Abstract
Background: A femur fracture is accounted for as one of the most common fractures in the population. The femoral neck has had an angle with the longitudinal axis of the bone shaft, which is defined as neck- shaft angle (NSA). Regional epidemiologic information about NSA might be useful for orthopedic surgeons. In the present study, we aimed conduct a comparative study of NSA in patients with femoral neck or intertrochanteric fractures in Rasht, Iran. Methods: The study population consisted of all patients with hip fractures. Patients with femoral fractures (neck and intertrochanteric) were examined by an emergency medicine specialist at the time of admission. An Anterior-Posterior X-ray image was taken at the time of admission. Patients NSA was measured by expert orthopedic surgeons and was compared between patients. Results: In the present study, we evaluated the data of 80 patients with femoral fractures and 40 healthy individuals as control group. Patients were divided into two groups of femoral neck fractures (40 patients) and intertrochanteric fractures (40 patients). Analysis of the NSA showed no significant differences between the NSA of patients with neck and intertrochanteric fractures and also control group (P>0.05). Our data showed that the mean NSA in patients with femoral neck fractures were 131.04±3.7° degrees while the NSA of patients with intertrochanteric fractures were 132.07±4.1°. The NSA of controls were also 132.8±6.9°. We also found no significant differences between the NSA of different age groups or between male and female patients. Conclusion: The results of this study showed that no significant differences could be indicated between NSA of healthy subjects and patients with femoral fractures. We believe that paradoxical results of former reports could be due to population and regional factors.
Keywords: Femur fracture, femoral neck, intertrochanteric fractures, neck- shaft angle, Iran ethnicity
Introduction
Femur fracture is accounted as one of the most common fractures among elderly individuals [1]. Previous reports show that the prevalence of femur fractures are rising in populations due to increased quality of life and life expectancy and increase in population of adolescents [2,3]. Femur fractures are mainly divided into intertrochanteric and femur neck fractures. Based on clinical data, almost 20% of performed surgeries by orthopedists are due to femur fractures and almost 50% of femur fractures are femur neck fractures [4,5]. It has been anticipated that with increased life expectancy, the number of femur neck fractures would rise from 1.66 million in 1990 to 6.26 million in 2050 [6,7]. Morbidities and mortalities following femur fractures put a heavy burden on societies and requires a huge economic and financial resources [8,9].
Trochanteric fractures include intertrochanteric, large trochanteric, subtrochantric, and a combination of inter and subtrochanteric fractures [10]. Most epidemiological studies consider only two categories for proximal femoral fractures: the femoral neck and intertrochanteric fractures [11]. The femoral neck is located along the longitudinal axis of the bone shaft and forms an angle which is called many names such as: neck-shaft angle (NSA), collodiaphyseal angle (CDA), diaphyseal-femoral neck angle, angle of the neck of the femur, angle of inclination, cervicodiaphyseal angle and collum diaphyseal angle [12,13].
The importance of NSA is well known for femoral bone mobility in the pelvis and lateral balance control during mobility. Based on evidence, the geometry of the proximal of femur is influenced by various factors such as ethnicity, genetics and environmental conditions [14]. The normal NSA varies between 120-140 degrees. Coxa vara is defined when the NSA is less than 120 and when the angle is more than 140, it is called coxa valga [15]. The knowledge of the NSA is invaluable in the diagnosis and treatment of upper femoral fractures. One of its applications can be expressed in the design of prostheses to repair the natural shaft angle. This knowledge about the geometry of the proximal femoral region is also important in planning preoperative procedures for arthroplasty, or fracture fixations. This issue is also useful in designing suitable implants with a more accurate angle of the femoral neck. The use of implants that are smaller or larger than the size of the femur can lead to improper tension in the soft tissue and more stress on joints such as the patellofemoral [16].
As mentioned, femoral fractures put heavy socio-economic burdens in both developing and developed countries. As a result, evaluation of NSA and type of femoral fracture in the Iranian population, especially in different regions can provide an appropriate knowledge in designing more profitable and accurate prosthesis and bring better therapeutic results. Furthermore, regional epidemiologic information about NSA might be useful for orthopedic surgeons. Previous studies conducted in different countries about the evaluation of NSA in different races have yielded variable results [17,18]. Therefore, here in the present study, we aimed conduct a comparative study of NSA in patients with femoral neck or intertrochanteric fractures in Rasht, Iran.
Methods and material
Study design
This cross sectional study was performed in 2018-2019 in Poursina hospital, Rasht, Iran. The study population consisted of all patients with hip fractures (femoral neck and intertrochanteric fractures) with the mechanism of falling down from the surface. The current study was approved by the Ethical committee of Guilan University of Medical Sciences. Patient’s written informed consents were also taken from each patient.
Inclusion and exclusion criteria
Our inclusion criteria were: patients older than 50 years, hip fractures following falling from the surface. The exclusion criteria were: congenital pelvic anomaly on the same or opposite fracture side, having a history of pelvic fracture on the same or opposite side, a history of previous surgery on the femur or hip, having a hip prosthesis, diseases such as renal failure, hyperparathyroidism, rheumatoid arthritis, Paget’s disease and bone malignancies, prolonged immobility, other hip fractures except for femoral and intertrochanteric neck or fractures with a different mechanism of falling from the surface. We also included 40 normal individuals as control group.
Measuring tools
All patients were examined by an emergency medicine specialist at the time of admission. An Anterior-Posterior X-ray image was taken at the time of admission. Diagnosis of femoral neck or intertrochanteric fractures was made using X-ray images. A total number of 80 patients entered our study. A medical student collected the demographic data of patients.
NSA measurements
The method of measuring the NSA in this study was as follows: The neck axis was drawn by measuring two points, one in the center of the head and the other at the end of the middle part of the narrowest part in the neck (highest pressure in the neck). The two points were then connected, showing the axis of the neck. The shaft axis was determined by considering two midpoints, one at the upper end in the shaft and the other at the middle of the shaft. The two points connected and extend at the upper end of the same line. We used a goniometer modality for measuring the NSA of patients. It should also be noted that all measurements were performed by an expert orthopedic surgeon. NSA was also measured in all control cases in order to compare with patients.
Statistical analysis
Data were collected and analyzed using SPSS software version 24 (SPSS 24.0, SPSS JAPAN, Tokyo, Japan). Quantitative variables with normal distribution were described with mean and standard deviation, quantitative variables with abnormal distribution of mean and mid-quarter amplitude and for qualitative variables, number and percentage were used. The normal distribution of the quantitative study variable in the subgroups was measured using the Shapiro-Wilk test. To compare the NSA in femoral and intertrochanteric neck fractures, independent t-test or non-parametric Mann-Whitney test (abnormal distribution) and for qualitative variable of Chi-square test or Fisher’s exact test was used. Logistic test was also used to relate the type of fracture to the NSA by adjusting the effect of other variables. The level of statistical significance of the tests was considered P<0.05.
Results
Study population
In the present study, we evaluated the data of 80 patients with hip fractures with the mean age of 68.2±10.7 ranging from 50 to 95 years. 40 healthy individuals were also included as control group with the mean age of 67.3±12.1 years. Data of patients were divided into two groups of femoral neck fractures (40 patients) and intertrochanteric fractures (40 patients).
Demographic data
Mean age of patients with femoral neck fractures was 67.9±9.3 and the mean age of patients with intertrochanteric fractures was 68.4±12.9 years. There were no significant differences between three groups regarding age and sex (P>0.05). The age and sex distribution of patients are summarized in Table 1 and Figure 1.
Table 1.
Age and sex distributions in patients
| Variable | Range | Femoral neck fracture | intertrochanteric fracture | Controls | p-value | |||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||
| Frequency | Percent | Frequency | Percent | Frequency | Percent | |||
| Age (years) | 50-60 | 9 | 22.5 | 12 | 30 | 15 | 37.5 | 0.361* |
| 60-70 | 13 | 32.5 | 12 | 30 | 10 | 25 | ||
| 70-80 | 14 | 35 | 7 | 17.5 | 9 | 22.5 | ||
| ≥80 | 4 | 10 | 9 | 22.5 | 6 | 15 | ||
| Sex | Male | 20 | 50 | 19 | 47.5 | 13 | 32.5 | 0.232** |
| Female | 20 | 50 | 21 | 52.5 | 27 | 67.5 | ||
P-value using Fisher’s test;
P-value using Chi-square test.
Figure 1.
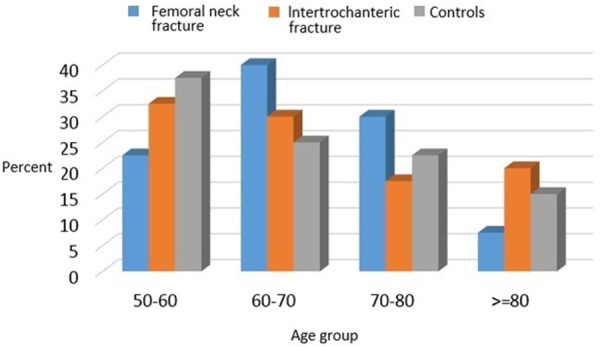
Age distribution of patients in different groups.
NSA measurements
Analysis of NSA showed no significant differences between NSA of patients with femoral neck fractures and intertrochanteric fractures and controls (P>0.05). Our data showed that the mean NSA in patients with femoral neck fractures were 131.04±3.7° while NSA of patients with intertrochanteric fractures were 132.07±4.1°. The NSA of controls were also 132.8±6.9°. We also found no significant differences between NSA of different age groups or between male and female patients (Table 2). In examining the relationship between fracture types (femoral neck and intertrochanteric fracture) with NSA by modulating the effect of other variables, no significant results were obtained based on logistic regression test (P>0.05) (Table 3).
Table 2.
Comparison of NSA based on different age and sex groups
| Variable | Range | NSA | p-value | |
|---|---|---|---|---|
|
| ||||
| Mean | SD | |||
| Age | 50-60 | 132.4 | 5.7 | 0.321 |
| 60-70 | 131.9 | 4.6 | ||
| 70-80 | 130.2 | 3.7 | ||
| ≥80 | 133.9 | 6.1 | ||
| Sex | Male | 131.7 | 4.2 | 0.620 |
| Female | 131.2 | 3.5 | ||
Table 3.
Relationship between fracture types with NSA by modulating the effect of other variables
| Variable | Beta coefficient | Standard Deviation (S.D) | 95% confidence interval (OR) (min-max) | T | p-value | |
|---|---|---|---|---|---|---|
| Groups | Intertrochanteric | -1.38 | 1.176 | -3.715, 0.946 | -1.177 | 0.470 |
| Femoral neck fracture | -0.837 | 1.158 | -3.130, 1.456 | -0.723 | ||
| Controls | Reference | |||||
| Sex | Male | -0.157 | 0.985 | -2.109, 1.795 | -0.159 | 0.874 |
| Female | Reference | |||||
| Age groups | 50-60 | -1.457 | 1.536 | -4.500, 1.586 | -.949 | 0.345 |
| 60-70 | -1.797 | 1.511 | -4.791, 1.197 | -1.189 | 0.237 | |
| 70-80 | -3.549 | 1.612 | -6.743, -0.355 | -2.202 | 0.03 | |
| ≥80 | Reference | |||||
Discussion
In the present study, we found no significant differences between the NSA of patients with femoral neck and intertrochanteric fractures and also control group. Besides, the mean the NSA in patients with femoral neck fractures were 131.04±3.7° while NSA of patients with intertrochanteric fractures were 132.07±4.1°. The NSA of controls were also 132.8±6.9°. We also found no significant differences between the NSA of different age groups or between males and females. There have also been some previous studies evaluating the NSA between different populations.
In a study by Panula and colleagues which was performed Finland in 2008, NSA of 428 patients with femur fractures were evaluated to evaluate the geometry of the proximal femoral region with intertrochanteric fractures and femoral neck fractures. They reported no significant differences between NSA of patients with femoral neck fractures and intertrochanteric fractures. They also showed no significant relationships between age and sex of patients and NSA [18]. Another study was conducted by Kazemi and others in 2016 on 60 patients with femur fractures. They reported that the mean NSA in patients with femoral neck fractures were 123.2±7.1° while NSA of patients with intertrochanteric fractures were 124±6.4° but no significant differences was reported between the two parameters [19]. These results are in line with the findings of our study showing no significant differences between NSA in different femoral fracture types. Another study was conducted in 2019 by Dehghan and colleagues. They evaluated the association between proximal femoral geometry and incidence of proximal femoral fractures. They evaluated 81 patients with proximal femur fracture and reported that the mean NSA among all patients was 133.71±6.33 and there were no significant differences between NSA and fracture types [20].
In another study by Gnudi and others in 2002 in Italy, proximal femur geometry was assessed to detect and distinguish femoral neck fractures from trochanteric fractures in postmenopausal women. In this study, compared to the control group, the femoral neck density was significantly lower in the fracture group, and it was also concluded that the NSA was associated with the risk of hip fracture in patients but was not independent of femoral neck bone density [21]. In another study by Tuck and colleagues in England, they showed that NSA is probably not a significant factor in prediction of hip fractures. They evaluated the relationship between NSA and fragility fracture. They showed that the mean NSA in femoral neck fractures were 129±6.1 degrees while NSA of patients with intertrochanteric fractures were 130.6±5.2 degrees [22]. These results are not in line with our findings. We indicated that no significant differences could be observed among NSA of different type of femoral fractures. We believe that such variations could be due to differences of study populations. An important point of our study was that we found no significant differences between NSA of patients with fractures and also healthy controls. This issue was indicated in some previous studies but some other studies have reported different results.
Some of the previous studies have showed that gender and bone density could influence the NSA [23,24] and suggested the development of a new pattern for design of prostheses to repair the natural shaft angle in patients with femoral fractures. On the other hand, Laxmi and others showed no significant differences between genders and NSA [25]. We believe that population and regional factors are most important affecting factors in NSA measurements. Jalali and colleagues performed a study on 260 patients in Iran in 2017. They reported that the NSA of the Iranian population is 6 to 7 degrees higher than the world average, and this angle is 2.5 degrees higher in women than men, and the average angle of this total population was 139.5 [17]. In contrast, we showed that the mean NSA in patients with femoral neck fractures were 131.04±3.7 degrees while NSA of patients with intertrochanteric fractures were 132.07±4.1 degrees which is lower than what Jalali and colleagues reported and almost similar to world average. These results also show the importance of regional and racial factors in evaluation of NSA.
The limitations of our study were: because of emergency of patients condition we did not evaluate factors such as: BMI, weight, lifestyle factors (:vitamin D deficiency, smoking, high caffeine intake, immobility, alcoholism), long-term use of drugs such as corticosteroids and genetic factors and also we were unable to measure the Bone Mineral Densitometry for samples.
Conclusion
In summary, the results of this study showed that there were no significant differences between healthy subjects and patients with femur fractures regarding NSA which could be used in terms of prosthesis selection in different regions. It should also be noted that all prostheses used in Iran are made from different ethnicity model of non-Iranians, and prosthesis companies can design a suitable model according to the results of this study and similar research in other parts of the country according to the ergonomics of Iranians. We suggest that more studies should be performed in this regard.
Disclosure of conflict of interest
None.
References
- 1.Dragomir-Daescu D, Rossman TL, Rezaei A, Carlson KD, Kallmes DF, Skinner JA, Khosla S, Amin S. Factors associated with proximal femur fracture determined in a large cadaveric cohort. Bone. 2018;116:196–202. doi: 10.1016/j.bone.2018.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lewiecki EM, Wright N, Curtis J, Siris E, Gagel RF, Saag K, Singer A, Steven P, Adler R. Hip fracture trends in the United States, 2002 to 2015. Osteoporosis Int. 2018;29:717–722. doi: 10.1007/s00198-017-4345-0. [DOI] [PubMed] [Google Scholar]
- 3.Wright NC, Blackston JW, Saag KG. Changing rates in fracture trends are temporally associated with declining testing and treatment: reality or ecologic fallacy? Curr Opin Rheumatol. 2019;31:316–320. doi: 10.1097/BOR.0000000000000596. [DOI] [PubMed] [Google Scholar]
- 4.Leonardsson O, Rolfson O, Rogmark C. The surgical approach for hemiarthroplasty does not influence patient-reported outcome: a national survey of 2118 patients with one-year follow-up. Bone Joint J. 2016;98:542–547. doi: 10.1302/0301-620X.98B4.36626. [DOI] [PubMed] [Google Scholar]
- 5.Kristensen TB, Vinje T, Havelin LI, Engesæter LB, Gjertsen JE. Posterior approach compared to direct lateral approach resulted in better patient-reported outcome after hemiarthroplasty for femoral neck fracture: 20,908 patients from the Norwegian hip fracture register. Acta Orthop. 2017;88:29–34. doi: 10.1080/17453674.2016.1250480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Starr J, Tay YKD, Shane E. Current understanding of epidemiology, pathophysiology, and management of atypical femur fractures. Curr Osteoporos Rep. 2018;16:519–529. doi: 10.1007/s11914-018-0464-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Elsoe R, Ceccotti AA, Larsen P. Population-based epidemiology and incidence of distal femur fractures. Int Orthop. 2018;42:191–196. doi: 10.1007/s00264-017-3665-1. [DOI] [PubMed] [Google Scholar]
- 8.Conway D, Albright P, Eliezer E, Haonga B, Morshed S, Shearer DW. The burden of femoral shaft fractures in Tanzania. Injury. 2019;50:1371–1375. doi: 10.1016/j.injury.2019.06.005. [DOI] [PubMed] [Google Scholar]
- 9.Lyons RF, Piggott RP, Curtin W, Murphy CG. Periprosthetic hip fractures: a review of the economic burden based on length of stay. J Orthop. 2018;15:118–121. doi: 10.1016/j.jor.2018.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gupta R, Sangwan K, Kamboj P, Punia SS, Walecha P. Unstable trochanteric fractures: the role of lateral wall reconstruction. Int Orthop. 2010;34:125–129. doi: 10.1007/s00264-009-0744-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kaplan K, Miyamoto R, Levine BR, Egol KA, Zuckerman JD. Surgical management of hip fractures: an evidence-based review of the literature. II: intertrochanteric fractures. J Am Acad Orthop Surg. 2008;16:665–673. doi: 10.5435/00124635-200811000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Doherty M, Courtney P, Doherty S, Jenkins W, Maciewicz RA, Muir K, Zhang W. Nonspherical femoral head shape (pistol grip deformity), neck shaft angle, and risk of hip osteoarthritis: a case-control study. Arthritis Rheum. 2008;58:3172–3182. doi: 10.1002/art.23939. [DOI] [PubMed] [Google Scholar]
- 13.Kim JT, Jung CH, Shen QH, Cha YH, Park CH, Yoo JI, Song HK, Jeon Y, Won YY. Mechanical effect of different implant caput-collum-diaphyseal angles on the fracture surface after fixation of an unstable intertrochanteric fracture: a finite element analysis. Asian J Surg. 2019;42:947–956. doi: 10.1016/j.asjsur.2019.01.008. [DOI] [PubMed] [Google Scholar]
- 14.Gilligan I, Chandraphak S, Mahakkanukrauh P. Femoral neck-shaft angle in humans: variation relating to climate, clothing, lifestyle, sex, age and side. J Anat. 2013;223:133–151. doi: 10.1111/joa.12073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eberl R, Singer G, Ferlic P, Weinberg AM, Hoellwarth ME. Post-traumatic coxa vara in children following screw fixation of the femoral neck. Acta Orthop. 2010;81:442–445. doi: 10.3109/17453674.2010.501744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Van Sikes C, Lai LP, Schreiber M, Mont MA, Jinnah RH, Seyler TM. Instability after total hip arthroplasty: treatment with large femoral heads vs constrained liners. J Arthroplasty. 2008;23:59–63. doi: 10.1016/j.arth.2008.06.032. [DOI] [PubMed] [Google Scholar]
- 17.Jalali Kondori B, Asadi MH, Bahadoran H, Dadseresht S. Anthropometric study of hip joint in tehran population using computed tomography scan. Anat Sci J. 2016;13:221–224. [Google Scholar]
- 18.Panula J, Sävelä M, Jaatinen P, Aarnio P, Kivelä SL. The impact of proximal femur geometry on fracture type-a comparison between cervical and trochanteric fractures with two parameters. Scand J Surg. 2008;97:266–271. doi: 10.1177/145749690809700311. [DOI] [PubMed] [Google Scholar]
- 19.Kazemi SM, Qoreishy M, Keipourfard A, Sajjadi MM, Shokraneh S. Effects of hip geometry on fracture patterns of proximal femur. Arch Bone Jt Surg. 2016;4:248. [PMC free article] [PubMed] [Google Scholar]
- 20.Dehghan M, Abdoli-Tafti A, Ahmadi A, Alavijeh S, Dehkordi F, Reyhani S. Association between proximal femoral geometry and incidence of proximal femoral fractures. Koomesh. 2019:21. [Google Scholar]
- 21.Gnudi S, Ripamonti C, Lisi L, Fini M, Giardino R, Giavaresi G. Proximal femur geometry to detect and distinguish femoral neck fractures from trochanteric fractures in postmenopausal women. Osteoporosis Int. 2002;13:69–73. doi: 10.1007/s198-002-8340-2. [DOI] [PubMed] [Google Scholar]
- 22.Tuck S, Rawlings D, Scane A, Pande I, Summers G, Woolf A, Francis R. Femoral neck shaft angle in men with fragility fractures. J Osteoporos. 2011;2011:903726. doi: 10.4061/2011/903726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Akbar W. Radiographic study of neck shaft angle in population of mardan region, khyber pukhtonkhwa-pakistan. Biomedica. 2015:31. [Google Scholar]
- 24.Adekoya-Cole TO, Akinmokun OI, Soyebi KO, Oguche OE. Femoral neck shaft angles: A radiological anthropometry study. Niger Postgrad Med J. 2016;23:17. doi: 10.4103/1117-1936.180130. [DOI] [PubMed] [Google Scholar]
- 25.Laxmi V. Study of neck-shaft angle of adult femur in relation to sex and bilateral asymmetry in population of bihar. J Med Sci Clin Res. 2016;6:1124–1127. [Google Scholar]


