Abstract
Fatigue is one of the most burdensome symptoms in interstitial lung disease (ILD) and can have a major impact on quality of life, social interactions, and work capacity. The cause of fatigue is complex; it is caused or aggravated by a combination of different predisposing, precipitating, and perpetuating factors. There is no uniform definition of fatigue, but it is often divided in physical and mental components. Several validated questionnaires can be used for structural assessment of fatigue in daily care. Although the high burden of fatigue in ILD is recognized increasingly, studies that have investigated pharmacologic and nonpharmacologic treatment options are scarce. Because fatigue in ILD is often a multifactorial problem, therapeutic interventions ideally should be aimed at different domains. One of the first steps is to optimize treatment of the underlying disease. Subsequently, treatable causes of fatigue should be identified and treated. Recently, an increasing number of studies showed that supportive measures have the potential to improve fatigue. However, evidence-based treatment guidelines are lacking, and more research is highly needed in this field. In clinical practice, a comprehensive, multidisciplinary, and individually tailored approach seems best fit to optimize treatment of fatigue in patients with ILD.
Abbreviations: FAS, fatigue assessment scale; ILD, interstitial lung disease; IPF, idiopathic pulmonary fibrosis; QoL, quality of life; sIL-2R, soluble IL-2 receptor (sIL-2R)
Interstitial lung disease (ILD) is a broad term for a group of >200 rare lung diseases. Some of these diseases are mainly inflammatory, while others are more fibrotic from the start, and many are a combination of both. This diversity in underlying pathobiologic conditions is also reflected in the variable clinical disease behavior: some ILDs are reversible; some have the potential to stabilize, and some have a progressive fatal course.1 ILDs often have a major impact on patients’ quality of life (QoL), daily living, work capacity, and social interactions.2 Most frequently reported symptoms are cough, dyspnea, and fatigue.3, 4, 5 Although the impact of fatigue is widely acknowledged, there is limited information about the cause and management of fatigue in ILDs. Most studies are conducted in patients with sarcoidosis, and, more recently, some small studies have been published on other ILDs. In this review, we will give an overview of the most recent insights of fatigue in ILD.
Case Report
A 37-year-old man presented at our outpatient clinic with sarcoidosis. His most burdensome symptoms were a dry cough and fatigue. The radiograph showed bilateral lymphadenopathy and discrete nodular abnormalities in the upper lobes. Pulmonary function tests were normal. Blood testing showed normal blood count and liver and kidney test results. Calcium and thyroid-stimulating hormone levels were also normal, while the soluble IL-2 receptor (sIL-2R) level was slightly elevated. Additional examination revealed OSA, for which he was treated successfully with CPAP, which resulted in his apnea-hypopnea index becoming normalized. However, fatigue did not improve. On follow up, his radiograph spontaneously improved; pulmonary function test results remained normal, and his sIL-2R normalized. Consultation at the cardiologist revealed no abnormalities. Subsequently, treatment with methylphenidate was initiated without success. Considering the major negative impact of fatigue on his QoL, we referred him to a psychologist for cognitive behavioral therapy.
Prevalence of Fatigue in ILD
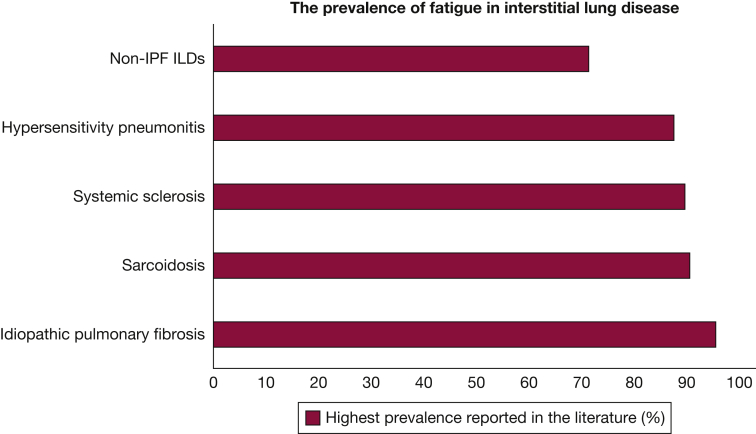
In the general population, fatigue is reported in 5% to 20%.6 Although fatigue is often reported as a common symptom in ILD, data about prevalence in different ILDs are scarce (Fig 1). In idiopathic pulmonary fibrosis (IPF), fatigue is reported in up to 95% of patients.4,7 In the European IPF registry, prevalence of fatigue was similar for patients with IPF (69.2%), compared with patients with non-IPF ILDs (70.6%). In systemic sclerosis studies, fatigue was present in up to 89% of the patients.8 In chronic hypersensitivity pneumonitis, fatigue has been reported in up to 87% of patients.9 A recent multinational survey showed that fatigue was present in 90% of patients with sarcoidosis, with up to 48% of patients mentioning extreme fatigue.5 Fatigue mostly occurs at disease onset and during the active phase of sarcoidosis. Nevertheless, even up to 56% of the patients with complete remission report fatigue.10 The prevalence of fatigue in different ILDs is difficult to compare, because different questionnaires were used. It also depends on whether fatigue is patient- or physician-reported. For instance, in a sarcoidosis registry study, physicians only reported fatigue in 30% of the patients, which is much lower than patient-reported fatigue in other studies.5,11 This emphasizes the importance of regularly asking patients whether fatigue is present.
Figure 1.
Reported prevalence of fatigue in interstitial lung disease. ILD = interstitial lung disease; IPF = idiopathic pulmonary fibrosis.
Cause of Fatigue in ILD
One of the complicating factors in studying fatigue is that there is no uniform definition of fatigue, although it is often divided into a physical and a mental component.6,12 Mental fatigue (perceived fatigability) can be described as a subjective symptom of malaise, tiredness, lack of energy, and aversion to activity.6,12,13 Physical fatigue (performance fatigability) refers to impaired physical performance.6,12 The cause of fatigue is poorly understood; however, physiologic, psychologic, and behavioral factors seem to play a role in the onset and persistence of fatigue.6,13 In most sarcoidosis studies, fatigue is poorly correlated with clinical parameters. However, in IPF and systemic sclerosis, there seems to be an association with disease severity.7,14, 15, 16 Many uncertainties still exist about the cause of fatigue, which are likely not ILD specific.
Fatigue is a prevalent symptom in many chronic disorders.17 A 2018 study demonstrated that only 11% of the variation in fatigue could be explained by the specific diagnosis. In this study, fatigue was explained mainly by transdiagnostic factors, such as reduced motivation, pain, limitations in physical functioning, concentration problems, reduced activity levels, poor sleep quality, and the ability to cope with fatigue.17
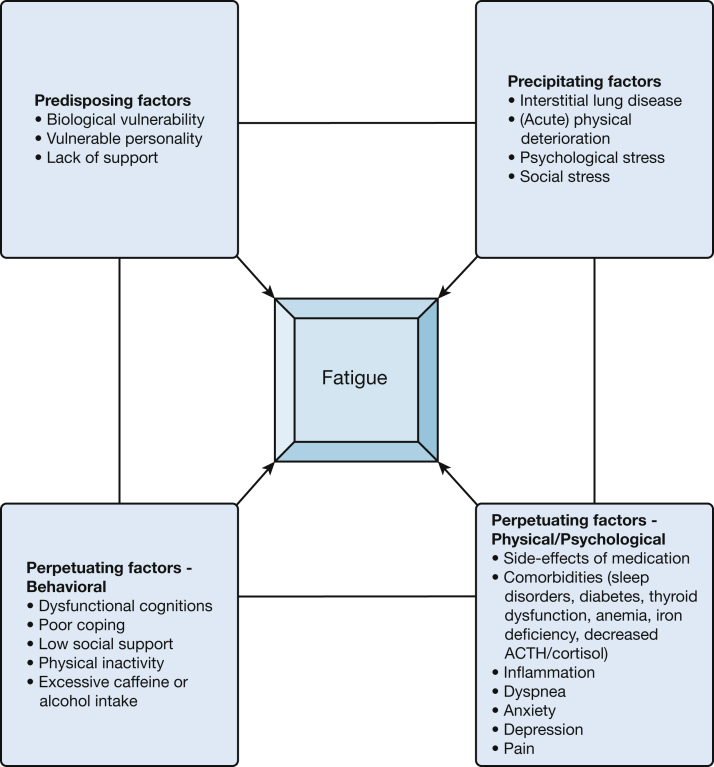
From other areas outside ILD, we have learned that factors that influence fatigue can be divided into predisposing factors, precipitating factors, and perpetuating factors.6,13 For a large part, many of these factors also hold true for ILD (Fig 2). Patients with predisposing factors such as biologic vulnerability, vulnerable personality, and lack of support are at increased risk of experiencing fatigue.6,18 In different forms of ILD, physical deterioration, psychological stress, and social stress have been described as precipitating factors that can cause fatigue.2,7,8,16 Furthermore, there is a wide range of physical, psychological, and behavioral factors that may further perpetuate fatigue and are described in more detail later.
Figure 2.
Predisposing, precipitating and perpetuating factors that can cause or aggravate fatigue in interstitial lung disease. Most of these factors are interrelated, and some are related in a bidirectional way. ACTH = adrenocorticotropic hormone.
Perpetuating Factors
Physical and Psychological Factors
Poor sleep quality is reported more frequently by patients with ILD than in the general population.16,19,20 Sleep architecture is often disrupted, with a decrease of rapid eye movement sleep, increase of sleep fragmentation, and more nocturnal desaturations compared with the general population.20,21 In a study on sleep quality in 15 patients with IPF, a significant correlation was found between nocturnal saturation and fatigue scores.22 Whether nocturnal supplemental oxygen has an effect on sleep quality and fatigue has not yet been studied. Other ILD-related factors that may alter the sleep architecture are cough, periodic limb movement, restless legs syndrome, and the side-effects of medication such as corticosteroids.19,20 Another reason for fatigue may be OSA, with a reported prevalence of up to 88% in ILD.20,21 The high prevalence of OSA could be explained partly by comorbidities, such as obesity or upper airway pathologic conditions. However, one study showed that, even when these comorbidities were excluded, OSA was found in 68% of the patients with ILD (82.3% in IPF, 66.6% in sarcoidosis, and 55.5% in systemic sclerosis). Another explanation proposed for the high prevalence of OSA is the upper airway collapse caused by the restrictive lung disease.20
It has been suggested that low-grade inflammation may play a role in fatigue; however, not many data for this exist in ILD. A study in patients with sarcoidosis who were in clinical remission demonstrated that a decrease in Th2 cytokine production was associated with fatigue.23 However, most studies have not found a relation between serologic markers (such as angiotensin-converting enzyme), sIL-2R and C-reactive protein, and fatigue.24 Furthermore, fatigue often persists in patients with sarcoidosis who are in clinical remission and have no signs of active inflammatory response.10
Medication is another factor that may cause or aggravate fatigue. Different studies have shown that corticosteroids are associated with fatigue and impaired QoL in sarcoidosis.25 Because fatigue is a registered common side-effect of corticosteroids, this may also play a role in other ILDs. Overall, corticosteroids often lead to side-effects such as weight gain, sleep disturbance, psychological disturbance, and diabetes mellitus, which are also associated independently with fatigue.20,24 Current treatment of IPF consists of the antifibrotic drugs nintedanib and pirfenidone.26 Fatigue is one of the registered side-effects of pirfenidone.26 Pooled data of the pirfenidone trials showed that fatigue occurred as an adverse event in 26% of the pirfenidone group and 19% of the placebo group.27 In an observational study on the long-term safety of pirfenidone in IPF, fatigue was reported as one of the most common adverse drug reactions in 18.5% of patients.28
Other comorbidities that are associated with fatigue are diabetes mellitus, thyroid dysfunction, anemia, iron deficiency, and decreased adrenocorticotropic hormone/cortisol levels.2,24,29 Evaluation of the presence of these comorbidities is important, because many are found to be more prevalent in ILDs and may impact not only fatigue but also influence the disease course. For instance, in patients with IPF, hypothyroidism and diabetes mellitus are more prevalent and are also associated with worse prognosis.16,29, 30, 31
Some small observational studies have found an association between physical activity, which was measured with wrist worn activity trackers, and fatigue in patients with ILD.10,32,33 Patients who were less active seemed to be more tired. The association between activity and fatigue seemed stronger in patients with IPF than in patients with sarcoidosis.32,33 Most patients with IPF report fatigue as physical exhaustion, while patients with sarcoidosis mainly report mental fatigue.7 This may explain the reason that fatigue is correlated more strongly with physical activity in IPF than in sarcoidosis. Other physical factors associated with fatigue in ILD are dyspnea, muscle strength, and pain.10,13,15
Anxiety, depressive symptoms, memory loss, and concentration problems (cognitive failure) are related to fatigue in a bidirectional way.34 Psychological symptoms are more prevalent not only in ILDs but also in other chronic diseases.7,8,16,17 Uncertainty about prognosis and a decrease in social and work participation are some of the factors that lead to increased stress and anxiety in ILD.2,35 In patients with (self-reported) cognitive impairment, normal daily tasks require more cognitive effort, which in turn might lead to higher fatigue levels.34 In sarcoidosis, small fiber neuropathy is reported frequently and is associated strongly with fatigue.5,34
Behavioral Factors
In general, behavioral factors, such as dysfunctional cognitions, poor coping, inactivity, excessive caffeine or alcohol intake, and low social support, can perpetuate fatigue.13 These factors have not been evaluated specifically in ILD in relation to fatigue. However, some of the aforementioned factors potentially could be managed by simple interventions and support from a social worker or psychologist. Therefore, we believe that behavioral factors should not be overlooked in the assessment and treatment of fatigue in ILD.
The Impact of Fatigue
Fatigue has a huge impact on many aspects of the lives of patients that include social relationships, work participation, and QoL. Many patients consider fatigue to be a very burdensome symptom.5,16 The impact of fatigue may be difficult to understand for family, friends, employers, and health care professionals because it is a nonspecific symptom and patients often look completely healthy. Consequently, some patients feel that they are not taken seriously, which may lead to further social isolation.2,6,34 Fatigue has been reported to be an important negative predictor of QoL in patients with ILD and has found to be associated with depression and anxiety, both in patients with sarcoidosis as well as with other ILDs.16,34 Furthermore, fatigue is associated with decreased work participation, loss of income, and social isolation.36, 37, 38 In turn, a low income has also been associated with the development of sarcoidosis-related comorbidities, such as fatigue.39 In a study on work performance in sarcoidosis, 43% of 755 patients underwent disability evaluation. In these patients, fatigue levels were significantly higher than in the group who had not undergone work capacity assessments.
Measurement of Fatigue
Although highly prevalent, fatigue is often not structurally assessed in patients with ILD. Evaluating fatigue can be challenging due to the different determinants of fatigue and the lack of a uniform approach.12 Obviously, active evaluation of fatigue and other burdensome symptoms should take place during every visit. Extensive history taking is needed to assess the severity and impact of fatigue on patients’ lives and to identify possible perpetuating factors. In addition to this, different questionnaires can be used for a more structured evaluation of fatigue. The Fatigue Assessment Scale (FAS) and the Sarcoidosis Assessment Tool fatigue subscale were developed to assess fatigue in patients with sarcoidosis. The FAS is used most commonly, also in other ILDs. It consists of ten questions on a five-point response scale; five questions about physical fatigue and five questions about mental fatigue. The total score ranges from 10 to 50 points; a score of ≥22 points indicates fatigue and ≥34 points severe fatigue. The minimal clinical importance difference is 4 points.40 The Sarcoidosis Assessment Tool fatigue subscale consist of five questions and is incorporated in a QoL questionnaire. Other questionnaires that have been used to measure fatigue in ILD are the Functional assessment of chronic illness Therapy-Fatigue and the Patient Reported Outcomes Measurement Information Systems Fatigue Instrument.41 These questionnaires may be used not only to quantify fatigue in clinical trials but also to assess the effect of treatment for individual patients in clinical practice.
Treatment of Fatigue in ILD
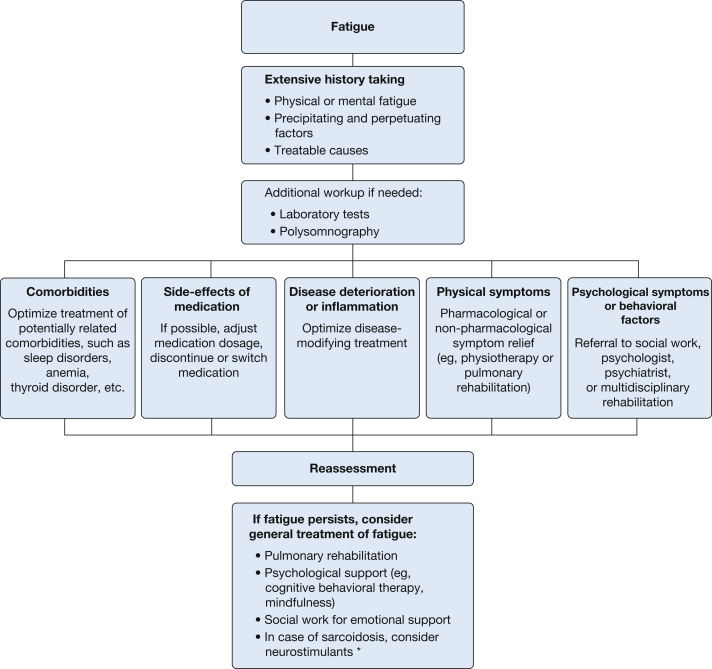
Even though the high burden of fatigue in ILD is well-recognized, studies that have investigated treatment options are limited. Because fatigue in ILD is often a multidimensional problem, therapeutic interventions ideally should be aimed at the different domains that are involved. Figure 3 shows a decision-making flowchart on how to handle fatigue in ILD. One of the first steps is to optimize treatment of the underlying disease and to exclude that fatigue is a side-effect of prescribed medication. The side-effects of corticosteroid use, especially, should be monitored thoroughly, and the prescribed dosage should be reassessed regularly and down-titrated if possible. Subsequently, treatable causes of fatigue should be excluded. As mentioned before, one of the treatable causes of fatigue in ILD is OSA. Two studies in IPF concluded that effective CPAP treatment improved daily living activities, quality of sleep, QoL, and daytime fatigue.21,42 Currently, a trial is ongoing to assess the prevalence and the effect of CPAP treatment in patients with sarcoidosis with OSA.43 Comorbidities, such as hypothyroidism, should be treated optimally, although no studies have reported on the effect of treatment of comorbidities on fatigue.30 In patients with depression, anxiety, or stress, referral to a psychologist could be considered. Because a high symptom burden of the underlying disease may also lead directly or indirectly to fatigue, treatment should also be directed at symptom relief. At the moment, a randomized controlled trial is assessing the effect of advancing symptom alleviation with palliative treatment in ILD. In that study, the intervention group is supported by a nurse and social worker with the aim of relieving burdensome symptoms, such as fatigue.44
Figure 3.
Decision-making flowchart on how to manage fatigue in interstitial lung disease. The asterisk indicates limited evidence, prescribe with caution.
When all systemic treatable causes have been excluded, the focus should be on the other domains. As far as possible, behavioral, precipitating, and perpetuating factors should be identified and, where possible, targeted. There is increasing evidence that exercise therapy or pulmonary rehabilitation could be beneficial in patients with ILD and fatigue. Pulmonary rehabilitation is a comprehensive intervention that consists of exercise training, education, and self-management strategies.45 One study showed a positive effect of a 6-week pulmonary rehabilitation program on fatigue in IPF.45 The treatment guideline of IPF also recommends pulmonary rehabilitation to alleviate symptoms.26 A randomized trial with patients with different ILDs demonstrated that an 8-week supervised exercise program improved fatigue scores, exercise capacity, and QoL.46 Similar positive results were found in sarcoidosis studies.47 Next to pulmonary rehabilitation, cognitive behavioral therapy has been proposed as a potential treatment option for patients with sarcoidosis-associated fatigue.2 A pilot study in sarcoidosis showed that a 45-minute mindfulness-based workshop improved fatigue and other symptom scores directly after the intervention.48 Long-term effects of this mindfulness workshop have not yet been evaluated. At the moment, a randomized controlled study to evaluate the effects of a 12-week online cognitive behavioral therapy in patients with sarcoidosis-associated fatigue (FAS score, ≥22 points) is ongoing.49 Although cognitive behavioral therapy has also been suggested in IPF, no studies have been conducted to date. Because fatigue is also perpetuated by inactivity, low social support, and psychological wellbeing, tailored interventions by physiotherapists, psychologists, or social workers may sometimes improve symptoms.
Neurostimulants have been suggested as potential treatment options for fatigue in sarcoidosis. The effect of dexmethylphenidate hydrochloride and armodafinil on sarcoidosis-associated fatigue was first described in 2008.50,51 Dexmethylphenidate hydrochloride, which inhibits dopamine and noradrenaline in the brain, was studied in 10 patients. Armodafinil, which increases extracellular dopamine levels in the brain and is mainly used in narcolepsy, was studied in 15 patients. Both of these neurostimulants led to a significant improvement in fatigue scores and appeared to be safe. While the results of these studies were promising, only a small number of patients were included.
Currently, a new study on the effect and side-effects of methylphenidate in sarcoidosis-associated fatigue is being conducted. This trial was mainly initiated to determine the feasibility and design of a future large-scale randomized, controlled trial. Hopefully, these results will enable larger scale future studies to provide better evidence for the use of neurostimulants for fatigue in sarcoidosis.52 The use of these agents has not been investigated, and their use cannot be recommended in other ILDs.
It has been suggested that anti-TNF-α treatment may have positive effects on sarcoidosis-associated fatigue; however, this finding has not been replicated in a randomized trial.53 At present, no studies have evaluated the effects of pharmacologic interventions in other ILDs.
Most of the data on how to deal with fatigue in ILD currently stem from sarcoidosis.41 Although we believe that there are many similarities between fatigue in chronic diseases and ILD and between sarcoidosis and other ILDs, important differences exist.2,7,16 Stable chronic diseases may have more general approaches; while in progressive fatal diseases like IPF, disease course and prognosis will also dictate treatment choices.54 In diseases with more rapid disease progression and worse prognosis, treatment of fatigue should be a part of integrated palliative care programs. To further advance insights into fatigue and develop better treatment strategies, more research obviously is needed. On one hand, the multifactorial cause in often heterogeneous populations increases the complexity of the research; on the other hand, collaboration with partners outside the ILD research area could help to generate progress in the field, because fatigue is a universal problem in many chronic diseases.
Conclusion
Fatigue is a major problem both for patients with ILD and for treating physicians. The cause of fatigue in ILD is likely multifactorial, but many aspects are still unknown. Different predisposing, precipitating, and perpetuating factors contribute to fatigue, of which many also play a role in other chronic diseases. Unfortunately, specific guidelines and evidence-based treatment recommendations for fatigue are still lacking. In clinical practice, a comprehensive, multidisciplinary, and individually tailored approach seems to be the best fit to optimize treatment of fatigue in ILDs. Hopefully, new studies will lead to better treatment options for fatigue and ultimately improve QoL for patients with ILD.
Acknowledgments
Financial/nonfinancial disclosures: None declared.
Footnotes
Drs Kahlmann and Moor share first authorship.
FUNDING/SUPPORT: The authors have reported to CHEST that no funding was received for this study.
References
- 1.Travis W.D., Costabel U., Hansell D.M. An official American Thoracic Society/European Respiratory Society statement: update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2013;188(6):733–748. doi: 10.1164/rccm.201308-1483ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Drent M., Strookappe B., Hoitsma E., De Vries J. Consequences of sarcoidosis. Clin Chest Med. 2015;36(4):727–737. doi: 10.1016/j.ccm.2015.08.013. [DOI] [PubMed] [Google Scholar]
- 3.Guenther A., Krauss E., Tello S. The European IPF registry (eurIPFreg): baseline characteristics and survival of patients with idiopathic pulmonary fibrosis. Respir Res. 2018;19(1):141. doi: 10.1186/s12931-018-0845-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rajala K., Lehto J.T., Sutinen E., Kautiainen H., Myllarniemi M., Saarto T. mMRC dyspnoea scale indicates impaired quality of life and increased pain in patients with idiopathic pulmonary fibrosis. ERJ Open Res. 2017;3(4) doi: 10.1183/23120541.00084-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Voortman M., Hendriks C.M.R., Elfferich M.D.P. The burden of sarcoidosis symptoms from a patient perspective. Lung. 2019;197(2):155–161. doi: 10.1007/s00408-019-00206-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sharpe M., Wilks D. Fatigue. BMJ. 2002;325(7362):480–483. doi: 10.1136/bmj.325.7362.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Atkins C.P., Gilbert D., Brockwell C., Robinson S., Wilson A.M. Fatigue in sarcoidosis and idiopathic pulmonary fibrosis: differences in character and severity between diseases. Sarcoidosis Vasc Diffuse Lung Dis. 2016;33(2):130–138. [PubMed] [Google Scholar]
- 8.Ibn Yacoub Y., Amine B., Bensabbah R., Hajjaj-Hassouni N. Assessment of fatigue and its relationships with disease-related parameters in patients with systemic sclerosis. Clin Rheumatol. 2012;31(4):655–660. doi: 10.1007/s10067-011-1906-z. [DOI] [PubMed] [Google Scholar]
- 9.Lubin M., Chen H., Elicker B., Jones K.D., Collard H.R., Lee J.S. A comparison of health-related quality of life in idiopathic pulmonary fibrosis and chronic hypersensitivity pneumonitis. Chest. 2014;145(6):1333–1338. doi: 10.1378/chest.13-1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Korenromp I.H.E., Heijnen C.J., Vogels O.J.M., van den Bosch J.M.M., Grutters J.C. Characterization of chronic fatigue in patients with sarcoidosis in clinical remission. Chest. 2011;140(2):441–447. doi: 10.1378/chest.10-2629. [DOI] [PubMed] [Google Scholar]
- 11.Thillai M., Chang W., Chaudhuri N. Sarcoidosis in the UK: insights from British Thoracic Society registry data. BMJ Open Respir Res. 2019;6(1) doi: 10.1136/bmjresp-2018-000357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gruet M. Fatigue in chronic respiratory diseases: theoretical framework and implications for real-life performance and rehabilitation. Front Physiol. 2018;9:1285. doi: 10.3389/fphys.2018.01285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Spruit M.A., Vercoulen J.H., Sprangers M.A.G., Wouters E.F.M., FAntasTIGUE Consortium Fatigue in COPD: an important yet ignored symptom. Lancet Respir Med. 2017;5(7):542–544. doi: 10.1016/S2213-2600(17)30158-3. [DOI] [PubMed] [Google Scholar]
- 14.Michielsen H.J., Drent M., Peros-Golubicic T., De Vries J. Fatigue is associated with quality of life in sarcoidosis patients. Chest. 2006;130(4):989–994. doi: 10.1378/chest.130.4.989. [DOI] [PubMed] [Google Scholar]
- 15.Swigris J.J., Yorke J., Sprunger D.B. Assessing dyspnea and its impact on patients with connective tissue disease-related interstitial lung disease. Respir Med. 2010;104(9):1350–1355. doi: 10.1016/j.rmed.2010.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Basta F., Afeltra A., Margiotta D.P.E. Fatigue in systemic sclerosis: a systematic review. Clin Exp Rheumatol. 2018;36(Suppl 113)(4):150–160. [PubMed] [Google Scholar]
- 17.Menting J., Tack C.J., Bleijenberg G. Is fatigue a disease-specific or generic symptom in chronic medical conditions? Health Psychol. 2018;37(6):530–543. doi: 10.1037/hea0000598. [DOI] [PubMed] [Google Scholar]
- 18.Korenromp I.H., Grutters J.C., van den Bosch J.M., Heijnen C.J. Post-inflammatory fatigue in sarcoidosis: personality profiles, psychological symptoms and stress hormones. J Psychosom Res. 2012;72(2):97–102. doi: 10.1016/j.jpsychores.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 19.Bosse-Henck A., Wirtz H., Hinz A. Subjective sleep quality in sarcoidosis. Sleep Med. 2015;16(5):570–576. doi: 10.1016/j.sleep.2014.12.025. [DOI] [PubMed] [Google Scholar]
- 20.Pihtili A., Bingol Z., Kiyan E., Cuhadaroglu C., Issever H., Gulbaran Z. Obstructive sleep apnea is common in patients with interstitial lung disease. Sleep Breath. 2013;17(4):1281–1288. doi: 10.1007/s11325-013-0834-3. [DOI] [PubMed] [Google Scholar]
- 21.Mermigkis C., Bouloukaki I., Antoniou K. Obstructive sleep apnea should be treated in patients with idiopathic pulmonary fibrosis. Sleep Breath. 2015;19(1):385–391. doi: 10.1007/s11325-014-1033-6. [DOI] [PubMed] [Google Scholar]
- 22.Mermigkis C., Stagaki E., Amfilochiou A. Sleep quality and associated daytime consequences in patients with idiopathic pulmonary fibrosis. Med Princ Pract. 2009;18(1):10–15. doi: 10.1159/000163039. [DOI] [PubMed] [Google Scholar]
- 23.Korenromp I.H., Grutters J.C., van den Bosch J.M., Zanen P., Kavelaars A., Heijnen C.J. Reduced Th2 cytokine production by sarcoidosis patients in clinical remission with chronic fatigue. Brain Behav Immun. 2011;25(7):1498–1502. doi: 10.1016/j.bbi.2011.06.004. [DOI] [PubMed] [Google Scholar]
- 24.Drent M., Lower E.E., De Vries J. Sarcoidosis-associated fatigue. Eur Respir J. 2012;40(1):255–263. doi: 10.1183/09031936.00002512. [DOI] [PubMed] [Google Scholar]
- 25.Judson M.A., Chaudhry H., Louis A., Lee K., Yucel R. The effect of corticosteroids on quality of life in a sarcoidosis clinic: the results of a propensity analysis. Respir Med. 2015;109(4):526–531. doi: 10.1016/j.rmed.2015.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Raghu G., Rochwerg B., Zhang Y. An official ATS/ERS/JRS/ALAT clinical practice guideline: treatment of idiopathic pulmonary fibrosis: an update of the 2011 Clinical Practice Guideline. Am J Respir Crit Care Med. 2015;192(2):e3–e19. doi: 10.1164/rccm.201506-1063ST. [DOI] [PubMed] [Google Scholar]
- 27.Costabel U., Albera C., Wijsenbeek M.S. Fatigue in patients with idiopathic pulmonary fibrosis (IPF) from the pooled pirfenidone (PFD) phase III trials. Eur Respir J. 2017;50:PA4875. [Google Scholar]
- 28.Cottin V., Koschel D., Gunther A. Long-term safety of pirfenidone: results of the prospective, observational PASSPORT study. ERJ Open Res. 2018;4(4):00084–2018. doi: 10.1183/23120541.00084-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Suzuki A., Kondoh Y. The clinical impact of major comorbidities on idiopathic pulmonary fibrosis. Respir Investig. 2017;55(2):94–103. doi: 10.1016/j.resinv.2016.11.004. [DOI] [PubMed] [Google Scholar]
- 30.Oldham J.M., Kumar D., Lee C. Thyroid disease is prevalent and predicts survival in patients with idiopathic pulmonary fibrosis. Chest. 2015;148(3):692–700. doi: 10.1378/chest.14-2714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yokoi K., Konomi A. Iron deficiency without anaemia is a potential cause of fatigue: meta-analyses of randomised controlled trials and cross-sectional studies. Br J Nutr. 2017;117(10):1422–1431. doi: 10.1017/S0007114517001349. [DOI] [PubMed] [Google Scholar]
- 32.Bahmer T., Kirsten A.M., Waschki B. Clinical correlates of reduced physical activity in idiopathic pulmonary fibrosis. Respiration. 2016;91(6):497–502. doi: 10.1159/000446607. [DOI] [PubMed] [Google Scholar]
- 33.Bahmer T., Watz H., Develaska M. Physical activity and fatigue in patients with sarcoidosis. Respiration. 2018;95(1):18–26. doi: 10.1159/000481827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hendriks C., Drent M., De Kleijn W., Elfferich M., Wijnen P., De Vries J. Everyday cognitive failure and depressive symptoms predict fatigue in sarcoidosis: a prospective follow-up study. Respir Med. 2018;138S:S24–S30. doi: 10.1016/j.rmed.2017.11.008. [DOI] [PubMed] [Google Scholar]
- 35.Russell A.M., Ripamonti E., Vancheri C. Qualitative European survey of patients with idiopathic pulmonary fibrosis: patients' perspectives of the disease and treatment. BMC Pulm Med. 2016;16:10. doi: 10.1186/s12890-016-0171-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hendriks C.M.R., Saketkoo L.A., Elfferich M.D.P., De Vries J., Wijnen P., Drent M. Sarcoidosis and work participation: the need to develop a disease-specific core set for assessment of work ability. Lung. 2019;197(4):407–413. doi: 10.1007/s00408-019-00234-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rice J.B., White A., Lopez A. Economic burden of sarcoidosis in a commercially-insured population in the United States. J Med Econ. 2017;20(10):1048–1055. doi: 10.1080/13696998.2017.1351371. [DOI] [PubMed] [Google Scholar]
- 38.Morrisroe K., Sudararajan V., Stevens W. Work productivity in systemic sclerosis, its economic burden and association with health-related quality of life. Rheumatology (Oxford) 2018;57(1):73–83. doi: 10.1093/rheumatology/kex362. [DOI] [PubMed] [Google Scholar]
- 39.Harper LJ, Gerke AK, Wang XF, et al. Income and other contributors to poor outcomes in U. S. patients with sarcoidosis. Am J Respir Crit Care Med. 2020;201(8):955-964. [DOI] [PMC free article] [PubMed]
- 40.de Kleijn W.P., De Vries J., Wijnen P.A., Drent M. Minimal (clinically) important differences for the fatigue assessment scale in sarcoidosis. Respir Med. 2011;105(9):1388–1395. doi: 10.1016/j.rmed.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 41.Judson M.A. Quality of life in sarcoidosis. Semin Respir Crit Care Med. 2017;38(4):546–558. doi: 10.1055/s-0037-1602589. [DOI] [PubMed] [Google Scholar]
- 42.Mermigkis C., Bouloukaki I., Antoniou K.M. CPAP therapy in patients with idiopathic pulmonary fibrosis and obstructive sleep apnea: does it offer a better quality of life and sleep? Sleep Breath. 2013;17(4):1137–1143. doi: 10.1007/s11325-013-0813-8. [DOI] [PubMed] [Google Scholar]
- 43.National Institutes of Health Clinical Center . National Institutes of Health; Bethesda, MD: 2019. Prevalence of obstructive sleep apnea syndrome in sarcoidosis and impact of CPAP treatment on associated fatigue status (sarcoidosas) NCT03926832. ClinicalTrials.gov.https://clinicaltrials.gov/ct2/show/NCT03926832 Updated October 23, 2019. [Google Scholar]
- 44.National Institutes of Health Clinical Center . National Institutes of Health; Bethesda, MD: 2016. Advancing symptom alleviation with palliative treatment (ADAPT). NCT02713347. ClinicalTrials.gov.https://clinicaltrials.gov/ct2/show/NCT02713347 Updated January 27. 2020. [Google Scholar]
- 45.Swigris J.J., Fairclough D.L., Morrison M. Benefits of pulmonary rehabilitation in idiopathic pulmonary fibrosis. Respir Care. 2011;56(6):783–789. doi: 10.4187/respcare.00939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dowman L.M., McDonald C.F., Hill C.J. The evidence of benefits of exercise training in interstitial lung disease: a randomised controlled trial. Thorax. 2017;72(7):610–619. doi: 10.1136/thoraxjnl-2016-208638. [DOI] [PubMed] [Google Scholar]
- 47.Lingner H., Buhr-Schinner H., Hummel S. Short-term effects of a multimodal 3-week inpatient pulmonary rehabilitation programme for patients with sarcoidosis: the ProKaSaRe study. Respiration. 2018;95(5):343–353. doi: 10.1159/000486964. [DOI] [PubMed] [Google Scholar]
- 48.Saketkoo L.A., Karpinski A., Young J. Feasibility, utility and symptom impact of modified mindfulness training in sarcoidosis. ERJ Open Res. 2018;4(2):00085–2017. doi: 10.1183/23120541.00085-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Netherlands Trial Register Trial NL7816. https://www.trialregister.nl/trial/7816
- 50.Lower E.E., Harman S., Baughman R.P. Double-blind, randomized trial of dexmethylphenidate hydrochloride for the treatment of sarcoidosis-associated fatigue. Chest. 2008;133(5):1189–1195. doi: 10.1378/chest.07-2952. [DOI] [PubMed] [Google Scholar]
- 51.Lower E.E., Malhotra A., Surdulescu V., Baughman R.P. Armodafinil for sarcoidosis-associated fatigue: a double-blind, placebo-controlled, crossover trial. J Pain Symptom Manage. 2013;45(2):159–169. doi: 10.1016/j.jpainsymman.2012.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Atkins C., Fordham R., Clark A.B., Stockl A., Jones A.P., Wilson A.M. Feasibility study of a randomised controlled trial to investigate the treatment of sarcoidosis-associated fatigue with methylphenidate (FaST-MP): a study protocol. BMJ Open. 2017;7(12) doi: 10.1136/bmjopen-2017-018532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Elfferich M.D., Nelemans P.J., Ponds R.W., De Vries J., Wijnen P.A., Drent M. Everyday cognitive failure in sarcoidosis: the prevalence and the effect of anti-TNF-alpha treatment. Respiration. 2010;80(3):212–219. doi: 10.1159/000314225. [DOI] [PubMed] [Google Scholar]
- 54.Kreuter M., Bendstrup E., Russell A.M. Palliative care in interstitial lung disease: living well. Lancet Respir Med. 2017;5(12):968–980. doi: 10.1016/S2213-2600(17)30383-1. [DOI] [PubMed] [Google Scholar]