Abstract
Background
The prevalence of gestational diabetes mellitus (GDM) is increasing worldwide. A healthy diet and stable blood glucose levels during pregnancy can prevent adverse health outcomes for the mother and the newborn child. Mobile health may be a useful supplement to prenatal care, providing women with targeted dietary information concerning GDM.
Objective
We analyzed secondary data from a two-arm, multicentered, nonblinded randomized controlled trial to determine if a smartphone app with targeted dietary information and blood glucose monitoring had an effect on the dietary behavior of women with GDM.
Methods
Women with a 2-hour oral glucose tolerance test level of ≥9 mmol/L were individually randomized to either the intervention group receiving the Pregnant+ app and usual care or the control group receiving usual care only. Eligible women were enrolled from 5 diabetes outpatient clinics in the Oslo region, Norway, between October 2015 and April 2017. The Pregnant+ app promoted 10 GDM-specific dietary recommendations. A healthy dietary score for Pregnant+ (HDS-P+) was constructed from a 41-item food frequency questionnaire and used to assess the intervention effect on the dietary behavior completed at trial entry and at around gestation week 36. Dietary changes from baseline to week 36 were examined by a paired sample two-tailed t test. Between-group dietary differences after the intervention were estimated with analysis of covariance, with adjustment for baseline diet.
Results
A total of 238 women participated: 115 were allocated to the intervention group and 123 to the control group. Of the 238 women, 193 (81.1%) completed the food frequency questionnaire both at baseline and around gestational week 36. All the participants showed improvements in their HDS-P+ from baseline. However, the Pregnant+ app did not have a significant effect on their HDS-P+. The control group reported a higher weekly frequency of choosing fish meals (P=.05). No other significant differences were found between the intervention and control groups. There were no significant demographic baseline differences between the groups, except that more women in the intervention group had a non-Norwegian language as their first language (61 vs 46; P=.02).
Conclusions
Our findings do not support the supplementation of face-to-face follow-up of women with GDM with a smartphone app in the presence of high-standard usual care, as the Pregnant+ app did not have a beneficial effect on pregnant women’s diet.
Trial Registration
ClinicalTrials.gov NCT02588729; https://clinicaltrials.gov/ct2/show/NCT02588729
Keywords: gestational diabetes mellitus, diet, mHealth, mobile phone, randomized controlled trial
Introduction
Gestational diabetes mellitus (GDM) is defined as hyperglycemia detected at any time during pregnancy [1]. The prevalence of GDM is increasing worldwide and ranges from 1% to 20% globally depending on the screening procedure and population characteristics [2]. The prevalence of GDM in Norway was 5% in 2018, according to the Norwegian Medical Birth Registry [3]. However, a cohort study in a district in Oslo identified GDM in 13% of all women, 11% of ethnic Norwegians, and 12%-17% of women in groups of non-European origin [4]. Women of South Asian and African origins tend to develop GDM at a lower body mass index and age compared to White Europeans [5]. The other risk factors for developing GDM include overweight and obesity, advanced maternal age, a family history of diabetes, and GDM in a previous pregnancy [6]. Even though GDM resolves in most women after delivery, its development may affect the health of both mothers and children in the short and long terms [7,8].
A healthy diet and stable blood glucose levels throughout pregnancy can prevent adverse health outcomes for the mother and the newborn child [9]. About 85% of the women diagnosed with GDM can manage the disease with lifestyle changes such as healthy eating and physical activity, without the need for oral metformin or insulin therapy [10]. However, lifestyle changes presuppose knowledge, motivation, and follow-up by health care professionals [11]. Pregnant women are often in contact with health care professionals; however, perinatal care involves dealing with many health-related issues, and there are some indications that women are not provided sufficient information about the management of GDM by their health care professionals [12,13].
Mobile health (mHealth)—defined as medical and public health practice supported by mobile devices such as smartphones, patient monitoring devices, personal digital assistants, and other wireless devices [14]—may be a useful supplement to perinatal care by providing women with GDM with dietary information and the opportunity to register blood glucose levels [15]. A scoping review has found several ongoing randomized controlled trials (RCTs) that evaluate the effectiveness of smartphone apps in the management of GDM [16]. Some results of these RCTs have been published recently [17,18]. Even though these studies did not find any effect on the glycemic, maternal, and neonatal outcomes [17,18], there is a lack of studies investigating the possible effects of an app on the diet of women with GDM. A systematic review has studied the usability of apps in the health care of pregnant women without GDM. That review indicated that apps may support women in reducing gestational weight gain and in increasing their intake of vegetables and fruits; however, the evidence of their effectiveness is still limited [19]. Dodd et al [20] evaluated the impact of a smartphone app as an adjunct to face-to-face consultation in facilitating dietary changes among pregnant women in South Australia. They found no significant benefit of the smartphone app in the intervention group. All women improved their dietary quality during pregnancy [20].
We have developed the Pregnant+ app for women with GDM [21]. This app provides tailored information on diet, physical activity, breastfeeding, and GDM, and the possibility to automatically transfer or manually record blood glucose levels from a glucometer to the smartphone (Multimedia Appendix 1 and Multimedia Appendix 2). The Pregnant+ app was developed in collaboration with experts in midwifery, obstetrics, physical activity, nutrition, and data security. Pregnant women with GDM of different ethnic origins were involved in several steps of its development [21]. A narrative review on studies with pregnancy-related apps found only 2 multilingual apps for use in prenatal care [22]. The Pregnant+ app is available in Norwegian, Urdu, and Somali languages. Information and pictures related to diet and physical activity are culturally adjusted according to the chosen language. This app was found to be the only app adapted to specific target groups (women born in Pakistan and Somalia) in a scoping review by Chen and Carbone [16]. The effect of this app on the main outcome (2-hour glucose level of the routine postpartum oral glucose tolerance test [OGTT]) was tested in a two-arm RCT at 5 diabetes outpatient clinics in the Oslo region, Norway [18,23]. The study showed that the Pregnant+ app did not have any significant effect on the main outcome [18].
The aim of this study was to examine if the Pregnant+ app had an effect on the dietary behavior of women. No specific dietary recommendation for women with GDM existed when the study was started in 2014. Women with GDM were recommended to follow the national dietary guidelines for healthy eating [24]. Some hospitals developed adjusted dietary advice for pregnant women with GDM. The Pregnant+ app promoted 10 GDM-specific dietary recommendations that were developed in cooperation with clinical nutritionists [21].
Methods
Study Design
We analyzed secondary data from a two-arm, multicentered, nonblinded RCT for women with GDM, which was conducted at 5 diabetes outpatient clinics in the Oslo region. This RCT is in accordance with the CONSORT-EHEALTH checklist (Multimedia Appendix 3).
Recruitment
Women with GDM were recruited from October 2015 to April 2017 by health care professionals at the diabetes outpatient clinics. At the time of recruitment, pregnant women with higher risk for GDM based on their prepregnancy weight, family history of diabetes, age, and ethnicity were sent for an OGTT [25]. Eligible women for this study were diagnosed with GDM by a 2-hour OGTT blood glucose level of ≥9 mmol/L, according to the definition of GDM in the Norwegian guidelines [25]. In addition, participants were older than 18 years, were less than 33-weeks pregnant, owned smartphones, and understood Norwegian, Urdu, or Somali. Women with type 1 or type 2 diabetes (OGTT blood glucose levels≥11 mmol/L), twin pregnancy, celiac disease, or lactose intolerance were excluded from the study. In total, 774 women were assessed for eligibility and 238 participated (Figure 1). Those who agreed to participate signed a consent form. All the participants in both groups received a glucometer and lancets from the study administrators. The Norwegian Social Science Data Services (identifier: 2014/38942) approved the study.
Figure 1.
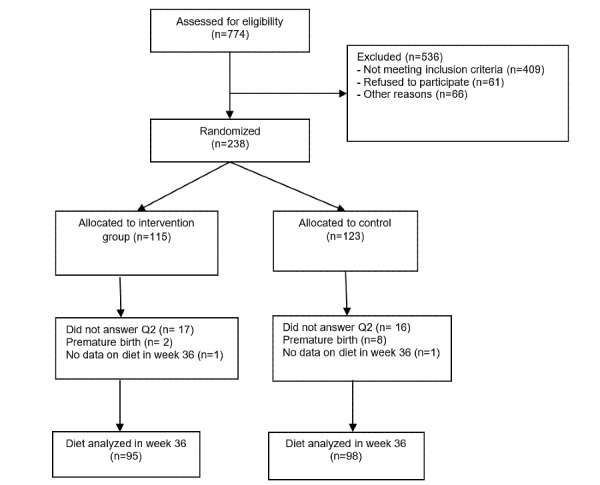
Flow chart describing the process leading up to the final number included in the analysis of dietary behavior in the Pregnant+ study.
Randomization and Blinding
The participants were randomly allocated to 2 groups: intervention (access to the Pregnant+ app and usual care) and control (usual care). Randomization was performed on a 1:1 basis with allocated blocks of 4. Women who agreed to participate filled out a baseline questionnaire (Q1) on an electronic tablet (average time 30-45 minutes). After completing Q1, a computer-based program randomized and allocated the women to either the intervention or the control group. The participating women, project workers, and health care professionals at the diabetes outpatient clinics were not blinded to the allocation.
Intervention and Control
Usual Care (Control) Group
The participants in the control group received usual care for GDM according to the national guidelines [26]. This included regular consultations (every 1-2 weeks) with midwives or nurses, both specialized in diabetes, at the diabetes outpatient clinics. According to the guidelines [26], women should be provided with information about a healthy diet, with emphasis on regular meals with limited intake of sugar-rich foods and increased intake of whole grains and vegetables. The women in the control group were instructed how to measure their blood glucose levels and were asked to record these levels in a paper diary. They received written and verbal dietary advice on the basis of their blood glucose levels. In the absence of specific dietary guidelines for women with GDM, the different diabetes outpatient clinics included in the study developed some specific dietary guidelines for these women that emphasized regular meals, increased intake of vegetables and whole grains, and limited intake of sugar. If women in the usual care group downloaded the Pregnant+ app, their access was restricted to a single page with a link to the website of the Norwegian Directorate of Health with generic health information for women with GDM and a link to the Norwegian Federation of Diabetes.
Pregnant+ App and Usual Care (Intervention) Group
The participants in the intervention group had access to the Pregnant+ app in addition to usual care, as described above. The women allocated to the app group could download the app from the Apple Store or Google Play at the hospital or home. The app contained 4 main icons: “Blood glucose,” “Physical activity,” “Food and beverages,” and “Diabetes information.” The 10 GDM-specific dietary recommendations that were developed for this study [21] were presented in the “Food and beverages” icon for women (Textbox 1). The women could select if the dietary recommendations should be presented with food items and pictures representing the Norwegian, Urdu, or Somali food culture. They were also referred to recipes on the home page from the Norwegian Diabetes Foundation. They could automatically transfer or manually register their blood glucose levels in the icon “Blood glucose.” After registering, they received feedback on their values. Those with too high values were directly referred to the dietary recommendations. A graphical representation of the blood glucose levels visually aided the monitoring.
The dietary recommendations in the Pregnant+ app.
Eat healthy meals regularly.
Eat and drink little sugar.
Eat more vegetables.
Choose whole-grain products.
Limit your intake of salt.
Eat enough fish.
Choose lean dairy milk produce.
Choose healthy and less oil.
Read nutrition labels on foods before buying.
Choose water when thirsty.
Measurements
The participants answered the questionnaires on an electronic tablet during their first consultation at a diabetes outpatient clinic and at their consultation around gestational week 36. The questionnaire included a 41-item food frequency questionnaire (FFQ). At baseline, they were asked to report their dietary habits prior to being diagnosed with GDM. In the second questionnaire, they were asked to report their current diet. The FFQ included the following food groups: beverages, milk and dairy products, bread and grain, fruit and vegetables, snacks, meat, and ready-to-eat meals. Answers to the questions on the frequency of intake ranged from 0 (never) to 9 (several times daily). The FFQ was based on the Fit for Delivery study and has been shown to have an adequate level of test-retest reliability [26]. The FFQs in Somali and Urdu were tested for comprehension and appropriateness by conducting qualitative interviews with Somali and Pakistani Norwegian women.
The healthy diet score for Pregnant+ (HDS-P+) was constructed using 9 subscales, with a possible range of 0 to 90. The subscales were constructed on the basis of the dietary recommendations (second point to tenth point) provided in Textbox 1 and consisted of different questions in the FFQ related to the dietary recommendations. The women were asked how often they choose different food groups, with the following answer options: 0=never, 1=less than once a week, 2=once a week, 3=twice, 4=three times, 5=four times, 6=five times, 7=six times, 8=every day, and 9=several times a day.
Information on background characteristics was obtained from the baseline questionnaire and consisted of different socioeconomic variables: age, education, income, country of birth, marital status, economic hardship, and language. Other variables related to pregnancy and health were parity, gestational age at baseline, prior GDM, and perceived health score [23].
Statistical Analysis
Maternal baseline characteristics were compared according to randomization status. The characteristics were presented as mean (SD) for continuous variables (independent sample two-tailed t test) and proportions (%) for categorical variables (χ2 test). Dietary changes from baseline to around gestational week 36 were examined by a paired sample two-tailed t test. A one-way between-group analysis (analysis of covariance) was conducted to measure the effect of the Pregnancy+ app. The dietary behavior after the intervention was examined with adjustment to the baseline values. The HDS-P+ and subscales related to the recommended dietary advice were the dependent variables, and the randomization status (use of the Pregnant+ app or not) was the independent variable. Sensitivity analysis was performed to evaluate the effect of the differences in nonnative and native Norwegian-speaking women between the intervention and control groups at baseline. This did not alter the results and the final model did not adjust for this. Levene test and normality checks were carried out and the assumptions were met. All statistical analyses were performed with SPSS for IBM statistical software package (version 25, IBM Corporation). A two-sided P value of ≤.05 was considered significant.
Power
The power calculation was for the primary outcome for the RCT [23].
Data Exclusion
Figure 1 presents the flowchart for this study. Two women were excluded because of missing dietary data at gestational week 36. No other participant had more than 2 values missing in the 41-item FFQ. The missing data in this study were not imputed.
Results
Participant Characteristics
A total of 238 women were recruited at 5 diabetes outpatient clinics in the southeast region of Norway and randomized to use the Pregnant+ app (intervention group, n=115) or no app (control group, n=123). Figure 1 shows an overview of the final numbers in the dietary analysis. Of the 238 women, 193 (81.1%) women completed the FFQ both at baseline and at gestational week 36. Background characteristics are described according to the randomization status (Table 1). There were no significant baseline differences between the groups, except for more women with a non-Norwegian language as their first language in the intervention group (61 vs 46, P=.02).
Table 1.
Background characteristics at baseline of the participants who provided dietary data at baseline (Q1) and after the intervention (Q2) in the study on the Pregnant+ app.
| Background characteristics | Total, N=193 | Control group, n=98 | Intervention group, n=95 | P value | |
| Age (years), n (%) | .11 | ||||
|
|
≤29 | 47 (24.4) | 22 (22) | 25 (26) |
|
|
|
30-37 | 110 (57.0) | 52 (53) | 58 (61) |
|
|
|
≥38 | 36 (18.7) | 24 (25) | 12 (13) |
|
| Gestational age at baseline, mean (SD) | 27.1 (4.6) | 27.3 (4.6) | 26.9 (4.5) | .66 | |
| Parity, n (%) | .21 | ||||
|
|
Primiparous | 86 (44.6) | 48 (49) | 38 (40) |
|
|
|
Multiparous | 107 (55.4) | 50 (51) | 57 (60) |
|
| Previous GDMa (N=107b), n (%) | .82 | ||||
|
|
No | 75(70.1) | 34 (68) | 41 (72) |
|
|
|
Yes | 32 (29.9) | 16 (32) | 16 (28) |
|
| BMI (N=190c), n (%) | .68 | ||||
|
|
<24.9 | 83 (43.7) | 44 (45) | 39 (42) |
|
|
|
25.0-29.9 | 57 (30.0) | 26 (27) | 31 (33) |
|
|
|
30.0-34.9 | 31 (16.3) | 18 (19) | 13 (14) |
|
|
|
35.0-45.0 | 19 (10.0) | 9 (9) | 10 (11) |
|
| Country of birth, n (%) | .15 | ||||
|
|
Norway | 90 (46.6) | 52 (53) | 38 (40) |
|
|
|
Western Europe + United States of America | 13 (6.7) | 9 (9) | 4 (4) |
|
|
|
Eastern Europe | 18 (9.3) | 9 (9) | 9 (10) |
|
|
|
Asia | 45 (23.3) | 16 (16) | 29 (31) |
|
|
|
Africa | 22 (11.4) | 10 (10) | 12 (13) |
|
|
|
South America | 5 (2.6) | 2 (2) | 3 (3) |
|
| Marital status, n (%) | .62 | ||||
|
|
Married/cohabiting | 179 (92.7) | 90 (92) | 89 (94) |
|
|
|
Single/other | 14 (7.3) | 8 (8) | 6 (6) |
|
| Education, n (%) | .51 | ||||
|
|
Primary school/no education | 19 (9.8) | 12 (12) | 7 (7) |
|
|
|
High school | 40 (20.7) | 23 (24) | 17 (18) |
|
|
|
College/university<4 years | 47 (24.4) | 23 (24) | 24 (25) |
|
|
|
College/university≥4 years | 87 (45.1) | 40 (41) | 47 (50) |
|
| Smoking or wet tobacco , n (%) | .69 | ||||
|
|
No | 189 (97.9) | 96 (98) | 93 (98) |
|
|
|
Yes | 4 (2.1) | 2 (2) | 2 (2) |
|
| Main activity, n (%) | .22 | ||||
|
|
Employed or self-employed | 147 (76.2) | 71 (72) | 76 (80) |
|
|
|
Not employed or not self-employed | 46 (23.8) | 27 (28) | 19 (20) |
|
| Joined income, n (%) | .78 | ||||
|
|
≤59,900 USD | 57 (29.9) | 26 (27) | 31 (33) |
|
|
|
60,000-79,900 USD | 28 (14.2) | 14 (14) | 14 (15) |
|
|
|
80,000-99,900 USD | 39 (19.8) | 20 (20) | 19 (20) |
|
|
|
≥100,000 USD | 35 (18.8) | 20 (20) | 15 (16) |
|
|
|
I don’t know | 34 (17.3) | 18 (18) | 16 (17) |
|
| Economic hardship (N=188c), n (%) | .85 | ||||
|
|
No | 58 (30.9) | 29 (30) | 29 (32) |
|
|
|
Yes | 130 (69.1) | 67 (70) | 63 (69) |
|
| Language, n (%) | .02 | ||||
|
|
Native Norwegian-speaking | 86 (45.1) | 52 (53) | 34 (36) |
|
|
|
Nonnative Norwegian-speaking | 107 (54.9) | 46 (47) | 61 (64) |
|
| Perceived health score (0-100), mean (SD) | 70.8 (19.7) | 70.5 (20.5) | 71.2 (18.9) | .80 | |
aGDM: gestational diabetes mellitus.
bAmong multiparous women only.
cSome values are missing.
Outcomes
Dietary Outcomes Around Gestational Week 36
Overall, the total HDS-P+ and most of the subscales, except the intake of healthy oils, improved from baseline to gestational week 36 (Table 2).
Table 2.
Dietary changes from baseline to gestational week 36.a
| Subscales | Baseline values, mean (SD) | Week 36 values, mean (SD) | P value | |
| 1. HDS-P+b | 40.36 (14.11) | 55.56 (13.70) | <.001 | |
| 2. Sugar (times/week) | 10.10 (7.88) | 1.89 (3.21) | <.001 | |
| 3. Vegetables (times/week) | 8.87 (3.52) | 10.35 (3.5) | <.001 | |
| 4. Whole grains (times/week) | 6.71 (2.96) | 8.87 (2.78) | <.001 | |
| 5. Salt (times/week) | 3.71 (3.10) | 2.39 (2.49) | <.001 | |
| 6. Fish (times/week) | 1.84 (1.17) | 2.21 (1.32) | <.001 | |
| 7. Low-fat milk (times/week) | 4.84 (4.08) | 4.22 (3.34) | .02 | |
| 8. Healthy oil (% of total dietary fat)c | 62.41 (25.32) | 65.09 (25.36) | .11 | |
| 9. Read nutrition labels | 5.78 (3.44) | 8.45 (2.64) | <.001 | |
| 10. Water (% of total fluid intake)c | 40.15 (14.67) | 51.21 (17.35) | <.001 | |
aPaired sample two-tailed t test.
bHDS-P+: healthy dietary score for Pregnant+.
cPercentage of weekly consumption.
Between-Group Differences After Intervention
A one-way between-group analysis of covariance was conducted to compare the effectiveness of the app on the participants’ dietary habits after being diagnosed with GDM. The women’s HDS-P+ preintervention was used as the covariate in the analysis. Table 3 presents the between-group differences for the overall HDS-P+ and the 9 different subscales at gestational week 36. No significant differences favored the intervention group. The analysis showed that the control group reported to eat more fish meals per week (P=.05). No other significant differences were found between the intervention and control groups.
Table 3.
Between-group differences in 10 dietary domains reported after the intervention (gestational week 36) in the Pregnant+ app.
| Dietary domain | Subscale(s) | Control group, n=98, mean (SE) | Intervention group, n=95, mean (SE) | Estimated difference after interventiona, mean (SE) | 95% CI | P value |
| Eat healthy | HDS-P+b | 56.11 (1.11) | 55.34 (1.13) | 0.77 (1.72) | –2.62, 4.16 | .65 |
| Eat and drink little sugar | Sugar (times/week) | 1.97 (0.31) | 1.79 (0.32) | 0.18 (0.45) | –0.70, 1.06 | .68 |
| Eat more vegetables | Vegetables (times/week) | 10.40 (0.32) | 10.30 (0.32) | 0.09 (0.45) | –0.83, 0.95 | .86 |
| Choose whole grains | Whole grains (times/week) | 8.23 (0.27) | 8.01 (0.28) | 0.14 (0.40) | –0.79, 0.99 | .73 |
| Limit your intake of salt | Salt (times/week) | 2.53 (0.12) | 2.25 (0.21) | 0.28 (0.31) | –0.31, 0.88 | .35 |
| Eat enough fish | Fish (times/week) | 2.34 (0.09) | 2.09 (0.09) | 0.26 (0.13) | –0.01, 0.51 | .05 |
| Choose lean dairy milk | Low-fat milk (times/week) | 4.40 (0.28) | 4.04 (2.85) | 0.35 (0.40) | –0.42, 1.14 | .38 |
| Eat less saturated fat | Healthy oil (% of total dietary fat)c | 66.30 (2.05) | 63.80 (2.10) | 2.50 (2.50) | –3.31, 8.33 | .40 |
| Read nutrition labels | Read labels | 8.76 (0.25) | 8.13 (0.25) | 0.63 (0.36) | –0.07, 1.33 | .08 |
| Choose water | Water (% of total fluid intake) c | 51.93 (1.57) | 50.47 (1.59) | 1.46 (2.24) | –2.69, 5.89 | .57 |
aAnalysis of covariance adjusted for baseline HDS-P+.
bHDS-P+: healthy dietary score for Pregnant+.
cPercentage of weekly consumption.
Discussion
Principal Results
The Pregnant+ app combined with usual care did not have any significant effect on the dietary behavior of the participants during pregnancy compared to the dietary behavior of the participants receiving usual care only. All the participants improved their diet from the time they were diagnosed with GDM to gestational week 36.
Comparison With Prior Work
This study adds to the literature on the development and effect of pregnancy-related apps for the management of GDM and for following a healthy diet [22,27,28]. Pregnant women consider these apps to be useful and convenient for nutrition information and management of their diets [27]; however, little is known about their effects on the dietary behavior [19]. mHealth apps may provide several functions targeting behavior change or monitoring. The most successful smartphone-based interventions for dietary change and health outcomes include elements of self-monitoring and personalized feedback [29]. Similar to other apps for women with GDM [21,30], the Pregnant+ app includes a function for self-monitoring of blood glucose levels. According to our qualitative study on women’s experience with the Pregnant+ app, the self-management of blood glucose levels was the most important aspect of the app for increasing self-awareness and motivation [31]. Ten of the 17 participants from the intervention group reported to use the Pregnant+ app daily for their blood glucose management. However, the monitoring of food intake was not possible in the app. A qualitative study about the acceptability of a smartphone app for patients with type 2 diabetes indicated that the use of a digital diabetes diary to monitor food intake supported them in eating a healthy diet [32]. Dodd et al [20] assessed the effect of a smartphone app on the dietary behavior of pregnant women. Their app included a combination of information provision, goal setting, feedback, and self-monitoring. The use of the app was poor, and it provided no additional benefit over face-to-face consultation and printed materials in improving dietary behaviors [20]. It should also be considered that adherence to self-monitoring has been shown to decrease over time and that self-monitoring is successful only when people are regularly reminded to use the app [33]. The women in our intervention group were not reminded to use the app.
Compared to studies demonstrating the positive impact of apps on healthy eating and blood glucose levels [29,34,35], the Pregnant+ app did not have any personal interaction with the women. For instance, a review on the use of telemedicine technology for managing diabetes in pregnancy (not just GDM) showed a modest but statistically significant improvement in HbA1c levels [35]. To avoid bias, the health care professionals were not asked to use the app actively during their consultations. However, the women automatically received specific dietary information when registering too high blood glucose levels in the Pregnant+ app. The women in our qualitative study wanted more involvement of the health care professionals in the usage of the app. In an RCT involving 203 pregnant women in the United Kingdom, women with access to a smartphone app had a higher level of satisfaction with care than the women in the control group [17]. In this study, the midwives checked the women’s registered blood glucose levels in the app 3 times a week and sent feedback via SMS text messaging [17].
Similar to that reported in other mHealth studies [36], technical problems with the app could be a reason for us to not find any effect of the app on the participants’ diets. Some of them experienced problems with the automatic transfer of the blood glucose levels [31]. A cross-sectional survey on the use of mHealth among Latino patients with diabetes found that the lack of operability between the smartphone app and other devices could serve as a barrier to using the app [37].
All the participants in this study improved their diet after being diagnosed with GDM. This is in accordance with previous research, indicating that the diagnosis of GDM motivates women to change their diets [38-40]. Our previous study about women’s dietary habits prior to being diagnosed with GDM showed low adherence to national dietary recommendations [41]. A significantly higher proportion of nonnative Norwegian-speaking women had a high healthy diet score compared with native Norwegian-speaking women. In this study, significantly more women with a non-Norwegian language as their first language were in the intervention group (P=.02). Previous research has shown that a combination of technological, health literacy, and language issues may result in a lower uptake of pregnancy apps among immigrant women [16]. These barriers may also have led to a lower usage of the Pregnant+ app.
Limitations
One of the main limitations of this study was that we did not have access to usage logs because of technical problems. To secure the participants’ privacy, we did not collect any additional data from the app. We do not know if those in the intervention group actually used the Pregnant+ app or about their frequency of usage or the pages in the app accessed by them. Our qualitative study on 17 participants from the intervention group showed that some women used the app regularly and some did not use it at all because of technical problems [31]. Patients participating in a study will often experience an effect even when not receiving the intervention—the Hawthorne effect. In our study, this could account for the lack of effects as women not using the app may have focused more on a healthy diet as a result of participating in a study. The data for this study were derived from self-completed questionnaires, which include the possibility for recall bias. Social desirability might have biased the self-report of dietary intake. The FFQ covered only selected aspects of the overall diet. Thus, the difference in the HDS-P+ should not be interpreted as an absolute measure of dietary change [42].
Conclusions
To our knowledge, this is one of the first studies to evaluate the effect of a smartphone app on the dietary behavior of women with GDM [17]. Our findings do not support the supplementation of face-to-face follow-up of women with GDM with a smartphone app in the presence of high-standard usual care. However, the app might be a useful tool for women who do not receive sufficient dietary counselling in person. Future research should explore the effects of various technological features provided in a smartphone app to improve the care of women with GDM.
Acknowledgments
This study was funded by the Norwegian Research Council (identifier: 228517). We also acknowledge the participating women as well as the health care professionals and project members involved in the recruitment process.
Abbreviations
- FFQ
food frequency questionnaire
- GDM
gestational diabetes mellitus
- HDS-P+
healthy diet score for Pregnant+
- mHealth
mobile health
- OGTT
oral glucose tolerance test
- RCT
randomized controlled trial
Appendix
Screenshot of the app.
Screenshot of the dietary recommendation in the app.
CONSORT-EHEALTH Checklist (V 1.6.1).
Footnotes
Authors' Contributions: LGH wrote the manuscript. LH and LET conducted all statistical analysis. All authors planned the study and reviewed the final manuscript.
Conflicts of Interest: None declared.
References
- 1.The World Health Organization. WHO recommendation on the diagnosis of gestational diabetes in pregnancy. Geneva, Switzerland: The WHO Reproductive Health Library; 2016. [2019-12-04]. https://tinyurl.com/y4lprrxw. [Google Scholar]
- 2.Rani PR, Begum J. Screening and Diagnosis of Gestational Diabetes Mellitus, Where Do We Stand. J Clin Diagn Res. 2016 Apr;10(4):QE01–4. doi: 10.7860/JCDR/2016/17588.7689. http://europepmc.org/abstract/MED/27190902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Medical Birth Registry Norway, The Medical Birth Registry Norway. 2018. [2019-12-04]. https://www.fhi.no/hn/helseregistre-og-registre/mfr/
- 4.Jenum AK, Diep LM, Holmboe-Ottesen G, Holme IMK, Kumar BN, Birkeland KI. Diabetes susceptibility in ethnic minority groups from Turkey, Vietnam, Sri Lanka and Pakistan compared with Norwegians - the association with adiposity is strongest for ethnic minority women. BMC Public Health. 2012 Mar 01;12:150. doi: 10.1186/1471-2458-12-150. https://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-12-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Makgoba M, Savvidou MD, Steer PJ. An analysis of the interrelationship between maternal age, body mass index and racial origin in the development of gestational diabetes mellitus. BJOG. 2012 Feb;119(3):276–82. doi: 10.1111/j.1471-0528.2011.03156.x. doi: 10.1111/j.1471-0528.2011.03156.x. [DOI] [PubMed] [Google Scholar]
- 6.Schneider S, Hoeft B, Freerksen N, Fischer B, Roehrig S, Yamamoto S, Maul H. Neonatal complications and risk factors among women with gestational diabetes mellitus. Acta Obstet Gynecol Scand. 2011 Mar;90(3):231–7. doi: 10.1111/j.1600-0412.2010.01040.x. doi: 10.1111/j.1600-0412.2010.01040.x. [DOI] [PubMed] [Google Scholar]
- 7.Aziz S, Munim TF, Fatima SS. Post-partum follow-up of women with gestational diabetes mellitus: effectiveness, determinants, and barriers. J Matern Fetal Neonatal Med. 2018 Jun;31(12):1607–1612. doi: 10.1080/14767058.2017.1321630. [DOI] [PubMed] [Google Scholar]
- 8.Plows JF, Stanley JL, Baker PN, Reynolds CM, Vickers MH. The Pathophysiology of Gestational Diabetes Mellitus. Int J Mol Sci. 2018 Oct 26;19(11) doi: 10.3390/ijms19113342. https://www.mdpi.com/resolver?pii=ijms19113342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Landon MB, Spong CY, Thom E, Carpenter MW, Ramin SM, Casey B, Wapner RJ, Varner MW, Rouse DJ, Thorp JM, Sciscione A, Catalano P, Harper M, Saade G, Lain KY, Sorokin Y, Peaceman AM, Tolosa JE, Anderson GB, Eunice Kennedy Shriver National Institute of Child HealthHuman Development Maternal-Fetal Medicine Units Network A multicenter, randomized trial of treatment for mild gestational diabetes. N Engl J Med. 2009 Oct 01;361(14):1339–48. doi: 10.1056/NEJMoa0902430. http://europepmc.org/abstract/MED/19797280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.American Diabetes Association Management of Diabetes in Pregnancy. Diabetes Care. 2017;40(Suppl 1):S114–S119. doi: 10.2337/dc17-S016. [DOI] [PubMed] [Google Scholar]
- 11.Schiavo R. Health communication: from theory to practice. 1st ed. San Francisco, CA: Jossey-Bass; 2007. [Google Scholar]
- 12.Carolan M, Gill GK, Steele C. Women's experiences of factors that facilitate or inhibit gestational diabetes self-management. BMC Pregnancy Childbirth. 2012 Sep 18;12:99. doi: 10.1186/1471-2393-12-99. https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/1471-2393-12-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Borgen I, Garnweidner-Holme LM, Jacobsen AF, Fayyad S, Cvancarova Småstuen Milada, Lukasse M. Knowledge of gestational diabetes mellitus at first consultation in a multi-ethnic pregnant population in the Oslo region, Norway - a cross-sectional study. Ethn Health. 2019 Aug 16;:1–14. doi: 10.1080/13557858.2019.1655530. [DOI] [PubMed] [Google Scholar]
- 14.Frequently asked questions on global task force on digital health for TB and its work. World Health Organization. [2020-09-09]. http://www.who.int/tb/areas-of-work/digital-health/faq/en/
- 15.Chan KL, Chen M. Effects of Social Media and Mobile Health Apps on Pregnancy Care: Meta-Analysis. JMIR Mhealth Uhealth. 2019 Jan 30;7(1):e11836. doi: 10.2196/11836. https://mhealth.jmir.org/2019/1/e11836/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen Q, Carbone ET. Functionality, Implementation, Impact, and the Role of Health Literacy in Mobile Phone Apps for Gestational Diabetes: Scoping Review. JMIR Diabetes. 2017 Oct 04;2(2):e25. doi: 10.2196/diabetes.8045. https://diabetes.jmir.org/2017/2/e25/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mackillop L, Hirst JE, Bartlett KJ, Birks JS, Clifton L, Farmer AJ, Gibson O, Kenworthy Y, Levy JC, Loerup L, Rivero-Arias O, Ming W, Velardo C, Tarassenko L. Comparing the Efficacy of a Mobile Phone-Based Blood Glucose Management System With Standard Clinic Care in Women With Gestational Diabetes: Randomized Controlled Trial. JMIR Mhealth Uhealth. 2018 Mar 20;6(3):e71. doi: 10.2196/mhealth.9512. https://mhealth.jmir.org/2018/3/e71/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Borgen I, Småstuen Milada Cvancarova, Jacobsen AF, Garnweidner-Holme LM, Fayyad S, Noll J, Lukasse M. Effect of the Pregnant+ smartphone application in women with gestational diabetes mellitus: a randomised controlled trial in Norway. BMJ Open. 2019 Nov 11;9(11):e030884. doi: 10.1136/bmjopen-2019-030884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Overdijkink SB, Velu AV, Rosman AN, van Beukering Monique Dm, Kok M, Steegers-Theunissen RP. The Usability and Effectiveness of Mobile Health Technology-Based Lifestyle and Medical Intervention Apps Supporting Health Care During Pregnancy: Systematic Review. JMIR Mhealth Uhealth. 2018 Apr 24;6(4):e109. doi: 10.2196/mhealth.8834. https://mhealth.jmir.org/2018/4/e109/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dodd JM, Louise J, Cramp C, Grivell RM, Moran LJ, Deussen AR. Evaluation of a smartphone nutrition and physical activity application to provide lifestyle advice to pregnant women: The SNAPP randomised trial. Matern Child Nutr. 2018 Jan;14(1) doi: 10.1111/mcn.12502. http://europepmc.org/abstract/MED/28836373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Garnweidner-Holme LM, Borgen I, Garitano I, Noll J, Lukasse M. Designing and Developing a Mobile Smartphone Application for Women with Gestational Diabetes Mellitus Followed-Up at Diabetes Outpatient Clinics in Norway. Healthcare (Basel) 2015 May 21;3(2):310–23. doi: 10.3390/healthcare3020310. https://www.mdpi.com/resolver?pii=healthcare3020310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hughson JP, Daly JO, Woodward-Kron R, Hajek J, Story D. The Rise of Pregnancy Apps and the Implications for Culturally and Linguistically Diverse Women: Narrative Review. JMIR Mhealth Uhealth. 2018 Nov 16;6(11):e189. doi: 10.2196/mhealth.9119. https://mhealth.jmir.org/2018/11/e189/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Borgen I, Garnweidner-Holme LM, Jacobsen AF, Bjerkan K, Fayyad S, Joranger P, Lilleengen AM, Mosdøl Annhild, Noll J, Småstuen Milada Cvancarova, Terragni L, Torheim LE, Lukasse M. Smartphone application for women with gestational diabetes mellitus: a study protocol for a multicentre randomised controlled trial. BMJ Open. 2017 Mar 27;7(3):e013117. doi: 10.1136/bmjopen-2016-013117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Holan S, Matheison M, Petersen K. A national clinical guideline for antenatal care. Short version. Norway, Oslo: Directorate for Health and Social Affairs; 2005. [Google Scholar]
- 25.Henriksen T, Thordardson H, Strøm-Raoum E. Svangerskapsdiabetes. Website. 2014. [2019-12-13]. http://legeforeningen.no/Fagmed/Norsk-gynekologisk-forening/Veiledere/Veileder-ifodselshjelp-2014/Diabetes-i-svangerskapet/
- 26.Øverby Nina C, Hillesund ER, Sagedal LR, Vistad I, Bere E. The Fit for Delivery study: rationale for the recommendations and test-retest reliability of a dietary score measuring adherence to 10 specific recommendations for prevention of excessive weight gain during pregnancy. Matern Child Nutr. 2015 Jan;11(1):20–32. doi: 10.1111/mcn.12026. http://europepmc.org/abstract/MED/23241065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang N, Deng Z, Wen LM, Ding Y, He G. Understanding the Use of Smartphone Apps for Health Information Among Pregnant Chinese Women: Mixed Methods Study. JMIR Mhealth Uhealth. 2019 Jun 18;7(6):e12631. doi: 10.2196/12631. https://mhealth.jmir.org/2019/6/e12631/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lupton D, Pedersen S. An Australian survey of women's use of pregnancy and parenting apps. Women Birth. 2016 Aug;29(4):368–75. doi: 10.1016/j.wombi.2016.01.008. [DOI] [PubMed] [Google Scholar]
- 29.Kankanhalli A, Shin J, Oh H. Mobile-Based Interventions for Dietary Behavior Change and Health Outcomes: Scoping Review. JMIR Mhealth Uhealth. 2019 Jan 21;7(1):e11312. doi: 10.2196/11312. https://mhealth.jmir.org/2019/1/e11312/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hirst JE, Mackillop L, Loerup L, Kevat DA, Bartlett K, Gibson O, Kenworthy Y, Levy JC, Tarassenko L, Farmer A. Acceptability and user satisfaction of a smartphone-based, interactive blood glucose management system in women with gestational diabetes mellitus. J Diabetes Sci Technol. 2015 Jan;9(1):111–5. doi: 10.1177/1932296814556506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Skar JB, Garnweidner-Holme LM, Lukasse M, Terragni L. Women's experiences with using a smartphone app (the Pregnant+ app) to manage gestational diabetes mellitus in a randomised controlled trial. Midwifery. 2018 Mar;58:102–108. doi: 10.1016/j.midw.2017.12.021. [DOI] [PubMed] [Google Scholar]
- 32.Torbjørnsen Astrid, Ribu L, Rønnevig Marit, Grøttland Astrid, Helseth S. Users' acceptability of a mobile application for persons with type 2 diabetes: a qualitative study. BMC Health Serv Res. 2019 Sep 06;19(1):641. doi: 10.1186/s12913-019-4486-2. https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-019-4486-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McCarroll R, Eyles H, Ni Mhurchu Cliona. Effectiveness of mobile health (mHealth) interventions for promoting healthy eating in adults: A systematic review. Prev Med. 2017 Dec;105:156–168. doi: 10.1016/j.ypmed.2017.08.022. [DOI] [PubMed] [Google Scholar]
- 34.Radhakrishnan K. The efficacy of tailored interventions for self-management outcomes of type 2 diabetes, hypertension or heart disease: a systematic review. J Adv Nurs. 2012 Mar;68(3):496–510. doi: 10.1111/j.1365-2648.2011.05860.x. [DOI] [PubMed] [Google Scholar]
- 35.Ming W, Mackillop LH, Farmer AJ, Loerup L, Bartlett K, Levy JC, Tarassenko L, Velardo C, Kenworthy Y, Hirst JE. Telemedicine Technologies for Diabetes in Pregnancy: A Systematic Review and Meta-Analysis. J Med Internet Res. 2016 Nov 09;18(11):e290. doi: 10.2196/jmir.6556. https://www.jmir.org/2016/11/e290/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kreps GL, Neuhauser L. New directions in eHealth communication: opportunities and challenges. Patient Educ Couns. 2010 Mar;78(3):329–36. doi: 10.1016/j.pec.2010.01.013. [DOI] [PubMed] [Google Scholar]
- 37.Arora S, Ford K, Terp S, Abramson T, Ruiz R, Camilon M, Coyne CJ, Lam CN, Menchine M, Burner E. Describing the evolution of mobile technology usage for Latino patients and comparing findings to national mHealth estimates. J Am Med Inform Assoc. 2016 Sep;23(5):979–83. doi: 10.1093/jamia/ocv203. http://europepmc.org/abstract/MED/26995564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Atakora L, Poston L, Hayes L, Flynn AC, White SL. Influence of GDM Diagnosis and Treatment on Weight Gain, Dietary Intake and Physical Activity in Pregnant Women with Obesity: Secondary Analysis of the UPBEAT Study. Nutrients. 2020 Jan 30;12(2) doi: 10.3390/nu12020359. https://www.mdpi.com/resolver?pii=nu12020359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jelsma JGM, van Leeuwen KM, Oostdam N, Bunn C, Simmons D, Desoye G, Corcoy R, Adelantado JM, Kautzky-Willer A, Harreiter J, van Assche FA, Devlieger R, Timmerman D, Hill D, Damm P, Mathiesen ER, Wender-Ozegowska E, Zawiejska A, Rebollo P, Lapolla A, Dalfrà Maria G, Del Prato S, Bertolotto A, Dunne F, Jensen DM, Andersen LLT, Snoek FJ, van Poppel MNM. Beliefs, Barriers, and Preferences of European Overweight Women to Adopt a Healthier Lifestyle in Pregnancy to Minimize Risk of Developing Gestational Diabetes Mellitus: An Explorative Study. J Pregnancy. 2016;2016:3435791. doi: 10.1155/2016/3435791. doi: 10.1155/2016/3435791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jones EJ, Roche CC, Appel SJ. A review of the health beliefs and lifestyle behaviors of women with previous gestational diabetes. J Obstet Gynecol Neonatal Nurs. 2009;38(5):516–26. doi: 10.1111/j.1552-6909.2009.01051.x. [DOI] [PubMed] [Google Scholar]
- 41.Garnweidner-Holme Lisa, Torheim LE, Henriksen L, Borgen I, Holmelid S, Lukasse M. Adherence to the Norwegian dietary recommendations in a multi-ethnic pregnant population prior to being diagnosed with gestational diabetes mellitus. Food Sci Nutr. 2020 Jul;8(7):3031–3040. doi: 10.1002/fsn3.1248. doi: 10.1002/fsn3.1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hillesund ER, Bere E, Sagedal LR, Vistad I, Øverby N C. Effect of a diet intervention during pregnancy on dietary behavior in the randomized controlled Norwegian Fit for Delivery study. J Dev Orig Health Dis. 2016 Oct;7(5):538–547. doi: 10.1017/S2040174416000258. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Screenshot of the app.
Screenshot of the dietary recommendation in the app.
CONSORT-EHEALTH Checklist (V 1.6.1).


