Abstract
We describe a safe technique for controlled deflation of pneumoperitoneum to facilitate safe laparoscopic surgery in the coronavirus disease 2019 (COVID‐19) era.
Introduction
The worldwide emergence of coronavirus disease 2019 (COVID‐19) has led to an increased awareness of occupational hazards in health care, in particular, the increased exposure and associated risk of COVID‐19 transmission in the operating theatre environment. The presence of aerosolized droplets during open and laparoscopic surgery has been reported, with a presumed increased risk of transmissible infection. 1 , 2 , 3 The exact transmission risk of COVID‐19 during laparoscopic surgery is not known. 1 Despite this, risk minimization strategies are important to help reduce the risk to operating room staff. We describe a safe technique for controlled deflation of pneumoperitoneum to facilitate safe laparoscopic surgery in the COVID‐19 era.
Over the years, there have been many who have questioned the safety of uncontained surgical smoke, with several studies demonstrating potentially harmful chemicals, including carcinogenic compounds. 2 There are reported, although rare, rates of disease transmission from surgical smoke. This has most widely been reported with human papilloma virus transmission during anogenital surgery. 3 The contents of surgical smoke are mostly water vapour with particulate matter containing the carcinogenic and potentially biologically active components. 4
Deflation of pneumoperitoneum at the completion of a laparoscopic procedure is an important step; however, it also provides an opportunity of increased pollution risk. Complete deflation of the abdomen results in reduced intra‐abdominal pressure, reduced post‐operative shoulder pain and assists fascial and skin closure. 5 Uncontrolled deflation of pneumoperitoneum, by removal of access ports or opening of the gas taps, results in rapid release of intraperitoneal air into the operating room. An appropriate method of containment is recommended to reduce contamination of the operating room.
Technique
Basic laparoscopic equipment including laparoscope, light source and suction cannula with wall suction is required. Upon completion of laparoscopic procedure or at time pneumoperitoneum deflation, the below steps for controlled deflation can be followed.
Step 1: insert suction cannula
The standard laparoscopic suction cannula is inserted via a laparoscopic port.
Step 2: withdraw all laparoscopic ports into the abdominal wall layer
All ports are partially removed such that the port tips are within the layers of the abdominal wall, thereby maintaining the pneumoperitoneum with laparoscope and suction catheter within the peritoneal cavity.
Step 3: stop gas insufflation and aspirate pneumoperitoneum under vision and then all ports are completely removed, including laparoscope and suction catheter
All laparoscopic access port taps are closed, and carbon dioxide insufflation is stopped. Whilst maintaining a view of the peritoneal cavity, the suction cannula is used to evacuate the pneumoperitoneum. Once deflated, the camera, suction catheter and all ports are removed. Routine closure of the fascia and skin is performed, and dressings are applied.
The technique can be used in conjunction with a variety of measures used in operating theatre to reduce the risk of transmission and reduce the operating theatre pollution. The method of controlled pneumoperitoneal deflation described is a simple and safe method to prevent release of surgical and potentially transmissible particulate matter into the operating room environment. The technique, although simple, allows the surgeon to evacuate intra‐abdominal gas under vision and protecting visceral and peritoneal structures. The technique utilized common laparoscopic equipment that is routinely used in many centres, thereby reducing the additional cost and financial impact of specialized smoke‐regulating systems. In addition, the technique is versatile and can be adapted for use in other closed cavity, video‐assisted surgery (Fig. 1).
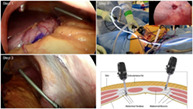
Fig 1.

Laparoscopic pneumoperitoneum deflation technique steps.
Author Contributions
Benjamin Birch: Conceptualization; data curation; formal analysis; methodology; project administration; resources; visualization; writing‐original draft; writing‐review and editing. Yuchen Luo: Data curation; formal analysis; project administration; resources; software; visualization; writing‐review and editing. Arun Dhir: Conceptualization; methodology; project administration; resources; supervision; writing‐review and editing.
Supporting information
Appendix S1. Online version.
Video S1. Laparoscopic Surgery: Reducing risk of droplet infection at Laparoscopic Surgery in the COVID Era.
References
- 1. Alp E, Bijl D, Bleichrodt RP, Hansson B, Voss A. Surgical smoke and infection control. J. Hosp. Infect. 2006; 62: 1–5. [DOI] [PubMed] [Google Scholar]
- 2. Kwak HD, Kim SH, Seo YS et al. Detecting hepatitis B virus in surgical smoke emitted during laparoscopic surgery. Occup. Environ. Med. 2016; 73: 857–63. [DOI] [PubMed] [Google Scholar]
- 3. Gloster HM, Roenigk RK. Risk of acquiring human papillomavirus from the plume produced by the carbon dioxide laser in the treatment of warts. J. Am. Acad. Dermatol. 1994; 32: 436–41. [DOI] [PubMed] [Google Scholar]
- 4. Bigony L. Risks associated with exposure to surgical smoke plume: a review of the literature. AORN J. 2007; 86: 1013–20. [DOI] [PubMed] [Google Scholar]
- 5. Phelps P, Cakmakkaya OS, Apfel CC, Radke OC. A simple clinical maneuver to reduce laparoscopy‐induced shoulder pain: a randomized control trial. Obstet. Gynecol. 2008; 111: 1155–60. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Online version.
Video S1. Laparoscopic Surgery: Reducing risk of droplet infection at Laparoscopic Surgery in the COVID Era.


