Abstract
Background: Recent reports suggest an association between ethnicity and COVID-19 mortality. In the present multi-center study, we aimed to assess the differences underlying this association, and ascertain whether ethnicity also mediates other aspects of COVID-19 like cardiovascular complications. Methods: Data were collected from a mixed-ethnicity UK cohort of 613 patients admitted and diagnosed COVID-19 positive, across six hospitals in London during the second half of March 2020: 292 were White Caucasian ethnicity, 203 were Asian and 118 were of Afro-Caribbean ethnicity. Results: Caucasian patients were older (P<0.001) and less likely to have hypertension (P=0.038), while Afro-Caribbean patients had higher prevalence of diabetes mellitus (P<0.001). Asian patients were more likely to present with venous thromboembolic disease (adj.OR=4.10, 95% CI 1.49-11.27, P=0.006). On the other hand, Afro-Caribbean had more heart failure (adj.OR=3.64, 95% CI 1.50-8.84, P=0.004) and myocardial injury (adj.OR=2.64, 95% CI 1.10-6.35, P=0.030). Importantly, our adjusted multi-variate Cox regression analysis revealed significantly higher all-cause mortality both for Asian (adj.HR=1.89, 95% CI 1.23-2.91, P=0.004) and Afro-Caribbean ethnicity (adj.HR=2.09, 95% CI 1.30-3.37, P=0.002). Conclusions: Our data show that COVID-19 may have different presentations and follow different clinical trajectories depending on the ethnicity of the affected subject. Awareness of complications more likely to arise in specific ethnicities will allow a more timely diagnosis and preventive measures for patients at risk. Due to increased mortality, individuals of Afro-Caribbean and Asian ethnicity should be considered as high-risk groups. This may have an impact on health-resource allocation and planning, definition of vulnerable groups, disease management, and the protection of healthcare workers at the frontline.
Keywords: COVID-19, mortality, ethnicity
Introduction
As the coronavirus disease (COVID-19) spreads globally, more scientific reports are published on its related mortality and clinical outcomes. Early data from Chinese populations suggested that main risk factors for hospital admission and mortality include: hypertension, diabetes, male gender, age and cardiovascular disease [1]. Further studies from Italy reported that smoking and cardio-metabolic comorbidity can have detrimental effects when these are combined with COVID-19 leading to significant number of deaths [2]. Beyond that, striking differences in mortality rates across such countries indicated that ethnicity is also involved in the outcome of this disease [3-5].
Ethnicity is actually a complex entity which involves a number of parameters such as genetics, cultural, social and behavioral aspects. The higher mortality in Black, Asian and Minority Ethnic (BAME) health professionals in the United Kingdom (UK) suggested that ethnicity could be a risk factor for mortality due to COVID-19. In the UK, the National Health Service (NHS) provides free healthcare to the entire population, suggesting that the aforementioned is not due to difficulties in accessing the healthcare system. A recent analysis suggests that social factors such as income deprivation are associated with COVID-19 mortality [3]. London has a multi-ethnic demography and data from this diverse population can be used to further understand potential reasons underlying the association of ethnicity with adverse outcomes in COVID-19.
In the present multi-center study of a mixed-ethnicity UK cohort of patients admitted to hospital with COVID-19, we aimed to clarify whether different clinical trajectories across the different ethnicities, with emphasis on cardiovascular complications, can explain the different mortality rates among certain ethnic groups.
Methods
Study population and design
In this multi-center observational study, we enrolled 613 patients admitted to six hospitals in London who were diagnosed as COVID-19 positive. The study period was the second half of March 2020. There were no experiments involved in this study. As per the UK Health Research Authority deliberation this investigation did not require Ethics Committee review (guidance toolkit available online [http://www.hra-decisiontools.org.uk/ethics/]). This study meets criteria for auditing as no active intervention, randomization to therapy, additional post-admission follow-up or survey was conducted. A clinical audit is a process for improving the quality of patient care and outcomes introduced to the NHS in the late 80s [https://navigator.health.org.uk/theme/working-patients-white-paper?gclid=CjwKCAjw97P5BRBQEiwAGflV6VzKOGvUszuqDeEFPDU7SD9YbrVxZNvJ_-GXOoGGBM5Dtb2kf-CrAhoCgUEQAvD_BwE]. In this case it involved reviewing the healthcare delivered to patients of different ethnicities and assessing their outcomes to ensure that best practices were carried out [http://www.clinicalauditsupport.com/what-is-clinical-audit.html] [https://www.england.nhs.uk/clinaudit/].
As an observational study and audit it was approved by the Clinical Effectiveness Unit at Barts Health NHS Trust (Project ID: 11103; Title: COVID-19 and cardiovascular disease (CVD) outcomes) and the Quality and Governance Department at Royal Free London NHS Trust (Audit: Cardiovascular Implications and Outcomes of Patients with COVID-19). Patients provided their oral consent for the treatment received and for their data to be used. In the UK, Section 60 of the Health and Social Care Act 2001 currently provides an interim power to ensure that patient identifiable information, needed to support a range of important work such as clinical audit, record validation and research, can be used without the consent of patients [https://www.legislation.gov.uk/ukpga/2001/15/section/60/enacted].
Patient demographic/clinical characteristics, laboratory results, procedures, comorbidities, treatments (cardiovascular and non-cardiovascular) and outcomes were extracted from the electronic records and paper notes. These were collected by 6 independent doctors in training, and subsequently blinded validated by 4 senior physicians/consultants.
All study patients were COVID-19 positive, as confirmed by polymerase chain reaction (PCR) swab. Patients with 2 positive swabs were considered eligible for inclusion in the study. All tests were requested on the basis of clinical suspicion for COVID-19.
Participants included in this study were of the following geographic areas/origins: India, Bangladesh, Pakistan, Africa, North and Sound America, Caribbean, China, Europe/United Kingdom, Philippines. Patients were grouped into three ethnicities: Caucasian (“White British” or “Other White Group”), Asian (“Indian”, “Bangladeshi”, “Pakistani”, “Chinese” and “Other Asian Group”) and Afro-Caribbean (“African”, “Caribbean”, and “Other Mixed Group”).
Measurement of blood parameters
Routine bloods were obtained from patients on and during admission, as per local Trusts’ protocols. Routine hospital laboratory methods were used for the analysis. These were available on the electronic systems and included: full blood count parameters, creatinine, C-reactive protein (CRP), creatine kinase (CK), lactate dehydrogenase (LDH), high-sensitivity troponin T, N-terminal pro B-type natriuretic peptide (NT-proBNP), D-Dimers, activated partial thromboplastin time (APTT), and international normalised ratio (INR). Glomerular filtration rate (eGFR) was estimated using the Modification of Diet in Renal Disease (MDRD) Study equation.
Study endpoints
We assessed the cohort for differences occurring across ethnicities relating to mortality and/or cardiovascular events (primary endpoints): (i) myocardial injury, defined as high sensitivity troponin above the 99th percentile of normal, (ii) acute heart failure (HF), (iii) acute atrial fibrillation (AF) episode, (iv) stroke, (v) venous thromboembolic disease (including pulmonary embolism and/or deep vein thrombosis) and (vi) all-cause mortality.
Two additional endpoints of interest in COVID-19 patients, secondary endpoints, were also assessed: pneumonia, and acute kidney injury (defined as a 50% in creatinine compared to chronic levels). All other variables, baselines and blood test results were compared across the three ethnic groups.
Statistical analysis
Descriptive data are presented as rates and median and inter-quartile. Parametric or the equivalent non-parametric tests (Chi-square, ANOVA or Kruskal-Wallis) were used where appropriate for comparisons among groups. Cox regression analysis was used to assess the role of ethnicity as a predictor of all-cause mortality. Binary logistic regression was used for all remaining endpoints. Adjustment was performed for baseline differences: age, hypertension, type 2 diabetes mellitus, body mass index (BMI), eGFR, use of immunosuppression, chronic (and on admission) use of non-steroidal anti-inflammatory drugs (NSAIDs), using Method Enter. Caucasian ethnicity was used as the comparator. Results with P<0.05 were considered as significant. PASW Statistics (SPSS Inc, Chicago, IL) version 18.0 was used for statistical analysis.
Results
Ethnicity, risk factors and baselines
The median age of our study population was 70 (57-82) years, with patients of Caucasian ethnicity [75 (62-84)] years being older than Asian [63 (53-76)] years and Afro-Caribbean [61 (53-79)] years ethnicity patients (P<0.001), (Table 1). One hundred and eighteen (118) patients out of 613 patients were of Afro-Caribbean ethnicity and these were more likely to have be diabetes (P<0.001), and had higher BMI (P=0.036) as compared to Caucasian and Asian ethnicity patients. Caucasian ethnicity patients (41 out of 292) were less likely to have hypertension (P=0.038). Comparisons across the 3 groups for known risk factors of cardiovascular/pulmonary and kidney disease are presented in Table 1.
Table 1.
Demographic and clinical characteristics of the study population
| All (n=613) | Caucasian (n=292) | Asian (n=203) | Afro-Caribbean (n=118) | P | |
|---|---|---|---|---|---|
| Demographics & Risk Factors | |||||
| Age | 70 (57-82) | 75 (62-84) | 63 (53-76) | 61 (53-79) | <0.001 |
| Men | 60.0% (68) | 59.2% (17) | 62.1% (126) | 58.5% (69) | 0.761 |
| BMI | 26.4 (23.5-30.6) | 26.0 (22.7-29.7) | 26.4 (23.7-30.5) | 27.9 (24.2-32.6) | 0.036 |
| Hypertension | 47.0% (288) | 41.8% (122) | 50.2% (102) | 54.2% (64) | 0.038 |
| Type 2 DM | 32.5% (199) | 24.1% (70) | 38.4% (78) | 43.2% (51) | <0.001 |
| Dyslipidaemia | 38.4% (235) | 39.5% (115) | 36.5% (74) | 39.0% (46) | 0.780 |
| Current Smoker | 3.4% (21) | 4.5% (13) | 2.0% (4) | 3.4% (4) | 0.328 |
| IHD | 14.1% (86) | 15.6% (45) | 12.7% (26) | 12.7% (15) | 0.582 |
| Previous Stroke | 9.5% (58) | 9.2% (27) | 11.8% (24) | 5.9% (7) | 0.217 |
| Asthma | 11.9% (73) | 13.4% (39) | 12.3% (25) | 7.6% (9) | 0.262 |
| COPD | 11.3% (69) | 14.0% (41) | 8.9% (18) | 8.5% (10) | 0.114 |
| Medication | |||||
| ACE-i | 20.1% (123) | 19.2% (56) | 22.2% (45) | 18.6% (22) | 0.653 |
| ARB | 13.1% (80) | 12.3% (36) | 13.8% (28) | 13.6% (16) | 0.878 |
| Statin | 46.8% (286) | 46.9% (136) | 44.3% (90) | 50.8% (60) | 0.529 |
| NSAIDs | 5.2% (32) | 2.4% (7) | 7.9% (16) | 7.6% (9) | 0.011 |
| Immunossupression | 10.8% (66) | 10.3% (30) | 7.9% (16) | 16.9% (20) | 0.038 |
| Disease Presentation | |||||
| Symptom onset before admission | 6 (2-9) | 5 (2-10) | 7 (3-9) | 6 (2-10) | 0.599 |
| Symptom at onset | |||||
| Cough | 28.2% (173) | 35.3% (103) | 21.7% (44) | 22.0% (26) | <0.001 |
| Fever | 19.1% (117) | 15.4% (45) | 19.2% (39) | 28.0% (33) | |
| Both | 33.0% (202) | 27.1% (79) | 43.8% (89) | 28.8% (34) | |
| Other | 19.7% (121) | 22.3% (65) | 15.3% (31) | 21.2% (25) | |
Abbreviations: BMI: body-mass index; IHD: ischemic heart disease; DM: diabetes mellitus, ACE-I: angiotensin-converting enzyme inhibitors, ARB: angiotensin receptor blockers, NSAID: non-steroidal anti-inflammatory drugs.
We found a significantly higher use of NSAIDs in the Asian ethnicity (16 out of 203 Asian patients) as compared to the 2 other groups (P=0.011). There was no difference across the study groups in the use of ACE-I and ARBs. A significant difference was observed in the use of immunosuppression drugs with their use being higher in the Afro-Caribbean ethnicity group [16.9% (20)], as compared to the Caucasian [10.3% (30)] and to the Asian [7.9% (16)] groups, Table 1.
Symptoms of fever and cough were the most commonly reported. Fever was significantly less frequently a presenting symptom in the Caucasian group, whereas cough was less common in Afro-Caribbean patients (P<0.001).
We found that coagulation parameters on admission, including INR (P=0.015), APTT (P=0.010) and D-Dimers (P=0.032) were deranged with significant differences across the study groups as shown in Table 2. In addition, LDH were significantly higher in the Afro-Caribbean ethnicity (P=0.006). Importantly, median admission high-sensitivity troponin levels were higher for Caucasian and Afro-Caribbean individuals (P=0.002). Leukocytes and CRP as inflammatory markers measured across the study groups did not differ significantly (Table 2).
Table 2.
Admission laboratory test results, and treatment/procedures
| All (n=613) | Caucasian (n=292) | Asian (n=203) | Afro-Caribbean (n=118) | P | |
|---|---|---|---|---|---|
| Laboratory Data | |||||
| Haemoglobin (g/l) | 12.5 (11.1-13.9) | 12.7 (11.2-13.9) | 12.6 (11.0-13.9) | 12.1 (10.8-13.4) | 0.117 |
| Platelets (109/L) | 217 (164-295) | 216 (166-299) | 222 (167-304) | 208 (158-281) | 0.297 |
| Leucocytes (109/L) | 7.5 (5.5-10.5) | 7.1 (5.2-10.8) | 8.0 (5.9-10.6) | 7.3 (5.4-10.1) | 0.190 |
| Lymphocytes (109/L) | 0.9 (0.7-1.3) | 0.9 (0.6-1.3) | 0.9 (0.6-1.3) | 1.0 (0.7-1.6) | 0.056 |
| INR (ratio) | 1.1 (1.0-1.2) | 1.1 (1.1-1.2) | 1.1 (1.0-1.1) | 1.1 (1.1-1.2) | 0.015 |
| APTT (seconds) | 26.7 (24.0-29.0) | 26.0 (23.8-28.3) | 27.2 (25.0-30.0) | 27.0 (25.0-31.0) | 0.010 |
| D-Dimers (mg/mL) | 1.19 (0.56-2.48) | 1.30 (0.65-2.79) | 1.01 (0.47-1.78) | 1.25 (0.60-3.56) | 0.032 |
| CRP (mg/L) | 95 (39-180) | 88 (30-171) | 97 (50-187) | 107 (46-189) | 0.145 |
| Creatinine (umol/L) | 91 (73-126) | 90 (74-123) | 93 (72-121) | 94 (70-151) | 0.429 |
| eGFR mL/min MDRD | 69.4 (48.5-93.3) | 66.8 (47.0-87.6) | 72.1 (48.4-93.2) | 76.2 (48.9-112) | 0.030 |
| CK (unit/L) | 133 (65-409) | 117 (58-382) | 161 (69-395) | 139 (75-587) | 0.192 |
| LDH (unit/L) | 376 (273-502) | 345 (246-473) | 392 (288-502) | 428 (313-599) | 0.006 |
| NT-proBNP (pg/mL) | 632 (197-2302) | 712 (209-2885) | 516 (150-1737) | 632 (243-1516) | 0.390 |
| hs-Troponin (ng/L) | 22 (9-52) | 25 (11-57) | 13 (7-46) | 25 (9-60) | 0.002 |
| Management & Procedures | |||||
| Non-Invasive Ventilation | 15.7% (96) | 14.4% (42) | 19.0% (38) | 13.6% (16) | 0.334 |
| Mechanical Ventilation | 18.7% (114) | 13.7% (40) | 24.5% (49) | 21.2% (25) | 0.007 |
| ECMO | 0.7% (4) | 0% (0) | 0.5% (1) | 2.5% (3) | 0.014 |
| Urgent RRT | 7.8% (28) | 6.9% (13) | 5.0% (6) | 19.1% (9) | 0.003 |
| Cardiac Pacing | 0.5% (3) | 0.7% (2) | 0.5% (1) | 0% (0) | 0.667 |
| PCI | 0.2% (1) | 0% (0) | 0.5% (1) | 0% (0) | 0.364 |
Abbreviations: INR: international normalised ratio; NT-proBNP: N-terminal pro B-type natriuretic peptide; LDH: lactate dehydrogenase; CK: creatine kinase; CRP: C-Reactive protein; APTT: activated partial thromboplastin time; ECMO: Extracorporeal membrane oxygenation; RRT: renal replacement therapy; PCI: percutaneous coronary intervention.
Management and treatment during admission
Median length of hospitalization was 12 days (IQR 6-20) and it was numerically higher in Caucasians (median 13 days, IQR 8-21), but comparable to Asian (median 10, IQR 6-19) & Afro-Caribbean (median 11, IQR 6-20).
In our multi-ethnic cohort, 15.7% (96) of patients required non-invasive ventilation, 18.7% (114) of patients required mechanical ventilation and extra corporeal membrane oxygenation (ECMO) was used in 4 (0.7%) patients. Mechanical ventilation was utilized more frequently in Asian patients and ECMO on Afro-Caribbean (P=0.007 and P=0.014, respectively). Afro-Caribbean patients required urgent renal replacement therapy (RRT) more often (P=0.003).
All patients were assessed for thromboembolic risk, and preventive measures, including low-molecular weight heparin were used. Among the 80 patients who had a transthoracic echocardiogram, median LV ejection fraction was comparable: 55% (IQR 45-60) for Caucasians, 55% (IQR 48-60) for Asians and 55% (40-60) for Afro-Caribbean.
All-cause mortality and cardiovascular outcomes
Intra-hospital death was observed for 33.4% (n=201) of the sample (Table 3). On multivariate Cox regression analysis age (HR per 10 years=1.30, 95% CI 1.15-1.48, P<0.001), prior use of immunosuppression (HR=1.73, 95% CI 1.06-2.82, P=0.029), type 2 diabetes mellitus (HR=1.51, 95% CI 1.04-2.20, P=0.030), hypertension (HR=0.67, 95% CI 0.46-0.97, P=0.036) and ethnicity were significantly associated with all-cause mortality (Asian vs. Caucasian - HR=1.89, 95% CI 1.24-2.90, P=0.003; Afro-Caribbean vs. Caucasian - HR=2.03, 95% CI 1.28-3.23, P=0.003) (Table 4).
Table 3.
Clinical progress & outcomes
| All (n=613) | Caucasian (n=292) | Asian (n=203) | Afro-Caribbean (n=118) | Adjusted OR/HR | Adjusted OR/HR | |
|---|---|---|---|---|---|---|
| 95% CI | 95% CI | |||||
| Asians* | Afro-Caribbean* | |||||
| Chest pain | 17.5% (63) | 12.7% (24) | 19.8% (24) | 31.9% (15) | 1.60 | 2.09 |
| 0.86-2.98 | 1.06-4.09 | |||||
| Myocardial Infarction | 3.1% (19) | 3.1% (9) | 3.0% (6) | 3.4% (4) | 0.76 | 0.92 |
| 0.21-2.80 | 0.22-3.93 | |||||
| Myocardial Injury** | 66.1% (287) | 72.1% (137) | 56.3% (90) | 71.4% (60) | 1.12 | 2.64 |
| 0.55-2.26 | 1.10-6.35 | |||||
| Acute HF | 7.2% (44) | 5.1% (15) | 6.9% (14) | 12.7% (15) | 1.72 | 3.64 |
| 0.71-4.15 | 1.50-8.84 | |||||
| Ischaemic Stroke | 2.4% (15) | 2.1% (6) | 2.5% (5) | 3.4% (4) | 0.81 | 0.66 |
| 0.26-2.56 | 0.16-2.77 | |||||
| AF episode | 7.3% (45) | 9.9% (29) | 6.4% (13) | 2.5% (3) | 0.55 | 0.25 |
| 0.24-1.30 | 0.07-0.90 | |||||
| Ventricular Tachycardia | 0.3% (2) | 0% (0) | 1.0% (2) | 0% (0) | N/A | N/A |
| Venous Thromboembolic disease | 5.5% (34) | 3.8% (11) | 8.4% (17) | 5.1% (6) | 4.10 | 1.77 |
| 1.49-11.27 | 0.52-6.07 | |||||
| Death During Admission | 33.4% (201) | 33.2% (97) | 32.7% (65) | 35.1% (39) | 1.89 | 2.03 |
| 1.24-2.90 | 1.28-3.23 | |||||
| Pneumonia | 75.4% (460) | 69.8% (20) | 82.3% (167) | 77.6% (90) | 1.90 | 1.41 |
| 1.10-3.31 | 0.77-2.59 | |||||
| Acute Kidney Injury | 36.3% (218) | 37.4% (108) | 31.6% (62) | 41.4% (48) | 0.87 | 2.11 |
| 0.51-1.49 | 1.15-3.86 |
Abbreviations: HF: heart failure;
Caucasian Ethnicity used as reference & OR used for all comparisons, except for survival;
High sensitivity troponin ≥15 ng/L, the 99th percentile of normal;
Note: Adjustment performed for: age, hypertension, type-2 diabetes mellitus, eGFR, BMI, and use of NSAIDs and Immunosupression prior to admission.
Table 4.
Adjusted model for ethnicity as a factor for all-cause mortality
| HR | 95% CI | P | |
|---|---|---|---|
| Age (per 10 years) | 1.30 | 1.15-1.48 | <0.001 |
| Asian Ethnicity* | 1.89 | 1.23-2.91 | 0.004 |
| Afro-Caribbean Ethnicity* | 2.09 | 1.30-3.37 | 0.002 |
| Type 2 DM | 1.51 | 1.04-2.20 | 0.030 |
| Hypertension | 0.67 | 0.46-0.97 | 0.036 |
| BMI | 1.00 | 0.99-1.01 | 0.872 |
| eGFR | 1.00 | 0.99-1.00 | 0.276 |
| Immunosuppression prior to admission | 1.73 | 1.06-2.82 | 0.029 |
| NSAIDs prior to admission | 0.82 | 0.38-1.76 | 0.613 |
| Hospital B | NA | 0-3.01exp191 | 0.958 |
| Hospital C | 0.83 | 0.50-1.38 | 0.469 |
| Hospital D | 0.76 | 0.47-1.24 | 0.274 |
| Hospital E | 1.01 | 0.53-1.95 | 0.970 |
| Hospital F | 0.73 | 0.44-1.22 | 0.233 |
Abbreviations: DM: diabetes mellitus; NSAID: on-steroid anti-inflammatory drugs;
Caucasian ethnicity and Hospital A as comparators;
Cox Regression (using Method Enter) adjusting for baseline differences between the different ethnicities.
Acute HF (adjusted OR=3.64, 95% CI 1.50-8.84, P=0.004), complaints of chest pain during the admission (adjusted OR=2.09, 95% CI 1.06-4.09, P=0.032) and myocardial injury (adjusted OR=2.64, 95% CI 1.10-6.35, P=0.030) were observed more frequently in the Afro-Caribbean group (Figure 1). Conversely, new AF was diagnosed less frequently in Afro-Caribbean patients when compared to Caucasians (adjusted OR=0.25, 95% CI 0.07-0.90, P=0.034). Venous thromboembolic disease (deep vein thrombosis and/or pulmonary embolism) was more frequently observed among Asian patients (adjusted OR=4.10, 95% CI 1.49-11.27, P=0.006).
Figure 1.
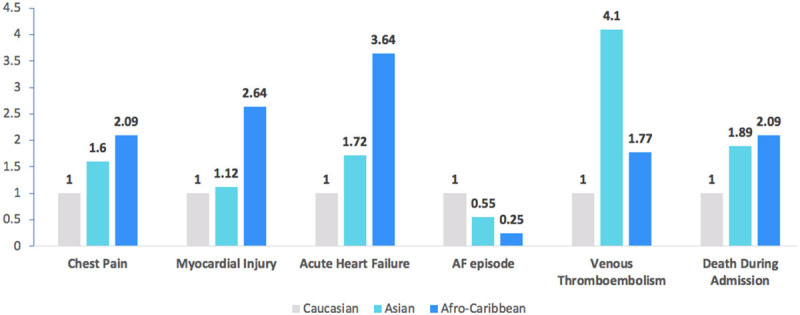
Adjusted odds ratio of cardiovascular outcomes across ethnicities (caucasian as comparator).
Non-cardiovascular covid-19 complications
A diagnosis of pneumonia was made in 460 (75.4%) patients. This complication occurred more frequently in patients of Asian ethnicity (adjusted OR=1.90, 95% CI 1.10-3.31, P=0.022). Acute kidney injury was observed in 36.3% (218) patients, and more frequently in individuals of Afro-Caribbean ethnicity (adjusted OR=2.11, 95% CI 1.15-3.86, P=0.015).
Discussion
In the present study, we found that patients presenting to six hospitals in London during the peak of the COVID-19 pandemic had slightly different clinical profiles, and different clinical trajectories, with observed complications and outcome depending on ethnicity. Caucasian patients were older, while Afro-Caribbean patients had higher prevalence of diabetes mellitus and hypertension. Asian patients more frequently presented with pneumonia and venous thromboembolic disease while Afro-Caribbean patients were more likely to present with acute kidney injury, heart failure and myocardial injury. Importantly, our multivariate Cox regression analysis showed that after adjustment both Asian and Afro-Caribbean ethnicity were associated with higher all-cause mortality as compared to Caucasian ethnicity.
Our data raise the hypothesis of different interaction of the SARS-CoV-2 virus and host depending on ethnicity, leading to differences in the prevalence of complications and observed mortality. Whether this occurs because of variation of the ACE2 receptor expression and regulation in different ethnicities [6] or other differences across ethnicities at an organ level [7,8] remains unclear.
However, our findings and study design do not allow causal inference between these complications and viral-related factors, and a completely different explanation may also possible. The observed differences in presentation/observed complication rate for the three assessed ethnicities may result from their underlying vulnerability for specific types of complications. Interestingly, a higher mortality from lower respiratory tract infections has been previously reported for Asians [9], and Afro-Caribbean individuals have been found to have higher cardiac troponin levels [10], higher incidence of HF hospitalizations [11], and acute kidney injury [11], and less frequently develop AF [12].
Nevertheless, the suggestion that a given ethnicity may experience a different disease trajectory and complication rate is of importance for improving prophylaxis (e.g. reinforcing hydration, and avoiding nephrotoxic drugs in individuals at risk of acute kidney injury) and potentially allowing earlier diagnosis and treatment in individuals at risk.
Beyond the baseline distinct clinical profile (age and risk factors), the observed differences in admission coagulation testing results, tissue and cardiac injury, suggest a potential role of these processes in explaining the observed increase in risk for Asian and Afro-Caribbean individuals which may merit further evaluation.
The intra-hospital mortality of our sample is higher than which was observed in some of the reports from Wuhan [13,14]. This can be due to the advanced age and higher prevalence of comorbidities observed in our cohort. Our data suggest that patients/individuals of Afro-Caribbean and Asian ethnicity should be considered as high-risk groups. This should be taken into account when introducing/lifting lockdown and isolation measures, as these may need to be more strict and prolonged for the individuals with higher risk.
Healthcare professionals from Asian and Afro-Caribbean ethnic groups may need more stringent precautions when treating COVID-19 patients. A recent report highlights the disproportionate rate of “Black, Asian, and minority ethnic” individuals among health care professionals who have died [15]. Urgent discussion is needed as to whether these professionals, particularly those who are greater than 50 years, and/or have COPD or any of the other recently described risk factors [16,17], should be offered highest level PPE on every occasion and have the option of remote working during the pandemic.
Limitations
The main limitation of this study is the relatively small number of patients and slight under-representation of individuals of Asian and Afro-Caribbean ethnicity. However, in light of the high mortality and rate of other events observed in this cohort there is enough statistical power to draw preliminary conclusions. Detailed data on inflammatory markers including specific interleukins such as Interleukin-6 (IL-6) and Tumor-Necrosis Factor alpha (TNF-a) are not available to support the role of inflammation. Also, routine echo-doppler and CT-pulmonary angiography were not performed in all patients. Finally, as multiple hospitals were involved, one could question the effect of treating hospital as a confounding variable due to potential differences in treatment or quality of care. However, all centers are located in very close proximity (i.e. within 15 miles) in North-East London and adhere to the same guidelines (the National Institute of Clinical Excellence guidance) making us believe that differences were unlikely. This was further confirmed on multivariate analysis.
Conclusions
Our data show that COVID-19 may have different presentations and follow different clinical trajectories depending on the ethnicity of the affected subject. Awareness of complications more likely to arise in specific ethnicities will allow a more timely diagnosis and preventive measures for patients at risk. COVID-19 patients of Afro-Caribbean and Asian ethnicity should be considered as high-risk groups with increased intra-hospital mortality. Asian individuals appear more likely to present with pneumonia and venous thromboembolic disease, and Afro-Caribbean individuals more frequently have acute kidney injury, myocardial involvement and HF. These data are of importance not only for health-resource allocation, but also for the planning/lifting of confinement and isolation measures, and optimization of staff protection at the frontline.
Disclosure of conflict of interest
None.
References
- 1.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Di Lorenzo G, Di Trolio R. Coronavirus disease (COVID-19) in Italy: analysis of risk factors and proposed remedial measures. Front Med (Lausanne) 2020;7:140. doi: 10.3389/fmed.2020.00140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yaya S, Yeboah H, Charles CH, Otu A, Labonte R. Ethnic and racial disparities in COVID-19-related deaths: counting the trees, hiding the forest. BMJ Glob Health. 2020;5:e002913. doi: 10.1136/bmjgh-2020-002913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sehra ST, Fundin S, Lavery C, Baker JF. Differences in race and other state-level characteristics and associations with mortality from COVID-19 infection. J Med Virol. 2020 doi: 10.1002/jmv.26095. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patel AP, Paranjpe MD, Kathiresan NP, Rivas MA, Khera AV. Race, socioeconomic deprivation, and hospitalization for COVID-19 in English participants of a national biobank. Int J Equity Health. 2020;19:114. doi: 10.1186/s12939-020-01227-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen J, Jiang Q, Xia X, Liu K, Yu Z, Tao W, Gong W, Han JJ. Individual variation of the SARS-CoV-2 receptor ACE2 gene expression and regulation. Aging Cell. 2020;19:e13168. doi: 10.1111/acel.13168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hou Y, Zhao J, Martin W, Kallianpur A, Chung MK, Jehi L, Sharifi N, Erzurum S, Eng C, Cheng F. New insights into genetic susceptibility of COVID-19: an ACE2 and TMPRSS2 polymorphism analysis. BMC Med. 2020;18:216. doi: 10.1186/s12916-020-01673-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ravi K. Ethnic disparities in COVID-19 mortality: are comorbidities to blame? Lancet. 2020;396:22. doi: 10.1016/S0140-6736(20)31423-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Simpson CR, Steiner MF, Cezard G, Bansal N, Fischbacher C, Douglas A, Bhopal R, Sheikh A. Ethnic variations in morbidity and mortality from lower respiratory tract infections: a retrospective cohort study. J R Soc Med. 2015;108:406–417. doi: 10.1177/0141076815588321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hackler E 3rd, Lew J, Gore MO, Ayers CR, Atzler D, Khera A, Rohatgi A, Lewis A, Neeland I, Omland T, de Lemos JA. Racial differences in cardiovascular biomarkers in the general population. J Am Heart Assoc. 2019;8:e012729. doi: 10.1161/JAHA.119.012729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lewis EF, Claggett B, Shah AM, Liu J, Shah SJ, Anand I, O’Meara E, Sweitzer NK, Rouleau JL, Fang JC, Desai AS, Retta TM, Solomon SD, Heitner JF, Stamos TD, Boineau R, Pitt B, Pfeffer MA. Racial differences in characteristics and outcomes of patients with heart failure and preserved ejection fraction in the treatment of preserved cardiac function heart failure trial. Circ Heart Fail. 2018;11:e004457. doi: 10.1161/CIRCHEARTFAILURE.117.004457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mathioudakis NN, Giles M, Yeh HC, Haywood C Jr, Greer RC, Golden SH. Racial differences in acute kidney injury of hospitalized adults with diabetes. J Diabetes Complications. 2016;30:1129–1136. doi: 10.1016/j.jdiacomp.2016.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shen AY, Contreras R, Sobnosky S, Shah AI, Ichiuji AM, Jorgensen MB, Brar SS, Chen W. Racial/ethnic differences in the prevalence of atrial fibrillation among older adults--a cross-sectional study. J Natl Med Assoc. 2010;102:906–913. doi: 10.1016/s0027-9684(15)30709-4. [DOI] [PubMed] [Google Scholar]
- 14.Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, Gong W, Liu X, Liang J, Zhao Q, Huang H, Yang B, Huang C. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5:802–810. doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, Wang H, Wan J, Wang X, Lu Z. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:1–8. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khunti K, Singh AK, Pareek M, Hanif W. Is ethnicity linked to incidence or outcomes of covid-19? BMJ. 2020;369:m1548. doi: 10.1136/bmj.m1548. [DOI] [PubMed] [Google Scholar]
- 17.Jordan RE, Adab P, Cheng KK. Covid-19: risk factors for severe disease and death. BMJ. 2020;368:m1198. doi: 10.1136/bmj.m1198. [DOI] [PubMed] [Google Scholar]


