Abstract
Introduction: Heart Failure (HF) treatment may be improved by good knowledge of the disease (Health Literacy) that, despite the well-established role on improving self-care, preventing complications and avoiding worse outcomes, has little evidence on affecting QoL of HF patients. Therefore, the objective of the present study was to evaluate the impact of Health Literacy on QoL in hospitalized HF patients. Methodology: A cross-sectional exploratory study was conducted with HF patients hospitalized at a public cardiological hospital. Health Literacy was assessed using the “Questionnaire about Heart Failure Patients’ Knowledge of Disease” and QoL using the “Minnesota Living with Heart Failure Questionnaire” (MLHFQ). The association between Health Literacy and QoL was assessed by linear regression (P<0.05). Results: 50 patients were included in the study; the mean Health Literacy score was 34.2 ± 15.1 (the majority presenting acceptable or better knowledge). The mean MLHFQ score was 73.5 ± 19.8. The one-year hospital readmission rate (β=+3.8; P=0.009) and the patients’ Health Literacy score (β=-0.4; P=0.024) or good knowledge category (β=-20.2; P=0.016) were independently associated with QoL. Conclusion: While the readmission rate was inversely associated with QoL, the better the HF knowledge the better QoL in hospitalized HF patients.
Keywords: Health literacy, knowledge, quality of life, heart failure, multidisciplinary team
Introduction
Heart failure (HF) affects 26 million people worldwide and, with 2 million new cases diagnosed each year [1-4], is considered a public health problem because of the increasing prevalence and high hospitalization and readmission rates [5,6], which impacts countries’ economies and quality of life (QoL) of its owners [4].
QoL may worsen during HF progression due to necessity of several pharmacological and non-pharmacological treatments, dietary restrictions, significant morbidity and to the occurrence of acute decompensations and hospitalizations [7,8]. In this setting, HF patients’ clinical stability is more than the pharmacological prescription, it includes improvement in adherence to treatment and in self-care behaviors [5,7], which can be enhanced through the multidisciplinary team follow-up [5] and by stimulation of health literacy [1], that “represents the cognitive and social skills which determine the motivation and ability of individuals to gain access to, understand and use information in ways which promote and maintain good health” [9].
However, few studies investigated the impact of health literacy on QoL of hospitalized HF patients [1,10-15]. Therefore, the objective of the present study is to evaluate the association between health literacy and QoL in hospitalized HF patients.
Materials and methods
Study design
This is a cross-sectional exploratory study. Patients were recruited in a public quaternary hospital, the National Institute of Cardiology (Rio de Janeiro, Brazil) (Figure 1).
Figure 1.
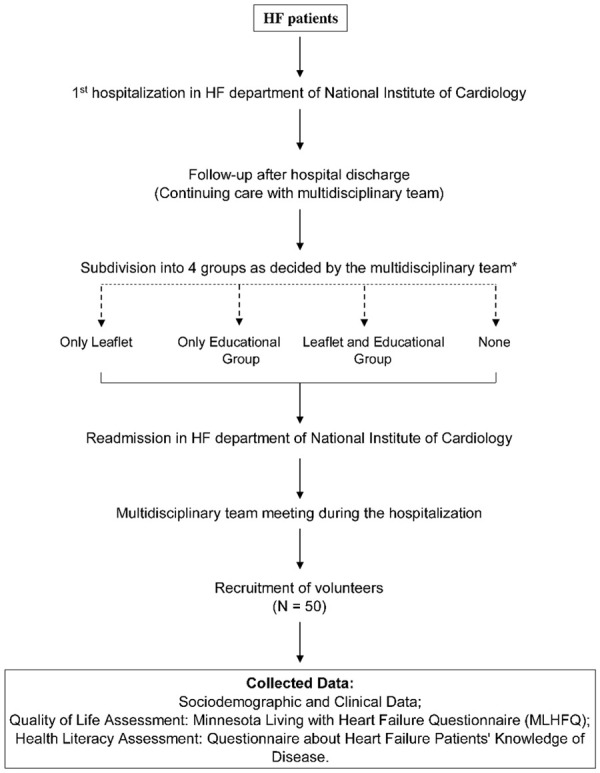
Recruitment and data collection processes. *Multidisciplinary team of HF department is responsible for allocate the HF patients in each educational strategy according to clinical decisions. HF = heart failure; MLHFQ = Minnesota Living with Heart Failure Questionary.
Inclusion criteria: patients ≥18 years old; previously diagnosed with HF; with left ventricular ejection fraction (LVEF) <45% on the last available echocardiogram; admitted (≥24 hours) in the hospital due to decompensated HF.
Exclusion criteria: illiterate patients or patients with communication difficulties; first hospitalization in the HF hospital department; patients in end-of-life care; or with acute decompensated HF in period of data collection.
After signing the informed consent, volunteers answered health literacy and QoL questionnaires. In addition, the research team collected clinical, sociodemographic, and educational strategy data.
Health literacy assessment
Patients’ knowledge about HF (health literacy) was evaluated using the “Questionnaire about heart failure patients’ knowledge of disease”, a 19 item questionnaire about ten important areas for patients’ education (HF pathophysiology; HF concept; risk factors; signs and symptoms; lifestyle; diagnosis; drugs; treatment; self-care; and physical exercise), each containing four multiple-choice alternatives scoring as follows: correct answer (3 points), incomplete answer (1 point), wrong answer (0 point) and “I do not know” (0 point). The total score ranging from 0 to 57 points and categorized as “excellent knowledge” (51-57 points), “good knowledge” (40-50 points), “acceptable knowledge” (29-39 points), “little knowledge” (17-28 points) and “insufficient knowledge” (<17 points) [4].
QoL assessment
The Minnesota Living with Heart Failure Questionnaire (MLHFQ) was used for assessing health-related QoL of volunteers. MLHFQ is composed by 21 items concerning about how the disease affects patient’s life, scoring from 0 to 105, with higher scores denote worse QoL [16-18].
Sociodemographic and clinical data assessment
Sociodemographic data (age, gender, ethnic group, occupation, level of education, religion, household income and the presence of a caregiver) was collected by interview. Clinical data (LVEF, New York Heart Association (NYHA) functional class, HF etiology, comorbidities and hemodynamic profile) was collected from the patient’s medical records.
Educational strategies
The hospital HF multidisciplinary team adopts an Institutional informative leaflet and an educational group, a HF patients and healthcare workers meeting occurring once a week, as educational strategies for HF patients after hospital discharge. The participation of volunteers in educational strategies was retrospectively assessed from medical records since their first admission in hospital HF department as follows: only leaflet, only educational group, leaflet and educational group or none.
Data analysis and statistics
Continuous variables data are expressed as mean and standard deviation (SD) or number (N) and percentage (%) and categorical variables data as number and percentage (%). The univariate association of each independent variable (age, gender, household income, ethnic group, religion, marital status, education, caregiver presence, comorbidities, HF etiology, ejection fraction, NYHA functional class, number of hospitalizations in the last year, educational strategies and health literacy) to the QoL score was assessed using linear regression. All variables presenting P<0.20 in the univariate analysis were included in the multivariate model analysis. The significance level was set as P<0.05. All analysis and statistics were performed with STATA 13 software (Stata Corp, USA).
Ethical issues
The study was in accordance of Helsinki Declaration amended in 2013 and approved by the Research Ethics Committee of the National Institute of Cardiology (CAAE: 78425617.6.00005272). All participants were informed about the aims and procedures of the study and signed an informed consent form before participation.
Results
Sociodemographic and clinical characteristics
Sociodemographic characteristics of the 50 patients included in the study are shown in Table 1. The mean age was 51.0 ± 12.8 years old and 62% were male. The most self-reported ethnic group was white (46%) and high school (34%) was the most cited education degree. The household income of the participants was approximately 389.1 US$/month. In addition, most of the patients (80%) declared Christian religion, 52% were married and 64% were actively working.
Table 1.
Sociodemographic characteristics of patients in the study
| VARIABLES | N (%) or Mean ± SD |
|---|---|
| Age (years) | 51.0 ± 12.8 |
| Gender | |
| Male | 31 (62%) |
| Female | 19 (38%) |
| Religion | |
| Atheism | 4 (8%) |
| Agnosticism | 6 (12%) |
| Catholicism | 13 (26%) |
| Protestantism | 25 (50%) |
| Spiritualism | 2 (4%) |
| Marital Status | |
| Single | 13 (26%) |
| Married | 26 (52%) |
| Divorced | 6 (12%) |
| Widowed | 5 (10%) |
| Household Income (US$) | 389.1 ± 248.8 |
| Occupation | |
| Active working | 32 (64%) |
| Retired | 18 (36%) |
| Education Degree | |
| Elementary (incomplete) | 14 (28%) |
| Elementary | 15 (30%) |
| High School | 20 (40%) |
| Graduate | 1 (2%) |
| Ethnic group | |
| White | 23 (46%) |
| Black | 20 (40%) |
| Brown | 7 (14%) |
HF = Heart Failure; SD = standard deviation.
The most common clinical characteristics (Table 2) were NYHA functional class II (58%) and idiopathic HF etiology (46%). Further, patients presented a reduced LVEF (26.7%). Further, hypertension (56%) and dyslipidemia (56%) were the most common comorbidities. The major hemodynamic profile was warm and wet (52%), the hospital readmission rate in the last year was 1.9 ± 1.8 times and the majority of the patients (88%) declared having a caregiver presence at home.
Table 2.
Clinical characteristics of patients in the study
| VARIABLES | N (%) or Mean ± SD |
|---|---|
| HF Etiology | |
| Idiopathic | 23 (46%) |
| Ischemic Heart Disease | 14 (28%) |
| Valve Dysfunction | 5 (10%) |
| Myocarditis | 3 (6%) |
| Congenital | 1 (2%) |
| Peripartum | 3 (6%) |
| Chagas Disease | 1 (2%) |
| NYHA Functional Class | |
| II | 11 (22%) |
| III | 29 (58%) |
| IV | 10 (20%) |
| Caregiver Presence | 44 (88%) |
| Comorbidities | |
| Hypertension | 28 (56%) |
| Diabetes Mellitus | 16 (32%) |
| Dyslipidemia | 28 (56%) |
| Acute Myocardial Infarction | 24 (48%) |
| Atrial Fibrillation/Flutter | 19 (36%) |
| Depression | 10 (20%) |
| LVEF (%) | 26.6 ± 7.9 |
| Hemodynamic Profile | |
| Warm and Wet | 26 (52%) |
| Warm and Dry | 16 (32%) |
| Cold and Dry | 1 (2%) |
| Cold and Wet | 7 (14%) |
| Readmission rates in the last year (frequency) | 1.9 ± 1.8 |
HF = Heart Failure; NYHA = New York Heart Association; LVEF = left ventricular ejection fraction.
QoL and educational strategies description
The questionnaires scores and the educational strategies are shown in Table 3. The mean score obtained in the questionnaire about HF patients’ knowledge of disease, used to evaluate health literacy, was 34.2 ± 15.1. The mean MLHFQ score was 73.5 ± 19.8. Almost half of the participants (48%) attended the educational group meeting and received the leaflet as educational strategy.
Table 3.
Questionnaires scores and educational strategies
| VARIABLES | N (%) or Mean ± SD |
|---|---|
| Health Literacy (total score) | 34.2 ± 15.1 |
| Health literacy (categories) | |
| Insufficient knowledge | 7 (14) |
| Little knowledge | 7 (14) |
| Acceptable knowledge | 13 (26) |
| Good knowledge | 17 (34) |
| Excellent knowledge | 6 (12) |
| MLHFQ (total score) | 73.5 ± 19.8 |
| Educational Strategies | |
| None | 7 (14%) |
| Only Leaflet | 17 (34%) |
| Only Educational Group | 2 (4%) |
| Leaflet and Educational Group | 24 (48%) |
| Frequency in the Educational Group | 0.9 ± 1.3 |
Health Literacy = Evaluated using the Questionnaire about heart failure patients’ knowledge of disease; MLHFQ = Minnesota Living with Heart Failure Questionnaire.
Association of sociodemographic, clinical and educational variables with with QoL
The Table 4 shows that NYHA functional class III is significantly associated with QoL score (β=+15.3; P=0.029), as well as the cold and wet hemodynamic profile (β=+22.6; P=0.010), the hospital readmission rate in the last year (β=+3.8; P=0.010), the patients’ health literacy total score (β=-0.4; P=0.038) and health literacy good knowledge category (β=-22.2; P=0.011).
Table 4.
Univariate regression using QoL as dependent variable
| VARIABLES | β | 95% CI | P-value |
|---|---|---|---|
| Age (years) | 0.2 | -0.2 to +0.7 | 0.282 |
| Gender (female) | 9.7 | -21.0 to +21.7 | 0.094 |
| Education Degree (Elementary incomplete) | |||
| Elementary | -4.6 | -19.6 to +10.4 | 0.543 |
| High School | +2.1 | -12.0 to +16.2 | 0.767 |
| Graduate | +15.3 | -26.6 to +57.1 | 0.466 |
| Occupation (retired) | 3.4 | -8.4 to +15.2 | 0.563 |
| Religion (atheism) | |||
| Agnosticism | 3.1 | -23.4 to +29.6 | 0.816 |
| Catholicism | -0.1 | -23.5 to +23.4 | 0.996 |
| Protestantism | -4.6 | -26.7 to +17.5 | 0.678 |
| Spiritualism | -8.2 | -43.8 to +27.3 | 0.643 |
| Household Income | -0.01 | -0.03 to +0.01 | 0.288 |
| Marital Status (single) | |||
| Married | -0.3 | -14.2 to +13.5 | 0.960 |
| Widowed | -1.9 | -23.3 to +19.5 | 0.857 |
| Divorced | 7.7 | -12.3 to +27.8 | 0.442 |
| Caregiver Presence | -3.0 | -20.5 to +14.4 | 0.727 |
| Comorbidities | |||
| Hypertension | -1.7 | -13.2 to +9.7 | 0.761 |
| Diabetes Mellitus | 1.8 | -14.0 to +10.4 | 0.767 |
| Dyslipidemia | -3.7 | -15.1 to +7.7 | 0.519 |
| Acute Myocardial Infarction | 5.2 | -6.1 to +16.4 | 0.362 |
| Atrial Fibrillation | -4.0 | -15.5 to +7.8 | 0.503 |
| Depression | -6.0 | -20.1 to +8.1 | 0.399 |
| HF etiology (Idiopathic) | |||
| Ischemic Heart Disease | -0.2 | -13.8 to +13.3 | 0.970 |
| Valve Dysfunction | +14.0 | -5.8 to +33.8 | 0.161 |
| Myocarditis | -1.6 | -26.2 to +23.0 | 0.896 |
| Congenital | -24.6 | -65.5 to +16.3 | 0.232 |
| Peripartum | +14.4 | -10.2 to +39.0 | 0.245 |
| Chagas Disease | +13.4 | -27.5 to +54.3 | 0.513 |
| LVEF (%) | -0.4 | -1.1 to +0.3 | 0.233 |
| NYHA Functional Class (II) | |||
| III | +15.3 | +1.6 to +28.9 | 0.029 |
| IV | +14.5 | -2.4 to +31.3 | 0.090 |
| Hemodynamic Profile (Warm and Dry) | |||
| Warm and Wet | +3.5 | -8.4 to +15.5 | 0.556 |
| Cold and Dry | +27.1 | -11.7 to +65.9 | 0.167 |
| Cold and Wet | +22.6 | +5.6 to +39.7 | 0.010 |
| Readmission rates in the last year (frequency) | +3.8 | +0.8 to +6.8 | 0.013 |
| Educational Strategies (none) | |||
| Only Leaflet | -2.7 | -20.6 to +15.2 | 0.763 |
| Only Educational Group | -26.8 | -58.7 to +5.1 | 0.098 |
| Leaflet and Educational Group | -3.8 | -20.9 to +13.3 | 0.658 |
| Frequency in the Educational Group | -3.3 | -7.7 to +1.1 | 0.137 |
| Health Literacy (total score) | -0.4 | -0.7 to -0.1 | 0.038 |
| Health literacy (Insufficient knowledge) | |||
| Little knowledge | -5.0 | -25.0 to + 15.0 | 0.617 |
| Acceptable knowledge | -6.5 | -24.1 to + 11.0 | 0.458 |
| Good knowledge | -22.2 | -39.0 to -5.4 | 0.011 |
| Excellent knowledge | -6.0 | -26.8 to +14.9 | 0.566 |
CI = confidence interval; HF = Heart Failure; NYHA = New York Heart Association; LVEF = left ventricular ejection fraction.
Moreover, only the hospital readmission rate in the last year (β=3.9; P=0.009) and the patients’ healthy literacy total score (β=-0.4; P=0.024) and good knowledge category (β=-20.2; P=0.016) are independently associated with QoL score of HF patients even when adjusted by age and sex (Table 5).
Table 5.
Multivariate regression using quality of life as dependent variable
| Variable | Without adjustment | Adjusted by age and sex | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| β | 95% CI | P-value | β | 95% CI | P-value | |
| Readmission rate in the last year (frequency) | +3.9 | +1.0 to +6.7 | 0.009 | +3.9 | +1.1 to +6.7 | 0.007 |
| Health Literacy (total score) | -0.4 | -0.7 to -0.1 | 0.024 | -0.3 | -0.7 to +0.1 | 0.066 |
| Health literacy (Insufficient knowledge) | ||||||
| Little knowledge | -6.9 | -26.2 to +12.4 | 0.475 | -11.6 | -32.1 to +8.9 | 0.261 |
| Acceptable knowledge | -5.0 | -21.9 to +11.9 | 0.556 | -8.1 | -25.7 to +9.3 | 0.353 |
| Good knowledge | -20.2 | -36.5 to -4.0 | 0.016 | -19.4 | -36.9 to -1.9 | 0.031 |
| Excellent knowledge | -11.0 | -31.5 to +9.6 | 0.288 | -13.5 | -35.1 to +7.9 | 0.210 |
CI = confidence interval; HF = Heart Failure.
Discussion
The main finding of the present study was that good knowledge about HF, expressed by health literacy, improves QoL of hospitalized HF patients. Also, lower readmission rates were associated with better QoL levels. Health literacy is one of 20 priority areas that could transform healthcare, as defined by the Institute of Medicine (National Academy of Medicine, USA) [19]. Our results emphasize health literacy potential for improving QoL in Hf patients.
Although some studies didn’t found consistent results between health literacy and QoL in patients with atrial fibrillation [20] or type 2 diabetes and depression [21], it has been shown that among hospitalized HF patients, health literacy was positively associated with the social component of QoL [12]. In addition, a recent systematic review and meta-analysis study showed that an inadequate level of health literacy among HF patients is associated with higher risk of mortality, increased risk of hospitalizations and emergency department visits [22].
Besides, the present study also demonstrate that hospital readmission rate is inversely associated with QoL of HF patients. Prior studies did not found a significant relationship between health literacy and 30-day readmission rate [11] and between QoL and number of previous hospitalizations for chronic HF patients [10]. However, Murray and cols demonstrated that patients with adequate health literacy present lower risk for hospitalization due to HF [23], a benefit, since the hospital readmission rate is a major risk factor for HF patients death and almost 50% of all hospitalized HF patients are readmitted within 90 days after hospital discharge [24].
Also, the participants in the present study were younger (approximately 51 years old) than those presented by others descriptive [11] and cross-sectional studies [1,10]. Most of the participants were male, white and married, as prior reported [1,25], but the most common education degree presented was high school, and over half of them were actively working, what differs from sociodemographic characteristics presented by others cross-sectional studies, that demonstrated the majority of participants being retired [25] and with less than 12 years of schooling [1]. Low educational level influences health literacy, generating vulnerable groups at higher risk of hospitalization, readmission and inappropriate use of emergency care services. Moreover, satisfactory level of health literacy is an important factor on promoting HF knowledge and confidence in self-care behaviors [11], in contrast, lower health literacy level could be a major barrier for achieving successful management of chronic conditions [26].
In this study, idiopathic etiology was the most frequent cause of HF while, for the I Brazilian Registry of Heart Failure (BREATHE) and Frail Heart Failure (FRAIL-HF) studies, ischemic and hypertensive were the most prevalent HF etiologies [15,24]. Comparatively, Chagas heart disease is commonly associated with worse prognosis than hypertensive and ischemic heart disease etiology of HF [27]. Chronic comorbidities presence and number in HF patients also affect clinical outcomes and, interestingly, approximately half of hospitalized HF patients exhibit at least one or two comorbidities [10]. In the present study, hypertension and dyslipidemia were the most common comorbidities occurring in HF patients, as also reported by BREATHE and FRAIL-HF studies [15,24].
Among the four hemodynamic profiles defined according to the classification of Stevenson, the most prevalent in the participants of this study was warm and wet (commonly called profile B), associated to the presence of pulmonary congestion without signs of peripheral tissue hypoperfusion [24]. A recent study demonstrated that warm and wet was the most common profile associated with acute decompensated HF in ischemic and dilated cardiomyopathy etiology. In addition, this was the secondary profile associated with major ratio death/heart transplant, after the cold and wet profile (patients with signs of pulmonary congestion and peripheral tissue hypoperfusion, also called as profile C), associated with poor prognosis [27].
Another relevant aspect related to HF prognosis is the loss of functional capacity [24]. The NYHA functional classification is commonly used for describing severity of HF symptoms [8]. Over half of patients in the present study demonstrated NYHA functional class II, similar as reported by the FRAIL-HF study [15]. Despite NYHA functional class II and III have already been demonstrated to have an univariate inversely association with QoL among hospitalized patients with chronic HF, in a multivariate analysis it was not proven, similarly to the present study’s findings [10].
Interestingly, almost 10 years ago, the American Heart Association (AHA) published a scientific statement demonstrating low health literacy as a challenge to effective self-care. Unsatisfactory health literacy impairs patients’ understanding of the complex healthcare systems as well as acting on essential health-related information. Therefore, health literacy affect patients ability to understand instructions of medications prescription, health information, importance of treatment adherence and self-care behaviors [28]. Together, AHA and Heart Failure Society of America have recommended further investigation of the effect of health literacy on self-care [28,29]. Although despite the present research had not specifically evaluate self-care, it brought important results regarding health literacy and QoL among hospitalized HF patients.
Limitations
This was an exploratory cross-sectional study with a small sample size. Nevertheless, our research evaluated sociodemographic and economic characteristics, clinical profile, education degree, health literacy, QoL and educational strategies-commonly used in the HF service-among hospitalized HF patients. Thus, it is necessary consider all difficulties of having access and enrolling inpatients in a research during in-hospital period. Although cross-sectional research cannot infer causality about the effect of educational strategies on QoL and health literacy, this study evaluates different educational strategies among hospitalized HF patients, which could be the basis for future clinical trials.
Conclusion
The main finding of the present study was that good levels of health literacy are associated with better levels of QoL in hospitalized HF patients. Additionally, higher hospital readmission rates are associated with poor QoL in those patients, which represents the impact of recurrent hospitalizations for HF. Finally, the multidisciplinary team could be a key point to improve the patients’ knowledge about their disease, their adherence to treatment and consequently their QoL.
Acknowledgements
We acknowledge the National Institute of Cardiology for the research support.
Disclosure of conflict of interest
None.
References
- 1.Jovanić M, Zdravković M, Stanisavljević D, Jović Vraneš A. Exploring the importance of health literacy for the quality of life in patients with heart failure. Int J Environ Res Public Health. 2018;15:1761. doi: 10.3390/ijerph15081761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Puggia I, Rowland TJ, Miyamoto SD, Sinagra G, Mestroni L. Chapter 1 - molecular and cellular mechanisms in heart failure. In: Jefferies JL, Chang AC, Rossano JW, Shaddy RE, Towbin JA, editors. Heart failure in the child and young adult. Boston: Academic Press; 2018. pp. 3–19. [Google Scholar]
- 3.Vasan Ramachandran S, Levy D. Defining diastolic heart failure. Circulation. 2000;101:2118–2121. doi: 10.1161/01.cir.101.17.2118. [DOI] [PubMed] [Google Scholar]
- 4.Bonin CD, Santos RZ, Ghisi GL, Vieira AM, Amboni R, Benetti M. Construction and validation of a questionnaire about heart failure patients’ knowledge of their disease. Arq Bras Cardiol. 2014;102:364–373. doi: 10.5935/abc.20140032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Linhares JC, Aliti GB, Castro RA, Rabelo ER. Prescribing and conducting non-pharmacological management of patients with decompensated heart failure admitted to a university hospital emergency. Rev Lat Am Enfermagem. 2010;18:1145–1151. doi: 10.1590/s0104-11692010000600015. [DOI] [PubMed] [Google Scholar]
- 6.Paz LFA, Medeiros CA, Martins SM, Bezerra SMMDS, Oliveira Junior W, Silva MBA. Quality of life related to health for heart failure patients. Rev Bras Enferm. 2019;72:140–146. doi: 10.1590/0034-7167-2018-0368. [DOI] [PubMed] [Google Scholar]
- 7.Inamdar AA, Inamdar AC. Heart failure: diagnosis, management and utilization. J Clin Med. 2016;5:62. doi: 10.3390/jcm5070062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Choi HM, Park MS, Youn JC. Update on heart failure management and future directions. Korean J Intern Med. 2019;34:11–43. doi: 10.3904/kjim.2018.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.WHO. World Health Organization. The WHO Health Promotion Glossary. 1998:1–36. [Google Scholar]
- 10.Zhang J, Gilmour S, Liu Y, Ota E. Effect of health literacy on quality of life among patients with chronic heart failure in China. Qual Life Res. 2020;29:453–461. doi: 10.1007/s11136-019-02332-4. [DOI] [PubMed] [Google Scholar]
- 11.Dennison CR, McEntee ML, Samuel L, Johnson BJ, Rotman S, Kielty A, Russell SD. Adequate health literacy is associated with higher heart failure knowledge and self-care confidence in hospitalized patients. J Cardiovasc Nurs. 2011;26:359–367. doi: 10.1097/JCN.0b013e3181f16f88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tung HH, Lu TM, Chen LK, Liang SY, Wu SF, Chu KH. Health literacy impact on elderly patients with heart failure in Taiwan. J Clin Gerontol Geriatr. 2014;5:72–76. [Google Scholar]
- 13.Meyers AG, Salanitro A, Wallston KA, Cawthon C, Vasilevskis EE, Goggins KM, Davis CM, Rothman RL, Castel LD, Donato KM, Schnelle JF, Bell SP, Schildcrout JS, Osborn CY, Harrell FE, Kripalani S. Determinants of health after hospital discharge: rationale and design of the vanderbilt inpatient cohort study (VICS) BMC Health Serv Res. 2014;14:10. doi: 10.1186/1472-6963-14-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schnipper JL, Roumie CL, Cawthon C, Businger A, Dalal AK, Mugalla I, Eden S, Jacobson TA, Rask KJ, Vaccarino V, Gandhi TK, Bates DW, Johnson DC, Labonville S, Gregory D, Kripalani S PILL-CVD Study Group. Rationale and design of the Pharmacist Intervention for Low Literacy in Cardiovascular Disease (PILL-CVD) study. Cir Cardiovasc Qual Outcomes. 2010;3:212–219. doi: 10.1161/CIRCOUTCOMES.109.921833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vidán MT, Sánchez E, Fernández-Avilés F, Serra-Rexach JA, Ortiz J, Bueno H. FRAIL-HF, a study to evaluate the clinical complexity of heart failure in nondependent older patients: rationale, methods and baseline characteristics. Clin Cardiol. 2014;37:725–732. doi: 10.1002/clc.22345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carvalho VO, Guimarães GV, Carrara D, Bacal F, Bocchi EA. Validation of the portuguese version of the minnesota living with heart failure questionnaire. Arq Bras Cardiol. 2009;93:39–44. doi: 10.1590/s0066-782x2009000700008. [DOI] [PubMed] [Google Scholar]
- 17.Bilbao A, Escobar A, García-Perez L, Navarro G, Quirós R. The Minnesota living with heart failure questionnaire: comparison of different factor structures. Health Qual Life Outcomes. 2016;14:23. doi: 10.1186/s12955-016-0425-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hsu TW, Chang HC, Huang CH, Chou MC, Yu YT, Lin LY. Identifying cut-off scores for interpretation of the heart failure impact questionnaire. Nurs Open. 2018;5:575–582. doi: 10.1002/nop2.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nielsen-Bohlman L, Panzer AM, Kindig DA, editors. Institute of Medicine Committee on Health L. Health Literacy: A Prescription to End Confusion. Washington (DC): National Academies Press (US) Copyright 2004 by the National Academy of Sciences; 2004. All rights reserved. [PubMed] [Google Scholar]
- 20.Montbleau KE, King D, Henault L, Magnani JW. Health literacy, health-related quality of life, and atrial fbrillation. Cogent Med. 2017;4:1412121. doi: 10.1080/2331205X.2017.1412121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Al Sayah F, Majumdar SR, Johnson JA. Association of inadequate health literacy with health outcomes in patients with type 2 diabetes and depression: secondary analysis of a controlled trial. Can J Diabetes. 2015;39:259–265. doi: 10.1016/j.jcjd.2014.11.005. [DOI] [PubMed] [Google Scholar]
- 22.Fabbri M, Murad MH, Wennberg AM, Turcano P, Erwin PJ, Alahdab F, Berti A, Manemann SM, Yost KJ, Finney Rutten LJ, Roger VL. Health literacy and outcomes among patients with heart failure: a systematic review and meta-analysis. JACC Heart Fail. 2020;8:451–460. doi: 10.1016/j.jchf.2019.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Murray MD, Tu W, Wu J, Morrow D, Smith F, Brater DC. Factors associated with exacerbation of heart failure include treatment adherence and health literacy skills. Clin Pharmacol Ther. 2009;85:651–658. doi: 10.1038/clpt.2009.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Albuquerque DC, Neto JD, Bacal F, Rohde LE, Bernardez-Pereira S, Berwanger O, Almeida DR Investigadores Estudo BREATHE. I Brazilian registry of heart failure - clinical aspects, care quality and hospitalization outcomes. Arq Bras Cardiol. 2015;104:433–442. doi: 10.5935/abc.20150031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen AM, Yehle KS, Plake KS, Murawski MM, Mason HL. Health literacy and self-care of patients with heart failure. J Cardiovasc Nurs. 2011;26:446–451. doi: 10.1097/JCN.0b013e31820598d4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kim MT, Kim KB, Ko J, Murry N, Xie B, Radhakrishnan K, Han HR. Health literacy and outcomes of a community-based self-help intervention: a case of korean americans with type 2 diabetes. Nurs Res. 2020;69:210–218. doi: 10.1097/NNR.0000000000000409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Terhoch CB, Moreira HF, Ayub-Ferreira SM, Conceição-Souza GE, Salemi VMC, Chizzola PR, Oliveira MT Jr, Lage SHG, Bocchi EA, Issa VS. Clinical findings and prognosis of patients hospitalized for acute decompensated heart failure: analysis of the influence of chagas etiology and ventricular function. PLoS Negl Trop Dis. 2018;12:e0006207. doi: 10.1371/journal.pntd.0006207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Riegel B, Moser DK, Anker SD, Appel LJ, Dunbar SB, Grady KL, Gurvitz MZ, Havranek EP, Lee CS, Lindenfeld J, Peterson PN, Pressler SJ, Schocken DD, Whellan DJ. State of the science: promoting self-care in persons with heart failure: a scientific statement from the American Heart Association. Circulation. 2009;120:1141–1163. doi: 10.1161/CIRCULATIONAHA.109.192628. [DOI] [PubMed] [Google Scholar]
- 29.Evangelista LS, Rasmusson KD, Laramee AS, Barr J, Ammon SE, Dunbar S, Ziesche S, Patterson JH, Yancy CW. Health literacy and the patient with heart failure--implications for patient care and research: a consensus statement of the heart failure society of America. J Card Fail. 2010;16:9–16. doi: 10.1016/j.cardfail.2009.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]


