Abstract
Objectives
This study described the needs of pregnant women and the contents of online obstetric consultation in representative areas with various severity of the epidemic in China.
Design
This was a cross- sectional study.
Setting
Yue Yi Tong (YYT), a free online communication platform that allows pregnant women to consult professional obstetricians.
Participants
All the pregnant women who used the YYT platform.
Intervention
From 10 to 23 February, we collected data on online obstetric consultations and participants’ satisfaction through the YYT platform in the mild, moderate and severe epidemic areas which were defined according to the local confirmed cases. The primary outcomes were the reasons for online consultations by the severity of the epidemic. All the comparisons were performed using χ2 test. Statistical analysis was performed using SPSS V.24.
Results
A total of 2599 pregnant women participated in this study, of whom 448 (17.24%), 1332 (51.25%) and 819 (31.51%) were from the mild, moderate and severe epidemic areas, respectively. The distribution of the amount of online consultations was significantly different not only in different areas (p<0.001) but also in different trimesters (p<0.001). A total of 957 participants completed the satisfaction part of the survey. In this study, 77.95% of the participants used e-health for the first time, and 94.63% of the participants were completely or mostly satisfied with the online consultations.
Conclusions
The distribution of the amount of online consultations was significantly different not only in different areas but also in different trimesters. In any trimester, the amount of consultations on the second category (obstetric care-seeking behaviour) was the highest in the severe epidemic areas. The needs for online consultations were substantial. In order to prevent irreversible obstetric adverse events, an appropriate antenatal care contingency plan with e-health services is highly recommended during the Public Health Emergency of International Concern.
Keywords: health policy, public health, telemedicine, COVID-19
Strengths and limitations of this study.
We collected these data during the most hopeless phase throughout the outbreak in China, and the data of Hubei province was also included.
Multiple centres were involved in the design to minimise biases.
This is a cross-sectional study with the short duration of data collection.
There may be bias as the satisfaction questionnaire was not a commonly structured scale.
Self-report bias might exist in our design.
Background
Since December 2019, a number of unexplained cases of viral pneumonia have been found in Wuhan, Hubei province.1 By 7 January 2020, Chinese scientists had isolated the novel coronavirus, which has been later termed as SARS-CoV-2. The official name of the related disease is COVID-19.2 Since 10:00 on 23 January 2020, traffic bans in Wuhan have been established and the whole city has been temporarily locked down.3 Subsequently, first-level emergency responses to public health emergencies have been launched successively throughout China. As of 8 April 2020, the number of confirmed cases of COVID-19 globally reached 1 384 146, of which 83 157 cases were confirmed in China, especially in Hubei province (67 803 confirmed cases).
Pregnant women are considered to be susceptible to this virus.4 For pregnant women, the routine antenatal care (ANC) during pregnancy is very important, by which high-risk pregnant women can be screened as soon as possible.5 6 However, the maternal ANC encountered great challenges during the COVID-19 outbreak due to limited accessibility of some medical resources caused by emergency traffic bans, and the risk of viral transmission. In the clinical setting, we noticed that some highly recommend antenatal check-ups had been cancelled or postponed beyond its opportune gestational age by many pregnant women. Moreover, recent studies have mainly focused on the therapeutics of pregnant women with COVID-19. Little was discussed about maternal ANC during the COVID-19 outbreak.7–9
e-Health refers to the integration of medical services and medical information through the internet and mobile technologies, such as computers, mobile phones, handheld tablets and other wireless devices.10 11 Compared with developed countries, e-health started relatively late in China.12 13 Previous reports have shown that the number of mobile phone users worldwide is nearly 7.7 billion, which equals to the total population in the world.14 By June 2019, only 5.27% internet users had used the ‘internet+medical’ (45 million).15 Yue Yi Tong (YYT) (Yue Yi Tong Science and Technology Co. in Chongqing, China) has set up an online communication platform that allows pregnant women to consult professional obstetricians without leaving home for hospitals.16
In this study, we focused on the specific content of online obstetric consultation for pregnant women during the COVID-19 outbreak based on the platform (YYT). To further investigate the role of e-health, we also conducted a survey on pregnant women who consulted online to understand their satisfaction with this consultation service and their future needs for e-health.
Methods
Study design and participants
This study was a descriptive, cross-sectional study. We collected data from two aspects, including contents of pregnant women’s online obstetric consultation and satisfaction. Gestational age and satisfaction degree were collected from registration information and satisfaction questionnaire, respectively. The content of the satisfaction questionnaire was reviewed by obstetricians (HQ and XL).
The free online service for obstetric consultation provided by YYT was promoted through several ways, including forwarding the link of the online medical consultation service website to colleagues and friends and distributing the free online treatment information. Within a few days after it was launched, the free online treatment mode had attracted over 800 maternal–fetal medicine specialists in 347 hospitals nationwide. Every pregnant woman had access to the free online treatment after registration on the platform and can choose obstetricians or hospitals at will. When a patient consults a doctor, the platform will prompt the doctor to reply within 24 hours. Before the consultation, the pregnant women were informed that the contents of the consultation would be used for scientific research and be kept absolutely confidential. If they chose ‘I already know and agree to the above’, they can continue their free online consultations. After the consultation, the platform would distribute a satisfaction questionnaire, which would take 2 min to complete, but pregnant women could choose whether to answer or not. The study started from 10 February 2020 to 23 February 2020.
All pregnant women who had submitted their online obstetric consultation were eligible for inclusion.
Procedures
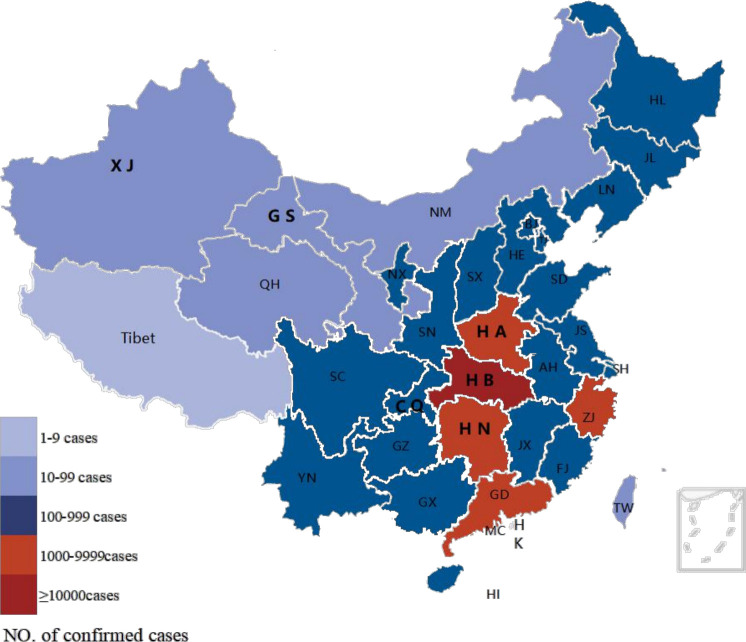
According to the map of national COVID-19 confirmed cases and the data we collected from each province, Xinjiang, Gansu (10–99 confirmed cases), Chongqing (100–999 confirmed cases), Hubei, Henan, and Hunan (≥1000 confirmed cases) were chosen as representative areas (figures 1 and 2). In this study, the number of confirmed cases of COVID-19 in different areas was used to assess the severity of epidemics (see online supplemental table 1). Hence, according to the confirmed cases, Hubei, Henan and Hunan were defined as the severe epidemic areas. Chongqing was defined as the moderate epidemic area for more confirmed cases than Xinjiang and Gansu (the mild epidemic areas).
Figure 1.
Map of confirmed cases of COVID-19 in China on 23 February.
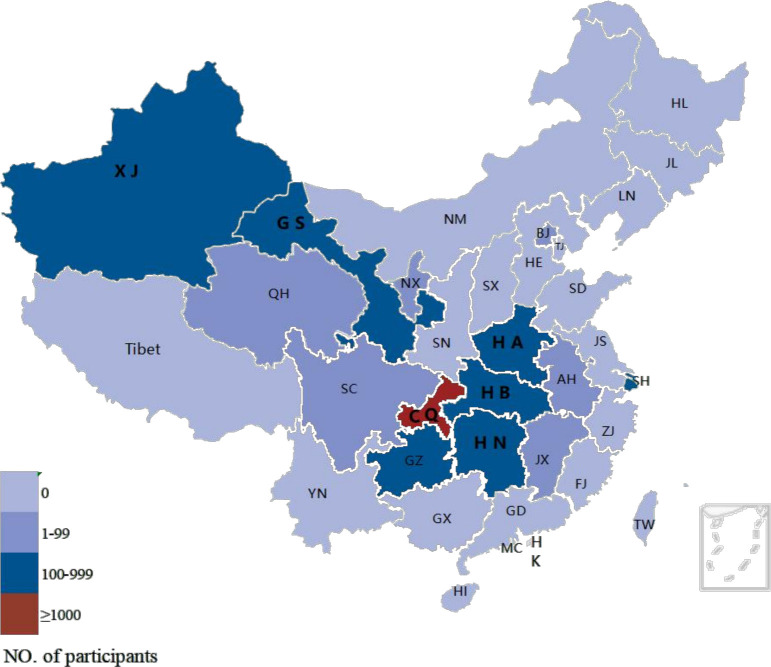
Figure 2.
Map of participants’ number in our study.
bmjopen-2020-043461supp001.pdf (59.2KB, pdf)
Data collection were conducted automatically and all data in our study were reviewed and classified independently by two authors (MC and XL). The data were sorted by different areas or different trimesters of pregnancy using manual classification method after the exclusion of unqualified data. The specific process of exclusion was shown in figure 3.
Figure 3.
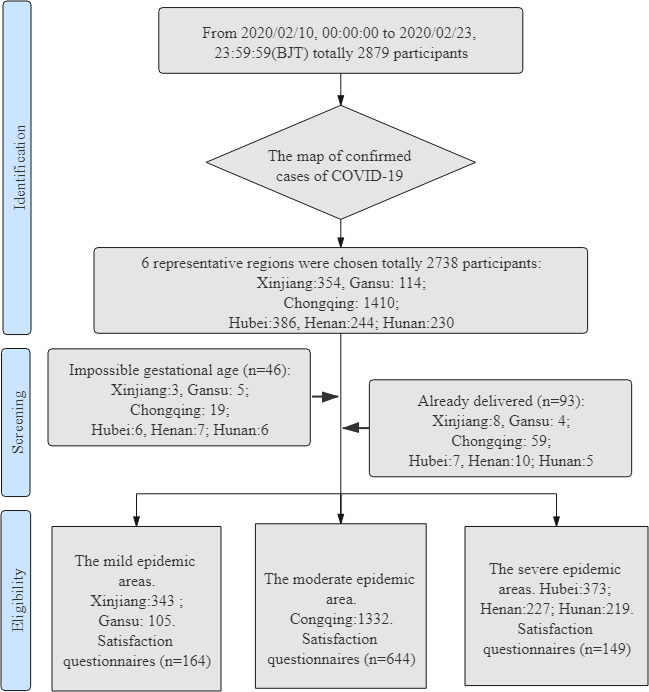
Process of classification and exclusion.
Impossible gestational age was identified whenever last menstrual or current gestational age showing less than 0 week or more than 45 weeks gestational age. According to gestational age, participants in each representative area were divided into three gestational periods: (1) the first trimester: <14 weeks; (2) the second trimester: from 14 weeks to 27 weeks and 6 days; and (3) the third trimester: ≥28 weeks. At the same time, the contents of online obstetric consultations were then subdivided into five primary categories: (1) routine antenatal check-up (reports of examination, appointments for antenatal check-up, method and time of delivery, and hospitalisation process; (2) obstetric care-seeking behaviours (cancel or postpone scheduled ANC visits; change method or time of delivery); (3) abnormal symptoms (vaginal bleeding, abnormal fetal movement and abdominal pain); (4) maternal comorbidities and pregnancy complications (gestational diabetes mellitus, hypertension disorders and hypothyroidism); and (5) other needs of e-health (remote fetal heart monitoring, electronic prescription and online pharmacies).
Since the satisfaction questionnaire was not a commonly structured scale, all the seven questions have been analysed separately. The questionnaire is shown in online supplemental appendix 1. Through the satisfaction questionnaire, we intended to understand the ‘4Ps’ situation during the COVID-19 outbreak in different areas: (1) percentage of users who use e-health for the first time, (2) proportion of problems solved by YYT, (3) pregnant women’s satisfaction with e-health and (4) preference for e-health versus outpatient visits during and after the outbreak of COVID-19.
bmjopen-2020-043461supp002.pdf (107.4KB, pdf)
Statistical analysis
All exact numbers and percentages for all variables were calculated, and the comparisons were performed using χ2 test. Logistic regression was used to examine the association between the distribution of the amount of online consultations and the trimesters. SPSS software V.24.0 was used for the statistics analysis, and the conventional p value less than 0.05 is defined as statistically significant. Percentage (%) was used to express categorical variables.
Patient and public involvement
We did not directly include patient and public involvement in the study.
Result
A total of 2599 pregnant women participated in this study, of whom 448 (17.24%), 1332 (51.25%) and 819 (31.51%) women were from the mild, moderate and severe epidemic areas, respectively. Among all the participants, 417 (16.04%), 1054 (40.55%) and 1128 (43.40%) were in their first, second and third trimesters of pregnancy, respectively. It was worth noting that it was the first time e-health was used in ANC during the COVID-19 outbreak, and 6.77% of participants generated additional requirements for e-health, such as remote fetal heart rate monitoring, electronic prescription and online pharmacies.
Reasons for online consultations by areas with different severity of the epidemic
As shown in table 1, the distribution of the amount of online consultations varied by areas with different severity of the epidemic (p<0.001). Moreover, 32.48% of pregnant women consulted the second category (obstetric care-seeking behaviour) in the most severe areas, which was significantly higher than the average value of 22.58% (table 1).
Table 1.
Reasons for online consultations by areas with different severity of the epidemic
| Classification of online medical care consultation | Severity of the epidemic situation in different areas | Total | χ2 | P value | ||
| Mild (n=448) |
Moderate (n=1332) |
Severe (n=819) |
||||
| Routine antenatal check-up | 184 (41.07) | 561 (42.12) | 263 (32.11) | 1008 (38.78) | 86.216 | <0.001† |
| Obstetric care-seeking behaviour | 91 (20.31) | 229 (17.19) | 266 (32.48) | 586 (22.55) | ||
| Abnormal symptoms | 110 (24.55) | 292 (21.92) | 143 (17.46) | 545 (20.97) | ||
| Maternal comorbidity and pregnancy complications | 46 (10.27) | 158 (11.86) | 80 (9.77) | 284 (10.93) | ||
| Other needs for e-health | 17 (3.79) | 92 (6.91) | 67 (8.18) | 176 (6.77) | ||
Note: Data are n (%); χ2 test was used for the analysis.
*P<0.05.
†P<0.01.
‡
Reasons for online consultations by trimesters of pregnancy
In table 2, the difference was shown in the distribution of the amount of online consultations by trimesters (p<0.01). The first category (routine antenatal check-up) was of highest concern in the first trimester (57.31%), compared with that in the second (39.75%) and third trimester (31.03%). While the distribution of the amount of online consultations on the second category in different trimesters were completely opposite to that on the first category. And the second category had attracted the most attention from pregnant women in the third trimester (25.18%). Compared with the distribution of the amount of online consultations on the first category, the second (OR=1.265, 95% CI 1.044 to 1.532), third (OR=1.380, 95% CI 1.134 to 1.680) and fourth (OR=2.639, 95% CI 2.031 to 3.429) categories were associated with the trimesters of pregnancy (table 2).
Table 2.
Reasons for online consultations by trimesters of pregnancy
| Trimesters of pregnancy | Total | OR (95% CI) | P value | |||
| First trimester (n=417) |
Second trimester (n=1054) |
Third trimester (n=1128) |
||||
| Classification of online medical care consultation | <0.001† | |||||
| Routine antenatal check-up | 239 (57.31) | 419 (39.75) | 350 (31.03) | 1008 (38.78) | Reference (1) | |
| Obstetric care-seeking behaviour | 45 (10.79) | 257 (24.38) | 284 (25.18) | 586 (22.55) | 1.265 (1.044 to 1.532) | 0.016* |
| Abnormal symptoms | 74 (17.75) | 211 (20.02) | 260 (23.05) | 545 (20.97) | 1.380 (1.134 to 1.680) | 0.001† |
| Maternal comorbidity and pregnancy complications | 28 (6.71) | 75 (7.12) | 181 (16.05) | 284 (10.93) | 2.639 (2.031 to 3.429) | <0.001† |
| Other needs for e-health | 31 (7.43) | 92 (8.73) | 53 (4.70) | 176 (6.77) | 0.742 (0.533 to 0.984) | 0.039* |
Note: Data are n (%).
*P<0.05.
†P<0.01.
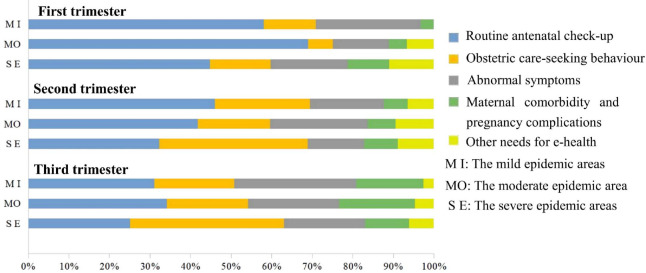
Reasons for online consultations by the trimesters of gestation and the severity of the epidemic
In this study, as shown in table 3, most participants were in the second or third trimester (40.55%, 43.40%). Regardless of the trimesters, the distribution of the amount of online consultations was region-dependent (p<0.001). In any trimester, the amount of consultations on the second category (obstetric care-seeking behaviour) was the highest in the severe epidemic areas. Moreover, the proportions of the second category in the second and third trimesters were 36.51% and 37.88% separately, while the corresponding average values were 24.38% and 25.18% (table 3).
Table 3.
Reasons for online consultations by the trimesters of gestation and the severity of the epidemic
| Classification of online medical care consultation | Severity of the epidemic situation in different areas | Total | χ2 | P value | ||
| Mild (n=448) |
Moderate (n=1332) |
Severe (n=819) |
||||
| First trimester | 417 (16.04) | 33.422 | <0.001† | |||
| Routine antenatal check-up | 36 (58.06) | 125 (69.06) | 78 (44.83) | 239 (57.31) | ||
| Obstetric care-seeking behaviour | 8 (12.90) | 11 (6.08) | 26 (14.94) | 45 (10.79) | ||
| Abnormal symptoms | 16 (25.81) | 25 (13.81) | 33 (18.97) | 74 (17.75) | ||
| Maternal comorbidity and pregnancy complications | 2 (3.23) | 8 (4.42) | 18 (10.34) | 28 (6.71) | ||
| Other needs for e-health | 0 (0.00) | 12 (6.63) | 19 (10.92) | 31 (7.43) | ||
| Second trimester | 1054 (40.55) | 48.869 | <0.001† | |||
| Routine antenatal check-up | 86 (45.99) | 231 (41.85) | 102 (32.38) | 419 (39.75) | ||
| Obstetric care-seeking behaviour | 44 (23.53) | 98 (17.75) | 115 (36.51) | 257 (24.38) | ||
| Abnormal symptoms | 34 (18.18) | 133 (24.09) | 44 (13.97) | 211 (20.02) | ||
| Maternal comorbidity and pregnancy complications | 11 (5.88) | 38 (6.88) | 26 (8.25) | 75 (7.12) | ||
| Other needs for e-health | 12 (6.42) | 52 (9.42) | 28 (8.89) | 92 (8.73) | ||
| Third trimester | 1128 (43.40) | 52.766 | <0.001† | |||
| Routine antenatal check-up | 62 (31.16) | 205 (34.22) | 83 (25.15) | 350 (31.03) | ||
| Obstetric care-seeking behaviour | 39 (19.60) | 120 (20.03) | 125 (37.88) | 284 (25.18) | ||
| Abnormal symptoms | 60 (30.15) | 134 (22.37) | 66 (20.00) | 260 (23.05) | ||
| Maternal comorbidity and pregnancy complications | 33 (16.58) | 112 (18.70) | 36 (10.91) | 181 (16.05) | ||
| Other needs for e-health | 5 (2.51) | 28 (4.67) | 20 (6.06) | 53 (4.70) | ||
Note: Data are n (%); χ2 test was used for the analysis.
*P<0.05.
†P<0.01.
Most concerned category during different trimesters
Generally, in any area, or during any trimester, routine antenatal check-up, obstetric care-seeking behaviour and abnormal symptoms were the top three consulted categories (figure 4). In the first trimester, pregnant women in different regions were the most frequently consulting for the first type of problems, which was consistent with that in the second and third trimesters both in the moderate and mild epidemic areas (figure 4). However, in the severe epidemic areas, the second category (obstetric care-seeking behaviour) was of most concern in the second and third trimesters of pregnancy (figure 4).
Figure 4.
Proportion of the five categories by trimesters in each area.
Participants’ experiences with e-health
The participants’ experiences with e-health are summarised in table 4. A total of 957 participants completed the satisfaction questionnaire, of whom 164 (17.14%), 644 (67.29%) and 149 (15.57%) were from the mild, moderate and severe epidemic areas, respectively. During the outbreak of COVID-19, we wanted to learn the following four aspects of the situation in different regions (‘4Ps’) from the questionnaire. The first is the percentage of users who use e-health for the first time. Surprisingly, for most of the participants, it was their first time to use the e-health, with the highest rate of 89.26% in the severe epidemic areas. The second is the proportion of problems solved by the platform. We found that more than 90% of online consultation issues were completely or partially resolved. The third is pregnant women’s satisfaction with e-health. In fact, the proportion of total satisfaction or relative satisfaction was the lowest in the severe epidemic areas, at 87.92%, while it was as high as 90% in other areas. The last was the preference for e-health or outpatient visits during and after the outbreak. Undoubtedly, the outbreak of COVID-19 had an obvious impact on participants’ choices. During the outbreak of COVID-19, most participants preferred to use e-health (the lowest rate of 88.41% in the mild epidemic areas), while about half of the participants chose the outpatient visits after the outbreak, which was most popular in moderate epidemic areas, with the highest rate of 62.11%. An average of 79.94% of the participants deemed that e-health could save time, and 82.45% of the participants thought it could reduce the risk of COVID-19 infection. In addition, 39.81% and 41.17% of the participants held the view that e-health could make them feel comfortable and could help them save money, respectively. As for their suggestions for e-health in the near future, 32.92%, 28.21%, 57.37% and 47.02% of the participants hoped for the function of online video, physician’ s replay within a defined time, automatic referral to appropriate obstetricians and management of maternal medical condition, respectively. There were 3.76% of participants who expressed more needs for e-health, such as remote fetal heart monitoring, electronic prescription and online pharmacies.
Table 4.
Satisfaction questionnaire
| Severity of the epidemic in different areas | Total | χ2 | P value | |||
| Mild | Moderate | Severe | ||||
| First time using e-health | 164 | 644 | 149 | / | 20.178 | <0.001† |
| No | 27 (16.46) | 168 (26.09) | 16 (10.74) | 211 (22.05) | ||
| Yes | 137 (83.54) | 476 (73.91) | 133 (89.26) | 746 (77.95) | ||
| Degree of trouble shooting | 164 | 644 | 149 | / | 23.274 | 0.001† |
| Completely solved | 124 (75.61) | 521 (80.90) | 98 (65.77) | 743 (77.64) | ||
| Largely solved | 34 (20.73) | 115 (17.86) | 42 (28.19) | 191 (19.96) | ||
| Barely solved | 4 (2.44) | 6 (0.93) | 6 (4.03) | 16 (1.67) | ||
| Not solved at all | 2 (1.22) | 2 (0.31) | 3 (2.01) | 7 (0.73) | ||
| Degree of satisfaction with e-health | 164 | 644 | 149 | / | 22.015 | 0.005† |
| Completely satisfaction | 109 (66.46) | 438 (68.01) | 82 (55.03) | 629 (65.73) | ||
| Mostly satisfied satisfaction | 43 (26.22) | 175 (27.17) | 49 (32.89) | 267 (27.90) | ||
| Neutral attitude | 11 (6.71) | 25 (3.88) | 14 (9.40) | 50 (5.22) | ||
| Mostly satisfied dissatisfaction | 1 (0.61) | 0 (0.00) | 2 (1.34) | 3 (0.31) | ||
| Completely dissatisfaction | 0 (0.00) | 6 (0.93) | 2 (1.34) | 8 (0.84) | ||
| Choice (during COVID-19) | 164 | 644 | 149 | / | 1.147 | 0.563 |
| E-health | 145 (88.41) | 576 (89.44) | 137 (91.95) | 858 (89.66) | ||
| Outpatient | 19 (11.59) | 68 (10.56) | 12 (8.05) | 99 (10.34) | ||
| Choice (after COVID-19) | 164 | 644 | 149 | / | 11.145 | 0.004† |
| E-health | 85 (51.83) | 244 (37.89) | 66 (44.30) | 395 (41.27) | ||
| Outpatient | 79 (48.17) | 400 (62.11) | 83 (55.70) | 562 (58.73) | ||
| Convenience of the e-health‡ | 395 | 1613 | 351 | / | 6.821 | 0.556 |
| Time -saving | 124 (75.61) | 535 (83.07) | 106 (71.14) | 765 (79.94) | ||
| Risk-reduction§ | 127 (77.44) | 534 (82.92) | 128 (85.91) | 789 (82.45) | ||
| Cost-saving | 71 (43.29) | 268 (41.61) | 55 (36.91) | 394 (41.17) | ||
| Feeling more relaxed | 64 (39.02) | 258 (40.06) | 59 (39.60) | 381 (39.81) | ||
| Others | 9 (5.49) | 18 (2.80) | 3 (2.01) | 30 (3.13) | ||
| Needs for e-health‡ | 285 | 1087 | 248 | / | 14.474 | 0.070 |
| Online video | 67 (23.51) | 198 (18.22) | 50 (20.16) | 315 (32.92) | ||
| Physician’s replay within a defined time | 52 (18.25) | 173 (15.92) | 45 (18.15) | 270 (28.21) | ||
| Automatic referral to appropriate obstetricians | 83 (29.12) | 370 (34.04) | 96 (38.71) | 549 (57.37) | ||
| Management of maternal medical condition | 79 (27.72) | 318 (29.25) | 53 (21.37) | 450 (47.02) | ||
| Others¶ | 4 (1.40) | 28 (2.58) | 4 (1.61) | 36 (3.76) | ||
Note: Data are n (%).
*P<0.05.
†P<0.01.
‡M: multiple choice allowed.
§Risk-reduction: risk-reduction of being infected with COVID-19 by avoiding extra exposure.
¶Others: remote fetal heart monitoring, electronic prescription, or online pharmacies.
Discussion
The COVID-19 outbreak represents a significant and urgent threat to global health. On 30 January 2020, COVID-19 was declared as ‘public enemy number one’ and ‘a very high level of global risk’ by WHO.17 18 As of 23 March 23, 2020, 186 countries worldwide had reported confirmed COVID-19 cases, including more than 10 000 confirmed cases in America, Germany, France, Italy and Iran. In this study, many pregnant women were found postponing or cancelling their scheduled ANC visits on their own, which was related to the severity of the epidemic situation in different areas, especially in the severe epidemic areas. Meanwhile, the needs of pregnant women for e-health have exceeded our expectation. Data showed that more than 15 000 consultations were conducted through the platform until 15 March. To the best of our knowledge, this is the first time to focus on the characteristics of online obstetric consultation for pregnant women during the COVID-19 outbreak. Since the majority of participants in the study was in their second and third trimesters, the data of the first trimester had certain limitations.
Changes in obstetric care-seeking behaviour during the COVID-19 outbreak
In our study, we discussed the associations between the distribution of the amount of online consultations and trimesters or the severity of the epidemic in different areas. The distribution of the amount of online consultations was significantly different not only in different areas but also in different trimesters. We also found that in any trimester, the amount of consultations on the second category (obstetric care-seeking behaviour) was the highest in the severe epidemic areas. During the COVID-19 outbreak, emergency traffic bans limited accessibility of some medical resources for pregnant women, and fear of viral transmission also prevented pregnant women from seeking routine ANC, especially in the severe epidemic areas. All of these phenomena can explain the cause of the highest concern for the second category in the areas with severe epidemic. Unlike the first and the second trimesters, the need for more frequent ANC in the third trimester is already a huge challenge for pregnant women.19 There were 16 120 outpatient visits in Obstetrics Clinic of the First Affiliated Hospital of Chongqing Medical University in last February, compared with 6859 in February 2020. Furthermore, this difference was more dramatic in Maternal and Child Health Hospital of Hubei Province, because more than 21 000 outpatient visits were reduced in February 2020, compared with that of last February (27 254 visits vs 5410 visits). The sharp decline of outpatient visits further reflected that pregnant women postponed or cancelled scheduled ANC visits on their own. This phenomenon raised our concerns over a series of potential irreversible obstetric adverse events.
Significance of ANC
In order to detect maternal complications, reduce adverse pregnancy events and promote doctor–patient communication, eight ‘contacts’ are recommended during pregnancy according to WHO.20 21 Referring to the ANC guideline developed by America, Britain, Canada and WHO, based on Chinese condition, Guideline of Preconception and Prenatal Care (2018), which was released by the Chinese Medical Association, Chapter of Perinatal Medicine recommends 7–11 contacts.19 If there are high-risk factors, the frequency should be increased appropriately. This guideline is widely applied by almost all domestic ANC institutions in China. Benefiting from the widespread application of the ANC guideline, birth defects and caesarean section rates have been reduced, and many other adverse pregnancy outcomes have been avoided in China.22–28 Nevertheless, during the COVID-19 outbreak, the routine ANC for pregnant women who are considered to be susceptible are extremely challenged.29 30 In the past month, a dramatic decline in ANC visit and an increase in the caesarean section rate had been observed by obstetricians, all of which could lead to irreversible obstetrical pregnancy outcome. The phenomenon might be related to the delayed detection of fetal malformation and a significant increasing incidence of diabetes, macrosomia and obesity due to lack of nutritional interventions or routine physical activities. What’s more, some pregnant women wanted to be hospitalised earlier to wait for the onset of labour or to have a caesarean in advance driven by an idea that as time went on, the chance of infection would increase. On the other hand, some pregnant women with indications of hospitalisation blindly refused to be hospitalised for fear of infection with COVID-19. To prevent irreversible obstetric adverse events, some highly recommended antenatal check-ups must be conducted on time, and when it comes to conduct ultrasound examination for confirming intrauterine pregnancy and nuchal translucency measurement, screening for fetal aneuploidy and oral glucose tolerance test, pregnant women have to visit the hospital in person. Moreover, prompt hospitalisation was highly recommended in the following circumstances: approaching terminal gestational age, pregnancy with severe maternal medical condition, with signs of labour.
Novel mode of ANC plan with full application of e-health
In our survey, most of the participants experienced e-health for the first time. What’s more, 91.95% pregnant women reported that they preferred e-health rather than a visit to hospital during the COVID-19 outbreak in the severe epidemic areas. The majority of pregnant women were completely or comparatively satisfied with e-health, and most of online obstetric consultations were completely or mostly solved. Except the second category, most pregnant women are more likely to consult about the first and third categories, which was probably due to the familiarity of e-health among the public. This result was consistent with the report of China Internet Network Information Center in June 2019.13 Actually, the ‘e’ in e-health not only stands for ‘electronic’, but also means telemedicine, telecare, clinical information systems and other non-clinical systems used for education, public health and medical management.10 e-Health has made some achievements in the management of chronic diseases, such as diabetes and hypertension disorders.31 32 The application of e-health in obstetrics is mainly reflected in the abortion of unplanned pregnancy in the first trimester.33 The popularity of wearable devices promotes quantitative health management.34 Nevertheless, ‘e-health’ cannot save everything. Some highly recommended antenatal check-ups and timely hospitalisation are still necessary. Our domestic clinical ANC guideline is divided into health education and guidance, routine healthcare and auxiliary examination.19 According to the investigation of online obstetric consultation during the COVID-19 outbreak, we recommend combining e-health with the ANC guideline in the following three aspects: (1) management of mental health, routine health education and care, authoritative prevention education on PHEs; (2) auxiliary procedures done through e-health for necessary check-ups recommended in hospital by obstetricians, such as making appointments and consulting examination reports; and (3) interventions of some maternal medical conditions performed through e-health, including gestational diabetes mellitus and hypertension disorders, which had been fully applied in non-pregnant people.31 We hold that the full application of e-health and prenatal care is highly recommended to be included in the contingency ANC plan during PHEs, which will be beneficial for pregnant women and will mitigate the risk of adverse pregnancy outcomes.
Conclusions
Our study found that during the outbreak, many pregnant women changed their scheduled ANC visits without the obstetrician’s authorisation, especially in the severe epidemic areas. This study also revealed that online obstetric consultation is highly accepted and greatly satisfied pregnant women during the COVID-19 outbreak in China. This investigation also indicated that e-health has played an important role in ANC during PHE. This novel model of ANC plan can make notable contributions not only in China but also in other emerging epidemic centres worldwide and in future PHEs.
Supplementary Material
Footnotes
MC and XL contributed equally.
Correction notice: This article has been corrected since it first published. 'Xin Luo' has been added as the corresponding author.
Contributors: HQ, XL and MC contributed to the protocol design. MC and XL collected and analysed the data. MC drafted the manuscript. JZ, GS, YG, YS and PB contributed to the interpretation of the results. JZ and YZ proofread and commented on the manuscript. HQ and XL revised the final version and are guarantors of this manuscript. All authors made substantial contributions to the paper and read and approved the final manuscript.
Funding: National Natural Science Foundation of China (No. 81771614 and No. 81771613), and the National Key Research and Development Program of China (No. 2016YFC1000407).
Map disclaimer: The depiction of boundaries on this map does not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. This map is provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Ethics approval and consent to participate: The cross-sectional study was approved by the ethics committee of the First Affiliated Hospital of Chongqing Medical University (20200501), and all the methods were performed in accordance with the relevant guidelines and regulations.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Ethics statements
Patient consent for publication
We followed guidelines ensuring the study was voluntary and confidential, and an electronic informed consent was obtained before the questionnaire.
References
- 1.Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. The Lancet 2020;395:507–13. 10.1016/S0140-6736(20)30211-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med 2020;382:1199–207. 10.1056/NEJMoa2001316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.People's Government of Hubei Province . Announcement from the Headquarter for novel coronavirus pneumonia prevention and control (no.1). Beijing: China National health Commission, 2020. Available: http://www.gov.cn/xinwen/2020-01/23/content_5471751.htm
- 4.Jamieson DJ, Honein MA, Rasmussen SA, et al. H1N1 2009 influenza virus infection during pregnancy in the USA. The Lancet 2009;374:451–8. 10.1016/S0140-6736(09)61304-0 [DOI] [PubMed] [Google Scholar]
- 5.Kogan MD, Alexander GR, Kotelchuck M, et al. Relation of the content of prenatal care to the risk of low birth weight. maternal reports of health behavior advice and initial prenatal care procedures. JAMA 1994;271:315. [PubMed] [Google Scholar]
- 6.Lin M-L, Wang H-H. Prenatal examination behavior of Southeast Asian pregnant women in Taiwan: a questionnaire survey. Int J Nurs Stud 2008;45:697–705. 10.1016/j.ijnurstu.2006.12.005 [DOI] [PubMed] [Google Scholar]
- 7.Qiao J. What are the risks of COVID-19 infection in pregnant women? The Lancet 2020;395:760–2. 10.1016/S0140-6736(20)30365-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen H, Guo J, Wang C, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. The Lancet 2020;395:809–15. 10.1016/S0140-6736(20)30360-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dowswell T, Carroli G, Duley L, et al. Alternative versus standard packages of antenatal care for low-risk pregnancy. Cochrane Database Syst Rev 2015;7:CD000934. 10.1002/14651858.CD000934.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eysenbach G. What is e-health? J Med Internet Res 2001;3:E20. 10.2196/jmir.3.2.e20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stevenson JK, Campbell ZC, Webster AC, et al. eHealth interventions for people with chronic kidney disease. Cochrane Database Syst Rev 2019;8:CD012379. 10.1002/14651858.CD012379.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rockoff ML. Telemedicine: explorations in the use of telecommunications in health care. Social Science & Medicine 1977;11:295–6. 10.1016/0037-7856(77)90078-6 [DOI] [Google Scholar]
- 13.Geneva, March(AM) . International Telecommunication Union. World Telecommunications 1994;4:493–4. [Google Scholar]
- 14.International Telecommunication Union . Ict facts and figures 2017, 2017. Available: https://www.itu.int/en/ITU-D/Statistics/Documents/facts/ICTFactsFigures2017.pdf
- 15.CNNIC . The 44th statistical report on Internet development in China. Available: http://www.cac.gov.cn/2019-08/30/c_1124939590.htm(inChinese)
- 16.YunYiTong . Version 1.0. Available: http://www.cqyyt.net/
- 17.WHO . The COVID-19 risk communication package for healthcare facilities, 2020. Available: https://iris.wpro.who.int/bitstream/handle/10665.1/14493/COVID-19-02282020.pdf
- 18.WHO . WHO Director-General's opening remarks at the media briefing on COVID-19 - 28 February 2020, 2020. Available: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---28-february-2020 [Accessed 28 February 2020].
- 19.Obstetrics Subgroup, Chinese Society of Obstetrics and Gynecology, Chinese Medical Association . Guideline of preconception and prenatal care. Chin J Obstet Gynecol 2018;53:7–13. [Google Scholar]
- 20.WHO . Recommendations on antenatal care for a positive pregnancy experience, 2016. Available: https://apps.who.int/iris/bitstream/handle/10665/250796/9789241549912-eng.pdf?sequence=1 [PubMed]
- 21.Tunçalp Ӧ, Pena-Rosas JP, Lawrie T, et al. WHO recommendations on antenatal care for a positive pregnancy experience-going beyond survival. BJOG 2017;124:860–2. 10.1111/1471-0528.14599 [DOI] [PubMed] [Google Scholar]
- 22.Kirk E, Daemen A, Papageorghiou AT, et al. Why are some ectopic pregnancies characterized as pregnancies of unknown location at the initial transvaginal ultrasound examination? Acta Obstet Gynecol Scand 2008;87:1150–4. 10.1080/00016340802443822 [DOI] [PubMed] [Google Scholar]
- 23.Kirk E, Bottomley C, Bourne T. Diagnosing ectopic pregnancy and current concepts in the management of pregnancy of unknown location. Hum Reprod Update 2014;20:250–61. 10.1093/humupd/dmt047 [DOI] [PubMed] [Google Scholar]
- 24.Committee on Practice Bulletins—Obstetrics and the American Institute of Ultrasound in Medicine . Practice bulletin No. 175: ultrasound in pregnancy. Obstet Gynecol 2016;128:e241–56. 10.1097/AOG.0000000000001815 [DOI] [PubMed] [Google Scholar]
- 25.National Institute for Health and Clinical Excellence . Antenatal care for uncomplicated pregnancies. NICE clinical guideline 62[EB/OL], 2017. Available: https://www.nice.org.uk/guidance/cg62 [PubMed]
- 26.Blencowe H, Cousens S, Jassir FB, et al. National, regional, and worldwide estimates of stillbirth rates in 2015, with trends from 2000: a systematic analysis. Lancet Glob Health 2016;4:e98–108. 10.1016/S2214-109X(15)00275-2 [DOI] [PubMed] [Google Scholar]
- 27.Lawn JE, Blencowe H, Waiswa P, et al. Stillbirths: rates, risk factors, and acceleration towards 2030. The Lancet 2016;387:587–603. 10.1016/S0140-6736(15)00837-5 [DOI] [PubMed] [Google Scholar]
- 28.Madhi SA, Briner C, Maswime S, et al. Causes of stillbirths among women from South Africa: a prospective, observational study. The Lancet Global Health 2019;7:e503–12. 10.1016/S2214-109X(18)30541-2 [DOI] [PubMed] [Google Scholar]
- 29.The State Council’s Joint Prevention and Control Mechanism for Pneumonia Epidemic in Response to New Coronavirus Infection . Notice on prevention and controof pneumonia in children and pregnant women with new coronavirus infection, 2020. Available: http://www.ljxw.gov.cn/news-93789.shtml
- 30.Wang J, Qi H, Bao L, et al. A contingency plan for the management of the 2019 novel coronavirus outbreak in neonatal intensive care units. Lancet Child Adolesc Health 2020;4:258–9. 10.1016/S2352-4642(20)30040-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chou C-F, Bullard KM, Saaddine JB, et al. Utilization of e-health services among U.S. adults with diabetes. Diabetes Care 2015;38:e200–1. 10.2337/dc15-1162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gray J, O’Malley P. Review: e-health interventions improve blood pressure level and control in hypertension. Ann Intern Med 2019;170:JC68. 10.7326/ACPJ201906180-068 [DOI] [PubMed] [Google Scholar]
- 33.Norman WV, Dickens BM. Abortion by telemedicine: an equitable option for Irish women. BMJ 2017;357:j2237. 10.1136/bmj.j2237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fanelli A, Ferrario M, Piccini L, et al. Prototype of a wearable system for remote fetal monitoring during pregnancy. Annu Int Conf IEEE Eng Med Biol Soc 2010;2010:5815–8. 10.1109/IEMBS.2010.5627470 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-043461supp001.pdf (59.2KB, pdf)
bmjopen-2020-043461supp002.pdf (107.4KB, pdf)
Data Availability Statement
Data are available upon reasonable request. The datasets used and analysed during the current study are available from the corresponding author on reasonable request.