Abstract
The outbreak of COVID-19 raised numerous questions on the interactions between the occurrence of new infections, the environment, climate and health. The European Union requested the H2020 HERA project which aims at setting priorities in research on environment, climate and health, to identify relevant research needs regarding Covid-19. The emergence and spread of SARS-CoV-2 appears to be related to urbanization, habitat destruction, live animal trade, intensive livestock farming and global travel. The contribution of climate and air pollution requires additional studies. Importantly, the severity of COVID-19 depends on the interactions between the viral infection, ageing and chronic diseases such as metabolic, respiratory and cardiovascular diseases and obesity which are themselves influenced by environmental stressors. The mechanisms of these interactions deserve additional scrutiny. Both the pandemic and the social response to the disease have elicited an array of behavioural and societal changes that may remain long after the pandemic and that may have long term health effects including on mental health. Recovery plans are currently being discussed or implemented and the environmental and health impacts of those plans are not clearly foreseen. Clearly, COVID-19 will have a long-lasting impact on the environmental health field and will open new research perspectives and policy needs.
Keywords: SARS-COV-2, Biodiversity, Urbanization, Climate, Chemicals, Transformational change
1. Introduction
The COVID-19 pandemic is challenging the world’s economic and health systems and exemplifies the degree of global interdependencies and need of preparedness for global health threats. Much of the focus is now on the response to the pandemic and the development of treatments and vaccines. Health threats due to human impacts on Earth may appear to be of less immediate concern: climate change, pollution, urbanisation and unsustainable consumption that have led to major environmental disturbances and biodiversity loss. It may be tempting to develop solutions to the pandemic independently of these threats, such as relying on disposable materials, reducing public transport use, and subsidizing heavily polluting industries. Such responses might yield short-term health and economic benefits but would forfeit needed long-term improvements in human health and sustainability. In fact, neither climate change nor other environmental stressors and their impacts on human and ecosystems health have receded. Furthermore, the COVID-19 crisis highlights the links between environmental changes and emergence of infectious diseases and warns us of the urgent need to prevent such pandemics, as their control has proven to be highly challenging in a globalized world. This calls for a planetary health perspective in governance and research and for inter-, trans-disciplinary and trans-sectorial approaches.
This work was conducted by HERA, an EU H2020 programme that includes 24 partner institutes across Europe and hundreds of collaborating researchers and wider community stakeholders (www.HERAresearchEU.eu). The aim of HERA is to set the priorities for an environment, climate and health research agenda in the EU by adopting a holistic and systemic approach in the face of global environmental changes. An interim agenda identifying six major research goals has already been set (https://www.heraresearcheu.eu/hera-2030-agenda). With the outbreak of the COVID-19 pandemic resulting from the emergence of the SARS-CoV-2 virus, HERA partners constituted a HERA-COVID-19 working group to reflect on the connections between COVID-19 and the Environment, Climate and Health nexus. In the course of this work, we developed a common understanding of the multiple and strong interactions between the pandemic and environmental issues and of the corresponding emerging research needs, while also reflecting on the environmental and health impacts of the response to the pandemic and of the recovery plans.
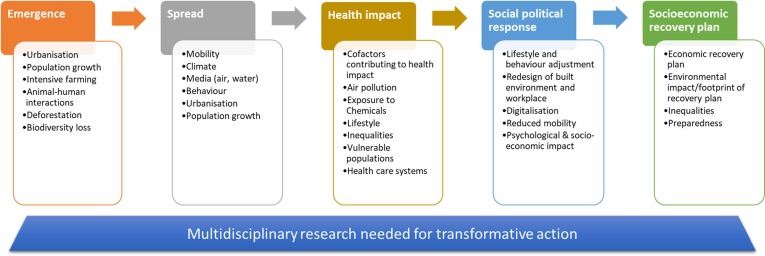
The response to COVID-19 is further complicated by concurrent threats such as heat waves (Pascal et al. 2018), wildfires, locusts in East Africa, drought in several parts of the world, and the severe 2020 cyclone season. Furthermore, the pandemic itself is likely to hamper an optimal response to these threats—stretching under-resourced public health systems, impeding evacuations and other emergency responses, fuelling on-line disinformation campaigns and conspiracy theories (Islam et al. 2020). The pandemic and environmental health issues are highly interconnected and we argue that only an integrated global approach simultaneously taking into account infectious agents and other environmental threats can lead to sustainable solutions and policies to protect humans and ecosystems, both now and for generations to come (Fig. 1 ). We discuss here the key messages of this work.
Fig. 1.
COVID-19 and Environment, Climate and Health. The figure shows the different stages of the pandemic development and, at each stage, the environmental factors that either contribute to or are impacted by that particular stage. The HERA consortium has made proposals for multidisciplinary research to achieve transformational change supporting and merging different agendas such as zero pollution, climate change resilience and mitigation, farm to fork, circular economy, EU chemical strategy for sustainability. These proposals can be found at https://www.heraresearcheu.eu/
1.1. Interlinkages of global environmental change and the emergence and impact of the COVID-19 pandemic
The emergence of a new pandemic was not unexpected given the increased understanding of how population growth and urbanization, habitat destruction, globalization of trade including live animal trade, and intensive livestock farming increase risk of transmission of zoonotic pathogens (Gibb et al., 2020, Plowright et al., 2017). Indeed, such human activities have contributed to the repeated emergence and spread of several zoonotic diseases since 2002 such as SARS (SARS-CoV), MERS-CoV, Zika and Ebola, all caused by viruses (OECD, 2020). These human activities, compounded by the increase in international mobility and weakened public health systems, created optimal conditions for the emergence and transmission of SARS-CoV-2. Decreased biodiversity, deforestation and ecosystem imbalance increase the likelihood of the emergence of an epidemic, but additional studies are needed to elucidate complexities and enable efficient countermeasures (Morand and Lajaunie, 2017). Likewise, climate change, which has direct effects on the distribution of pathogens, their animal reservoirs and vectors, is recognized as a key driver of epidemic emergence (Boissier et al., 2016, Ryan et al., 2019, Caminade et al., 2019, Bartlow et al., 2019). While there is evidence that climate conditions and air pollution may also facilitate viral spread (Woodby et al., 2020, Karan et al., 2020, O'Reilly et al., 2020), additional investigations are needed. Features of the built environment, from crowded housing to inadequate ventilation in commercial spaces and mass transit vehicles, may facilitate virus transmission; research is needed not only to elucidate these effects but to reconcile disease control with broader goals in housing, transport, and other sectors. A better understanding of these aspects is critical to improve both the prospects for prevention and to develop predictive models for public health risk management.
Improving knowledge of the ecological and behavioural drivers of coronavirus infection emergence and spread is essential. Although the zoonotic nature of SARS-CoV-2 has been clearly demonstrated (Zhou et al. 2020), there is still a missing link between the viral variants isolated from bat, pangolin and human (Wang et al. 2020) and the intermediary host(s) from which the virus passed to human. Understanding the ecology and epidemiology of COVID-19 also requires determining the genetic bases of the susceptibility of hosts, whether they are reservoir animal species or human populations.
Examples of key research questions include the impact of ecosystem changes, such as deforestation, land use, road-building, and urban expansion, on human-wildlife interactions and subsequent risk of zoonotic disease spill over. Thus, there is an important need to determine how much habitat destruction on the one hand and human activities/behaviours (farming practices, hunting, markets,…) on the other hand, which both favour contacts between wild and domestic fauna and humans, have contributed to the recent emergences of zoonotic diseases (in particular SARS-CoV-2). Similarly, in a context of climate change, there is a need to better characterize the role of biodiversity loss in disease emergence (Morand and Lajaunie, 2018).
Method development is also important. For example, ecological health observatories are needed to understand the social-ecology of SARS-CoV-2 and characterize the temporal and spatial patterns of its occurrence in diverse ecological compartments (wild and domestic fauna, water and air), both in cities and rural areas. Screening wild fauna for viral genomes (metagenomics), and implementing open-access databases is necessary to trace the thread of transmission and viral evolution within the intermediary hosts of SARS-CoV-2. This information will also be needed for future emerging viruses.
Modelling the spread and course of the pandemic proved to be critical for decision making throughout the course of the pandemic. It is therefore important to improve data integration and processing and to increase modelling capacities across Europe and the world. This could include models that better describe infection spread accounting for both the climatic conditions and their effect on transmissibility (Sarigiannis, 2020), as well as efforts that describe the interactions among community members to help estimate the effective contact rate. Thus, models should incorporate epidemiological and demographic data, as well as ecological, evolutionary, climatic, social and cultural data, which are also key factors influencing disease evolution.
Research will require close collaboration across different disciplines including microbiology, medicine and epidemiology, ecology, environmental sciences and engineering, evolutionary sciences, agricultural sciences, veterinary sciences, and social sciences, as well as urban planning and mobility studies, anthropology and behavioural economics. Such data are needed both to implement and to validate models of emergence and transmission. For that, integrative approaches should be promoted on multiple systems, including knowledge of human activities/practices, and health status.
1.2. Health impact of COVID-19 and environmental stressors
The combined effects of infectious and environmental stressors are a major concern. The severity of COVID-19 is strongly associated with age and co-morbidities such as lung, heart, metabolic diseases and obesity (Guan et al. 2020), which are partly caused by exposure to environmental stressors such as poor urban design, an unhealthy food environment, air pollution and chemical toxicants (Landrigan et al. 2018). Better characterization of the immune and cardiometabolic effects of pollutants is essential to identify susceptibilities or exacerbating factors on a population level. The impact of COVID-19 is disproportionate in low-income and minority groups reflecting the role of socio-economic factors in exposure and vulnerability to the virus. The co-ordination of existing cohort studies across Europe presents a significant first step, as will the Europe-wide identification, development and exploitation of appropriate tools and models to better understand, assess and predict the health, social and environmental determinants and impacts of COVID-19.
The COVID-19 pandemic has dramatically shown that infectious diseases and non-communicable diseases are highly interconnected, the latter strongly contributing to the severity of the former. It is therefore important to study the interaction between viral infections and environmental factors of chronic diseases such as chemical toxicants, air pollution, climate change and socio-economic determinants. For instance, the dual role of indoor air quality in both environmental contamination and viral spread requires more research focus, as well as innovative solutions for mitigation, including development of air purification technologies (Domínguez-Amarillo et al. 2020). Moreover, inhalation of wood smoke at a relatively low level was associated with suppressed respiratory immunity, resulting in increased susceptibility to infections as well as to several types of lung disease (Sarigiannis et al. 2015); this is of particular importance in relation to the energy poverty associated with the recent financial crisis. Similarly, the balance of risks and benefits associated with time spent in parks and green and blue spaces needs to be elucidated. Along these lines, health, environmental and socio-economic impact assessment tools should be further developed and harmonized. Development and coordination of large-scale infrastructures and tools such as cohorts and analytical facilities as well as harmonization of impact prediction capacities is also an important objective for the EU.
1.3. Integrated socio-economic, political and health implications of COVID-19 and intervention strategies
COVID-19 has influenced behaviour, working conditions and business in many parts of the world, including increased digitalisation and decreased physical interactions and mobility, and will have long lasting effects on the built environment and the way cities are organized. In addition to the disease itself, the recovery plans may have their own influence on the environment and on future population physical and mental health. Furthermore, both the pandemic and the related control measures have highlighted profound inequalities in most societies that may further increase with the economic crisis. While the pandemic has been a tragedy, many of the responses offer lessons for environmental health, and researchable questions. These are discussed below, and some are exemplified in more detail in the Table 1 .
Table 1.
Research questions related to the impacts of COVID-19 and the social response to the pandemic.
| Impacts of COVID-19 and social response | Research questions |
|---|---|
| Behavioural changes | |
| Consuming fewer or different goods and services | What is the association between reduced or changed consumption, environmental sustainability, and human well-being? Can reduced or changed consumption be maintained post-COVID? |
| Frequenting parks and greenspaces | How best to balance the risks and benefits of greenspace/bluespace visits during a pandemic? Access to green/bluespaces and implications for urban planning? |
| Shifting to walking and cycling | What were the benefits of these shifts? |
| Ordering food and other essentials on-line, for delivery | What are the health and environmental implications of increasing e-commerce? |
| Workplace changes | |
| Working from home | How does remote working affect productivity and job satisfaction? Will these changes be permanent? implications for urban planning? |
| Changed workplace configurations, improved ventilation, etc. | How do these changes affect indoor air quality, energy demand, worker satisfaction, and infection risk? |
| Occupational exposure to virus and protective measures for different occupational groups, e.g. health care workers | Which occupational groups are most affected? What protective strategies are effective and sustainable? How to implement them? |
| Reduced business travel, shift to on-line meetings | What were the health and environmental benefits of these changes, in particular reduced air travel? How can these benefits be prolonged? |
| Urbanisation | |
| Repurposing streets from vehicles to walking and cycling | To what extent can these changes drive a long-term shift in transportation modes? What are the health and environmental benefits? |
| Improved air quality from reduced fuel combustion. | What were the health benefits? What were the public responses, especially in chronically polluted places? How can the value of clean air be maintained? |
| Role of environment and living conditions | Will there be a shift toward suburban/rural living and what will be the environmental and health implications? Socio-economic determinants and impact on health in different population groups (and areas)? |
| Public health system | |
| COVID tested capabilities in epidemiologic data collection, texting and contact tracing, triage and medical care | What elements of the health system need to be strengthened in preparation for the next pandemic or other disaster? |
| COVID tested capabilities in health crisis management | What are the lessons for organisation, communication, health democracy, and international collaboration? How best to integrate environmental health into the management of acute health challenges? |
| Development of specific health surveillance during the crisis | How did this crisis provide better tools for health surveillance considering different populations of interest (older, vulnerable,…) |
| Increased use of tele-healthcare and reduced visits in healthcare centres | What are the safety, efficacy, environmental and health impacts of this shift, including longer term health impacts? |
| Disparate morbidity and mortality among minorities, the poor | What were the mechanisms of inequitable impact, and how to rectify these inequities? |
| Numerous public health messages from various sources | Which communications strategies functioned well, and which did not? How best to provide credible, evidence-based, actionable guidance to the public, and suppress disinformation? |
| Combination of environmental threats | |
| COVID-19 pandemic combined with air pollution,heat weaves, wildfires or other environmental threats | Risk perception and management by public authorities;Impact of multiple exposures and combined risks |
A major challenge in responding to COVID is balancing reduced economic activity to control disease spread, and restored economic activity to avoid the harsh social and health consequences of the shutdown. An equally critical challenge is balancing a return to a pre-COVID “normal” condition versus resetting our economy to a new and better one, that avoids the health risks, inequities, and environmental depredations of recent decades (IEA report, 2020). While this is a devastating moment, it is also an opportunity for transformative change that advances planetary health (WHO, 2020, Belesova et al., 2020a).
There are multiple behavioural, economic and societal impacts of the COVID-19 pandemic that need to be deciphered. These impacts could be due to the pandemic itself, due to the initial strategies to limit its spread and/or the longer term recovery plans. Research is needed to better characterize the impacts on urban/rural life, transport, work conditions and inequalities and to better explore the causal relationships leading to those impacts. Research can also inform what the optimal recovery pathway should look like and how it can most effectively promote health.
Concerning the health crisis management per se, this pandemic has highlighted the difficulties of taking into account environmental health perspectives in policies and control measures which have mostly focused on curbing the infectious outbreak. In different settings, outdoor recreation, exercise, cycling and enjoyment of natural spaces have been either encouraged or hampered. Moreover, the pandemic seems to have fuelled excess use of plastics and disposables, thus failing the sustainability targets in this area. Exploring benefits and risks as well as potential consequences of the decisions taken to control the spread of an infectious agent is needed to better integrate and promote environmental health issues into the health crises management of an infectious outbreak.
Such progress must be informed by rigorous evidence. The needed research must evaluate the environmental, health, economic, and social impacts of many aspects of the COVID response, from local to national and to international levels, as shown in the Table 1, and it must project future impacts through scenario-building, modelling and forecasting. International efforts could focus on how to achieve efficient alert systems, including their organisation, coordination and communication from an environmental health perspective. Research must involve citizens and stakeholders, particularly the voices of the disenfranchised, to ensure fair and practical solutions. It will require deeply interdisciplinary collaboration of earth and planetary sciences, ecology, biomedical science, and economics and social sciences.
2. Conclusion
Most of the research proposals made in this review require transdisciplinary approaches and are embedded in a planetary health perspective. In order to strengthen both aspects, continuous endeavours at various scales are needed, ranging from institutional research funding, organisation of research and education in universities and academic settings to dedicated and generic research calls and programmes as well as international collaboration. Most importantly, education at all levels, including life-long learning, is critical to foster development of problem-solving skills and multi-, inter- and trans-disciplinary research that is required to tackle complex interlinked global challenges. While additional knowledge is required in many cases, there are several instances where it is the implementation of acquired knowledge that is at stake and that needs to be improved. Efforts to facilitate translation of scientific findings into society to support evidence-based policymaking are also required and can be promoted via knowledge brokers and new ways of working, including platforms for collaboration and communication between researchers, policymakers, experts and citizens.
What started as a health crisis has become a social, economic, environmental and political challenge. It is imperative that recovery plans and taxpayers’ funds go beyond the current economic and social crisis, support and reinforce the EU’s ambitious Green Deal and Sustainable Development Goals (SDGs) to benefit health and efficiently prevent future crises (WHO, 2020, Haines and Scheelbeek, 2020). The pandemic has revealed the need to consider environmental health systematically, also in the face of an acute, infectious pandemic. It is unveiling knowledge gaps in several fields and research orientations that go beyond COVID-19: 1) the ecological origin of diseases; 2) the interaction between environmental health stressors and infectious diseases; 3) an integrated assessment of societal impacts of the disease, the global response and the recovery plans. There is a need to identify and implement policies that will bring short-term and long-term benefits to health and sustainability. What we are learning on the research needs concerning this pandemic may also be true for other environmental changes such as climate change and biodiversity, and their impact on human health (Belesova et al. 2020b). Previous warnings about a pandemic went largely unheeded for many reasons including the immediate costs of preventive measures. In hindsight, it is easy to see that prevention appears to be extremely cost-efficient (World Bank, 2012).
Disclaimer
The authors alone are responsible for the views expressed in this article and they do not necessarily represent the views, decisions or policies of the institutions with which they are affiliated.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors acknowledge the HERA project that has received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement N° 825417.
Handling Editor: Adrian Covaci
References
- Bartlow A.W., Manore C., Xu C., Kaufeld K.A., Del Valle S., Ziemann A., et al. Forecasting Zoonotic Infectious Disease Response to Climate Change: Mosquito Vectors and a Changing Environment. Vet Sci. 2019;6(2):40. doi: 10.3390/vetsci6020040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belesova K., Heymann D.L., Haines A. Integrating climate action for health into covid-19 recovery plans. BMJ. 2020;370 doi: 10.1136/bmj.m3169. [DOI] [PubMed] [Google Scholar]
- Belesova K., Haines A., Ranganathan J., Seddon J., Wilkinson P. Monitoring environmental change and human health: Planetary Health Watch. Lancet. 2020;395(10218):96–98. doi: 10.1016/S0140-6736(19)33042-9. [DOI] [PubMed] [Google Scholar]
- Boissier J., Grech-Angelini S., Webster B.L., Allienne J.-F., Huyse T., Mas-Coma S., et al. Outbreak of urogenital schistosomiasis in Corsica (France): an epidemiological case study. Lancet Infect Dis. 2016;16(8):971–979. doi: 10.1016/S1473-3099(16)00175-4. [DOI] [PubMed] [Google Scholar]
- Caminade C., McIntyre K.M., Jones A.E. Impact of recent and future climate change on vector-borne diseases. Ann N Y Acad Sci. 2019;1436(1):157–173. doi: 10.1111/nyas.13950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Domínguez-Amarillo S., Fernández-Agüera J., Cesteros-García S., González-Lezcano R.A. Bad Air Can Also Kill: Residential Indoor Air Quality and Pollutant Exposure Risk during the COVID-19 Crisis. Int J Environ Res Public Health. 2020;17(19):7183. doi: 10.3390/ijerph17197183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibb R., Redding D.W., Qing Chin K., et al. Zoonotic host diversity increases in human-dominated ecosystems. Nature. 2020;584:398–402. doi: 10.1038/s41586-020-2562-8. [DOI] [PubMed] [Google Scholar]
- Guan W.-J., Liang W.-H., Zhao Y., Liang H.-N., Chen Z.-S., Li Y.-M., et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. European Respiratory Journal. 2020;56(4) doi: 10.1183/13993003.00547-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haines A., Scheelbeek P. European Green Deal: A Major Opportunity for Health Improvement. Lancet. 2020;395(10233):1327–1329. doi: 10.1016/S0140-6736(20)30109-4. [DOI] [PubMed] [Google Scholar]
- Report I.E.A. Shaping a secure and sustainable energy future for all. ( 2020 [Google Scholar]
- Islam M.S., Sarkar T., Khan S.H., Mostofa Kamal A.-H., Hasan S.M.M., Kabir A., et al. COVID-19–Related Infodemic and Its Impact on Public Health: A Global Social Media Analysis. The American Journal of Tropical Medicine and Hygiene. 2020;103(4):1621–1629. doi: 10.4269/ajtmh.20-0812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karan A., Ali K., Teelucksingh S., Sakhamuri S. The impact of air pollution on the incidence and mortality of COVID-19. Glob Health Res Policy. 2020;5:39. doi: 10.1186/s41256-020-00167-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landrigan P.J., Fuller R., Acosta N.J.R., Adeyi O., Arnold R., Basu N., et al. The Lancet Commission on pollution and health. The Lancet. 2018;391(10119):462–512. doi: 10.1016/S0140-6736(17)32345-0. [DOI] [PubMed] [Google Scholar]
- Morand S., Lajaunie C. Biodiversity and Health; Linking life, Ecosystems and Societies. ISTE Press - Elsevier. 2017 (https://www.elsevier.com/books/biodiversity-and-health/morand/978-1-78548-115-4) [Google Scholar]
- Morand S., Lajaunie C. Loss of Biological Diversity and Emergence of Infectious Diseases. Biodiversity and Health. Chapter. 2018;3:29–48. doi: 10.1016/B978-1-78548-115-4.50003-2. [DOI] [Google Scholar]
- OECD. 2020. Biodiversity and the economic response to COVID-19 : Ensuring a green and resilient recovery. (http://www.oecd.org/coronavirus/policy-responses/biodiversity-and-the-economic-response-to-covid-19-ensuring-a-green-and-resilient-recovery-d98b5a09/#contactinfo-d7e7152).
- O'Reilly K.M., Auzenbergs M., Jafari Y., Liu Y., Flasche S., Lowe R. Effective transmission across the globe: the role of climate in COVID-19 mitigation strategies. The Lancet Planetary Health. 2020;4(5):E172. doi: 10.1016/S2542-5196(20)30106-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pascal M., Wagner V., Corso M., et al. Heat and cold related-mortality in 18 French cities. Environment International. 2018;121(1):189–198. doi: 10.1016/j.envint.2018.08.049. [DOI] [PubMed] [Google Scholar]
- Plowright R.K., Parrish C.R., McCallum H., Hudson P.J., Ko A.I., Graham A.L., et al. Pathways to zoonotic spillover. Nature reviews Microbiology. 2017;15:502–510. doi: 10.1038/nrmicro.2017.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan S.J., Carlson C.J., Mordecai E.A., Johnson L.R. Global expansion and redistribution of Aedes-borne virus transmission risk with climate change. PLoS Negl Trop Dis. 2019 doi: 10.1371/journal.pntd.0007213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarigiannis D.A., Karakitsios S.P., Kermenidou M.V. Health impact and monetary cost of exposure to particulate matter emitted from biomass burning in large cities. Science of the Total Environment. 2015;524–525:319–330. doi: 10.1016/j.scitotenv.2015.02.108. [DOI] [PubMed] [Google Scholar]
- Sarigiannis, Dimosthenis A., 2020. COVID-19 Risk Evaluation model. (https://www.enve-lab.eu/index.php/covid-19-risk-evaluation-model/).
- Wang H., Pipes L., Nielsen R. Synonymous mutations and the molecular evolution of SARS-Cov-2 origins. BioRxiv. 2020 doi: 10.1101/2020.04.20.052019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO, 2020. Manifesto for a healthy recovery from COVID-19. (https://reliefweb.int/report/world/who-manifesto-healthy-recovery-covid-19).
- Woodby B., Arnold M.M., Valacchi G. SARS-CoV-2 infection, COVID-19 pathogenesis, and exposure to air pollution: What is the connection? Ann N Y Aca Sci. 2020 doi: 10.1111/nyas.14512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World, Bank. 2012. Pathogens and Our Planet: The Economics of One Health. Washington, DC. © World Bank. (https://openknowledge.worldbank.org/handle/10986/11892).
- Zhou P., Yang X.L., Wang X.G., Hu B., Zhang L., Zhang W., et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]