Abstract
COVID-19 has brought tremendous and abrupt threats to various aspects of our daily lives, from school and work to interpersonal relationships. Self-compassion is put forth as a salutogenic perspective on oneself that buffers the adverse mental health impacts of these threats. During the peak of a local outbreak in Hong Kong in Spring 2020, 761 participants completed questionnaires on self-compassion, perceived threats, as well as perceived benefits and psychological distress. Controlling for demographic variables, negative indicators of self-compassion (aka self-coldness) was found to intensify the impacts of threats on psychological distress. The positive indicators of self-compassion also moderated the link between threats and perceived benefits, such that perceived benefits tend to be less related to threats in participants with higher self-compassion. Our findings highlight the impacts of both positive and negative indicators of self-compassion on the adjustment to such unprecedented challenges, and point to the possibility of enhancing people's resilience through fostering self-compassion and alleviating self-coldness.
Keywords: self-compassion, mental health, perceived benefit, COVID-19, Hong Kong, self-coldness
Introduction
The Coronavirus Disease-2019 (COVID-19) has imposed unprecedented changes to our everyday lives. In countries where cities were locked down, citizens were forced into furlough or work-/school-at-home arrangements with wide-spread suspension of services and businesses, entailing pervasive loneliness, and sense of insecurity (1, 2). The perfect storm from coupling psychological tension with 24/7 interactions with one's family in an enclosed space breeds conflicts or even domestic violence (3).
This study was conducted during the peak of the Spring 2020 outbreak in Hong Kong, when public health orders banning public gatherings, restricting catering capacity of restaurants to half and mandating closure of high-risk businesses were enforced for the first time after reports of infection clusters in March. Conceivably, these measures have drastically changed the citizens' daily routines and resulted in enormous challenges to the local businesses and the civil society, especially after months of conflicts during the Anti-extradition law amendment bill (Anti-ELAB) movement (4). In fact, Hong Kong experienced the worst drop in year-to-year GDP (8.9%) during Spring 2020 where the worst wave of local outbreak occurred, whilst the unemployment rate has reached a 15-years high (5.9%) (5). The ban on mass gatherings and apprehension over physical socializing has also hindered connections among stakeholders of the civil society, adversely impacting the community support networks. In such unprecedentedly challenging time, this study was conducted to explore how self-compassion, defined as a warm, kind and non-judgmental attitude to oneself during setbacks, modulates individuals' adjustment to the pandemic-related threats (6).
Neff proposed that self-compassion entails (i) extending kindness and understanding to oneself rather than treating oneself with harshness and criticism (self-kindness vs. self-judgment), (ii) seeing one's suffering as a part of the shared human experience rather than an isolated experience (common humanity vs. isolation), and (iii) a balanced perspective of one's suffering rather than overly attached to it (mindfulness vs. over-identification) (6). Accordingly, meta-analyses have reported robust negative associations of self-compassion with psychopathology and positive associations with well-being (7–9).
Self-compassion may modulate how people confront threats by encouraging adaptive coping responses. Allen and Leary summarized the associations between self-compassion and coping styles (10). Self-compassion tends to foster positive reappraisal and proactive coping and reduce avoidant behaviors. Evidence regarding self-compassion's salutary effects on problem-solving, support seeking and distraction was however mixed. Allen and Leary postulated that these associations could be qualified by perceived control, such that people with higher self-compassion exhibit higher proactivity (vs. passivity) when perceived control is higher (vs. lower) (10). Another line of research suggests that self-compassion induces favorable emotional regulation (e.g., emotion clarity, impulse control, acceptance of emotional response) which in turn engenders mental health benefits (11, 12). From a self-regulation perspective, self-compassion may facilitate healthy attainment of goals by facilitating proactivity, enabling one to take responsibility to both success and failure, evaluating the situation with equanimity, disengaging from relentless pursuits and countering the toxic effects of guilt and embarrassment (13–15). Accordingly, self-compassion moderated the impacts of stressors on well-being and adjustment in various samples, including women with breast cancer, college students, women with restricting eating tendencies, and even in a laboratory-induced stressful setting (16–19).
Self-compassion is often assessed with the full- or short-version of Self-Compassion Scale [SCS; (20, 21)]. Both versions assume a higher-order single factor structure and a six-factor structure encompassing three positive (self-kindness, mindfulness, common humanity) and three negative (self-judgment, over-identification, and isolation) factors. Thus, responses on the negative indicators are often reversed to attain an overall scale score of self-compassion. However, the construct validity of these scales is contentions, as many studies failed to replicate the six-factor model, but instead, yielded a bifactor structure with distinct but related positive (self-compassion/self-reassuring) and negative factors (self-coldness/self-criticism) (22–24).
Moreover, the positive and the negative factors appear to be asymmetrically related to psychopathology and well-being. Muris and Petrocchi found that while the positive and the negative indicators are related to psychopathology in expected directions, comparisons over the strengths of the relationships revealed the negative indicators as significantly stronger predictors than the positive ones (9). Such an observation indicates the possibility of an inflated association between self-compassion and psychopathology when the overall scale score, with the oppositely-phrased items reversed, has been used. In fact, the tendencies to be reassuring vs. critical to oneself rely on distinct biological impetuses. Longe et al. found that self-reported measures of self-criticism were associated with areas for error-processing and behavioral inhibition, including the dorsolateral prefrontal cortex, and those of self-reassurance with areas of empathy, including the ventrolateral prefrontal cortex (25). Accordingly, Brenner et al. proposed a theoretical model of self-relating based on Gilbert's theories of social mentalities (26–28). While self-compassion, which stems from a safeness system rooted in the parasympathetic nervous system, infers a non-judgmental, caring lens to own sufferings and therefore encourages positive connections to oneself and others; self-coldness, which stems from a threat-defense system rooted in the sympathetic nervous system, indicates a tendency to be critical, judgmental and overly attached to one's suffering, and exhibit vigilance or avoidance in behaviors toward others.
A bifactor model that distinguishes self-compassion from self-coldness may better fit how Asians affectively evaluate things in general. For instance, a dialectical thinking style, which has roots in Asian philosophies and religions (e.g., Confucianism and Buddhism), facilitates tolerance and flexible integration of affectively opposite judgments and coping strategies (29, 30). The Chinese circumplex model of affect also postulates the positive and the negative affect as independent but associated constructs, rather than two poles on the same line (31). Hence, we reckon that in the ethnic context of Hong Kong, it may make more sense to assume individuals can exhibit both self-compassion and self-coldness, although likely to different degrees and on different aspects of even the same event. For instance, one can be compassionate about one's worsening job prospect due to the financial meltdown, but still be self-critical about not being industrious enough to follow up with every client.
In this study, we tested the moderation effects of self-compassion and self-coldness simultaneously on the impacts of pandemic-related perceived threats on well-being. Also, as self-compassion and self-coldness may be differentially associated with well-being and psychopathology, we tested on outcomes indicating both negative and positive adaptations (26). The negative impacts were indicated by psychological distress that encompasses symptoms of anxiety and depression. Perceived benefits experienced in the pandemic were used to indicate positive adaptation to the challenging situation (32, 33). We expected self-compassion to buffer the positive relationship between perceived threats and psychological distress, as well as the negative relationship with perceived benefits. In other words, individuals with higher self-compassion should experience less emotional harm from threats and that their perceived benefits will be less hampered by threats. Brenner et al. put forth self-coldness as a separate vulnerability factor (26). We therefore anticipated self-coldness to intensify the positive relationship between perceived threats with psychological distress and the negative relationship with perceived benefits. That is, individuals with higher self-coldness should be more susceptible to the emotional harm from perceived threats and that their perceived threats should hamper perceived benefits more.
Methods
Design
This is a part of a longitudinal study on how people of Hong Kong adjust to the COVID-19 pandemic. The current analysis utilized only the cross-sectional data collected between mid-March to early-April 2020, right after the World Health Organization declaring COVID-19 a pandemic (34). The study was approved by the Human Research Ethics Committee of the University of Hong Kong (EA2003003).
Participants
Adults aged 18 or above residing in Hong Kong were eligible for the study. Participants who could not read traditional Chinese or had no access to the internet were excluded. Conducted as a swift response to the situation, participants were recruited through snowballing by social media and email lists. Participants were reimbursed HKD$50 in cash or supermarket coupons for participating in the current survey.
Instruments
Perceived Threats
Participants were asked to rate the extent to which the pandemic has rendered threats to their (i) work/academic life, (ii) personal finance, (iii) family relationships, and (iv) social life on a 10-point scale running from 1 (not at all) to 10 (extremely). The four self-constructed items were averaged to form an overall perceived threats scale, with good reliability (Cronbach α = 0.79).
Self-Compassion and Self-Coldness
The 12-item Self-Compassion Scale Short Form [SCS-SF; (21)] were used. These twelve short-form items were drawn from the published translation of the Chinese Self-Compassion Scale (35). Participants answered on a 5-point scale running from 1 (almost never) to 5 (almost always). The positive subscale (self-compassion) included the six items on self-kindness, mindfulness and common humanity, whereas the negative subscale (self-coldness) encompassed the six items on self-judgment, over-identification and isolation. The subscale scores were obtained by taking the average across responses on the items. The reliability of the two subscales were adequate with Cronbach alphas of 0.83 (positive) and 0.81 (negative), respectively.
Psychological Distress
Psychological distress over the past 2 weeks was measured by the Patient Health Questionnaire-4 [PHQ-4; (36)]. The first two items indicated anxiety levels and were taken from the Generalized Anxiety Disorder-7 [GAD-7; (37)]; while the last two items were from the Patient Health Questionnaire-2 (PHQ-2) that has been used for screening depression (38). These items were drawn from the published translation of the Chinese GAD-7 and PHQ-2 (39, 40). Participants answered on a four-point scale running from 0 (not at all) to 3 (nearly everyday). A summed response exceeding 5 indicates moderate to severe psychological distress. The reliability of the scale was good (Cronbach α = 0.87).
Perceived Benefits
Eleven self-constructed items were employed to indicate perceived benefits experienced by our participants during the pandemic (34). Example items include “The pandemic afforded me more time for rest and relaxation,” “I learned a new skill/knowledge from the pandemic,” and “I gained greater trust in the power of the citizens.” Participants answered on a seven-point scale running from 1 (strongly disagree) to 7 (strongly agree). The scale score was derived by taking the average across the responses on the items. The scale exhibited good reliability (Cronbach α = 0.86).
Demographic information, such as gender, age, education background, marital status, income, religion as well as health and pandemic exposure related data, such as presence of a chronic health condition, co-residence with an individual vulnerable to a severe course of illness in case of infection (e.g., children, elderly, individuals with chronic illness, pregnant women, etc.), level of risk at occupational setting, SAR-CoV-2 test results (if any) and medical quarantine experience were also collected from the online survey. The online survey was conducted in traditional Chinese.
Statistical Analyses
Descriptive statistics were used to explore the levels of perceived threats, self-compassion, self-coldness, perceived benefits and psychological distress of the participants, while the intercorrelations among the key variables were scrutinized by Pearson's correlations. The moderating role of self-compassion and self-coldness were tested with SPSS PROCESS macro (version 3). Assuming a moderate effect size (f2 = 0.15), alpha of 0.05, power of 95% and 13 predictors (control variables, predictor variables and two interaction terms), a minimum of 189 participants were needed based on the calculation by G*Power (version 3.1.9.2). The current sample size exceeded what is minimally required for testing the model. The directions of the moderation effects were indicated by the effects of the focal predictor (i.e., perceived threats) on the outcome (i.e., psychological distress and perceived benefits) at 16th, 50th, and 84th percentile of the moderators (i.e., self-compassion and self-coldness). All analyses were conducted with SPSS (version 25.0).
Results
Sample Characteristics
Among the 761 participants (Table 1), 67.7% were female with age ranging from 18 to 79 [Mean (SD) = 40.31 (14.02)]. 62.4% of the sample received university education or above and 49.9% were married. 47.0% were affiliated to a religion. The median monthly family income was HKD$40,000–49,999, which was higher than the population median (HKD$27,000). About one-third of the participants (35.7%) reported they were working in a high-risk occupation (e.g., healthcare, retail, catering, and beverage, jobs that require frequent travel abroad). A quarter (24.6%) declared having at least one chronic physical or psychological illness, while about half of the sample (50.6%) were living with individuals vulnerable to a severe course of illness in case of COVID-19 infection. There were seven cases (0.9%) of positive test results of SAR-CoV-2 and 11 (1.4%) cases subjected to medical quarantine.
Table 1.
Sample characteristics (N = 761).
| N/M | Valid %/SD | |
|---|---|---|
| Gender | ||
| Female | 515 | 67.7 |
| Male | 246 | 32.3 |
| Age | 40.31 | 14.02 |
| Education backgrounds | ||
| Primary or less | 6 | 0.8 |
| Secondary | 157 | 20.6 |
| Higher diploma/Associate degree | 123 | 16.2 |
| Undergraduate | 262 | 34.4 |
| Post-graduate or above | 213 | 28.0 |
| Marital status | ||
| Single, divorced, separated, bereaved | 381 | 50.1 |
| Married | 380 | 49.9 |
| Income (in Hong Kong Dollar) | ||
| <10,000 | 57 | 7.5 |
| 10,000–19,999 | 91 | 12 |
| 20,000–29,999 | 107 | 14.1 |
| 30,000–39,999 | 89 | 11.7 |
| 40,000–49,999 | 86 | 11.3 |
| 50,000–69,999 | 132 | 17.4 |
| 70,000–89,999 | 85 | 11.2 |
| 90,000 or more | 114 | 15 |
| Religion | ||
| Yes | 358 | 47 |
| No | 403 | 53 |
| Own chronic health condition | ||
| Yes | 187 | 24.6 |
| No | 574 | 75.4 |
| Live with a vulnerable person | ||
| Yes | 385 | 50.6 |
| No | 376 | 49.4 |
| In a high-risk occupation | ||
| Yes | 272 | 35.7 |
| No | 489 | 64.3 |
Italics refers to M/SD = (means/standard deviation).
Both perceived threats and benefits from COVID-19 were moderate [Means (SDs) = 4.89 (2.10), 4.65 (0.99), respectively]. The mean of PHQ-4 was 3.29 (SD = 2.91). The percentages of participants showing none (score 0–2), mild (score 3–5), moderate (score 6–8), and severe (score 9–12) psychological distress were 46.3, 35.9, 11.4, 6.4%, respectively. In other words, 17.8% of the sample scored above the cut-off for moderate to severe psychological distress.
Table 2 shows the intercorrelations among the key variables. The negative association between self-compassion and self-coldness was moderate in magnitude. Perceived threats were positively related to psychological distress and self-coldness, but negatively associated with self-compassion. Self-compassion and self-coldness were negatively and positively related to psychological distress, respectively. Of note, perceived benefits were unrelated to perceived threats and psychological distress, but were positively and negatively correlated with self-compassion and self-coldness.
Table 2.
Intercorrelations among the key variables (N = 761).
| Mean (SD) | 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|---|
| 1. Self-compassion | 4.89 (2.10) | 1.00 | – | – | – | – |
| 2. Self-coldness | 3.59 (0.68) | −0.28*** | 1.00 | – | – | – |
| 3. Perceived threats | 3.19 (0.73) | −0.16*** | 0.28*** | 1.00 | – | – |
| 4. Psychological distress | 3.29 (2.91) | −0.29*** | 0.40*** | 0.41*** | 1.00 | – |
| 5. Perceived benefits | 4.65 (0.99) | 0.32*** | −0.11** | 0.06 | −0.06 | 1.00 |
SD, standard deviation.
* p < 0.05;
p < 0.01;
p < 0.001.
Moderating Roles of Self-Compassion and Self-Coldness
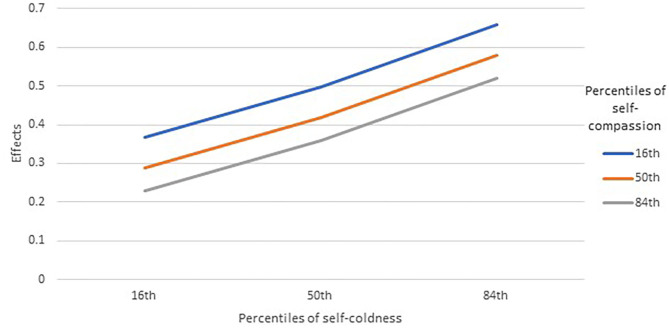
Table 3 provides the results of the moderation models. For psychological distress, the relationship with perceived threats was significantly moderated by both self-coldness (p = 0.0009) and self-compassion (p = 0.0439). Inspecting the effects of perceived threats on psychological distress at the 16th, 50th, and 84th percentiles of the moderators (Figure 1), self-coldness appeared to strengthen the positive association between perceived threats and psychological distress, while higher self-compassion was related to weaker positive association. The main effects of perceived threats, self-compassion, and self-coldness were non-significant.
Table 3.
Results of moderation models (N = 761).
| Psychological distress | Perceived benefits | |
|---|---|---|
| B (SE) | B (SE) | |
| Female (vs. male) | 0.36 (0.19) | 0.20 (0.07)** |
| Age | −0.00 (0.01) | 0.00 (0.00) |
| University educated (vs. no) | 0.08 (0.21) | −0.01 (0.08) |
| Income | −0.00 (0.03) | −0.01 (0.01) |
| Presence of own chronic health problems (vs. no) | 0.25 (0.22) | 0.02 (0.08) |
| Co-living with a vulnerable individual (vs. no) | 0.25 (0.18) | 0.02 (0.07) |
| Religious affiliation (vs. no) | −0.24 (0.18) | 0.04 (0.07) |
| In a high-risk occupation (vs. no) | 0.05 (0.19) | −0.05 (0.07) |
| Perceived threats | 0.24 (0.29) | 0.34 (0.11)** |
| Self-coldness | 0.13 (0.30) | 0.09 (0.11) |
| Self-compassion | −0.15 (0.32) | 0.73 (0.12)*** |
| Self-coldness × perceived threats | 0.19 (0.06)*** | −0.03 (0.02) |
| Self-compassion × perceived threats | −0.12 (0.06)* | −0.05 (0.02)* |
| Model summary: Δr2 | 0.2968*** | 0.1412*** |
B, unstandardized coefficient; SE, standard error.
p < 0.05;
p < 0.01;
p < 0.001.
Figure 1.
Moderation roles of self-compassion and self-coldness on the effects between perceived threats and psychological distress (N = 761). Effects were unstandardized coefficients of the conditional effects of perceived threats on psychological distress.
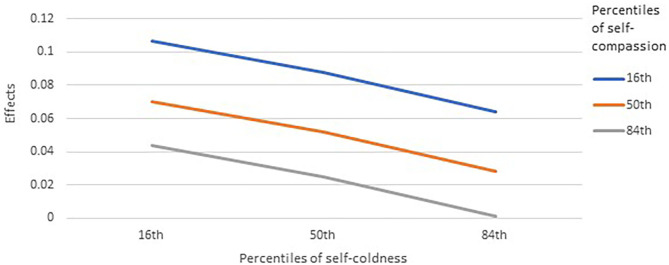
For perceived benefits, the main effect of self-compassion was significant, meaning that higher self-compassion was related to more perceived benefits, whereas that from self-coldness was non-significant. The main effect of perceived threat remained significant but positive, indicating more perceived benefits from higher levels of perceived threat. Only the moderation effect from self-compassion was significant (p = 0.0151). Inspecting the direction of the moderation, higher self-compassion was related to a weaker positive relationship between perceived threats and perceived benefits (Figure 2). In other words, in people with lower self-compassion, greater perceived threats instill more perceived benefits. However, in people with higher self-compassion, perceived benefits were weakly related to perceived threats. Higher self-coldness appeared to be related to weaker association between threats and benefits, but the moderation was non-significant.
Figure 2.
Moderation roles of self-compassion and self-coldness on the effects between perceived threats and perceived benefits (N = 761). Effects were unstandardized coefficients of the conditional effects of perceived threats on perceived benefits.
Discussion
Based on a bifactor model that distinguishes self-compassion from its negative counterpart—self coldness, our findings underscore the moderating roles of both constructs on how pandemic-related threats may impact well-being (26). Specifically, as hypothesized, self-compassion buffered, while self-coldness amplified, the association between perceived threats and psychological distress. We also anticipated that self-compassion would reduce, while self-coldness would intensify, the negative impacts of perceived threats on perceived benefits. However, first, the moderating role of self-coldness was not supported in our findings. Second, rather than diminishing a negative relationship between perceived threats and perceived benefits, self-compassion dampened a positive relationship between perceived threats and perceived benefits.
The findings on the buffering role of self-compassion and the amplifying role of self-coldness on the threat-psychopathology link echo with the conceptualization of the former as a protective factor in Neff and colleagues as well as the model of self-relating of Brenner et al. that views the latter as a risk factor (6, 26). Under both models, self-compassion may palliate the adverse impact of pandemic-related threats by enabling people to be kinder to oneself, evaluate the global threat as a shared experience with others and being mindful to one's needs. On the other hand, self-coldness may exacerbate psychological distress through further isolating one's pain from the fact that everyone is going through similar pains under the pandemic, forcing one to take more criticism than one's fair share in this macro catastrophe and hindering one from putting their difficulties in perspective.
In contrary to our expectation, more benefits were actually perceived in people facing more pandemic-related threats. The levels of perceived threats experienced by our participants were in general moderate. Such a level of threats would be threatening enough to trigger a response, but not too severe to have “frozen” the participants from responding or incurred resource loss so severe that adaptive coping strategies became impossible. Hence, greater threat perceptions could have triggered vigilance as well as cognitive and behavioral adaptations, which in turn enabled the discovery of benefits (41, 42). Our findings further suggest that those who scored higher on self-compassion experienced a weaker threats-benefits contingency than their counterparts who scored lower on that scale. Studies have noted people with high self-compassion were more inclined to using positive reinterpretation as a coping strategy and attuned to the positive aspects of their life even at the pre-conscious level (10, 43–45). Hence, our participants with high self-compassion were likely to have found benefits, regardless of their levels of perceived threats.
The relationship of self-coldness with perceived benefits might be less straight forward then the one with psychological distress. In the Asian culture that rewards modesty and emphasizes group harmony, being critical to oneself is not necessarily bad (46–48). Self-effacement may motivate self-improvement (49). That is, if benefit-finding is a way to improve oneself, individuals who have a tendency to self-efface may comply to win over the situation. Surely, if such efforts were ingenuine, there could be emotional costs. The line between of self-criticism due to adherence to social norms vs. self-disparagement is however often unclear (24).
Study Limitations
Due to the unprecedented nature of COVID-19 pandemic, we relied on self-constructed measures to assess the degree of perceived threats imposed onto the participants' daily lives and the extent to which benefits and gains are experienced from the disrupted livelihood. As noted by Horesh and Brown, COVID-19 may represent a new type of mass trauma characterized by its global nature, lethality, novelty, and unpredictability, as well as the enormous anticipatory anxiety it ensues (50). As the pandemic appears to continue at least for a while with lasting aftermaths to our socio-economic-political landscape, psychologists should gather efforts to conceptualize the similarities and differences of the threats and benefits experienced by people under this global catastrophe, as compared to those of the victims of other disease outbreaks and disasters. Also, as the sample was non-random, the generalizability of our findings to the general population could be compromised. Specifically, males and individuals with lower socio-economic statuses were under-represented in this survey that took about 20–30 min to complete. COVID-19 could hit particularly hard on people without a financial and social safety net to fall on, including gig workers, individuals with physical or psychological disability and their caregivers, people living in poverty, and ethnic minorities. The suspension of support services and the worsening economic outlook means immense threats to their already-challenging lives. Thus, our estimates of psychological distress and perceived threats could be underestimates.
Practical Implications
Mental health scientists are calling for studies on the causal and modifiable psychological factors that foster people's coping in the pandemic (51). Our findings point to the need to not only enhance the protective factors, such as self-compassion, but also to alleviate risk factors, such as self-coldness. Ferrari et al. conducted a meta-analysis with 27 randomized controlled trials and found that self-compassion interventions may result in a large effect size for rumination and moderate effect sizes for self-compassion, stress, depression, self-criticism, mindfulness, and anxiety, with sustained effects on self-compassion gains (52). Studies have also shown that regular but brief compassion meditation training via mobile applications and webpages can enhance well-being and self-compassion (53, 54). These interventions can be adapted to reach a larger audience during the pandemic using online channels. Based on the bifactor model of self-relating, therapists should explore means to, on one hand, facilitate a compassionate attitude to self, and on the other hand, alleviate toxic self-criticism, excessive rumination, and isolation (26).
Conclusions
The COVID-19 pandemic is a humbling experience for many of us. Instead of a relentless chase after self-enhancement and self-esteem, acknowledging one's limitations as a part of the shared human experience with compassion could be particularly salutogenic, especially in such an unprecedented, challenging time. Our findings highlight the role of self-compassion to buffer the adverse consequences of perceived threats on well-being and to facilitate a general tendency to find benefits regardless of threats. Our findings also caution mental health professionals against the detrimental effects of self-coldness, as it may amplify psychological distress from perceived threats.
Data Availability Statement
The raw data supporting the conclusion of this article will be available upon request to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Human Research Ethics Committee of University of Hong Kong. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
BL conducted the data analysis. All authors contributed significantly to the conception, data collection, and writing up of the study.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors thank Lian Pat for her support in this manuscript and the administration of the project.
Footnotes
Funding. This study was supported by an Innovative Research Grant awarded to CC.
References
- 1.Killgore WDS, Cloonan SA, Taylor EC, Dailey NS. Loneliness: a signature mental health concern in the era of COVID-19. Psychiatry Res. (2020) 290:113117. 10.1016/j.psychres.2020.113117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arafat SMY, Kar SK, Marthoenis M, Sharma P, Hoque AE, Kabir R. Psychological underpinning of panic buying during pandemic (COVID-19). Psychiatry Res. (2020) 289:113061. 10.1016/j.psychres.2020.113061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Usher K, Bhullar N, Durkin J, Gyamfi N, Jackson D. Family violence and COVID-19: increased vulnerability and reduced options for support. Int J Mental Health Nurs. (2020) 29:549–52. 10.1111/inm.12735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ng SM. Mental health of adults in Hong Kong & Mainland China. In: Paper Presented in Virtual Forum on Social Distance, Social Responses: Solutions and Strategies for Coping With COVID-19. Hong Kong: University of Hong Kong; (2020). [Google Scholar]
- 5.Census and Statistics Department Gross Domestic Product (Quarterly) (Fourth Quarter 2019). (2020). Available online at: https://www.statistics.gov.hk/pub/B10300012019QQ04B0100.pdf
- 6.Neff KD. Self-compassion: an alternative conceptualization of a healthy attitude toward oneself. Self Identity. (2003) 2:85–101. 10.1080/15298860309032 [DOI] [Google Scholar]
- 7.Zessin U, Dickhäuser O, Garbade S. The relationship between self-compassion and well-being: a meta-analysis. Appl Psychol. (2015) 7:340–64. 10.1111/aphw.12051 [DOI] [PubMed] [Google Scholar]
- 8.MacBeth A, Gumley A. Exploring compassion: a meta-analysis of the association between self-compassion and psychopathology. Clin Psychol Rev. (2012) 32:545–52. 10.1016/j.cpr.2012.06.003 [DOI] [PubMed] [Google Scholar]
- 9.Muris P, Petrocchi N. Protection or vulnerability? A meta-analysis of the relations between the positive and negative components of self-compassion and psychopathology. Clin Psychol Psychother. (2017) 24:373–83. 10.1002/cpp.2005 [DOI] [PubMed] [Google Scholar]
- 10.Allen AB, Leary MR. Self-compassion, stress, and coping. Soc Pers Psychol Compass. (2010) 4:107–18. 10.1111/j.1751-9004.2009.00246.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Finlay-Jones AL, Rees CS, Kane RT. Self-compassion, emotion regulation and stress among Australian psychologists: testing an emotion regulation model of self-compassion using structural equation modeling. PLoS ONE. (2015) 10:e0133481. 10.1371/journal.pone.0133481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Inwood E, Ferrari M. Mechanisms of change in the relationship between self-compassion, emotion regulation, and mental health: a systematic review. Appl Psychol. (2018) 10:215–35. 10.1111/aphw.12127 [DOI] [PubMed] [Google Scholar]
- 13.Terry ML, Leary MR. Self-compassion, self-regulation, and health. Self Identity. (2011) 10:352–62. 10.1080/15298868.2011.558404 [DOI] [Google Scholar]
- 14.Neff KD, Hsieh YP, Dejitterat K. Self-compassion, achievement goals, and coping with academic failure. Self Identity. (2005) 4:263–87. 10.1080/13576500444000317 [DOI] [Google Scholar]
- 15.Neely ME, Schallert DL, Mohammed SS, Roberts RM, Chen YJ. Self-kindness when facing stress: the role of self-compassion, goal regulation, and support in college students' well-being. Motiv Emot. (2009) 33:88–97. 10.1007/s11031-008-9119-8 [DOI] [Google Scholar]
- 16.Abdollahi A, Taheri A, Allen KA. Self-compassion moderates the perceived stress and self-care behaviors link in women with breast cancer. Psychooncology. (2020) 29:927–33. 10.1002/pon.5369 [DOI] [PubMed] [Google Scholar]
- 17.Stutts LA, Leary MR, Zeveney AS, Hufnagle AS. A longitudinal analysis of the relationship between self-compassion and the psychological effects of perceived stress. Self Identity. (2018) 17:609–26. 10.1080/15298868.2017.1422537 [DOI] [Google Scholar]
- 18.Beekman JB, Stock ML, Howe GW. Stomaching rejection: self-compassion and self-esteem moderate the impact of daily social rejection on restrictive eating behaviours among college women. Psychol Health. (2017) 32:1348–70. 10.1080/08870446.2017.1324972 [DOI] [PubMed] [Google Scholar]
- 19.Bluth K, Roberson PNE, Gaylord SA, Faurot KR, Grewen KM, Arzon S, et al. Does self-compassion protect adolescents from stress? J Child Fam Stud. (2016) 25:1098–109. 10.1007/s10826-015-0307-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Neff KD. Development and validation of a scale to measure self-compassion. Self Identity. (2003) 2:223–50. 10.1080/1529886039020903527409075 [DOI] [Google Scholar]
- 21.Raes F, Pommier E, Neff KD, VanGucht D. Construction and factorial validation of a short form of the Self-Compassion Scale. Clin Psychol Psychother. (2011) 18:250–5. 10.1002/cpp.702 [DOI] [PubMed] [Google Scholar]
- 22.López J, Camilli C, Noriega C. Posttraumatic growth in widowed and non-widowed older adults: religiosity and sense of coherence. J Religion Health. (2015) 54:1612–28. 10.1007/s10943-014-9876-5 [DOI] [PubMed] [Google Scholar]
- 23.Brenner RE, Heath PJ, Vogel DL, Credé M. Two is more valid than one: examining the factor structure of the Self-Compassion Scale (SCS). J Counsel Psychol. (2017) 64:696–707. 10.1037/cou0000211 [DOI] [PubMed] [Google Scholar]
- 24.Hayes JA, Lockard AJ, Janis RA, Locke BD. Construct validity of the Self-Compassion Scale-Short Form among psychotherapy clients. Counsel Psychol Q. (2016) 29:405–22. 10.1080/09515070.2016.1138397 [DOI] [Google Scholar]
- 25.Longe O, Maratos FA, Gilbert P, Evans G, Volker F, Rockliff H, et al. Having a word with yourself: neural correlates of self-criticism and self-reassurance. Neuroimage. (2010) 49:1849–56. 10.1016/j.neuroimage.2009.09.019 [DOI] [PubMed] [Google Scholar]
- 26.Brenner RE, Vogel DL, Lannin DG, Engel KE, Seidman AJ, Heath PJ. Do self-compassion and self-coldness distinctly relate to distress and well-being? A theoretical model of self-relating. J Counsel Psychol. (2018) 65:346–57. 10.1037/cou0000257 [DOI] [PubMed] [Google Scholar]
- 27.Gilbert P. Human Nature and Suffering. Hove: Lawrence Erlbaum Associates; (1989). [Google Scholar]
- 28.Gilbert P. Social mentalities: internal ‘social’ conflicts and the role of inner warmth and compassion in cognitive therapy. In: Gilbert P, Bailey KG. editor. Genes on the Couch: Explorations in Evolutionary Psychotherapy. Hove: Psychology Press; (2000). p. 118–50. [Google Scholar]
- 29.Lau HPB, Cheng C. Coping with the Yin/Yang of stress: the link between dialectical thinking and coping. In: Spender-Rodgers J, Peng K. editors. The Cultural and Psychological Foundations of East Asian Cognition: Contradiction, Change, and Holism. New York, NY: Oxford University Press; (2018). p. 573–94. [Google Scholar]
- 30.Cheng C. Dialectical thinking and coping flexibility: a multimethod approach. J Pers. (2009) 77:471–94. 10.1111/j.1467-6494.2008.00555.x [DOI] [PubMed] [Google Scholar]
- 31.Yik M. How unique is Chinese emotion. In: Bond MH, editor. The Oxford Handbook of Chinese Psychology. Oxford University Press; (2010). p. 205–20. 10.1093/oxfordhb/9780199541850.013.0015 [DOI] [Google Scholar]
- 32.McMillen JC, Fisher RH, Smith EM. Perceived benefit and mental health after three types of disaster. J Consult Clin Psychol. (1997) 65:733–9. 10.1037/0022-006X.65.5.733 [DOI] [PubMed] [Google Scholar]
- 33.Cheng C, Wong WM, Tsang KW. Perception of benefits and costs during SARS outbreak: an 18-month prospective study. J Consult Clin Psychol. (2006) 74:870–9. 10.1037/0022-006X.74.5.870 [DOI] [PubMed] [Google Scholar]
- 34.Lau BHP, Chan Cecilia LW, Ng SM. Resilience of Hong Kong people in the COVID-19 pandemic: lessons learned from a survey at the peak of the pandemic in Spring 2020. Asia Pac J Soc Work Dev. (2020) 1–10. 10.1080/02185385.2020.1778516. [Epub ahead of print]. [DOI] [Google Scholar]
- 35.Chen J, Yan L, Zhou L. Reliability and validity of Chinese version of Self-compassion Scale. Chinese J Clin Psychol. (2011) 19:734–6. [Google Scholar]
- 36.Kroenke K, Spitzer RL, Williams JBW, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. (2009) 50:613–21. 10.1176/appi.psy.50.6.613 [DOI] [PubMed] [Google Scholar]
- 37.Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder the GAD-7. Archiv Intern Med. (2006) 166:1092–7. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 38.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. (2003) 41:1284–92. 10.1097/01.MLR.0000093487.78664.3C [DOI] [PubMed] [Google Scholar]
- 39.Yu X, Stewart SM, Wong PT, Lam TH. Screening for depression with the Patient Health Questionnaire-2 (PHQ-2) among the general population in Hong Kong. J Affect Disord. (2011) 134:444–7. 10.1016/j.jad.2011.05.007 [DOI] [PubMed] [Google Scholar]
- 40.Zeng QZ, He YL, Liu H, Miao JM, Chen JX, Xu HN, et al. Reliability and validity of Chinese version of the generalized anxiety disorder 7-item (GAD-7) scale in screening anxiety disorders in outpatients from traditional Chinese internal department. Chinese Mental Health J. (2013) 27:163–8. [Google Scholar]
- 41.Lazarus RS, Folkman S. Stress, Appraisal, and Coping. New York, NY: Springer; (1984). [Google Scholar]
- 42.Helgeson VS, Reynolds KA, Tomich PL. A meta-analytic review of benefit finding and growth. J Consult Clin Psychol. (2006) 74:797–816. 10.1037/0022-006X.74.5.797 [DOI] [PubMed] [Google Scholar]
- 43.Wong CCY, Yeung NCY. Self-compassion and posttraumatic growth: cognitive processes as mediators. Mindfulness. (2017) 8:1078–87. 10.1007/s12671-017-0683-4 [DOI] [Google Scholar]
- 44.Ewert C, Gaube B, Geisler FCM. Dispositional self-compassion impacts immediate and delayed reactions to social evaluation. Pers Indiv Differ. (2018) 125:91–6. 10.1016/j.paid.2017.12.037 [DOI] [Google Scholar]
- 45.Phillips WJ, Hine DW, Marks ADG. Self-compassion moderates the predictive effects of implicit cognitions on subjective well-being. Stress Health. (2018) 34:143–51. 10.1002/smi.2773 [DOI] [PubMed] [Google Scholar]
- 46.Yang SY, Sternberg RJ. Taiwanese Chinese people's conceptions of intelligence. Intelligence (Norwood). (1997) 25:21–36. 10.1016/S0160-2896(97)90005-2 [DOI] [Google Scholar]
- 47.Takata T. Self-enhancement and self-criticism in Japanese culture. J Cross Cult Psychol. (2003) 34:542–51. 10.1177/0022022103256477 [DOI] [Google Scholar]
- 48.Kitayama S, Markus HR, Matsumoto H, Norasakkunkit V. Individual and collective processes in the construction of the self: self-enhancement in the United States and self-criticism in Japan. J Pers Soc Psychol. (1997) 72:1245–67. 10.1037/0022-3514.72.6.1245 [DOI] [PubMed] [Google Scholar]
- 49.Hamamura T, Heine SJ. Approach and avoidance motivation across cultures. In: Elliot AJ. editor. Handbook of Approach and Avoidance Motivation. Psychology Press; (2008). p. 557–70. [Google Scholar]
- 50.Horesh D, Brown AD. Traumatic stress in the age of COVID-19: a call to close critical gaps and adapt to new realities. Psychol Trauma. (2020) 12:331–5. 10.1037/tra0000592 [DOI] [PubMed] [Google Scholar]
- 51.Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. (2020) 7:547–60. 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ferrari M, Hunt C, Harrysunker A, Abbott MJ, Beath AP, Einstein DA. Self-compassion interventions and psychosocial outcomes: a meta-analysis of RCTs. Mindfulness. (2019) 10:1455–73. 10.1007/s12671-019-01134-6 [DOI] [Google Scholar]
- 53.Eriksson T, Germundsjö L, Åström E, Rönnlund M. Mindful self-compassion training reduces stress and burnout symptoms among practicing psychologists: a randomized controlled trial of a brief web-based intervention. Front Psychol. (2018) 9:2340–9. 10.3389/fpsyg.2018.02340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Donovan E, Rodgers RF, Cousineau TM, McGowan KM, Luk S, Yates K, et al. Brief report: feasibility of a mindfulness and self-compassion based mobile intervention for adolescents. J Adolesc. (2016) 53:217–21. 10.1016/j.adolescence.2016.09.009 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusion of this article will be available upon request to the corresponding author.