Abstract
Purpose
To evaluate the intraocular pressure (IOP)-lowering effect of a multi-pressure dial (MPD) at targeted negative pressure settings.
Methods
Prospective, intrasubject controlled study of 65 healthy subjects randomized to receive no negative pressure for 60 minutes or negative pressure application at designated levels of 25%, 50%, and 75% of baseline IOP for 20 minutes each. The main outcome measure was mean IOP with application of negative pressure.
Results
In the study eye group, from a baseline IOP of 15.8 ± 3.6 mm Hg, the mean IOP was 13.5 ± 3.4, 11.5 ± 3.1, and 10.2 ± 2.7 mm Hg with negative pressure settings of 25%, 50% and 75%, respectively. In the control eye group, from a baseline IOP of 15.5 ± 3.0 mm Hg, the mean IOP values at the same time points, without negative pressure, were 15.6 ± 3.0, 15.5 ± 2.5 and 15.3 ± 2.4 mm Hg. The difference between the mean IOPs of the two groups was significantly different at all negative pressure settings (P < 0.001) in comparison with baseline. There was one minor adverse event, a corneal abrasion, that was unrelated to device wear.
Conclusions
Negative pressure application to the periocular space with a multi-pressure dial can produce titratable IOP reduction while the device is worn with active negative pressure. To our knowledge, this technology represents the first nonpharmacologic, nonlaser, nonsurgical method for IOP reduction.
Translational Relevance
This represents the first study demonstrating the IOP-lowering ability of the multi-pressure dial, a device that uses a novel IOP-lowering strategy by delivering negative pressure to the periocular region.
Keywords: open-angle glaucoma, normal tension glaucoma, severe open-angle glaucoma, multi-pressure dial, MPD, multi-pressure glaucoma management, CSF pressure
Introduction
Glaucoma is the second leading cause of global blindness.1,2 Currently, intraocular pressure (IOP) remains the only modifiable and clinically validated risk factor with conventional treatment strategies for glaucoma aimed at lowering IOP.3,4 Even with the emergence of new treatment options,5–7 many patients do not achieve sufficient IOP reduction with current therapies and exhibit disease progression despite maintenance of seemingly controlled IOP values.8 The current treatment options for IOP reduction include medications, laser procedures, and a variety of surgical procedures or implants.9–11 Although notable innovation has occurred across the glaucoma treatment landscape, currently available treatments still have limitations and often require the clinician to weigh effectiveness against safety.
In this study, we evaluate the multi-pressure dial (MPD; Equinox Ophthalmic, Inc., CA). The MPD consists of a pair of goggles connected to a pressure-modulating pump. When the goggles are securely worn over the eyes of a subject, negative pressure (or vacuum) is applied to produce a localized decrease in the atmospheric pressure contacting the surface of the eye. Upon programming a specified negative pressure into the pump and fitting the goggles to achieve a complete seal, the localized negative pressure microenvironment created leads to a corresponding reduction in IOP.12 The design of the MPD, which includes right and left periorbital goggle compartments individually connected to the pressure-modulating pump, allows for titratable, negative pressure application to each eye separately. To our knowledge, this is the first device that uses localized negative pressure to the periocular space to decrease the IOP.
Favorable results regarding the safety and tolerability of the MPD device for up to 8 hours of wear time have been demonstrated in prior studies.13,14 The IOP-lowering capability of localized negative pressure to the periocular space using the MPD has not been investigated or reported in prior work. The goal of this study was to evaluate the IOP-lowering capability of the MPD at multiple negative pressure settings.
Methods
Subjects
In this prospective, randomized, controlled, open-label study, 65 subjects (130 eyes) were enrolled and successfully completed the duration of the study. Twenty-five subjects did not adequately meet inclusion/exclusion criteria and did not enter the study. Of the 25 subjects that failed screening, 11 were either unable to cooperate for repeated IOP measurements via pneumatonometry or were unable to achieve a secure fit with the goggles. The other subjects that failed screening occurred owing to reasons listed in the exclusion criteria. After entry, the study eye was randomized to receive negative pressure application, and the contralateral eye served as an intrasubject control. This study was approved by the Aspire Institutional Review Board (Santee, CA) and was performed at a single site (Vance Thompson Vision, Sioux Falls, SD). Written consent was obtained before participation in the study.
Key inclusion criteria were subjects 18 years of age or older with orbital anatomy that permitted a proper seal when the goggles are placed over the eyes and an ability to tolerate IOP measurements with the MPD in place. Exclusion criteria included the presence or history of any eye disease or condition that could interfere with the assessment of the study results or subject safety. Subjects with glaucoma in either eye, macular degeneration, retinal detachment, or other fundus findings that could inhibit visualization of the retina in either eye were excluded. Subjects with eyelid edema or conjunctival chemosis in either eye, history of corneal transplant in either eye, or history of allergy to any of the testing materials (e.g., silicone) were excluded, as were female subjects who were pregnant or lactating during the time of the study.
A summary of the visit schedule with the clinical assessments and when they were performed is included in Table 1. The visits included screening, day 0, and week 1. Screening and day 0 (testing) could be performed on the same day.
Table 1.
Overview of the Study Design and When Specific Diagnostic Occurred During the Screening, Study Period, and 1-Week Follow-up Visits
| Screening | Baseline/Day 0 | Week 1 | ||||
|---|---|---|---|---|---|---|
| Procedure | MPD Off | MPD Off | MPD On, Negative Pressure off | MPD on, Negative Pressure on | MPD Off | MPD Off |
| MPD check and sensitivity to pneumatonometry | X | |||||
| Informed consent | X | |||||
| Manifest refraction | OU | OU | ||||
| BCVA | OU | OU | ||||
| SLE | OU | OU | ||||
| OPTIC nerve assessment (OCT RNFL) | OU | OU | ||||
| Reichert model 30 pneumatonometry | OU1 | OU | OU | OU | OU2 | |
| CH via ORA | OU | OU | ||||
| Visual field | OU | OU | ||||
| Subjective assessment | X | X | X | |||
| Adverse event assessment | X | X | X | X | ||
Control eyes will not receive application of negative pressure.
Measured with MPD off only, one measurement.
Abbreviations: X = action performed; blank spaces = not performed; BCVA = best-corrected visual acuity; SLE = slit lamp examination; OCT RNFL = optical coherence tomography retinal nerve fiber layer; ORA = ocular response analyzer; OU = both eyes.
Study Design
Study participants were recruited from the local population where the study was performed (Sioux Falls, SD). Subjects who met eligibility criteria were enrolled and the study eye was determined by randomization and the contralateral eye from each subject served as an intrasubject control. Randomization occurred via a randomization schedule generated by a statistician.
All subjects underwent a baseline ophthalmological exam. The examination included the following diagnostic tests: best-corrected distance visual acuity, OCT of the retinal nerve fiber layer, IOP, visual field (24-2 SITA Fast utilizing Humphrey Visual Field), and corneal hysteresis (CH). IOP measurement was obtained via Reichert Model 30 Pneumatonometry. CH was collected via the Ocular Response Analyzer (Reichert, NY). In addition, a comprehensive slit lamp and dilated fundus examination were performed.
All baseline tests were performed before device exposure. Before application of negative pressure, subjects were fitted with the MPD to obtain a proper seal. This study included a specially adapted version of the goggles, referred to as the Excursion MPD model (shown in Fig. 1), that allowed pneumatonometry measurements during negative pressure application. This method of IOP measurement, also known as the excursion test method (shown in Fig. 2), was described in a prior study with favorable results, supporting its use as an accurate and reliable form of IOP measurement.15 To obtain IOP measurements with the excursion test method, a silicone support tube and Tono-Pen cover is placed within the access port of the goggle lens with the proximal end (containing the Tono-Pen cover) gently contacting the corneal surface. Through the open, distal end, the pneumatonometer tip is inserted and placed against the Tono-Pen cover on the cornea to measure IOP.
Figure 1.

Excursion MPD, an adaptation of the MPD that allows for IOP measurement while negative pressure is active, which includes the goggles and the pressure-modulating pump with crush-resistant tubing that permits independent negative pressure settings for each eye.
Figure 2.
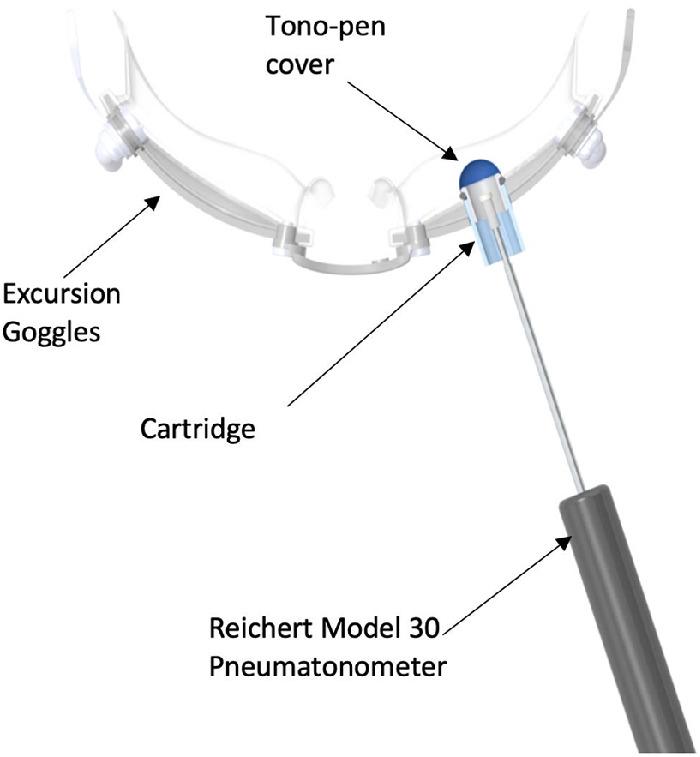
How the pneumatonometer is inserted through the access port on the Excursion MPD, a modified version of the MPD that facilitates IOP measurement during wear via pneumatonometry across a Tono-Pen tip cover acting as a membrane.
Before application of negative pressure, two IOP measurements were obtained. The first IOP measurement was obtained before wear of the device. The second measurement occurred with the MPD goggles securely positioned but before application of negative pressure to establish a baseline measurement in both the study and the control eye for comparison with negative pressure application and to ensure there was no increase in IOP by securely placing the goggles on the subject. Multiple negative pressure levels were programmed and applied according to the predesignated schedule described in Table 2: 25% of baseline IOP for 20 minutes, 50% of baseline IOP for 20 minutes, and 75% of baseline IOP for 20 minutes (not to exceed 20 mm Hg of negative pressure). For example, a patient's study eye with a baseline IOP of 20 mm Hg was programmed for –5 mm Hg at the 25% setting and –10 mm Hg at the 50% setting and –15 mm Hg at the 75% setting. Of note, our prior work has demonstrated that a decrease in atmospheric pressure does not translate to a 1:1 decrease in IOP and, hence, we would not expect a subject with a baseline IOP of 20 mm Hg programmed for 75% negative pressure to achieve a reduction in IOP down to 5 mm Hg. IOP measurements were obtained at each negative pressure setting, and the mean value was used for analysis; IOP measurements occurred using the excursion test method. At each negative pressure setting, measurements were obtained immediately after the application of negative pressure at each negative pressure setting and at the end of each 20-minute segment. Control eyes underwent the exact same IOP measurements, but without active negative pressure at each stage for comparison.
Table 2.
Timeline and Overview of the Vacuum (Negative Pressure) Application During the Study Period
| Time | MPD | Vacuum (Negative Pressure) |
|---|---|---|
| Baseline | Off | Off |
| Baseline | On | Off |
| PUMP negative pressure setting adjusted to 25% of baseline IOP | ||
| 0–20 min* | 25% reduction from baseline IOP | On |
| PUMP negative pressure setting adjusted to 50% of baseline IOP | ||
| 20–40 min* | 50% reduction from baseline IOP | On |
| PUMP negative pressure setting adjusted to 75% of baseline IOP (not to exceed 20 mm Hg) | ||
| 40–60 min* | 75% reduction from baseline IOP (not to exceed 20 mm Hg) | On |
| MPD OFF | ||
| 60–62 min | Off | Off |
IOP measurements occurred at the beginning and end of each 20-minute segment with negative pressure active.
Immediately after the completion of negative pressure application with the MPD (day 0) and device removal, IOP measurements were repeated in both control and study eyes via pneumatonometry. A slit lamp examination was also performed to assess any potential adverse events and a subjective assessment was administered to subjects immediately after the study period on the same day as the application of negative pressure with the MPD. The subject assessment aimed to assess overall comfort of the device during application of negative pressure; the scale used was 1 to 10 with 10 signifying most comfortable and 1 signifying least comfortable. Subjects were also asked to report issues with tolerability. Subjects returned once again within 1 week (5–8 days) of day 0 to repeat all baseline assessments, including IOP measurements.
Statistical Analysis
Analysis was performed using a repeated-measures analysis of variance procedure to evaluate the difference between the IOP measurements of the study and control eye at each of the three programmed negative pressure settings (ie, 25%, 50%, 75%) in addition to baseline (MPD goggles fitted but without negative pressure). The analyses evaluated the difference in IOP between the study and control eye where subject data are treated as dependent. A post hoc analysis was performed using paired t-tests to evaluate the difference in IOP between the study and control eye at each negative pressure setting in comparison with baseline. In addition, a paired t-test was performed at baseline (before negative pressure with the MPD securely placed) to compare the IOP values of the study and control eye at baseline before application of negative pressure. To account for the potential inflation of type I error with multiple t-tests, a Benjamini–Hochberg correction was used.
Analysis of variance was also performed to evaluate the difference between the IOP of the study and control eye at baseline before wear of the goggles, immediately following the application of negative pressure (1 hour) and at the 1-week follow-up visit. Of note, all of the IOP measurements included in this analysis were without wear of the goggles. All statistical analysis was performed using Python software (Python Software Foundation, Wilmington, DE).
Results
A total of 65 subjects (130 eyes) entered and completed the duration of the study. The mean age of the subjects was 35.3 ± 12.4 years. Of the 65 subjects, 40 were female and 25 were male. There were no losses to follow-up.
The CH values were collected at baseline and at the 1-week follow-up visit. The mean CH at baseline in the study and fellow eye was 10.5 ± 1.6 and 10.5 ± 1.6, respectively. At 1 week, the CH values were 10.7 ± 1.8 in the study eye and 10.3 ± 1.6 in the fellow eye. A post hoc analysis did not identify a relationship between the magnitude of the IOP response and the baseline CH. The mean OCT retinal nerve fiber layer global average at baseline in the study and fellow eye was 99.5 ± 10.1 µm and 98.5 ± 10.4 µm, respectively. After the 7-day period, there were no significant changes from baseline with a mean retinal nerve fiber layer global average value of 100.4 ± 11.2 µm in the study eye and 98.6 ± 11.5 µm in the control eye. In addition, there were no qualitative changes observed at the 1-week visit in comparison to baseline.
At each negative pressure setting (25%, 50%, and 75%), two IOP measurements were obtained in both the study and fellow eye. The two measurements were combined for a mean IOP measurement and used for analysis. At each negative pressure setting, the difference between the initial and final IOP measurement was less than 0.4 mm Hg.
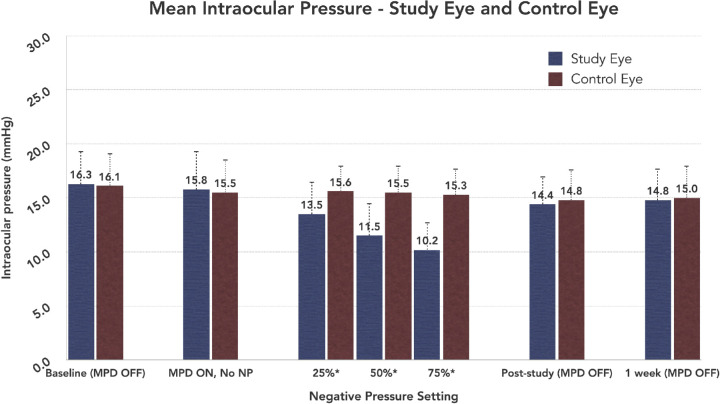
The IOP results are demonstrated in Figure 3. The mean baseline IOPs (before any device exposure) were 16.3 ± 3.0 mm Hg for the study eye group and 16.1 ± 2.9 mm Hg for the control eye group. With the MPD goggles fitted but before application of negative pressure, the mean IOPs were 15.8 ± 3.6 mm Hg in the study eye group and 15.5 ± 3.0 mm Hg in the control eye group. At baseline, with the MPD goggles fitted before negative pressure, the mean IOP of the study and control eyes were not significantly different (P = 0.37). At the negative pressure settings of 25%, 50%, and 75%, the mean IOPs in the study eye were 13.5 ± 3.4 mm Hg, 11.5 ± 3.1 mm Hg, and 10.2 ± 2.7 mm Hg, respectively. In contrast, the mean IOPs in the control eye at the same time points, without negative pressure, were 15.6 ± 3.0 mm Hg, 15.5 ± 2.5 mm Hg, and 15.3 ± 2.4 mm Hg, respectively. The difference between the mean IOPs of the two groups (study eye and control eye) was significantly different at all three negative pressure settings (P < 0.001) in comparison with baseline (Table 3). Moreover, the difference in IOP between the study and control eye was significantly different when comparing each negative pressure setting (P < 0.001).
Figure 3.
The comparison of the mean IOP via pneumatonometry during the study period in both the study and control eye. The baseline value (far left) represents the IOP measurements obtained before wear of the MPD. Only the study eye underwent application of negative pressure. NP = negative pressure; MPD OFF indicates the device was not being worn by the subject during IOP measurement. *The difference between the study and control eye at these time points (25%, 50%, 75%) was statistically significantly different (P < 0.001) than the IOP difference between the study and control eye before the application of negative pressure.
Table 3.
Statistical Comparisons During the 60-Minute Study Period
| Control Eye IOP | Study Eye IOP | Difference in Mean IOP | |
|---|---|---|---|
| (mm Hg) | (mm Hg) | (Control Eye – Study Eye) | |
| MPD on, no negative pressure | 15.5 ± 3.0 | 15.8 ± 3.6 | –0.3 mm Hg (P = 0.37*) |
| 25% Negative pressure | 15.6 ± 3.0 | 13.5 ± 3.4 | 2.1 mm Hg (P < 0.001) |
| 50% Negative pressure | 15.5 ± 2.5 | 11.5 ± 3.1 | 4.0 mm Hg (P < 0.001) |
| 75% Negative pressure | 15.3 ± 2.4 | 10.2 ± 2.7 | 5.1 mm Hg (P < 0.001) |
This P value is a result of a paired t-test performed at baseline comparing the mean IOP of the study and control eye before application of negative pressure.
The difference between the mean IOPs of the study and control eye was significantly different at all 3 negative pressure settings (P < 0.001) in comparison with baseline.
Immediately after the removal of the device, the mean IOPs were 14.4 + 2.8 mm Hg in the study eye and 14.8 ± 2.6 mm Hg in the control eye. At the 1-week follow-up visit, the mean IOPs in the study eye and control eye were 14.8 ± 2.9 mm Hg and 15.0 ± 3.0 mm Hg, respectively. The difference between the mean IOPs in the study eye and control eye were not significantly different immediately after removal of the MPD (P = 0.24) or at the 1-week follow-up visit (P = .34). There were no IOP spikes above baseline observed in either the study eye or the control eye immediate after the study period at the 1-week follow-up visit.
In comparison with baseline and with the control eye, the decrease in the mean IOP in the study eye group was statistically significant at all negative pressure settings (P < .001). The magnitude of IOP reduction increased in association with increasing levels of negative pressure application; at 25%, 50%, and 75%, the reduction in IOP was 2.3, 4.3, and 5.6 mm Hg, respectively. The 5.6 mm Hg decrease at the highest, designated negative pressure (75%) setting resulted in a 35% decrease from baseline (15.8 mm Hg). Of the subjects included in the study, 97% (63/65) demonstrated a pressure reduction in the study eye with the application of negative pressure.
There was no clinically or statistically significant change in either the study eye or control eye for mean best-corrected distance visual acuity at the 1-week follow-up visit. At baseline, the mean BCVAs (logarithm of the minimum angle of resolution) were –0.1 ± 0.2 in the study eye and –0.1 ± 0.1 in the control eye. One week after the study visit, the mean BCVAs in the study eye and control eye were –0.1 ± 0.3 and –0.1 ± 0.2, respectively. One subject experienced an adverse event, a corneal abrasion, in the study eye, during the IOP measurement. This abrasion was treated with antibiotic drops and resolved within 24 hours. There were no other observed differences from baseline in either the study eye or control eye in the slit lamp or dilated fundus examinations after exposure to the MPD device. At the 1-week follow-up visit, there were no new or abnormal slit lamp or dilated fundus exam findings noted. The OCT images immediately after wear of the MPD and at the 1-week visit were also unchanged from baseline.
The subjective assessment, which used a scale of 1 (least comfortable) to 10 (most comfortable) was administered immediately after the study period after wear of the MPD. The overall mean value was 7.3 ± 1.7 with a greater than 50% (54%) rating the comfort as at least 8 on the 10-point scale. Five subjects provided a response of less than 5 on the assessment, all related to poor fit of the device with comments related to localized discomfort. Beyond the formalized assessment, subjects were also asked to report issues with tolerability during the 60-minute test duration. There were no such reports; all subjects successfully tolerated the 60-minute test duration.
Discussion
This short-term, prospective, randomized study demonstrated a clinically and statistically significant IOP decrease at all negative pressure settings (25%, 50%, and 75%) with the MPD while the device was worn with active negative pressure. The stepwise increase in IOP reduction at each negative pressure setting highlights the capability of the device to titrate IOP lowering precisely. Mechanistically, the MPD lowers the local atmospheric pressure within the goggles to decrease the pressure force on the eye, which produces a corresponding decrease in the IOP.12 A recent study by Ethier et al.12 used a mathematical model to describe the mechanism of IOP reduction with application of negative pressure; this model suggests that the IOP quickly achieves a steady state with application of negative pressure and should maintain the decreased IOP level indefinitely while the MPD is active.
The safety results of this study are consistent with prior studies evaluating the safety and tolerability of the device, including a study by Samuelson et al that demonstrated the device is safe and tolerable for up to 8 hours of continuous wear.13,14 One subject experienced an adverse event (corneal abrasion) owing to IOP measurement and unrelated to wear of the device. There were no IOP spikes in either the study or control eyes measured during or after negative pressure application or at the 1-week follow-up.
The current treatment options in open-angle glaucoma are exclusively focused on lowering IOP, which remains the only modifiable risk factor. The emergence of MIGS (minimally invasive glaucoma surgery)7 has improved the management of glaucoma and newer medical therapies have expanded the armamentarium for providers with improved safety and efficacy.10–12 Despite these notable innovations, the available range of treatments have well-established limitations. Currently, there are no treatment options that are nonlaser, nonpharmacologic, and noninvasive. Further, no currently available treatment offers an ability to precisely titrate IOP reduction.
Owing to the challenges of treating and lowering IOP in normal tension glaucoma with the less invasive treatment option,16–18 the results of this study—IOP a decrease of more than 35% from a baseline IOP of 16.3 ± 3.0 mm Hg to 10.2 ± 2.7 mm Hg—suggest that the MPD may be a promising treatment option for this subgroup of patients.19
Given the novelty of the mechanism used to reduce IOP with the MPD, future investigation and study is critical. The findings of this study demonstrate that the IOP reduction achievable with the MPD is titratable and clinically significant (>35% from a baseline IOP of approximately 16 mm Hg). However, it is important to note that the IOP reduction achieved with the MPD is limited to when the device is worn with active negative pressure. When the device is removed, the IOP returns to baseline. Thus, the duration of the wear time and whether periodic, daily IOP reduction can impact disease progression are important questions going forward.
There are potential concerns related to use of the MPD. Although the safety results of prior studies and this present study are favorable, delivery of negative pressure to the periocular space is a newly introduced idea for lowering IOP and the potential risks, if any, remain unclear. Given the potential concern, future studies should evaluate the optic nerve head biomechanics and vasculature changes in response to negative pressure. The proposed mechanism of the device alters the local atmospheric pressure in the periocular microenvironment and subsequently modifies the IOP without disturbing other pressures in the body (eg, cerebrospinal fluid pressure, blood pressure); however, additional study would be valuable to further elucidate the details of the proposed mechanism.
Although the IOP can be lowered, there is not a 1:1 ratio of pressure reduction with the programmed negative pressure to IOP. A prior study12 used a model to explore the mechanism of IOP reduction with application of negative periocular pressure. The model from this study demonstrated that negative periocular pressure application leads to an IOP reduction coinciding with an increase in blood flow and total ocular volume. This is followed by an equilibration phase that leads to a new, but still decreased IOP. The data from this model suggests that aqueous humor dynamics, episcleral venous pressure and tissue dampening effects may also collectively impact the degree of IOP reduction.
This study is not without limitations. The duration of exposure to the study device was relatively short. Although there were no visual changes after wear of the device, visual acuity was not measured while the device was worn. It is important to note that the lenses of the MPD goggles can modified to include a visual prescription or bifocal. In addition, this study was performed in young, healthy subjects without glaucoma and future studies in glaucomatous eyes are underway to investigate the efficacy in diseased eyes. Lastly, it remains unknown what negative effects, if any, the MPD may have over an extended treatment period. Future studies will be valuable for investigating long-term side effects and more completely defining the safety profile of the device.
A localized application of negative pressure with a MPD can lower IOP in a titratable fashion. To our knowledge, this study describes the first nonpharmacologic, nonlaser, and nonsurgical option for lowering IOP, introducing a novel, titratable and well-tolerated treatment approach for multi-pressure glaucoma management.
Acknowledgments
The authors thank Richard Gorham for his help and expertise with statistical analysis.
Sponsored by Equinox Ophthalmic, Inc. (Newport Beach, California).
Presented at the 2019 American Glaucoma Society Annual Meeting, San Francisco, California; Presented at the 2019 American Society of Cataract and Refractive Surgeons Annual Meeting, San Diego, California.
Disclosure: R.J. Swan, Equinox Ophthalmic, Inc. (C); T.J. Ferguson, Equinox Ophthalmic, Inc. (C); M. Shah, None; K.W. Muir, None; T.W. Samuelson, Equinox Ophthalmic, Inc. (C); I.I.K. Ahmed, Equinox Ophthalmic, Inc. (C); R.L. Lindstrom, Equinox Ophthalmic, Inc. (C); N.M. Radcliffe, Equinox Ophthalmic, Inc. (C); J.P. Berdahl, Equinox Ophthalmic, Inc. (I)
References
- 1. Tham Y-C, Li X, Wong TY, Quigley HA, Aung T, Cheng C-Y. Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis. Ophthalmology. 2014; 121(11): 2081–2090, doi: 10.1016/j.ophtha.2014.05.013. [DOI] [PubMed] [Google Scholar]
- 2. Kingman S. Glaucoma is second leading cause of blindness globally. Bull World Health Organ. 2004; 82: 887–888, doi: 10.1590/S0042-96862004001100019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Heijl A, Leske MC, Bengtsson B, et al.. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol. 2002; 120(10): 1268–1279. [DOI] [PubMed] [Google Scholar]
- 4. Boland MV, Ervin A-M, Friedman DS, et al.. Comparative effectiveness of treatments for open-angle glaucoma: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2013; 158(4): 271–279, doi: 10.7326/0003-4819-158-4-201302190-00008. [DOI] [PubMed] [Google Scholar]
- 5. Garcia GA, Ngai P, Mosaed S, Lin KY. Critical evaluation of latanoprostene bunod in the treatment of glaucoma. Clin Ophthalmol Auckl NZ. 2016; 10: 2035–2050, doi: 10.2147/OPTH.S103985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Agrawal P, Bradshaw SE.. Systematic literature review of clinical and economic outcomes of micro-invasive glaucoma surgery (MIGS) in primary open-angle glaucoma. Ophthalmol Ther. 2018; 7(1): 49–73, doi: 10.1007/s40123-018-0131-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Shah M. Micro-invasive glaucoma surgery – an interventional glaucoma revolution. Eye Vis Lond Engl. 2019; 6(1): 29, doi: 10.1186/s40662-019-0154-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Leske MC, Heijl A, Hussein M, Bengtsson B, Hyman L, Komaroff E. Factors for glaucoma progression and the effect of treatment: the Early Manifest Glaucoma Trial. Arch Ophthalmol. 2003; 121(1): 48–56, doi: 10.1001/archopht.121.1.48. [DOI] [PubMed] [Google Scholar]
- 9. Conlon R, Saheb H, Ahmed IIK. Glaucoma treatment trends: a review. Can J Ophthalmol J Can Ophthalmol. 2017; 52(1): 114–124, doi: 10.1016/j.jcjo.2016.07.013. [DOI] [PubMed] [Google Scholar]
- 10. Gazzard G, Konstantakopoulou E, Garway-Heath D, et al.. Selective laser trabeculoplasty versus eye drops for first-line treatment of ocular hypertension and glaucoma (LiGHT): a multicentre randomised controlled trial. Lancet Lond Engl. 2019; 393(10180): 1505–1516, doi: 10.1016/S0140-6736(18)32213-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kahook MY, Serle JB, Mah FS, et al.. Long-term safety and ocular hypotensive efficacy evaluation of netarsudil ophthalmic solution: Rho Kinase Elevated IOP Treatment Trial (ROCKET-2). Am J Ophthalmol. 2019; 200: 130–137, doi: 10.1016/j.ajo.2019.01.003. [DOI] [PubMed] [Google Scholar]
- 12. Ethier CR, Yoo P, Berdahl JP. The effects of negative periocular pressure on intraocular pressure. Exp Eye Res. 2020; 191: 107928, doi: 10.1016/j.exer.2020.107928. [DOI] [PubMed] [Google Scholar]
- 13. Thompson VM, Ferguson TJ, Ahmed IIK, et al.. Short-term safety evaluation of a multi-pressure dial: a prospective, open-label, mon-randomized study. Ophthalmol Ther. 2019; 82(11): 887–9, doi: 10.1007/s40123-019-0181-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Samuelson TW, Ferguson TJ, Radcliffe NM, et al.. 8 hrs safety evaluation of a multi-pressure dial in eyes with glaucoma: prospective, open-label, randomized study. Clin Ophthalmol Auckl NZ. 2019; 13: 1947–1953, doi: 10.2147/OPTH.S217736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ferguson TJ, Knier CG, Chowdhury UR, et al.. Intraocular pressure measurement with pneumatonometry and a tonometer tip cover. Ophthalmol Ther. 2020; 9(1): 127–137, doi: 10.1007/s40123-020-00235-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Brown RH, Gibson Z, Zhong L, Lynch MG. Intraocular pressure reduction after cataract surgery with implantation of a trabecular microbypass device. J Cataract Refract Surg. 2015; 41(6): 1318–1319, doi: 10.1016/j.jcrs.2015.01.015. [DOI] [PubMed] [Google Scholar]
- 17. Ferguson TJ, Berdahl JP, Schweitzer JA, Sudhagoni RG. Clinical evaluation of a trabecular microbypass stent with phacoemulsification in patients with open-angle glaucoma and cataract. Clin Ophthalmol Auckl NZ. 2016; 10: 1767–1773, doi: 10.2147/OPTH.S114306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. De Moraes CG. Natural history of normal-tension glaucoma with (very) low intraocular pressure. Ophthalmology. 2019; 126(8): 1117–1118, doi: 10.1016/j.ophtha.2019.02.003. [DOI] [PubMed] [Google Scholar]
- 19. Mallick J, Devi L, Malik PK, Mallick J. Update on normal tension glaucoma. J Ophthalmic Vis Res. 2016; 11(2): 204–208, doi: 10.4103/2008-322X.183914. [DOI] [PMC free article] [PubMed] [Google Scholar]