Abstract
Objective
To characterize system-level barriers to bariatric surgery from the perspectives of Veterans with severe obesity and obesity care providers.
Summary Background Data
Bariatric surgery is the most effective weight loss option for Veterans with severe obesity, but fewer than 0.1% of Veterans with severe obesity undergo it. Addressing low utilization of bariatric surgery and weight management services is a priority for the Veterans Health Administration (VHA).
Methods
We conducted semi-structured interviews with Veterans with severe obesity who were referred for or underwent bariatric surgery, and providers who delivered care to Veterans with severe obesity, including bariatric surgeons, primary care providers, registered dietitians, and health psychologists. We asked study participants to describe their experiences with the bariatric surgery delivery process in the VA system. All interviews were audio-recorded and transcribed. Four coders iteratively developed a codebook and used conventional content analysis to identify relevant systems or “contextual” barriers within Andersen’s Behavioral Model of Health Services Use.
Results
73 semi-structured interviews with Veterans (n=33) and providers (n=40) throughout the VHA system were completed. More than three fourths of Veterans were male, while nearly three fourths of the providers were female. Eight themes were mapped onto Andersen’s model as barriers to bariatric surgery: poor care coordination, lack of bariatric surgery guidelines, limited provider knowledge about bariatric surgery, long travel distances, delayed referrals, limited access to healthy foods, difficulties meetings preoperative requirements and lack of provider availability and/or time.
Conclusions
Addressing system-level barriers by improving coordination of care and standardizing some aspects of bariatric surgery care may improve access to evidence-based severe obesity care within VA.
MINI ABSTRACT
In this qualitative study of 73 interviews with Veterans with severe obesity and obesity care providers, participants identified barriers to surgery including poor care coordination, lack of bariatric surgery care guidelines within VA, and limited provider knowledge about bariatric surgery care. Improving care coordination and optimizing provider knowledge about the bariatric surgery evaluation process, pre-operative care and post-operative follow-up may help improve the delivery of evidence-based severe obesity care within VA.
INTRODUCTION
Observational studies and randomized trials have led to the conclusion that bariatric surgery is the most effective weight loss treatment for adults with severe obesity (body mass index [BMI] ≥ 40 kg/m2 or 35.0 – 39.9 kg/m2 in addition to an obesity-related comorbidity).1 Bariatric surgery is associated with improved quality of life and resolution of obesity-related comorbidities compared to dietary changes and increased physical activity alone.2–9 Bariatric surgery mortality rates have also decreased more than 10-fold over the past three decades10,11 and are now similar to cholecystectomy mortality rates.12
Despite its effectiveness and favorable safety profile, bariatric surgery utilization rates remain low. Fewer than 1% of U.S. adults who meet BMI criteria for bariatric surgery undergo it annually.13,14 Utilization of bariatric surgery is even lower within the Veterans Health Administration (VHA) system, where an average of fewer than 500 bariatric procedures are performed annually for approximately 700,000 Veterans with severe obesity.15,16 This rate of bariatric surgery utilization (0.07%) is nearly 20 times lower than the utilization rate for non-Veterans. In 2016, invited subject matter experts participating in a VA “State of the Art” (SOTA) conference on weight management in Washington, DC, acknowledged low utilization of bariatric surgery in VA and cited addressing barriers to bariatric surgery as a research priority.17
The objective of this study was to describe system-level barriers to referral and receipt of bariatric surgery from the perspectives of Veterans with severe obesity and obesity care providers. Further, we sought to identify barriers that could be targeted to improve access to evidence-based obesity care in the VA system.
METHODS
Study design and population
We performed a qualitative study that included semi-structured interviews with patients and providers in VA.
Patients – Veterans were eligible if they met National Institutes of Health (NIH) BMI criteria for bariatric surgery [1) BMI of 35.0–39.9 kg/m2 with an obesity-related comorbidity (coronary artery disease, dyslipidemia, hypertension, diabetes, GERD, obstructive sleep apnea); or 2) BMI ≥ 40 kg/m2] and had participated in either behavioral or surgical weight management at one of two VA medical centers in the Midwest region. Participation in behavioral weight management included attendance at least three “Weight Management Program for Veterans” (MOVE!) visits, with the first visit occurring 6–18 months prior to study initiation. This allowed us to identify patients who participated in the MOVE! program long enough that they could have reasonably been evaluated for bariatric surgery (typically 6–12 months). MOVE! is VA’s evidence-based weight management program that was adapted from the Diabetes Prevention Program18 and involves individual or group sessions with providers, often dietitians, focused on nutrition, physical activity, and related behavioral strategies (e.g., goal-setting, problem solving, stimulus control).
Bariatric surgery patients were defined as Veterans who attended at least one MOVE! visit 12–72 months prior to study initiation and were either referred for bariatric surgery and/or underwent bariatric surgery. This longer period allowed the study team to identify an adequate sample size of patients. All potentially eligible patients were identified through an administrative data pull of electronic health records. Veterans older than 70 years of age were excluded from the analysis because some VA bariatric surgery programs exclude them from bariatric surgery.
Providers – Four groups of providers were eligible for participation. Health psychologists, registered dietitians (RDs), and primary care providers (PCPs) were eligible if they practiced at one of three hospitals in our region (also known as our Veterans Integrated Services Network or VISN). PCPs were required to have a panel of at least 250 patients and had to be a physician, physician assistant, or nurse practitioner. To obtain an adequate sample size of bariatric surgeons, all surgeons who performed bariatric surgery at one of the 21 VA bariatric surgery programs nationally were eligible for participation. We attempted to recruit 2 surgeons from each of the 5 VA regions.
Data collection
Eligible Veterans and providers were sent recruitment letters or emails, respectively, asking them to participate in a 60-minute, semi-structured interview. Written consent was obtained for in-person interviews (for Veterans and providers who were able to complete an in-person interview), and verbal consent was obtained for telephone interviews (for providers who were unable to complete an in-person interview due to logistics or distance). Veterans were asked to describe their experiences with weight loss treatment options in VA (Supplemental Digital Content 1). Veterans were also asked about their motivations for pursuing bariatric surgery or behavioral weight management, and how their experiences with weight loss treatments compared to their weight loss treatment intentions and goals. Providers were asked to describe their experiences with managing patients with severe obesity in the VA system. Upon completion of their interviews, participants were asked to complete a demographic survey, which included questions about their age, sex, race/ethnicity, and socioeconomic status.
Data analysis
All interviews were audio-recorded, transcribed, de-identified, and uploaded to NVivo Version 11.19 We analyzed the data using conventional content analysis,20 which included both emergent codes and a priori codes based on our research questions. Five members of the research team (SAJ, EA, RG, CV, LF) consensus-coded seven transcripts (approximately 10% of the total) independently to draft the initial set of codes. After each of the first seven transcripts was coded independently, the group convened to discuss themes, adjudicate differences, and determine code definitions. Coders’ memos and annotations were reviewed to facilitate group discussions. to refine and finalize the codebook. Once the codebook was finalized, using the technique of constant comparison,21 three coders (SAJ, EA, GES) each coded approximately one-third of the remaining transcripts independently. These individuals met regularly as a group to discuss segments for which codes could not easily be applied. Through discussion, they achieved coding consensus.
For this analysis, we examined all data associated with codes relating to bariatric surgery (15 codes from patient transcripts and 28 codes from provider transcripts; Supplemental Digital Content 2). We used data matrices22 organized by the study participant group (Veterans or one of the four provider groups) to perform higher-level analysis and generate themes within the framework of Andersen’s Behavioral Model of Health Services Use.23 Andersen’s model was chosen because our research group previously reviewed the literature regarding bariatric surgery access and applied these findings to Andersen’s conceptual framework.24
Andersen’s model includes two general types of determinants: contextual and individual. In the current study, we report the contextual determinants, which represent the circumstances and environment of health care access, and include providers, the health care system, and community characteristics. A patient’s use of the health care system (for both contextual and individual determinants) involves three components in Andersen’s model: 1) a predisposition to use a service; 2) factors that impede or enable use of that service; and 3) the need for that service. Per Andersen’s Model, there are three types of “predisposing” contextual determinants (provider demographics, social factors, and beliefs) and three types of “enabling” contextual determinants (health policy, financing, and organizational factors). “Care coordination” was defined as processes that “facilitat[ed] integration of, and navigation through, healthcare services, within and across care settings, to help patients receive the care they need and want without unnecessary duplication of services or avoidable inconvenience.”25
This study was approved by the UW-Madison IRB and the William S. Middleton VA Research & Development Committee (VA R&D). The study procedures, including obtaining informed consent, were performed in accord with the ethical standards of the Helsinki Declaration of 1975.
RESULTS
Study participant characteristics
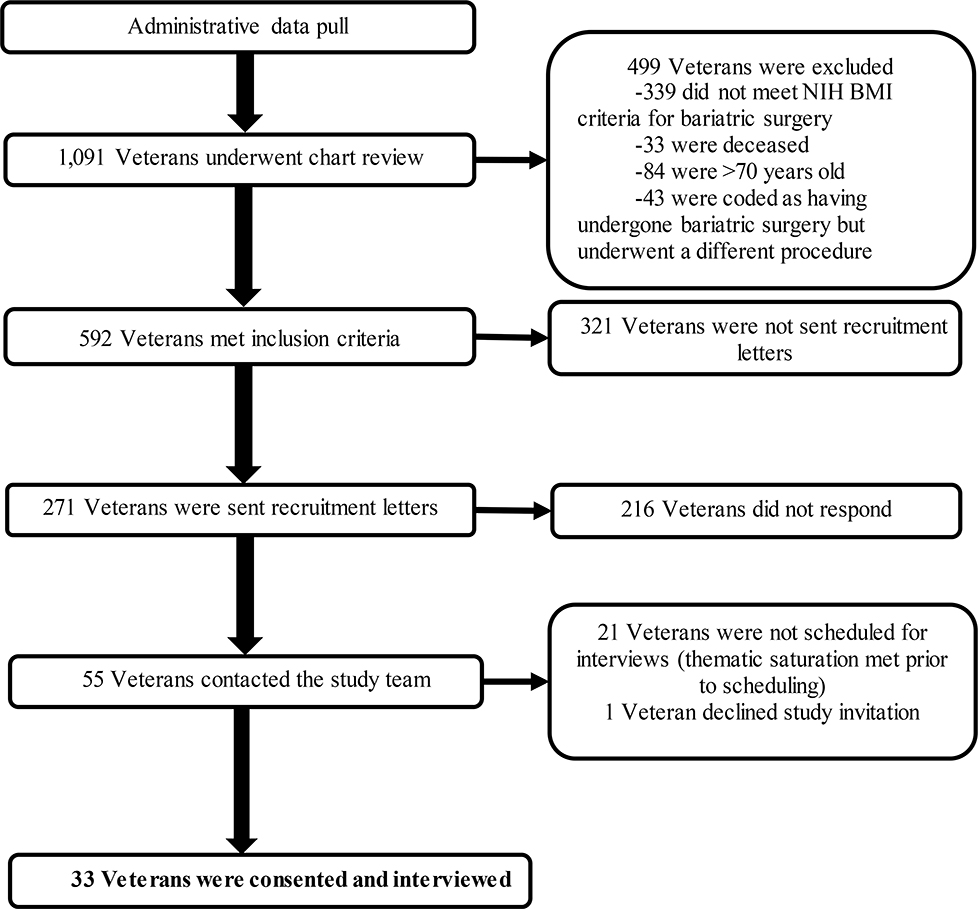
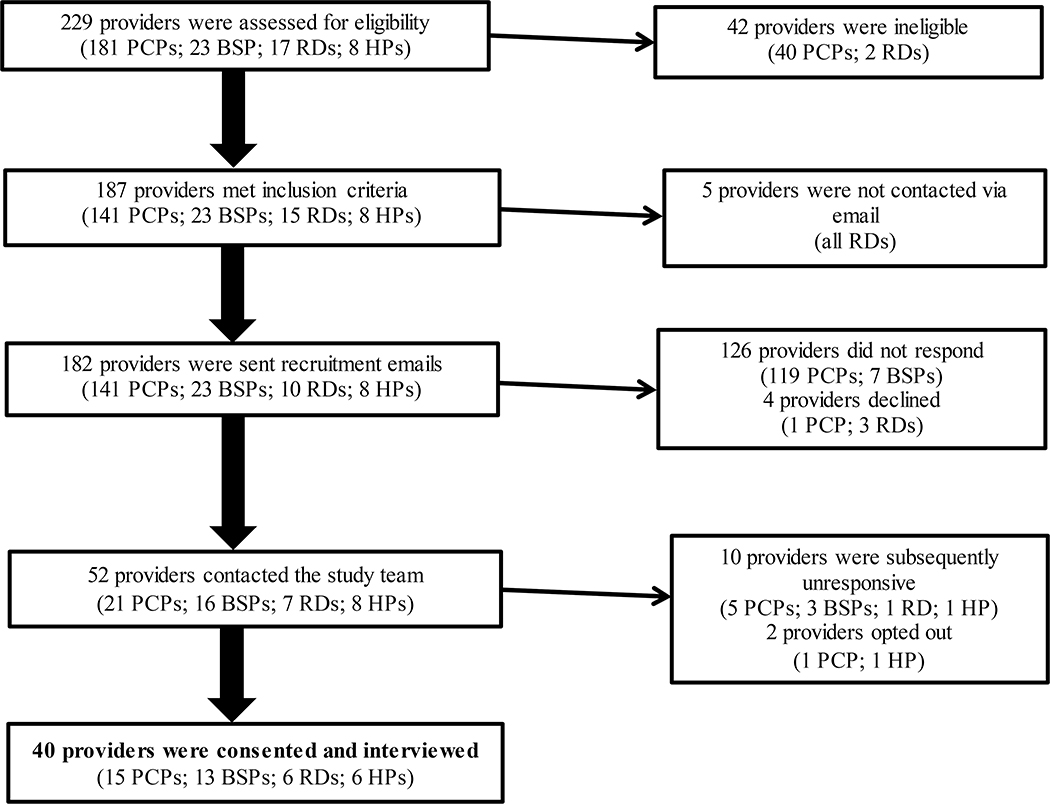
We assessed 1,091 Veterans and 229 providers for eligibility (Figures 1 and 2). 592 Veterans and 187 providers met inclusion criteria. Of those who met inclusion criteria, 271 Veterans and 182 providers were contacted for recruitment. We reached thematic saturation prior to contacting all Veterans, and thus 321 Veterans were not sent recruitment letters. We obtained informed consent from and interviewed 73 participants: 33 Veterans and 40 providers (15 PCPs, 13 bariatric surgeons, 6 RDs and 6 health psychologists). Bariatric surgeons represented all 5 VA regions in the U.S. The mean age of Veteran and provider participants was 58.5 and 44.0 years, respectively (Table 1). Nearly three-fourths of Veterans were male (n=26) and white (n=25). Nearly three-fourths of providers were female (n=29) and white (n=31). Forty-three percent (n=17) of the provider participants had a dual appointment at a university.
Figure 1.
Flowchart detailing patient recruitment
Figure 2: Flowchart detailing provider recruitment.
PCP: Primary care providers; BSP: Bariatric surgery provider; RD: Registered dietitian; HP: Health psychologist;
Table 1.
Patient and provider demographics
| Veterans (n=33) | Providers (n=40) | |
|---|---|---|
| Age (mean, SD) | 58.5 (±8.4) | 44.0 (±9.9) |
| Gender (n, %) | ||
| Male | 26 (79) | 11 (27) |
| Female | 7 (21) | 29 (73) |
| Ethnicity (n, %) | ||
| White | 25 (76) | 31 (78) |
| Black or African American | 7 (21) | 0 |
| Asian | 0 | 2 (5) |
| Hispanic | 1 (3) | 1 (2.5) |
| American Indian or Alaska Native | 0 | 1 (2.5) |
| Other | 0 | 3 (12) |
| Marital status (n, %) | ||
| Married | 18 (55) | |
| Single, never married | 9 (27) | |
| Divorced/Separated | 6 (18) | |
| Years in practice (mean, SD) | 13.7 (±9.3) | |
| Dual appointment at university (n, %) | 17 (43) | |
| Highest level of education (n, %) | ||
| Graduate or post graduate | 7 (21) | |
| Bachelor’s degree (BA or BS) | 1 (3) | |
| Associate Degree (AA or AS) or Trade/Technical/vocational school | 7 (21) | |
| High school graduate or some college credit but no degree | 16 (49) | |
| Some high school | 2 (6) | |
| Current work status (n, %) | ||
| Working full-time or part-time | 8 (24) | |
| Unemployed, searching for work | 1 (3) | |
| Student | 1 (3) | |
| Retired | 10 (30) | |
| Disabled | 13 (40) | |
| Annual household income (n, %) | ||
| Greater than $100,000 | 4 (12) | |
| $50,000-$99,999 | 13 (40) | |
| $25,000-$49,000 | 8 (24) | |
| Less than $25,000 | 7 (21) | |
| Declined to answer | 1 (3) | |
Bariatric surgery barriers within Andersen’s Framework
Eight themes were mapped onto Andersen’s model as barriers to bariatric surgery (Table 2). Two themes were categorized as “predisposing” contextual determinants within the “social” and “beliefs” categories in Andersen’s model. Six of the eight study themes fit within Andersen’s “organization” category, which is an “enabling” contextual determinant. Each theme that was identified within a participant group was reported in Table 3. Representative quotes for each theme from the perspectives of each participant group were included in Table 4. The eight study themes were:
Limited access to healthy foods – Within the “social” category, limited access to healthy foods was a barrier. One PCP located at “inner-city” VA reported that patient “access to healthy food probably isn’t great.” Veterans reported difficulty obtaining foods such as fruits and vegetables at food pantries, while noting that processed foods were easily obtained.
Not referring patients for bariatric surgery early enough or at all – PCPs acknowledged discomfort with referring patients for surgery. One PCP alluded to concerns about the risks of bariatric surgery: “It’s not a totally benign surgery by any means. There can be a lot of morbidity associated with it, so if you don’t choose the patient right…” PCPs also reported they had been “more conservative with bariatric surgery referrals than other healthcare areas.” Bariatric surgeons highlighted discussions with patients who felt that they deserved referral for bariatric surgery, but did not get one from their PCP. One Veteran stated that he worked with a nutritionist who shared that she “had never got that doctor to approve anybody” for bariatric surgery.
Poor coordination of care between services and providers – All five study participant groups – PCPs, bariatric surgeons, RDs, health psychologists and patients – felt that severe obesity care was poorly coordinated. PCPs were concerned that Veterans were not getting consistent messages across providers and reported that transmitting information between hospitals and clinics through the electronic health record was problematic at times. One PCP remarked, “Primary care doesn’t always hear when the patient is going [for bariatric surgery] unless we are specifically notified. And then, did the patient have surgery since we’re in a different system? I don’t get any alert that the patient was admitted to the [VA medical center] unless they have surgery, until the patient comes back or we get a follow up.” RDs suggested that the preoperative evaluation process could be “streamlined” and involve more teamwork. One RD stated that “if we had a bariatric team where consults came in and we had the surgeon, the dietitian, a pharmacist, all talking about that patient and saying ‘yes this patient is a good medical candidate’ or ‘no, this patient is not’ that would be ideal. Veterans also expressed concerns about continuity of care because they were evaluated by different clinicians at facilities that were different from where their operations took place.
Long travel distances for patients – PCPs, bariatric surgeons, RDs, and Veterans all reported that travel distances to reach one of the 21 bariatric surgery centers in VA could be long. One Veteran remarked, “I live in one part of [City], and [VA medical center] was like, it takes me about forty, fifty minutes. And that’s if somebody’s driving….that’s just a hassle.”
Lack of pre- and post-operative guidelines for patient care – All provider groups reported that a lack of pre- and post-operative guidelines was a barrier to care. PCPs felt uncomfortable given they were often responsible for a significant amount of post-operative care, including monitoring vitamin levels and adjusting vitamin regimens. One PCP remarked, “the dietitian did all the lab ordering and now that dietitian’s gone. And that patient is just mine. I just keep ordering the same labs.” Bariatric surgeons, health psychologists and RDs felt that standardization of the pre-operative evaluation process would be helpful.
Lack of education and training about bariatric surgery care – All provider groups reported that referring providers, often PCPs, lacked knowledge and felt uncomfortable managing bariatric surgery patients. One PCP remarked, “it’s not talked a lot about in our VA. It doesn’t seem like a lot of people are [aware] this is an option. We should be doing this for more patients. I don’t feel like it’s being promoted or encouraged.” One bariatric surgeon reported an interaction with a PCP in which the PCP stated that “I don’t believe in bariatric surgery.” The surgeon also felt that some referring providers, “for some reason, with their weight bias or obesity bias, don’t even think that this is a valid option, despite all the research saying it is.”
Difficulty meeting preoperative requirements – PCPs, bariatric surgeons, RDs, and Veterans identified patient inability to meet preoperative requirements, which are established by each bariatric surgery program, as barriers to undergoing bariatric surgery. One preoperative requirement that was difficult for participants was attendance at a minimum number of dietitian visits. According to one bariatric surgeon, “I think a lot of the hurdles…with like six months of [dietitian visits that one bariatric surgery program requires], patients just kind of get disinterested and fall off the map.” Lack of childcare, travel distances, and work-related constraints made attendance at these visits challenging.
Lack of provider availability and/or time – PCPs, bariatric surgeons, and RDs all noted limitations in availability and/or time. One PCP remarked, “sometimes there is no time to talk about those things [referring to obesity], especially if the patient doesn’t bring it up.” An RD stated that “with sixty people in a class, and there’s only two of us, two dietitians up there leading the class, you can only individualize so much.” Bariatric surgeons identified limited OR space as another constraint on their availability. “The [bariatric surgery centers] are also doing heart surgery, often complex orthopedic surgery…so all those services have to be satisfied within the limited OR space.”
Table 2.
Contextual determinants (per Andersen’s Behavioral Model of Health Services Use) that are barriers to bariatric surgery within VA
| Contextual determinant | Contextual determinant description according to Andersen’s Model | Study theme |
|---|---|---|
| Predisposing | ||
| Social | Measures of how patients’ communities might affect their access to health services; also may include socioeconomic composition of providers | 1. Limited access to healthy foods |
| Beliefs | Refers to the underlying attitudes, values, and knowledge of a community, organization, or provider regarding disease management and how health services should be organized and made accessible | 2. Not referring patients for bariatric surgery early enough or at all |
| Enabling | ||
| Organization | The amount, distribution, and connectedness of hospitals, clinics, and healthcare personnel available for a given service (e.g. bariatric surgery), as well as how care is delivered at a given institution | 3. Poor coordination of care between services and providers |
| 4. Long travel distances for patients | ||
| 5. Lack of pre- and post-operative guidelines for patient care | ||
| 6. Lack of education and training about bariatric surgery care | ||
| 7. Difficulty meeting preoperative requirements | ||
| 8. Lack of provider availability and/or time |
Table 3.
Barriers to bariatric surgery from provider and patient perspectives
| Contextual determinant | Theme | PCP | Bariatric surgeon | Registered dietitian | Health psychologist | Veteran |
|---|---|---|---|---|---|---|
| Social | 1. Limited access to healthy foods | X | X | |||
| Beliefs | 2. Not referring patients for bariatric surgery early enough or at all | X | X | X | ||
| Organization | 3. Poor coordination of care between services and providers | X | X | X | X | X |
| 4. Long travel distances for patients | X | X | X | X | ||
| 5. Lack of pre- and post-operative guidelines for patient care | X | X | X | X | ||
| 6. Lack of education and training about bariatric surgery care | X | X | X | X | ||
| 7. Difficulty meeting preoperative requirements* | X | X | X | |||
| 8. Lack of provider availability and/or time | X | X | X |
X indicates the barrier was identified as a theme during interviews with that type of study participant
Preoperative requirements are established by each bariatric surgery program independently and are not requirements of the national MOVE! program or National Surgery Office.
Table 4.
Representative provider and patient quotes regarding barriers to bariatric surgery
| Theme | PCP | Bariatric surgeon | Registered dietitian | Health psychologist | Veteran |
|---|---|---|---|---|---|
| 1. Limited access to healthy foods | “I guess it’s hard. We’re an urban, inner-city VA. A lot of our patients…I would say their access to healthy food probably isn’t great.” | Not discussed | Not discussed | Not discussed | “I get a lot of my food out of the food pantry and they’re not giving a lot of fresh vegetables and fruits. They’re giving you rice and mashed potatoes, cheese and spaghetti noodles…” |
| 2. Not referring patients for bariatric surgery early enough or at all | “I’d say, yeah, we’ve probably been a little bit more conservative [with bariatric surgery referrals] than other healthcare areas is my guess.” | “There’s a lot that rests on the decision making and prejudices of the PCP. We have heard from patients who have made it to our clinic who felt that they were stuck for a long time at the level of the PCP who for one reason or another did not think a referral was appropriate.” | Not discussed | Not discussed | “The doctor that I had…he had never approved somebody. I was the one that had made it the farthest in the nine years that the nutritionist had worked with that doctor. She had never got that doctor to approve anybody.” |
| 3. Poor coordination of care between services and providers | “Well one of the biggest problems is, because it’s going from facility to facility sometimes the transmission of information [through the electronic health record] isn’t that good.” | “There’s so many different groups involved that it’s not uniform. My personal fantasy would be to create like a bariatric super group in the VISN. And provide it either via telehealth where they’re getting a consistent message.” | “I think that the referrals for these surgeries could be streamlined a little bit more, if we had a team here that was a bariatric team where consults came in and we had the surgeon, the dietitian, a pharmacist, all talking about that patient and saying “yes this patient is a good medical candidate…” | “It doesn’t seem that we have state-of-the-art, multi-disciplinary, organized collaborative care for this, around this health issue in Veterans.” | “I was going to see people about diabetes, I’d see somebody different every time. And that would really cause me problems because one would contradict what the other had said. Nobody really knew my story.” |
| 4. Long travel distances for patients | “They have to travel far from home to get a surgery and that can be really hard on a patient. Just the travel, no support, and a place that’s two hours away.” | “You’re probably not going to be getting [bariatric surgery], at least not here, when you have to travel many, many hours to get here. You want to first and foremost be safe, do a safe procedure...that they go home safely.” | “There aren’t as many facilities doing bariatric surgery so they have to travel, possibly farther, to a surgical center.” | Not discussed | “I live in one part of [city]. And [VA medical center] was like, it takes me about forty, fifty minutes. And that’s if somebody’s driving…that’s just a hassle.” |
| 5. Lack of pre- and post-operative guidelines for patient care | Interviewer: “Was it clear to you what the plan was?” PCP: “You know it wasn’t made clear to me…The dietitian did all the lab ordering and now that dietitian’s gone. And that patient is just mine. I just keep ordering the same labs.” |
“If they would standardize the referral across the VA…I think they need to have a bariatric handbook again that addresses this so that the referring hospital knows exactly what they have to do and what their responsibilities are. Right now it’s helter-skelter. There’s no rules about bariatric surgery. There’s no handbook to guide it in the VA.” | “The PCPs…I don’t know if they encourage surgery as much, because of the fact that they don’t really know. Or they’re a little anxious about what would happen after, kind of thing.” | “My understanding [is that] that there’s no kind of standard practice within the VA…regionally, programs just make their own decisions.” | Not discussed |
| 6. Lack of education and training about bariatric surgery care | “The other thing about bariatric surgery was, I was a little bit terrified because they just send them back to you as a PCP who has no experience in post-op bariatric surgery care, and they expect you to do all of it. And, they will not help.” | “I’ve actually had the primary say flat out, ‘I don’t believe in bariatric surgery’… the providers for some reason, with their weight bias or obesity bias, don’t even think that this is a valid option, despite all the research saying it is.” | “I’m much more open to [bariatric surgery] as an option for people than I was in the past...When I see people who are significantly overweight, and the demoralization, the lack of confidence in themselves for making change, or the discomfort that they feel. Those that have really tried in the past and had limited results, I feel like it’s a viable option. And then the medical, the improvements in their medical [comorbidities] afterwards are pretty amazing.” | “I think sometimes they’re getting that from their physicians who refer them. So like the orthopedic doctors will say, ‘Oh you need to lose a hundred pounds for us to do a knee replacement, go get bariatric surgery and well check in with you in a few months and do the surgery.’ | Not discussed |
| 7. Difficulty meeting preoperative requirements * | There’s just a lot of no’s from [VA]. I mean, I don’t know how perfect you can be. I mean massively obese people have issues. They all have issues and it was so hard and so frustrating to try to get through this intensive, first the three months and then all the various stuff and back and forth.” | “I think a lot of the hurdles with like six months of MOVE!, etc. patients just kind of get disinterested and fall off the map.” | Not discussed | Not discussed | “I’m still really interested in [bariatric surgery]. It’s just very difficult. Like I said it’s just a pain to get everything together and talk to everybody at the same time and get everybody on the same page.” |
| 8. Lack of provider availability and/or time | “Sometimes there is no time to talk about those things (referring to obesity) especially if the patient doesn’t bring it up.” | “Bariatric surgery is done in places that perform complex surgery, and it’s appropriate. But those centers are also doing heart surgery, often complex orthopedic surgery…so all those services have to be satisfied within the limited OR space.” | “With sixty people in a class, and there’s only two of us…two dietitians up there leading the class, you can only individualize so much.” | Not discussed | Not discussed |
Preoperative requirements are established by each bariatric surgery program independently and are not requirements of the national MOVE! program or National Surgery Office.
DISCUSSION
Veterans with severe obesity and obesity care providers encountered numerous contextual or systems barriers to obesity care within the Veterans Health Administration system. All groups reported that coordination of care between clinical services and providers was a challenge. All provider groups noted that the absence of bariatric surgery care guidelines and limited education about bariatric surgery care were barriers to care. Veterans and nearly all provider groups reported that long travel distances were barriers to obesity care. Patients and PCPs also identified limited access to healthy foods and delayed referrals to bariatric surgery as obstacles.
Though the VA system has more than 170 medical centers, bariatric surgery occurs at only 21 of these medical centers.16 This system requires coordination of care across many different VA medical centers and clinical specialties. Our study participants found this to be challenging. In 2016, experts at the VA “State of the Art Conference” on Weight Management reported challenges and potential solutions to obesity care coordination.26 Identifying which VA providers were responsible for tracking patients and outcomes was identified an important barrier, particularly because these responsibilities were not typically assigned to specific providers or service lines (e.g. primary care or bariatric surgery). The authors felt that it was unrealistic to expect primary care teams to coordinate weight management services given the high prevalence of obesity in Veteran populations.26
In 2019, McDonald and colleagues reviewed four care coordination initiatives within VA: primary care, “complex patients,” medication management, and transitions between care systems.27 A theory-based approach was used to examine the context, locus (setting, level and purpose) and design for these systematically implemented care coordination programs throughout VA. A similar approach could be used to establish a severe obesity and bariatric surgery care coordination program. Solutions that have been considered for other chronic diseases include the establishment of “care trackers” for Veterans with cancer to help them navigate the medical system during multiple visits with different providers.28 Creating provider “points of contact” who serve as clinical leaders for patients and establishing “patient liaisons” who streamline communication between patients and providers are options that have been discussed.
Given that bariatric surgery patients are required to have multiple visits with the RD, health psychologist, and surgeon over the course of at least several months, many Veterans are unable to travel to the bariatric center for each visit. Travel distances to VA bariatric surgery centers can also be long. One of VA’s 21 bariatric surgery programs (Palo Alto) reported that patients traveled an average of 236 miles to undergo bariatric surgery.29 The creation of multidisciplinary care teams that incorporate telemedicine into bariatric surgery care is one systems-based initiative that has been piloted within VA.30 Sudan and colleagues published the results of their telemedicine bariatric surgery program in 2011 and found that Veterans who lived an average of more than 300 miles from their VA bariatric surgery center were satisfied with their program, which involved teleconferencing and use of the electronic health record.30 Of note, telemedicine visits tripled over the 5-year study period at the center that implemented the program.
National telemedicine programs focused more on weight management have also been implemented in VA and could be applied to bariatric surgery patients. TeleMOVE, which was piloted from 2009 to 2011 at 9 demonstration sites, involved Veterans having in-home messaging devices through which they received daily messages about weight management. Veterans reported their weight back to clinicians who were monitoring their progress.31 Weight loss was comparable for TeleMOVE and in-person MOVE! participants 6 months after enrollment (approximately 5 pounds). Telemedicine programs in VA have been implemented for other conditions including dementia,32 dermatologic diseases,33 and urologic care.34
Our participants reported that a lack of clear guidelines was a barrier to care. In 2010, the VA National Center for Health Promotion and Disease Prevention created a reference manual for the VA behavioral weight management program, MOVE!. This reference includes a “Bariatric Surgery Quick Reference” chapter and general information about pre- and post-operative care and is publicly available on-line.35 Our findings suggest that this reference is not well known and is likely not used in a systematic manner in our region or others. Additionally, the most commonly performed bariatric procedure – sleeve gastrectomy – is not included in the reference. Updating this guideline, possibly by convening a multi-disciplinary group of VA bariatric surgery care experts, and disseminating it throughout the VA system in a systematic manner may be one effective way to address these concerns.
All provider participant types also reported that limited bariatric surgery-related education and training for PCPs and referring providers was a barrier to care. PCPs participants acknowledged that this likely contributed to another barrier, late or non-existent bariatric surgery referrals. PCPs reported being uncomfortable with post-operative care and management of surgical complications and were less likely to refer patients. Similarly, a focus group study of non-VA PCPs published in 2016 found that limited PCP knowledge of bariatric surgery was a barrier to referral.36 Ferrante and colleagues surveyed 255 non-VA PCPs and concluded that those with better knowledge of bariatric surgery were more likely to recommend it.37 These study findings suggest that there is a significant disconnect between PCP and bariatric surgeon perspectives on the safety and effectiveness of bariatric surgery. Bariatric surgery education for PCPs and improved communication between PCPs and bariatric surgeons may help bridge this gap.
This study has several limitations. First, although we interviewed a nationally representative sample of VA bariatric surgeons from all five VA regions, our interviews with the other types of providers and patients were all from the Midwest region. Some of the barriers identified by these participant groups may not present for Veterans in other VA regions. Second, our interview guides did not explicitly target all six contextual determinants within Andersen’s Behavioral Model of Health Services Use. The other three determinants – provider demographics, health policy and financing – should be analyzed with other research approaches, such as population-based provider surveys and policy analysis. Third, recall bias may have impacted our interview results. However, most of the themes identified in our analysis were reported by multiple types of participant groups, including both patients and providers.
In conclusion, to address what one previous VA National Director of Surgery described as a “woefully low” number of bariatric procedures performed in the VA system,16 system-based solutions that more strongly support collaboration and communication between patients and providers across the VA system and enhance provider knowledge are important. These challenges are not unique to adults with obesity, nor are they present only in the VA system. Theory-based solutions are available and should be pursued in a multidisciplinary fashion to ensure optimal outcomes and access for our Veterans.
Supplementary Material
ACKNOWLEDGMENTS
Effort on this study and article was made possible by a VA Career Development Award to Dr. Funk (CDA 15-060). Dr. Voils was supported by a VA Career Scientist Award (RCS 14-443). The views represented in this article represent those of the authors and not those of the VA or the U.S. Government. This research was also supported by an American College of Surgeons George H.A. Clowes Career Development Award (Dr. Funk). Dr Alagoz, Ms. Jolles, Ms. Shea, Dr. Gunter, Dr. Raffa, and Dr. Voils declare no conflicts of interest for the work under consideration for publication.
Both funding sources (the Veterans Health Administration and the American College of Surgeons) provided funding which allowed our research group to design/conduct the study and collect, manage, analyze, and interpret the data. Neither funding source was involved in the preparation, review, or approval of the manuscript or the decision to submit the manuscript for publication.
Dr. Funk had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Conflicts of interest and Sources of Funding: Effort on this study and manuscript was made possible by a VA HSR&D Career Development Award to Dr. Funk (CDA 15-060) and a VA Research Career Scientist award to Dr. Voils (RCS 14-443) as well as an American College of Surgeons George H. A. Clowes, Jr., MD, FACS, Memorial Research Career Development Award to Dr. Funk. The views represented in this article represent those of the authors and not those of the Department of Veterans Affairs or the US Government. The authors declare no conflicts of interest related to these funding sources.
REFERENCES
- 1.Chang SH, Stoll CR, Song J, et al. The Effectiveness and Risks of Bariatric Surgery: An Updated Systematic Review and Meta-analysis, 2003–2012. JAMA Surg 2013;149(3):275–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sjostrom L, Lindroos AK, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med 2004;351(26):2683–93. [DOI] [PubMed] [Google Scholar]
- 3.Sjostrom L, Narbro K, Sjostrom CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med 2007;357(8):741–52. [DOI] [PubMed] [Google Scholar]
- 4.Christou NV, Sampalis JS, Liberman M, et al. Surgery decreases long-term mortality, morbidity, and health care use in morbidly obese patients. Ann Surg 2004;240(3):416–23; discussion 23–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ikramuddin S, Korner J, Lee WJ, et al. Roux-en-Y gastric bypass vs intensive medical management for the control of type 2 diabetes, hypertension, and hyperlipidemia: the Diabetes Surgery Study randomized clinical trial. JAMA 2013;309(21):2240–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mingrone G, Panunzi S, De Gaetano A, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med 2012;366(17):1577–85. [DOI] [PubMed] [Google Scholar]
- 7.Schauer PR, Kashyap SR, Wolski K, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med 2012;366(17):1567–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric Surgery versus Intensive Medical Therapy for Diabetes - 3-Year Outcomes. N Engl J Med 2014;370:2002–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Heshka S, Anderson JW, Atkinson RL, et al. Weight loss with self-help compared with a structured commercial program: a randomized trial. JAMA 2003;289(14):1792–8. [DOI] [PubMed] [Google Scholar]
- 10.Flum DR, Salem L, Elrod JA, et al. Early mortality among Medicare beneficiaries undergoing bariatric surgical procedures. JAMA 2005;294(15):1903–8. [DOI] [PubMed] [Google Scholar]
- 11.Chaar ME, Lundberg P, Stoltzfus J. Thirty-day outcomes of sleeve gastrectomy versus Roux-en-Y gastric bypass: first report based on Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program database. Surg Obes Relat Dis 2018;14(5):545–51. [DOI] [PubMed] [Google Scholar]
- 12.Ingraham AM, Cohen ME, Ko CY, et al. A current profile and assessment of north american cholecystectomy: results from the american college of surgeons national surgical quality improvement program. J Am Coll Surg 2010;211(2):176–86. [DOI] [PubMed] [Google Scholar]
- 13.Sturm R, Hattori A. Morbid obesity rates continue to rise rapidly in the United States. Int J Obes 2013;37(6):889–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Estimate of Bariatric Surgery Numbers, 2011–2017. (Accessed February 1, 2019, at https://asmbs.org/resources/estimate-of-bariatric-surgery-numbers.)
- 15.Breland JY, Phibbs CS, Hoggatt KJ, et al. The Obesity Epidemic in the Veterans Health Administration: Prevalence Among Key Populations of Women and Men Veterans. J Gen Int Med 2017;32(Suppl 1):11–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gunnar W Bariatric Surgery Provided by the Veterans Health Administration: Current State and a Look to the Future. J Gen Intern Med 2017;32(Suppl 1):4–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Funk LM, Gunnar W, Dominitz JA, et al. A Health Services Research Agenda for Bariatric Surgery Within the Veterans Health Administration. J Gen Intern Med 2017;32(Suppl 1):65–69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346(6):393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.QSR International Pty Ltd. Version 11.
- 20.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15(9):1277–88. [DOI] [PubMed] [Google Scholar]
- 21.Charmaz K Constructing Grounded Theory: a practical guide through qualitative analysis: Sage Publications, Ltd; 2006. [Google Scholar]
- 22.Miles MB, Huberman AM. Qualitative Data Analysis: An expanded sourcebook. Second edition ed. Thousand Oaks: Sage Publications, Inc; 1994. [Google Scholar]
- 23.Babitsch B, Gohl D, von Lengerke T. Re-revisiting Andersen’s Behavioral Model of Health Services Use: a systematic review of studies from 1998–2011. Psychosoc Med 2012;9:Doc11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Imbus JR, Voils CI, Funk LM. Bariatric surgery barriers: a review using Andersen’s Model of Health Services Use. Surg Obes Relat Dis 2018;14(3):404–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cordasco KM, Hynes DM, Mattocks KM, Bastian LA, Bosworth HB, Atkins D. Improving Care Coordination for Veterans Within VA and Across Healthcare Systems. J Gen Intern Med 2019;34(Suppl 1):1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Raffa SD, Maciejewski ML, Zimmerman LE, et al. A System-Level Approach to Overweight and Obesity in the Veterans Health Administration. J Gen Intern Med 2017;32(Suppl 1):79–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McDonald KM, Singer SJ, Gorin SS, et al. Incorporating Theory into Practice: Reconceptualizing Exemplary Care Coordination Initiatives from the US Veterans Health Delivery System. J Gen Intern Med 2019;34(Suppl 1):24–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zuchowski JL, Chrystal JG, Hamilton AB, et al. Coordinating Care Across Health Care Systems for Veterans With Gynecologic Malignancies: A Qualitative Analysis. Med Care 2017;55 Suppl 7 Suppl 1:S53–S60. [DOI] [PubMed] [Google Scholar]
- 29.Eisenberg D, Lohnberg JA, Kubat EP, et al. Systems innovation model: an integrated interdisciplinary team approach pre- and post-bariatric surgery at a veterans affairs (VA) medical center. Surg Obes Relat Dis 2017;13(4):600–6. [DOI] [PubMed] [Google Scholar]
- 30.Sudan R, Salter M, Lynch T, et al. Bariatric surgery using a network and teleconferencing to serve remote patients in the Veterans Administration Health Care System: feasibility and results. Am J Surg 2011;202(1):71–6. [DOI] [PubMed] [Google Scholar]
- 31.Goodrich DE, Lowery JC, Burns JA, et al. The Phased Implementation of a National Telehealth Weight Management Program for Veterans: Mixed-Methods Program Evaluation. JMIR Diabetes 2018;3(3):e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chang W, Homer M, Rossi MI. Use of Clinical Video Telehealth as a Tool for Optimizing Medications for Rural Older Veterans with Dementia. Geriatrics (Basel) 2018;3(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Baranowski MLH, Balakrishnan V, Chen SC. Patient Satisfaction with the Veteran’s Administration Teledermatology Service. J Am Acad Dermatol 2019. pii: S0190–9622(19)30143–4. [DOI] [PubMed] [Google Scholar]
- 34.Chu S, Boxer R, Madison P, et al. Veterans Affairs Telemedicine: Bringing Urologic Care to Remote Clinics. Urology 2015;86(2):255–60. [DOI] [PubMed] [Google Scholar]
- 35.Bariatric Surgery. MOVE! Weight Management Program Reference Manual. (Accessed August 6, 2019, at https://www.move.va.gov/docs/moveReferenceManual/11_BariatricSurgery.pdf.)
- 36.Funk LM, Jolles SA, Greenberg CC, et al. Primary care physician decision making regarding severe obesity treatment and bariatric surgery: A qualitative study. Surg Obes Relat Dis. 2016. May;12(4):893–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ferrante JM, Piasecki AK, Ohman-Strickland PA, et al. Family physicians’ practices and attitudes regarding care of extremely obese patients. Obesity 2009;17(9):1710–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.