Abstract
BACKGROUND
Patellar instability is an uncommon complication after total knee arthroplasty (TKA). Partial lateral patella facetectomy (LPF) with lateral retinaculum release treatment of patellar instability is rarely reported.
CASE SUMMARY
We present a case of patellar instability 8 mo after primary TKA. Treatment of this complication was adapted to address the cause of the dislocation. To eliminate patellar instability, we restored the vastus medialis and performed LPF with lateral retinaculum release. We achieved normal patellar tracking. Clinical and radiographic evaluations at the 1-year postoperative follow-up were satisfactory.
CONCLUSION
LPF with lateral retinaculum release represents a promising option to restore central patellar tracking in patients with patellar instability after TKA in cases without component malposition.
Keywords: Total knee arthroplasty, Patellar instability, Lateral patella facetectomy, Complication, Case report
Core Tip: Patellar instability is an uncommon complication after total knee arthroplasty (TKA). We report a case who had patellar instability 8 mo after primary TKA, and skyline view revealed a lateral shift of the patella. To eliminate patellar instability, we restored the vastus medialis and performed partial lateral patella facetectomy with lateral retinaculum release. This report is the first to describe successful treatment of patellar instability after TKA by lateral patella facetectomy with lateral retinaculum release. This procedure represents a promising option to restore central patellar tracking in patients with patellar instability after TKA.
INTRODUCTION
Total knee arthroplasty (TKA) is an effective surgical procedure; however, a range of complications can occur. Patellar instability is a serious complication of TKA that may require revision surgery[1-3]. Patients with patellar instability after TKA present with anterior knee pain, giving-way, and functional limitation. Risk factors for patellar instability after TKA include surgical technique, prosthetic causes, and soft-tissue imbalance[4]. Management of patellar instability after TKA requires surgery[2,5-8]. Implant revision is required when patellar instability is related to prosthetic malposition. For soft-tissue imbalance, reconstruction of the medial patellofemoral ligament with lateral retinaculum release represents an effective treatment option.
Reports describing management of patellar instability after TKA using partial lateral patella facetectomy (LPF) with lateral retinaculum release has not been previously reported. Here, we present a case of patellar instability after TKA due to rupture of the vastus medialis that was treated by vastus medialis restoration and partial LPF with lateral retinaculum release. To our knowledge, this is first published report of patellar instability after TKA treated with LPF with lateral retinaculum release.
CASE PRESENTATION
Chief complaints
An 84-year-old female experienced severe anterior right knee pain 8 mo after TKA. In January 2018, the patient was referred to our department for therapy.
History of present illness
The patient was diagnosed with bilateral knee osteoarthritis and underwent right primary TKA in November 2016. Physical examination prior to primary TKA revealed a decrease in range of motion to 15°-50°. Figure 1 shows preoperative anteroposterior and lateral radiographs of the right knee and full-length weight-bearing radiographs of the lower extremities. The patient underwent posterior stabilized TKA with patellar denervation using the medial parapatellar approach. After implantation, functional patellar tracking was assessed by the surgeon (Prof. JLZ) using the “no thumb technique”. Lateral release was not performed. Range of motion and isometric quadriceps exercises were initiated immediately, and weight-bearing was allowed on postoperative day 1. Postoperatively, range of motion improved to 0°-120°. Eight months after surgery, the patient experienced severe anterior right knee pain.
Figure 1.
Primary total knee arthroplasty. A: Preoperative radiographs, anteroposterior view; B and C: Lateral views; and D: Full length weight-bearing of the lower extremities.
History of past illness
The patient had medical history of hypertension (American Society of Anesthesiologists physical status classification II due to hypertension).
Physical examination
Physical examination revealed patellar instability of the right knee, especially when the knee was in the flexion position, and that quadriceps strength was obviously lower in the right knee compared to the left. Clinical examination showed a limited range of motion.
Imaging examinations
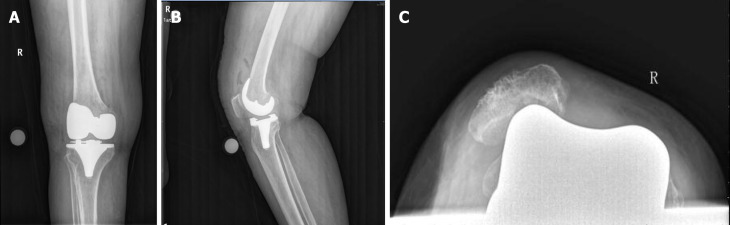
Radiographs did not demonstrate any obvious fractures or prosthetic malposition. Weight-bearing full length X-rays of the lower extremity demonstrated a well-restored mechanical axis. Skyline view revealed a lateral shift of the patella (Figure 2).
Figure 2.
Primary total knee arthroplasty. A: Postoperative radiographs of the right knee, anteroposterior view; B: Lateral view; and C: Skyline view.
FINAL DIAGNOSIS
As there were no structural imbalances or weakness in the injured knee, we diagnosed lateral patellar dislocation after TKA due to soft-tissue imbalance.
TREATMENT
We intended to stabilize the patella by medial patellofemoral ligament (MPFL) reconstruction combined with lateral retinaculum release. Exposure occurred through the same incision used for primary TKA, and the patella was everted and displaced laterally. During surgery, we found rupture of the vastus medialis, damage to the patella articular cartilage, and osteophyte formation in the lateral patella (Figure 3). In addition, the patella was small and thin and not suitable for patellar resurfacing. Therefore, we tentatively adopted a more targeted surgical method. We restored the vastus medialis, partially resected the lateral patella, and released the lateral retinaculum. Functional patellar tracking was confirmed throughout the range of motion. The operation took about 40 min.
Figure 3.
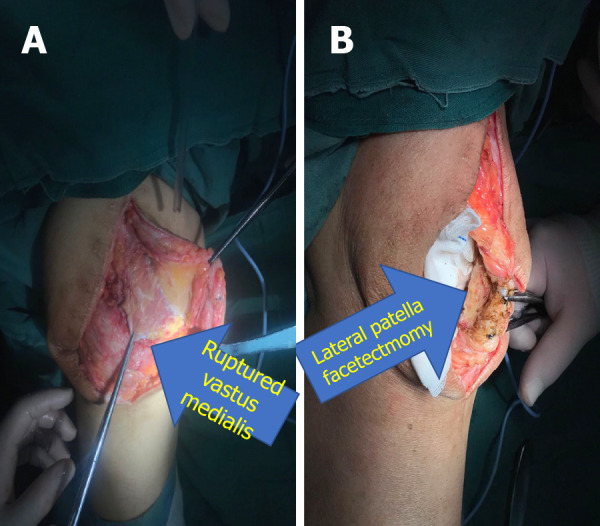
Reoperation. A: An intraoperative view of the ruptured vastus medialis; B: Partial lateral facetectomy.
OUTCOME AND FOLLOW-UP
This case shows that LPF with release of lateral retinaculum is effective in the treatment of patellar dislocation after TKA. The patient underwent clinical (Hospital for Special Surgery Clinical Score) and radiographic (anteroposterior, lateral, and skyline views) evaluation during 1-year of follow-up with no complaints of knee pain or subluxation. At the 1-year of follow-up, the patient was able to walk with a crutch, had active range of motion was 0°-110°, and had the Hospital for Special Surgery Clinical Score of 85.
DISCUSSION
TKA is a well-established procedure that is effective for the treatment of advanced knee joint arthritis. Management of the patellofemoral joint in TKA remains controversial but has an important impact on outcomes[9]. Inappropriate management of the patellofemoral joint may lead to a series of complications. Risk factors for patellofemoral joint instability in TKA include component positioning and limb alignment, component design, patellar preparation, and soft-tissue balancing[1].
To our knowledge, we are the first to report on the use of LPF with lateral retinaculum release for the treatment of patellar instability after TKA. In the present case, the patient had a small thin patella; therefore, she had undergone primary TKA with denervation instead of patella resurfacing, which may have led to patellar fracture[10]. Postoperatively, the femoral and tibial components were aligned and stable and tracking of the patella was normal[11-14]. After 8 mo, the patient experienced severe anterior right knee pain. We diagnosed lateral patellar dislocation. We speculated that nonresurfacing of the patella and soft-tissue imbalance contributed to patellofemoral instability in this patient. Seo et al[15] reported no significant clinical and radiological differences in patients with resurfaced vs nonresurfaced patellae; however, several meta-analyses have revealed a higher risk for reoperation in patients with nonresurfaced patellae[9,16-18]. The patient underwent primary TKA by a medial parapatellar approach, which may have damaged the vastus medialis, resulting in soft-tissue imbalance.
MPFL reconstruction and distal realignment of the patella represents an effective treatment option for patellar instability after TKA[2,8,19-21]. Carmont et al[22] and Goto et al[21] achieved good results using MPFL for patellar dislocation due to rupture of the medial structures after TKA. Similarly, Nakajima et al[8] reported satisfactory outcomes after adopting an Elmslie-Trillat procedure in combination with extensive lateral release to treat patellar instability after primary TKA in cases without component malposition (Table 1).
Table 1.
Published literature describing treatment for patellar instability after total knee arthroplasty
|
Ref.
|
Year
|
Case
|
Surgical technique
|
Follow-up
|
Outcome
|
Complication
|
| Nakajima et al[8] | 2010 | 1 | Elmslie-Trillat procedure with lateral release | 12 mo | Good | None |
| van Gennip et al[2] | 2012 | 9 | 7 MPFL reconstruction with lateral release, 2 MPFL reconstruction with lateral release and tibial tuberosity transfer | Mean 33 mo | Generally good | One report of subluxation |
| Goto et al[21] | 2014 | 1 | MPFL reconstruction and lateral release | 12 mo | Good | None |
| Lamotte et al[19] | 2016 | 6 | 5 MPFL reconstruction with additional procedure, 1 TKA revision | Mean 23 mo | Good | None |
| Current study | 2019 | 1 | Partial LPF with lateral retinaculum release | 12 mo | Good | None |
LPF: Lateral patella facetectomy; MPFL: Medial patellofemoral ligament; TKA: Total knee arthroplasty.
In this patient, we tentatively adopted a novel surgical approach to stabilize effectively the patella. We reconstructed the vastus medialis and performed partial LPF in combination with lateral retinaculum release. Patella facetectomy was first introduced by O’Donoghue[23]; subsequently, partial LPF was reported as an effective treatment for patellofemoral osteoarthritis, especially for alleviating anterior knee pain[24-29]. However, clinical evidence supporting the use of this method in the treatment of patellar instability after TKA is lacking. A number of studies showed that lateral retinaculum release is beneficial for correcting patellar maltracking[2,30-33]. The present case provides clinical evidence supporting the use of partial LPF in combination with lateral retinaculum release for the treatment of patellar instability after TKA.
CONCLUSION
In conclusion, to the authors’ knowledge, this report is the first to describe successful treatment of patellar instability after TKA by LPF with lateral retinaculum release. This procedure represents a promising option to restore central patellar tracking in patients with patellar instability after TKA.
Footnotes
Informed consent statement: The patient consented to the publication of this study.
Conflict-of-interest statement: The authors declare no conflicts of interest.
CARE Checklist (2016) statement: The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
Manuscript source: Unsolicited manuscript
Peer-review started: June 11, 2020
First decision: September 13, 2020
Article in press: September 28, 2020
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Nikolopoulos DD S-Editor: Zhang L L-Editor: Filipodia P-Editor: Wang LL
Contributor Information
Xian-Yue Shen, Department of Orthopedics, China-Japan Union Hospital of Jilin University, Changchun 130033, Jilin Province, China; Department of Orthopedics, The Second Hospital of Jilin University, Changchun 130041, Jilin Province, China.
Jian-Lin Zuo, Department of Orthopedics, China-Japan Union Hospital of Jilin University, Changchun 130033, Jilin Province, China.
Jian-Peng Gao, Department of Orthopedics, China-Japan Union Hospital of Jilin University, Changchun 130033, Jilin Province, China.
Tong Liu, Department of Orthopedics, China-Japan Union Hospital of Jilin University, Changchun 130033, Jilin Province, China.
Jian-Lin Xiao, Department of Orthopedics, China-Japan Union Hospital of Jilin University, Changchun 130033, Jilin Province, China. xiaojianlin10@jlu.edu.cn.
Yan-Guo Qin, Department of Orthopedics, The Second Hospital of Jilin University, Changchun 130041, Jilin Province, China.
References
- 1.Song SJ, Detch RC, Maloney WJ, Goodman SB, Huddleston JI 3rd. Causes of instability after total knee arthroplasty. J Arthroplasty. 2014;29:360–364. doi: 10.1016/j.arth.2013.06.023. [DOI] [PubMed] [Google Scholar]
- 2.van Gennip S, Schimmel JJ, van Hellemondt GG, Defoort KC, Wymenga AB. Medial patellofemoral ligament reconstruction for patellar maltracking following total knee arthroplasty is effective. Knee Surg Sports Traumatol Arthrosc. 2014;22:2569–2573. doi: 10.1007/s00167-012-2269-y. [DOI] [PubMed] [Google Scholar]
- 3.Archibeck MJ, White RE Jr. What's new in adult reconstructive knee surgery. J Bone Joint Surg Am. 2005;87:1656–1666. doi: 10.2106/JBJS.E.00364. [DOI] [PubMed] [Google Scholar]
- 4.Motsis EK, Paschos N, Pakos EE, Georgoulis AD. Review article: Patellar instability after total knee arthroplasty. J Orthop Surg (Hong Kong) 2009;17:351–357. doi: 10.1177/230949900901700322. [DOI] [PubMed] [Google Scholar]
- 5.Malo M, Vince KG. The unstable patella after total knee arthroplasty: etiology, prevention, and management. J Am Acad Orthop Surg. 2003;11:364–371. doi: 10.5435/00124635-200309000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Rosenberg AG, Jacobs JJ, Saleh KJ, Kassim RA, Christie MJ, Lewallen DG, Rand JA, Rubash HE. The patella in revision total knee arthroplasty. J Bone Joint Surg Am. 2003;85-A Suppl 1:S63–S70. doi: 10.2106/00004623-200300001-00012. [DOI] [PubMed] [Google Scholar]
- 7.Whiteside LA. Distal realignment of the patellar tendon to correct abnormal patellar tracking. Clin Orthop Relat Res. 1997:284–289. [PubMed] [Google Scholar]
- 8.Nakajima A, Watanabe H, Rokkaku T, Koda M, Yamada T, Murakami M. The Elmslie-Trillat procedure for recurrent patellar subluxation after total knee arthroplasty. J Arthroplasty 2010; 25: 1170.e1-1170. :e5. doi: 10.1016/j.arth.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 9.Abdel MP, Parratte S, Budhiparama NC. The patella in total knee arthroplasty: to resurface or not is the question. Curr Rev Musculoskelet Med. 2014;7:117–124. doi: 10.1007/s12178-014-9212-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lie DT, Gloria N, Amis AA, Lee BP, Yeo SJ, Chou SM. Patellar resection during total knee arthroplasty: effect on bone strain and fracture risk. Knee Surg Sports Traumatol Arthrosc. 2005;13:203–208. doi: 10.1007/s00167-004-0508-6. [DOI] [PubMed] [Google Scholar]
- 11.Pulavarti RS, Raut VV, McLauchlan GJ. Patella denervation in primary total knee arthroplasty - a randomized controlled trial with 2 years of follow-up. J Arthroplasty. 2014;29:977–981. doi: 10.1016/j.arth.2013.10.017. [DOI] [PubMed] [Google Scholar]
- 12.Beaupre L, Secretan C, Johnston DW, Lavoie G. A randomized controlled trial comparing patellar retention vs patellar resurfacing in primary total knee arthroplasty: 5-10 year follow-up. BMC Res Notes. 2012;5:273. doi: 10.1186/1756-0500-5-273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xie X, Pei F, Huang Z, Tan Z, Yang Z, Kang P. Does patellar denervation reduce post-operative anterior knee pain after total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc. 2015;23:1808–1815. doi: 10.1007/s00167-015-3566-z. [DOI] [PubMed] [Google Scholar]
- 14.Li T, Zhou L, Zhuang Q, Weng X, Bian Y. Patellar denervation in total knee arthroplasty without patellar resurfacing and postoperative anterior knee pain: a meta-analysis of randomized controlled trials. J Arthroplasty. 2014;29:2309–2313. doi: 10.1016/j.arth.2014.01.024. [DOI] [PubMed] [Google Scholar]
- 15.Seo SS, Kim CW, Moon SW. A Comparison of Patella Retention vs Resurfacing for Moderate or Severe Patellar Articular Defects in Total Knee Arthroplasty: Minimum 5-year Follow-up Results. Knee Surg Relat Res. 2011;23:142–148. doi: 10.5792/ksrr.2011.23.3.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen K, Li G, Fu D, Yuan C, Zhang Q, Cai Z. Patellar resurfacing vs nonresurfacing in total knee arthroplasty: a meta-analysis of randomised controlled trials. Int Orthop. 2013;37:1075–1083. doi: 10.1007/s00264-013-1866-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Patel K, Raut V. Patella in total knee arthroplasty: to resurface or not to--a cohort study of staged bilateral total knee arthroplasty. Int Orthop. 2011;35:349–353. doi: 10.1007/s00264-010-1063-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yim SJ, Jang MS, Kim WJ, Lee SH, Kang HK. The Effect of Electrocautery around the Patellar Rim in Patellar Non-Resurfacing Total Knee Arthroplasty. Knee Surg Relat Res. 2012;24:104–107. doi: 10.5792/ksrr.2012.24.2.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lamotte A, Neri T, Kawaye A, Boyer B, Farizon F, Philippot R. Medial patellofemoral ligament reconstruction for patellar instability following total knee arthroplasty: A review of 6 cases. Orthop Traumatol Surg Res. 2016;102:607–610. doi: 10.1016/j.otsr.2016.03.018. [DOI] [PubMed] [Google Scholar]
- 20.Csintalan RP, Latt LD, Fornalski S, Raiszadeh K, Inacio MC, Fithian DC. Medial patellofemoral ligament (MPFL) reconstruction for the treatment of patellofemoral instability. J Knee Surg. 2014;27:139–146. doi: 10.1055/s-0033-1360652. [DOI] [PubMed] [Google Scholar]
- 21.Goto T, Hamada D, Iwame T, Suzue N, Takeuchi M, Egawa H, Sairyo K. Medial patellofemoral ligament reconstruction for patellar dislocation due to rupture of the medial structures after total knee arthroplasty: a case report and review of the literature. J Med Invest. 2014;61:409–412. doi: 10.2152/jmi.61.409. [DOI] [PubMed] [Google Scholar]
- 22.Carmont MR, Crane T, Thompson P, Spalding T. Medial patellofemoral ligament reconstruction for subluxating patellofemoral arthroplasty. Knee. 2011;18:130–132. doi: 10.1016/j.knee.2010.02.011. [DOI] [PubMed] [Google Scholar]
- 23.O'Donoghue DH. Facetectomy. South Med J. 1972;65:645–654. [PubMed] [Google Scholar]
- 24.Yuenyongviwat V, Iamthanaporn K, Hongnaparak T. Lateral facetectomy decreased patellofemoral contact pressure in total knee replacement: A cadaveric study. J Clin Orthop Trauma. 2017;8:82–84. doi: 10.1016/j.jcot.2016.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wetzels T, Bellemans J. Patellofemoral osteoarthritis treated by partial lateral facetectomy: results at long-term follow up. Knee. 2012;19:411–415. doi: 10.1016/j.knee.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 26.Montserrat F, Alentorn-Geli E, León V, Ginés-Cespedosa A, Rigol P. Treatment of isolated patellofemoral osteoarthritis with lateral facetectomy plus Insall's realignment procedure: long-term follow-up. Knee Surg Sports Traumatol Arthrosc. 2013;21:2572–2577. doi: 10.1007/s00167-013-2431-1. [DOI] [PubMed] [Google Scholar]
- 27.Zhang LZ, Zhang XL, Jiang Y, Wang Q, Chen YS, Shen H. Lateral patellar facetectomy had improved clinical results in patients with patellar-retaining total knee arthroplasty. J Arthroplasty. 2012;27:1442–1447. doi: 10.1016/j.arth.2011.12.018. [DOI] [PubMed] [Google Scholar]
- 28.Pagenstert G, Seelhoff J, Henninger HB, Wirtz DC, Valderrabano V, Barg A. Lateral patellar facetectomy and medial reefing in patients with lateral facet syndrome after patellar-retaining total knee arthroplasty. J Arthroplasty. 2014;29:2156–2162. doi: 10.1016/j.arth.2014.06.014. [DOI] [PubMed] [Google Scholar]
- 29.Lakstein D, Naser M, Adar E, Atoun E, Edelman A, Hendel D. Partial lateral patellar facetectomy as an alternative to lateral release in Total Knee Arthroplasty (TKA) J Arthroplasty. 2014;29:2146–2149. doi: 10.1016/j.arth.2014.06.013. [DOI] [PubMed] [Google Scholar]
- 30.Roth S, Madarevic T, Vukelic L, Roth A, Gudac Madarevic D, Cicvaric T. Influence of arthroscopic lateral release on functional recovery in adolescents with recurrent patellar dislocation. Arch Orthop Trauma Surg. 2013;133:1441–1445. doi: 10.1007/s00402-013-1805-7. [DOI] [PubMed] [Google Scholar]
- 31.Unal B, Hinckel BB, Sherman SL, Lattermann C. Comparison of Lateral Retinaculum Release and Lengthening in the Treatment of Patellofemoral Disorders. Am J Orthop (Belle Mead NJ) 2017;46:224–228. [PubMed] [Google Scholar]
- 32.Menschik F, Landsiedl F. [Results of isolated lateral retinaculum release as a treatment method in patello-femoral dysfunction] Z Orthop Ihre Grenzgeb. 1992;130:218–222. doi: 10.1055/s-2008-1040142. [DOI] [PubMed] [Google Scholar]
- 33.Frosch S, Balcarek P, Walde TA, Schüttrumpf JP, Wachowski MM, Ferleman KG, Stürmer KM, Frosch KH. [The treatment of patellar dislocation: a systematic review] Z Orthop Unfall. 2011;149:630–645. doi: 10.1055/s-0030-1250691. [DOI] [PubMed] [Google Scholar]