Abstract
To design a new breast vacuum bag to reduce global and local setup errors in post-mastectomy radiation therapy (PMRT). A total of 24 PMRT patients were immobilized with an old vacuum bag and 26 PMRT patients were immobilized with a new vacuum bag. The registration results were analysed using four regions of interest (ROI): the global ROI [including the whole region of the planning target volume (PTV), GROI], the supraclavicular area (SROI), the ipsilateral chest wall region (CROI) and the ipsilateral arm region (AROI). The global and local setup errors of the two groups were compared. The global setup errors of the new vacuum group were significantly smaller than those in the old vacuum group with the exception of yaw axes (P < 0.05). The systematic error (Σ) and random error (σ) ranged from 1.21 to 2.13 mm. In the new vacuum group, the local setup errors in the medial-lateral (ML) direction and roll axes for CROI (the Σ and σ ranged from 0.65 to 1.35 mm), and the local setup errors in ML and superior-inferior (SI) directions for SROI were significantly smaller than those in the old vacuum group. The total required PTV margins for the chest wall in ML, SI, and anterior-posterior (AP) were 4.40, 3.12 and 3.77 mm respectively. The new vacuum bag can significantly reduce the global setup errors and local setup errors in PMRT. The respiratory motion of the chest wall was negligible, and the 5 mm PTV margin could cover the local setup errors in PMRT using the new vacuum bag with cone beam CT (CBCT) correction.
Keywords: breast vacuum bag, global and local setup errors, post-mastectomy radiation therapy
INTRODUCTION
Post-mastectomy radiation therapy (PMRT) can significantly reduce the local recurrence of breast cancer and improve the overall survival rate of patients. To further improve the uniformity and accuracy of the target dose and reduce the dose to organs at risk (OAR), intensity modulation radiation therapy (IMRT), field in field (FIF) and other technologies are widely used [1]. However, the target area of PMRT is large, and there is a large setup error [2], which causes uncertainty regarding the target dose. Currently, reported breast immobilization methods include breast cradles, Alpha Cradle (foam), vacuum bag and arm support. There are a large number of setup errors associated with each of these different immobilisation methods, with system errors ranging from 0.7 to 5.7 mm, and random errors ranging from1.0 to 4.1 mm [2, 3].
What we have found in clinical practice is that the size of the vacuum bag is relatively small, making it difficult to fix it well to the body and arm. Therefore, we hypothesised that changing the size and shape of the vacuum bag and strengthening the support of the body and arm can improve the fixation effect. At present, all reports about the setup errors have analysed the global setup errors [the errors of the whole region of planning target volume (PTV)], and do not involve the local setup errors (the difference errors between the whole region and sub-region of interest) [2, 4]. However, in our previous study, we found that there were large global setup errors and local setup errors in the use of vacuum bags [5]. Therefore, evaluation of the effect of the immobilization device should include the global setup errors and the local setup errors. Secondly, the patient’s breathing motion can cause chest wall motion. Computed tomography (CT) simulation positioning is only a snapshot image and does not include the patient’s breathing motion information. Therefore, the residual local setup errors and respiratory motion movement are the main factors when setting the PTV margin in PMRT treatment using imaged-guided radiation therapy (IGRT).
The purpose of this study was to design a new breast vacuum bag to strengthen the support of the arm, and to compare the global and local setup errors with the traditional vacuum bag. The study also aimed to quantify the respiratory motion amplitude of the chest wall, to analyse the correlation between the motion amplitude of the chest wall and the amplitude of the diaphragm and to determine the corresponding PTV margin based on the local setup errors and the motion amplitude of the chest wall.
MATERIALS AND METHODS
Patients
From March 2019 to December 2019, a total of 50 patients with PMRT were included in this study, and they were randomly divided into two groups. The old vacuum group was immobilised with an old vacuum bag (CIVCO Radiotherapy, Orange City, IA, USA) (24 patients), while the new vacuum group was immobilized with a new vacuum bag (Klarity Medical, Shenzhen, China) (26 patients). Each patient signed an informed consent form before treatment, and this study was approved by the Ethics Committee on Biomedical Research, West China Hospital of Sichuan University (No.2020180). There were 26 patients with breast cancer on the left and 24 patients with breast cancer on the right, with a median age of 48 years.
Immobilization
Based on the recommendations of the multidisciplinary team (including the radiation oncologists, the physicists and the radiotherapists), we designed and determined the shape and size of the new vacuum bag, which is 130 cm long and 100 cm wide. Then the manufacturer produced it (Klarity Medical, Shenzhen, China) (Fig. 1 A and C). Meanwhile, we measured the dimensions of the old vacuum bag (Fig. 1 B and D), which is 100 cm long and 70 cm wide (inner size 90 × 55 cm). The two types of vacuum bags were placed on a 15° wedge plate, and the upper side of the bag was formed to fit the shape of the patient’s head and to limit the longitudinal movement of the head. The abduction of the upper limb on the involved side was greater than 90°. Pressing on both sides of the upper part of the vacuum bag forms an arm shape to prevent the movement of the arm from causing deformation and motion of the adjacent chest wall. In the new vacuum bag group, the arms were fixed for more than half the length of the arm, and more than one-third of lower limbs were fixed on the lower side. In the old vacuum bag group, only one-third of the arms were fixed, and the buttocks were fixed on the lower side.
Fig. 1.
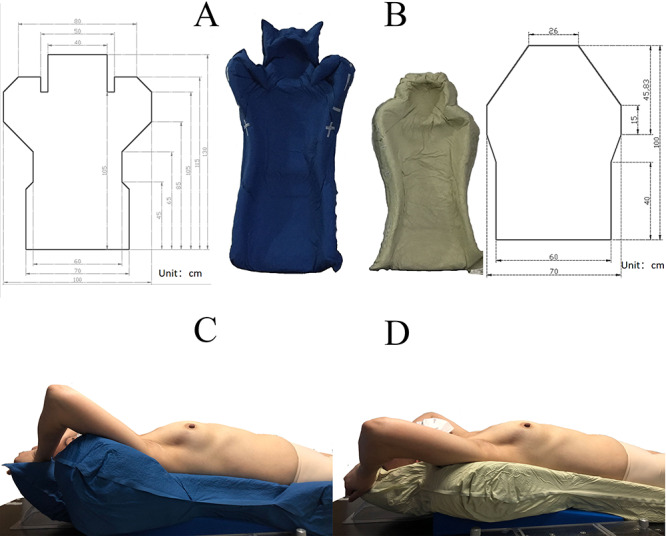
The shape and size of the new vacuum bag (A) and the old vacuum bag (B). The same patient immobilised with the new vacuum bag (C) and the old vacuum bag (D).
Simulation and planning
Free-breathing patients were simulated using Siemens 64-slice CT with a 3-mm slice thickness from the chin to the lower edge of the liver with intravascular contrast. The treatment plan was generated using the RayStation 4.7 (RaySearch, Stockholm, Sweden) treatment-planning system.
Setup errors analysis
The global and the local setup errors were analyzed using cone beam CT (CBCT) registration to the planning CT. A total of 945 CBCT images were obtained by XVI Release 5.0.3 for 40 patients (Synergy, Elekta, Crawley, UK). The number of frames per CBCT acquisition was ~400. The scanning parameters were tube voltage of 100 kV, tube current of 36.1 mA, S20 F1 filter plate, acquisition speed of 5.5 frames/s and acquisition angle of 50–210°.
The whole region of PTV was defined as a single region of interest (GROI) in planning CT to registration with CBCT image online. The other three sub-regions of interest were defined and analysed offline [including the supraclavicular area (SROI), the ipsilateral chest wall region (CROI) and the ipsilateral arm region (AROI)]. The registration results between CBCT and the planning CT using the GROI were defined as the global setup errors. The difference between the registration results of GROI and the registration results of the other three sub-regions was defined as the local setup errors. The automatic registration gray value (translation errors and rotation errors, T+R) was used to obtain the coarse registration first, and then manual fine adjusting followed. The systematic errors (Σ) and random errors (σ) were computed along the medial–lateral (ML), superior–inferior (SI) and anterior–posterior (AP) axes, and the rotation errors along the pitch, roll and yaw axes were also recorded. A radiotherapist with 10 years of experience performed all the image registration. Two experience radiation oncologist audited the registration results for 40 CBCT images. The clinical target volume (CTV) CBCT PTV margin recipe by Van Herk [6]: 2.5 Σ + 0.7σ, was used, in which Σ is the standard deviation (SD) of the individual means for each ROI registration result per patient, and σ is the root mean square of the individual SD for each ROI registration result per patient.
Evaluation of motion amplitude of the chest wall and diaphragm
Six opaque lead markers with a diameter of 1 mm were put on the chest wall, arranged from the second rib to the sixth rib (Fig. 2). The motion amplitude of the chest wall and diaphragm were quantified by fluoroscopy (XVI motion view function) in the AP and ML directions. The correlation between the amplitude of the chest wall and diaphragm was analysed. The 95th percentile motion amplitude (A) of the chest wall was evaluated, then 0.45A [6] was added linearly to the CTV–PTV margin of the chest wall when the motion amplitude of respiration exceeded 1 cm.
Fig. 2.
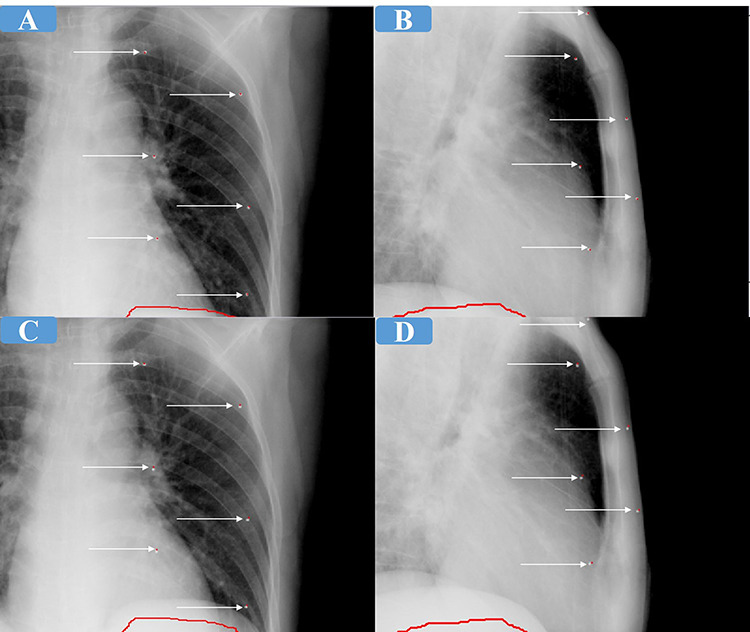
The motion of the chest wall and the diaphragm for the same patient. (A, B) The position of the six markers and the diaphragm at the end of inspiration. (C, D) The position of the six markers and the diaphragm at the end of expiration. Each white arrow indicates an opaque lead marker. The red line represents the position of the diaphragm at the end of inspiration.
Statistical analysis
SPSS 22.0 (IBM, Chicago, IL, USA) was used for all statistical analyses, with a significance level of P < 0.05. Differences were assessed for significance using the t-test (ANOVA). Pearson’s correlation coefficient was used to analyse the correlation between the amplitude of the chest wall and diaphragm.
RESULTS
Comparison of means between the two groups
The comparison of the global setup errors and local setup errors is shown in Table 1. In the global setup errors, except that there was no statistical difference in the yaw axis, the errors of the new vacuum group in other directions were significantly smaller than that of the old vacuum group (P < 0.05). In the new vacuum group, the local errors in ML and yaw directions for chest wall (P < 0.05) and the local setup errors in the ML and SI directions for the supraclavicular were statistically different than those in the old vacuum group (P < 0.05). In terms of the local setup errors of the arm, except that there was no statistical difference in the pitch axis, the errors of the new vacuum group in other directions were significantly smaller than those in the old vacuum group (P < 0.05).
Table 1.
Comparison of means of the global and the local setup errors between the old vacuum group and the new vacuum group (mm). GN, the new vacuum group. GO, the old vacuum group. GROI represent the global setup errors. GROI-CROI, GROI-SROI, and GROI-AROI represent the local setup errors for the supraclavicular area (SROI), the ipsilateral chest wall region (CROI) and the ipsilateral arm region (AROI), respectively
| GROI | GROI-CROI | GROI-SROI | GROI-AROI | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Directions | ML | SI | AP | ML | SI | AP | ML | SI | AP | ML | SI | AP | ||||||||||||
| Group | GN | GO | GN | GO | GN | GO | GN | GO | GN | GO | GN | GO | GN | GO | GN | GO | GN | GO | GN | GO | GN | GO | GN | GO |
| n | 500 | 446 | 500 | 446 | 500 | 446 | 500 | 446 | 500 | 446 | 500 | 446 | 500 | 446 | 500 | 446 | 500 | 446 | 500 | 446 | 500 | 446 | 500 | 446 |
| Mean | −0.02 | 0.07 | −0.02 | −0.14 | −0.03 | −0.33 | 0.02 | −0.01 | 0.1 | 0.1 | −0.09 | −0.08 | 0.03 | 0.06 | −0.15 | −0.1 | 0.02 | 0.02 | −0.05 | 0.17 | −0.13 | −0.25 | −0.03 | −0.29 |
| SD | 0.24 | 0.39 | 0.23 | 0.51 | 0.22 | 0.48 | 0.15 | 0.16 | 0.1 | 0.14 | 0.13 | 0.18 | 0.14 | 0.23 | 0.14 | 0.28 | 0.14 | 0.21 | 0.49 | 0.71 | 0.51 | 0.97 | 0.58 | 1.03 |
| P value | 0.00 | 0.00 | 0.00 | 0.00 | 0.78 | 0.38 | 0.01 | 0.00 | 0.93 | 0.00 | 0.02 | 0.00 | ||||||||||||
| Directions | Pitch | Roll | Yaw | Pitch | Roll | Yaw | Pitch | Roll | Yaw | Pitch | Roll | Yaw | ||||||||||||
| Group | GN | GO | GN | GO | GN | GO | GN | GO | GN | GO | GN | GO | GN | GO | GN | GO | GN | GO | GN | GO | GN | GO | GN | GO |
| n | 500 | 446 | 500 | 446 | 500 | 446 | 500 | 446 | 500 | 446 | 500 | 446 | 500 | 446 | 500 | 446 | 500 | 446 | 500 | 446 | 500 | 446 | 500 | 446 |
| Mean | −0.09 | 0.47 | 0.62 | −0.1 | −0.07 | −0.1 | 0.22 | 0.28 | 0.11 | 0.02 | 0.09 | −0.06 | −0.44 | −0.34 | 0.12 | 0.25 | −0.19 | −0.39 | −0.58 | −0.16 | 0.3 | −0.6 | 0.39 | −1.26 |
| SD | 1.05 | 1.55 | 1.01 | 1.63 | 0.84 | 1.38 | 0.9 | 1.08 | 1.25 | 1.04 | 0.8 | 0.92 | 1.18 | 2.06 | 1.18 | 1.78 | 1.26 | 1.91 | 3.13 | 5.35 | 3.09 | 8.41 | 3.08 | 5.41 |
| P value | 0.00 | 0.00 | 0.73 | 0.33 | 0.24 | 0.01 | 0.39 | 0.17 | 0.05 | 0.13 | 0.03 | 0.00 | ||||||||||||
The bold P value indicates that this group of comparison is statistically significant.
Global setup errors and the local setup errors between the two groups
The global setup errors and the local setup errors for the new vacuum group and the old vacuum group are shown in Table 2 (translational results) and Table 3 (rotational results). The global setup errors of the old vacuum group ranged from 2.35 to 3.92 mm, and the corresponding PTV margins range from 9.79 to 12.18 mm. The global setup errors of the new vacuum group ranged from 1.21 to 2.13 mm, and the corresponding PTV margins ranged from 4.33 to 4.55 mm.
Table 2.
The global setup errors and the local set-up errors of translational directions in the old vacuum group and the new vacuum group (mm). GROI represents the global setup errors; GROI-CROI, GROI-SROI and GROI-AROI represent the local setup errors for the supraclavicular area (SROI), the ipsilateral chest wall region (CROI) and the ipsilateral arm region (AROI), respectively
| Directions | The old vacuum group | The new vacuum group | |||||
|---|---|---|---|---|---|---|---|
| Σ | σ | Margin | Σ | σ | Margin | ||
| GROI | ML | 3.26 | 2.35 | 9.79 | 1.22 | 2.13 | 4.55 |
| SI | 3.92 | 3.41 | 12.18 | 1.26 | 1.95 | 4.52 | |
| AP | 3.79 | 3.32 | 11.79 | 1.21 | 1.85 | 4.33 | |
| GROI-CROI | ML | 1.02 | 1.22 | 3.41 | 1.35 | 0.83 | 3.95 |
| SI | 0.90 | 1.20 | 3.08 | 0.65 | 0.85 | 2.22 | |
| AP | 1.19 | 1.44 | 3.98 | 0.88 | 0.97 | 2.87 | |
| GROI-SROI | ML | 1.67 | 1.70 | 5.36 | 1.02 | 0.97 | 3.24 |
| SI | 2.37 | 1.83 | 7.20 | 1.00 | 1.04 | 3.24 | |
| AP | 1.31 | 1.68 | 4.46 | 1.21 | 0.82 | 3.60 | |
| GROI-AROI | ML | 5.63 | 4.24 | 17.04 | 3.90 | 3.11 | 11.91 |
| SI | 8.37 | 4.85 | 24.31 | 4.29 | 3.04 | 12.86 | |
| AP | 8.94 | 5.13 | 25.95 | 5.33 | 2.76 | 15.25 | |
Table 3.
The global set-up errors and the local set-up errors in rotational axis for the old vacuum group and the new vacuum group (°)
| Directions | The old vacuum group | The new vacuum group | |||
|---|---|---|---|---|---|
| Σ | σ | Σ | σ | ||
| GROI-CROI | Pitch | 0.79 | 0.77 | 0.65 | 0.65 |
| Roll | 0.67 | 0.85 | 0.97 | 0.83 | |
| Yaw | 0.68 | 0.62 | 0.61 | 0.54 | |
| GROI-SROI | Pitch | 1.44 | 1.58 | 1.04 | 0.64 |
| Roll | 1.28 | 1.39 | 0.99 | 0.68 | |
| Yaw | 1.55 | 1.14 | 0.94 | 0.87 | |
| GROI-AROI | Pitch | 4.51 | 3.05 | 2.66 | 1.78 |
| Roll | 7.52 | 3.75 | 2.63 | 1.78 | |
| Yaw | 4.4 | 3.12 | 2.55 | 1.82 | |
The local setup errors of the chest wall in the old vacuum group ranged from 0.9 to 1.44 mm, and the corresponding PTV margin ranged from 3.08 to 3.98 mm. In the new vacuum group, the local setup errors of the chest wall ranged from 0.65 to 1.35 mm, and the corresponding PTV margins ranged from 2.22 to 3.95 mm. In the old vacuum group, the local setup errors of the supraclavicular area were larger than those of the chest wall, especially in the SI direction. The local setup errors of the arm were considerable in the old vacuum group, ranging from 4.24 to 8.94 mm. These errors dropped dramatically in the new vacuum group, ranging from 2.76 to 5.33 mm. The local setup errors of SROI and AROI for rotational axis in the new vacuum group were smaller than those in the old vacuum group.
Motion amplitude of the chest wall and diaphragm
The motion amplitude of the chest wall and diaphragm were evaluated randomly for 34 patients (20 patients in the new vacuum group and 14 patients in the old vacuum group) (Table 4). Eleven patients received respiration motion evaluation once and 23 patients received respiration motion evaluation twice according to patients’ agreements. A total of 57 measurements in the ML and AP directions were obtained. Since the SI direction can be measured in both the AP and ML directions, there were 114 measurements in the SI direction. The motion of markers located in different ribs in the same direction was similar. The motion (mean ± SD) of all markers was 0.50 ± 0.50 mm in the ML direction, 0.84 ± 0.54 mm in the SI direction and 0.89 ± 0.58 mm in the AP direction. The motion amplitude of the diaphragm in the SI direction was 15.7 ± 3.60 mm, which was not statistically related to any direction of the markers on the chest wall. Meanwhile, there was no statistical difference in the chest wall motion between the new vacuum group and the old vacuum group. The motion amplitude of the 95th percentile in the ML, SI and AP directions was 1.0, 2.0 and 2.0 mm, respectively. If added linearly to the calculated chest wall PTV with 0.45A [6], the total required PTV margins for chest wall were 4.40 mm, 3.12 mm, and 3.77 mm for the ML, SI and AP directions respectively.
Table 4.
The motion amplitude of the chest wall (six markers) and PTV margins (mm)
| ML | SI | AP | ||||
|---|---|---|---|---|---|---|
| Average | SD | Average | SD | Average | SD | |
| Mark 1 | 0.54 | 0.50 | 1.05 | 0.23 | 0.93 | 0.57 |
| Mark 2 | 0.59 | 0.50 | 0.98 | 0.51 | 1.13 | 0.69 |
| Mark 3 | 0.39 | 0.49 | 0.99 | 0.46 | 1.09 | 0.66 |
| Mark 4 | 0.54 | 0.50 | 1.01 | 0.60 | 1.00 | 0.79 |
| Mark 5 | 0.47 | 0.50 | 0.99 | 0.51 | 1.00 | 0.71 |
| Mark 6 | 0.43 | 0.50 | 1.13 | 0.46 | 1.13 | 0.62 |
| Total | 0.50 | 0.50 | 0.84 | 0.54 | 0.89 | 0.58 |
| Diaphragm | / | / | 15.70 | 3.60 | / | / |
| 95th Percentile | 1.00 | 2.00 | 2.00 | |||
| 0.45Aa | 0.45 | 0.90 | 0.90 | |||
| CROI margin | 3.95 | 2.22 | 2.87 | |||
| Total margin | 4.40 | 3.12 | 3.77 | |||
aWe used 0.45A linearly added to the calculated PTV margin according to the 95th percentile of amplitude (see [6]).
DISCUSSION
In this study, the global setup errors (systematic errors and random errors) of the old vacuum group were 3.26/2.35 mm in the ML direction, 3.92/3.41 mm in the SI direction and 3.79/3.32 in the AP direction. We summarised these errors reported by different authors [3, 7–11] in Table 5. These results are similar to the results of the old vacuum group in this study, indicating that there are large global setup errors in breast cancer radiation therapy, and we need to improve the current immobilisation device.
Table 5.
The systematic and random errors of PMRT reported by different authors (mm)
| Author | Immobilization | ROI | Systematic errors | Random errors | ||||
|---|---|---|---|---|---|---|---|---|
| ML | SI | AP | ML | SI | AP | |||
| Topolnjak et al. [3] | Double-arm support | Chest wall | 3.10 | 3.80 | 2.50 | 2.20 | 2.80 | 2.60 |
| Batumalai et al. [7] | Vacuum bag | Chest wall | 3.41 | 3.49 | 2.24 | 2.98 | 2.82 | 2.74 |
| Veldeman et al. [8] | Arm support | Surgical clips | -1.49 | 1.44 | 2.80 | 7.34 | 2.31 | 3.21 |
| Offerman et al. [9] | Vacuum bag | Breast and the seroma cavity | 3.22 | 3.83 | 5.72 | 2.00 | 1.50 | 2.60 |
| Topolnjak et al. [10] | Supine | Excision cavity and clips | 3.40 | 2.70 | 3.40 | 2.50 | 2.30 | 2.40 |
| Jain et al. [11] | Breast board | Skin contour and bony anatomy | 5.70 | 2.80 | 2.30 | 3.90 | 3.50 | 3.20 |
To simplify comparison with other studies, the local setup errors of the chest wall were used. The local setup errors in the old vacuum group in ML, SI and AP were 3.43/2.40 mm, 4.33/3.66 mm and 4.35/3.51 mm, respectively, which were slightly larger than the results reported in the above studies. However, the local setup errors in ML, SI and AP of the new vacuum group were 2.31/2.22 mm, 1.52/2.19 mm and 1.42/2.10 mm, respectively, which were smaller than the results reported in those studies. At the same time, the global setup errors in ML, SI and AP of the new vacuum group in this study were 1.22/2.13 mm, 1.26/1.95 mm and 1.21/1.85 mm, respectively. The global setup errors of the new vacuum group were significantly lower than those of the old vacuum group except for the yaw axis (P < 0.05). The local setup errors of the chest wall in the new vacuum group and the old vacuum group were significantly different in the ML direction and roll axis (P < 0.05). Meanwhile, the local setup errors of the supraclavicular area between the new vacuum group and the old vacuum group were significantly different in the ML and SI directions (P < 0.05). The local setup errors of the arm in the new vacuum group were significantly smaller than those in the old vacuum group except for the pitch axis. However, the local setup errors of the arm in the new vacuum group were still large. Fortunately, the PTV does not include the arm area.
Based on these findings, we believe that the new breast vacuum bag can significantly reduce the global setup errors and the local setup errors of PMRT and is worthy of popularisation and application in clinical practice. We consider that the new vacuum bag is mainly widened and lengthened, which strengthens the fixation of the patient’s arm, head and chest wall. Unfortunately, to our knowledge, apart from our own research on PMRT local setup errors, no other institution has done similar research and cannot directly compare these errors.
When using IGRT, the residual errors after table correction and the intra-fraction errors (such as the respiratory motion) should be considered. The residual errors include the mechanical errors of the imaging system and the correction system, and the local setup errors. For example, Feng et al. [12] used kilovolt (KV) image to register the chest wall and correct it. If it was registered with a titanium clip, the PTV margins 5.9 mm (AP), 3.9 mm (LR) and 7.9 mm (SI) were still needed. All patients in this study underwent a mastectomy, and the PTV included the chest wall and the corresponding lymphatic drainage area. Local setup errors after registration with a large ROI (GROI) were found in our study, which is an important part of the residual errors. At the same time, the chest wall is affected by respiratory movement which should be considered in terms of intra-fraction errors. Lee et al. used the Alpha Cradle and found that the inter-fraction errors under free-breathing ranged from 1.8 to 3.3 mm [13]. Thomsen et al. [14] used continuous MV imaging to find that the chest wall movement of free-breathing during breast cancer radiation therapy ranged from 1.1 mm to 3.3 mm. Feng et al. [12] found that the chest wall had small breathing movements, so they used CT scan positioning under free breathing. Harris et al. [15] reported that the average movement of titanium clips during treatment was 0.4 mm. The results of Yue et al. [16] showed that the chest wall breathing movement was only 1 mm. These results are similar to the results of this study. At the same time, this study found that there was no difference in the motion of the chest wall from the second rib to the sixth rib in the same direction, and there was no correlation between the motion of the chest wall and the diaphragm. The 95th percentile motion amplitude of chest wall in ML, SI and AP directions was 1.0, 2.0 and 2.0 mm respectively. If added linearly to the calculated chest wall PTV with 0.45A [6], the total required PTV margins for chest wall were below 5 mm. However, van Herk suggests treating respiration with a peak-peak amplitude of <1 cm the same as random errors [6]. So, we believe that when using the new breast vacuum bag, a 5 mm PTV margin can ensure the target dose, considering the local setup errors and respiration motion for PMRT with CBCT online correction.
This study mainly analysed the effects of a new vacuum bag and traditional vacuum bag for global setup errors, local setup errors and chest wall respiratory motion. However, there are some limitations of our study. First, there were differences between individual patients for these two groups because there were no data using both vacuum bags in the same patient. Furthermore, both the global setup errors and the local setup errors can be affected by different radiotherapist groups in immobilization, CT simulation and treatment. To ensure the accuracy of radiation therapy and reduce the patient’s additional radiation dose, optical surface imaging (OSI) systems [17, 18] play an increasingly important role in breast radiation therapy. Furthermore, to reduce the radiation dose to the lung and the heart, changing the patient’s position [13, 19, 20] and using deep inspiration breath-hold (DIBH) [21, 22] technology were studied. Based on these studies, we will combine OSI and DIBH technology with the new vacuum bag in a further study.
CONCLUSION
The new vacuum bag can significantly reduce the global setup errors and local setup errors in PMRT. The respiratory motion of the chest wall is negligible. The 5 mm PTV margin could cover the local setup errors of the sub-regions in PMRT using the new vacuum bag with CBCT online correction.
AUTHOR CONTRIBUTIONS
Konglong Shen collected data and drafted the manuscript. Zhiguo Wang, Jie Xiong, An Li, Weifeng Wang, Wan Li, Jidan Zhou, Zhonghua Deng, and Bin Li helped to collect the data. Renming Zhong designed the study, and revised and approved the final manuscript. All authors read and confirmed the manuscript.
CONFLICT OF INTEREST
The authors declare that they have no competing interests.
FUNDING
This work was supported by the Science and Technology Support Program of Sichuan province, China (Grant number.2016FZ0086).
Contributor Information
Konglong Shen, Department of Radiotherapy, Division of Radiation Physics, State Key Laboratory of Biotherapy and Cancer Center, West China Hospital, Sichuan University, Chengdu 610041, P.R. China.
Jie Xiong, Radiology Department, West China Hospital, Sichuan University, Chengdu 610041, P.R. China.
Zhiguo Wang, Department of Radiotherapy, Division of Radiation Physics, State Key Laboratory of Biotherapy and Cancer Center, West China Hospital, Sichuan University, Chengdu 610041, P.R. China.
Weifeng Wang, Jingzhou Central Hospital, the Second Clinical Medical College, Yangtze University, Jinzhou 121001, P.R. China.
Wan Li, Department of Radiotherapy, Division of Radiation Physics, State Key Laboratory of Biotherapy and Cancer Center, West China Hospital, Sichuan University, Chengdu 610041, P.R. China.
Jidan Zhou, Department of Radiotherapy, Division of Radiation Physics, State Key Laboratory of Biotherapy and Cancer Center, West China Hospital, Sichuan University, Chengdu 610041, P.R. China.
Zhonghua Deng, Department of Radiotherapy, Division of Radiation Physics, State Key Laboratory of Biotherapy and Cancer Center, West China Hospital, Sichuan University, Chengdu 610041, P.R. China.
Bin Li, Department of Radiotherapy, Division of Radiation Physics, State Key Laboratory of Biotherapy and Cancer Center, West China Hospital, Sichuan University, Chengdu 610041, P.R. China.
Renming Zhong, Department of Radiotherapy, Division of Radiation Physics, State Key Laboratory of Biotherapy and Cancer Center, West China Hospital, Sichuan University, Chengdu 610041, P.R. China.
References
- 1. Jin GH, Chen LX, Deng XW et al. A comparative dosimetric study for treating left-sided breast cancer for small breast size using five different radiotherapy techniques: Conventional tangential field, filed-in-filed, tangential-IMRT, multi-beam IMRT and VMAT. Radiat Oncol 2013;8:89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Batumalai V, Holloway L, Delaney GP. A review of setup error in supine breast radiotherapy using cone -beam computed tomography. Med Dosim 2016;41:225–9. [DOI] [PubMed] [Google Scholar]
- 3. Topolnjak R, Sonke JJ, Nijkamp J et al. Breast patient setup error assessment: Comparison of electronic portal image devices and cone-beam computed tomography matching results. Int J Radiat Oncol Biol Phys 2010;78:1235–43. [DOI] [PubMed] [Google Scholar]
- 4. Zhong R, Song Y, Yan Y et al. Analysis of which local set-up errors can be covered by a 5-mm margin for cone beam CT-guided radiotherapy for nasopharyngeal carcinoma. Br J Radiol 2018;91: 20160849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zhou J, Li S, Ye C et al. Analysis of local setup errors of sub-regions in cone-beam CT-guided post-mastectomy radiation therapy. J Radiat Res 2020;61:457–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. van Herk M. Errors and margins in radiotherapy. Semin Radiat Oncol 2004;14:52–64. [DOI] [PubMed] [Google Scholar]
- 7. Batumalai V, Phan P, Choong C et al. Comparison of setup accuracy of three different image assessment methods for tangential breast radiotherapy. Journal of Medical Radiation Sciences 2016;63:224–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Veldeman L, De Gersem W, Speleers B et al. Alternated prone and supine whole-breast irradiation using IMRT: Setup precision, respiratory movement and treatment time. Int J Radiat Oncol Biol Phys 2012;82:2055–64. [DOI] [PubMed] [Google Scholar]
- 9. Offerman S, Lamba M, Lavigne R. Effect of breast volume on treatment reproducibility on a tomotherapy unit in the treatment of breast cancer. Int J Radiat Oncol Biol Phys 2011;80:417–21. [DOI] [PubMed] [Google Scholar]
- 10. Topolnjak R, de Ruiter P, Remeijer P et al. Image-guided radiotherapy for breast cancer patients: Surgical clips as surrogate for breast excision cavity. Int J Radiat Oncol Biol Phys 2011;81:e187–e95. [DOI] [PubMed] [Google Scholar]
- 11. Jain P, Marchant T, Green M et al. Inter-fraction motion and dosimetric consequences during breast intensity-modulated radiotherapy (IMRT). Radiother Oncol 2009;90:93–8. [DOI] [PubMed] [Google Scholar]
- 12. Feng CH, Gerry E, Chmura SJ et al. An image-guided study of setup reproducibility of postmastectomy breast cancer patients treated with inverse-planned intensity modulated radiation therapy. Int J Radiat Oncol Biol Phys 2015;91:58–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lee J, Liu SH, Lin JB et al. Image-guided study of inter-fraction and intra-fraction set-up variability and margins in reverse semi-decubitus breast radiotherapy. Radiat Oncol 2018;13:254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Thomsen MS, Harrov U, Fledelius W et al. Inter- and intra-fraction geometric errors in daily image-guided radiotherapy of free-breathing breast cancer patients measured with continuous portal imaging. Acta Oncol 2014;53:802–8. [DOI] [PubMed] [Google Scholar]
- 15. Harris EJ, Donovan EM, Coles CE et al. How does imaging frequency and soft tissue motion affect the PTV margin size in partial breast and boost radiotherapy? Radiother Oncol 2012;103:166–71. [DOI] [PubMed] [Google Scholar]
- 16. Yue NJ, Goyal S, Zhou J et al. Intrafractional target motions and uncertainties of treatment setup reference systems in accelerated partial breast irradiation. Int J Radiat Oncol Biol Phys 2011;79:1549–56. [DOI] [PubMed] [Google Scholar]
- 17. Kost S, Guo B, Xia P et al. Assessment of setup accuracy using anatomical landmarks for breast and Chest Wall irradiation with surface guided radiation therapy. Pract Radiat Oncol 2019;9:239–47. [DOI] [PubMed] [Google Scholar]
- 18. Sa AC, Fermento A, Neves D et al. Radiotherapy setup displacements in breast cancer patients: 3D surface imaging experience. Reports of Practical Oncology and Radiotherapy 2018;23:61–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mulliez T, Gulyban A, Vercauteren T et al. Setup accuracy for prone and supine whole breast irradiation. Strahlenther Onkol 2016;192:254–9. [DOI] [PubMed] [Google Scholar]
- 20. Kawamura M, Maeda Y, Yamamoto K et al. Development of the breast immobilization system in prone setup: The effect of bra in prone position to improve the breast setup error. J Appl Clin Med Phys 2017;18:155–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Testolin A, Ciccarelli S, Vidano G et al. Deep inspiration breath-hold intensity modulated radiation therapy in a large clinical series of 239 left-sided breast cancer patients: A dosimetric analysis of organs at risk doses and clinical feasibility from a single center experience. Br J Radiol 2019;92: 20190150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bergom C, Currey A, Desai N et al. Deep inspiration breath hold: Techniques and advantages for cardiac sparing during breast cancer irradiation. Front Oncol 2018;8:87. [DOI] [PMC free article] [PubMed] [Google Scholar]


