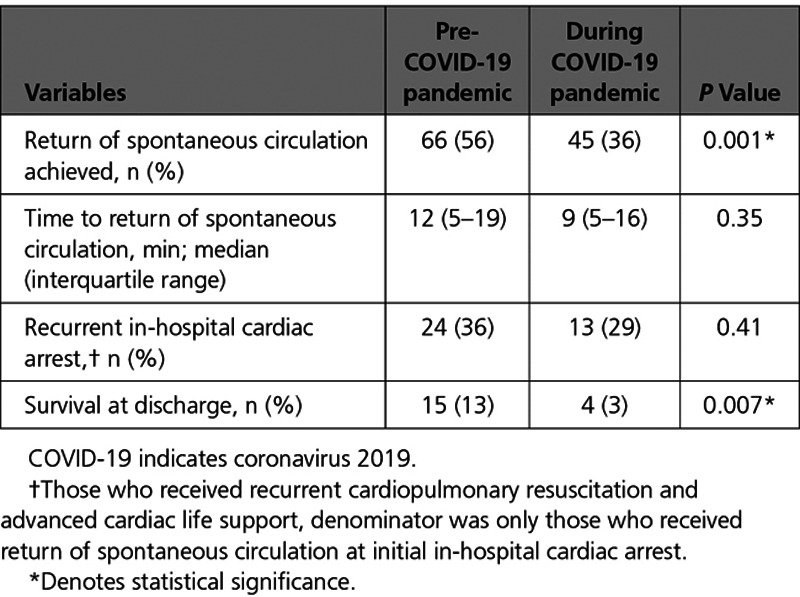
Figure 2.
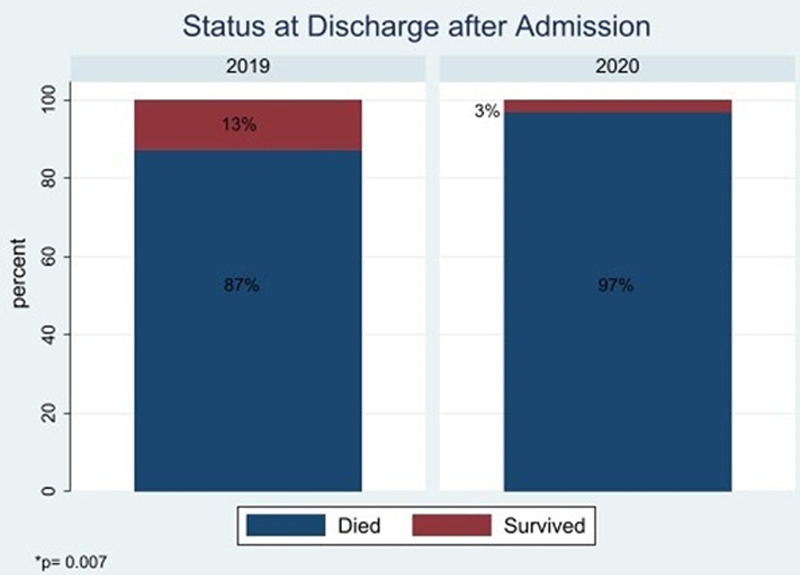
Overall survival at discharge after in-hospital cardiac arrest before coronavirus disease 2019 (COVID-19) pandemic and during the COVID-19 pandemic.
Discussion
To our knowledge, this is the first detailed analysis of the characteristics and outcomes of IHCAs during the COVID-19 pandemic in the United States. At our hospital, specific features, interventions, and outcomes of IHCAs during the COVID-19 surge differed significantly compared with IHCAs occurring before the COVID-19 pandemic. Specifically, they had shorter cardiac arrest durations, less endotracheal intubations, and higher mortality. Moreover, IHCAs occurred more frequently in general medicine units than ICUs during the pandemic.
Before COVID-19, studies showed a 10% to 20% survival rate in patients with IHCAs.6,9 At our institution, the survival rate of IHCAs in 2019 was 13% (18.3% survival rate in 2018). However, the survival rate of IHCAs during the 2.5 months of the surge was significantly lower at ≈3%. Our findings are similar to Shao et al,3 who demonstrated an IHCA survival rate of 2.9% at 30 days in patients from Wuhan, China. One hypothesis to explain the discrepancy of survival rates is because of the underlying cause of the cardiac arrest as the large majority of patients were COVID-19 positive. COVID-19 is associated with severe systemic inflammation and profound hypoxia.10,11 Studies have demonstrated various other systemic complications that occur in patients with COVID-19, such as cardiac injury, kidney dysfunction, and coagulation activation leading to thromboembolic events.12–15 These insults to the body are presumably irreversible and, without meaningful treatments at this time, thus leading to worse outcomes. In contrast, common causes of IHCAs before the pandemic such as cardiac events, severe electrolyte abnormalities or trauma portend to higher survival rates as they may be reversible.16
Furthermore, more IHCAs occurred on general medicine units than the ICUs during the pandemic. Triage of patients with COVID-19 has been difficult during the surge because of the lack of available intensive care unit beds and the unpredictability of the clinical course.3,17,18 Many patients with severe COVID-19 required admission to an intensive care unit or a monitored setting but were unfortunately limited by bed availability. This may have placed patients at a higher risk for unmonitored clinical deterioration.19 We also suspect that more IHCAs occurred because of a lack of continuous oximetry monitoring in the general medicine units as rapid respiratory failure was often difficult to predict.
Moreover, an added complexity during the COVID-19 surge was the need for personal protective equipment and the risk of infection among health care workers.20,21 ACLS protocols including chest compressions and endotracheal tube insertion for patients with COVID-19 placed health care workers at a higher risk of exposure. CPR and mechanical ventilation are aerosol generating procedures, which increases transmission of the virus.22 Studies emphasize the importance of rescuer safety and the need for appropriate personal protective equipment donning during cardiac arrest care.23,24 Because of increased personal protective equipment requirements and the complexity of the donning process, the preparation time for IHCAs may have been longer and studies have demonstrated worse mortality in IHCAs when there are longer delays to chest compressions and ACLS.25 Additionally, the sheer volume of IHCAs, often at similar times, may have contributed to delays or complexities in care. Other considerations need to be considered, such cases where the patient’s overall poor prognosis may have deemed cardiac resuscitation unhelpful compounded by the concerns for unnecessary staff exposure. All of the above may explain why there was shorter average cardiac arrest durations and fewer endotracheal intubations during the pandemic. In addition, it is possible that some patients had a do-not-intubate order although not a Do-Not-Resuscitate order or CPR and/or intubation was terminated at the request of patients’ families during the cardiac arrest event.
Various recommendations have been made to improve resuscitation care in patients with COVID-19, while maintaining provider safety, since the beginning of the pandemic. Specific examples include limiting personnel involved, using mechanical CPR devices, having an experienced intubator involved and utilizing video laryngoscopy.26 However, it is unclear currently if any of these interventions are effective in improving resuscitation care in patients with COVID-19.
Our study has certain limitations. First, the retrospective nature of our analysis allows for potential confounding and selection bias. Second, our study is a single-center study from NYC and thus might not be generalizable to other hospital settings. In addition, our hospital did not have specific resuscitation policies that were in place during the pandemic, which might be the case in other hospital settings, but instead were assessed on a case by case basis. Last, certain details surroundings the IHCAs were unable to be obtained, including some demographic data, neurological status in those who survived, time of arrest to timing of CPR, exact oxygen requirements, quality of chest compressions, and the reasons for termination of CPR.
Conclusions
Our study demonstrated that the overall survival of IHCAs was worse during the peak of the COVID-19 pandemic in a New York City hospital compared with before the pandemic. Certain features of IHCAs during the pandemic differed from prior, such as the in-hospital location of IHCAs and the overall duration of IHCAs. Our findings highlight the important differences in IHCAs during the pandemic compared with before the pandemic. Further study is needed on cardiac arrest care in patients with COVID-19 to improve overall in-hospital survival.
Disclosures
This work represents the authors’ independent analysis of local data gathered using the American Heart Association (AHA) Get With The Guidelines (GWTG) Patient Management Tool but is not an analysis of the national GWTG dataset and does not represent findings from the AHA GWTG National Program. The other authors report no conflicts.
Supplementary Material
Footnotes
The Data Supplement is available at https://www.ahajournals.org/doi/suppl/10.1161/CIRCOUTCOMES.120.007303.
References
- 1.Wadhera RK, Wadhera P, Gaba P, Figueroa JF, Joynt Maddox KE, Yeh RW, Shen C. Variation in COVID-19 hospitalizations and deaths across New York city boroughs. JAMA. 2020;323:2192–2195. doi: 10.1001/jama.2020.7197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shao F, Xu S, Ma X, Xu Z, Lyu J, Ng M, Cui H, Yu C, Zhang Q, Sun P, Tang Z. In-hospital cardiac arrest outcomes among patients with COVID-19 pneumonia in Wuhan, China. Resuscitation. 2020;151:18–23. doi: 10.1016/j.resuscitation.2020.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nallamothu BK, Guetterman TC, Harrod M, Kellenberg JE, Lehrich JL, Kronick SL, Krein SL, Iwashyna TJ, Saint S, Chan PS. How do resuscitation teams at top-performing hospitals for in-hospital cardiac arrest succeed? A qualitative study. Circulation. 2018;138:154–163. doi: 10.1161/CIRCULATIONAHA.118.033674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, Ferguson TB, Ford E, Furie K, Gillespie C, Go A, Greenlund K, Haase N, Hailpern S, Ho PM, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott MM, Meigs J, Mozaffarian D, Mussolino M, Nichol G, Roger VL, Rosamond W, Sacco R, Sorlie P, Roger VL, Stafford R, Thom T, Wasserthiel-Smoller S, Wong ND, Wylie-Rosett J; WRITING GROUP MEMBERS; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics–2010 update: a report from the American Heart Association. Circulation. 2010;121:e46–e215. doi: 10.1161/CIRCULATIONAHA.109.192667 [DOI] [PubMed] [Google Scholar]
- 6.Girotra S, Nallamothu BK, Spertus JA, Li Y, Krumholz HM, Chan PS; American Heart Association Get with the Guidelines–Resuscitation Investigators. Trends in survival after in-hospital cardiac arrest. N Engl J Med. 2012;367:1912–1920. doi: 10.1056/NEJMoa1109148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, Barnaby DP, Becker LB, Chelico JD, Cohen SL, Cookingham J, Coppa K, Diefenbach MA, Dominello AJ, Duer-Hefele J, Falzon L, Gitlin J, Hajizadeh N, Harvin TG, Hirschwerk DA, Kim EJ, Kozel ZM, Marrast LM, Mogavero JN, Osorio GA, Qiu M, Zanos TP; the Northwell COVID-19 Research Consortium. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York city area. JAMA. 2020;323:2052–2059. doi: 10.1001/jama.2020.6775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Starks MA, Dai D, Nichol G, Al-Khatib SM, Chan P, Bradley SM, Peterson ED; American Heart Association’s Get With the Guidelines-Resuscitation Investigators. The association of duration of participation in get with the guidelines-resuscitation with quality of care for in-hospital cardiac arrest. Am Heart J. 2018;204:156–162. doi: 10.1016/j.ahj.2018.04.018 [DOI] [PubMed] [Google Scholar]
- 9.Schluep M, Gravesteijn BY, Stolker RJ, Endeman H, Hoeks SE. One-year survival after in-hospital cardiac arrest: a systematic review and meta-analysis. Resuscitation. 2018;132:90–100. doi: 10.1016/j.resuscitation.2018.09.001 [DOI] [PubMed] [Google Scholar]
- 10.Tay MZ, Poh CM, Rénia L, MacAry PA, Ng LFP. The trinity of COVID-19: immunity, inflammation and intervention. Nat Rev Immunol. 2020;20:363–374. doi: 10.1038/s41577-020-0311-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tang X, Du RH, Wang R, Cao TZ, Guan LL, Yang CQ, Zhu Q, Hu M, Li XY, Li Y, Liang LR, Tong ZH, Sun B, Peng P, Shi HZ. Comparison of hospitalized patients with ARDS caused by COVID-19 and H1N1. Chest. 2020;158:195–205. doi: 10.1016/j.chest.2020.03.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, Mehra MR, Schuepbach RA, Ruschitzka F, Moch H. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–1418. doi: 10.1016/S0140-6736(20)30937-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, Kant KM, Kaptein FHJ, van Paassen J, Stals MAM, Huisman MV, Endeman H. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–147. doi: 10.1016/j.thromres.2020.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, Gong W, Liu X, Liang J, Zhao Q, Huang H, Yang B, Huang C. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5:802–810. doi: 10.1001/jamacardio.2020.0950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cheng Y, Luo R, Wang K, Zhang M, Wang Z, Dong L, Li J, Yao Y, Ge S, Xu G. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020;97:829–838. doi: 10.1016/j.kint.2020.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hirlekar G, Karlsson T, Aune S, Ravn-Fischer A, Albertsson P, Herlitz J, Libungan B. Survival and neurological outcome in the elderly after in-hospital cardiac arrest. Resuscitation. 2017;118:101–106. doi: 10.1016/j.resuscitation.2017.07.013 [DOI] [PubMed] [Google Scholar]
- 17.Li R, Rivers C, Tan Q, Murray MB, Toner E, Lipsitch M. Estimated demand for US hospital inpatient and intensive care unit beds for patients with COVID-19 based on comparisons with Wuhan and Guangzhou, China. JAMA Netw Open. 2020;3:e208297. doi: 10.1001/jamanetworkopen.2020.8297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Remuzzi A, Remuzzi G. COVID-19 and Italy: what next?. Lancet. 2020;395:1225–1228. doi: 10.1016/S0140-6736(20)30627-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Phua J, Weng L, Ling L, Egi M, Lim CM, Divatia JV, Shrestha BR, Arabi YM, Ng J, Gomersall CD, Nishimura M, Koh Y, Du B; Asian Critical Care Clinical Trials Group. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respir Med. 2020;8:506–517. doi: 10.1016/S2213-2600(20)30161-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cook TM. Personal protective equipment during the coronavirus disease (COVID) 2019 pandemic - a narrative review. Anaesthesia. 2020;75:920–927. doi: 10.1111/anae.15071 [DOI] [PubMed] [Google Scholar]
- 21.Mahase E, Kmietowicz Z. Covid-19: doctors are told not to perform CPR on patients in cardiac arrest. BMJ. 2020;368:m1282. doi: 10.1136/bmj.m1282 [DOI] [PubMed] [Google Scholar]
- 22.Couper K, Taylor-Phillips S, Grove A, Freeman K, Osokogu O, Court R, Mehrabian A, Morley PT, Nolan JP, Soar J, Perkins GD. COVID-19 in cardiac arrest and infection risk to rescuers: a systematic review. Resuscitation. 2020;151:59–66. doi: 10.1016/j.resuscitation.2020.04.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Torabi-Parizi P, Davey RT, Jr, Suffredini AF, Chertow DS. Ethical and practical considerations in providing critical care to patients with Ebola virus disease. Chest. 2015;147:1460–1466. doi: 10.1378/chest.15-0278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Monsieurs KG, Nolan JP, Bossaert LL, Greif R, Maconochie IK, Nikolaou NI, Perkins GD, Soar J, Truhlář A, Wyllie J, Zideman DA; ERC Guidelines 2015 Writing Group. European resuscitation council guidelines for resuscitation 2015: section 1. Executive summary. Resuscitation. 2015;95:1–80. doi: 10.1016/j.resuscitation.2015.07.038 [DOI] [PubMed] [Google Scholar]
- 25.Chan PS, Krumholz HM, Nichol G, Nallamothu BK; American Heart Association National Registry of Cardiopulmonary Resuscitation Investigators. Delayed time to defibrillation after in-hospital cardiac arrest. N Engl J Med. 2008;358:9–17. doi: 10.1056/NEJMoa0706467 [DOI] [PubMed] [Google Scholar]
- 26.Edelson DP, Sasson C, Chan PS, Atkins DL, Aziz K, Becker LB, Berg RA, Bradley SM, Brooks SC, Cheng A, Escobedo M, Flores GE, Girotra S, Hsu A, Kamath-Rayne BD, Lee HC, Lehotsky RE, Mancini ME, Merchant RM, Nadkarni VM, Panchal AR, Peberdy MAR, Raymond TT, Walsh B, Wang DS, Zelop CM, Topjian AA; American Heart Association ECC Interim COVID Guidance Authors. Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19: from the Emergency Cardiovascular Care Committee and get with the guidelines-resuscitation adult and pediatric task forces of the American Heart Association. Circulation. 2020;141:e933–e943. doi: 10.1161/CIRCULATIONAHA.120.047463 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


