Graphical Abstract
This study used a national administrative database to estimate perioperative SARS-CoV-2 infection risk, and associated mortality, relative to nosocomial transmission rates. The impact of nosocomial transmission was greatest after major emergency surgery, whereas laparoscopic surgery may be protective owing to reduced duration of hospital stay. Procedure-specific risk estimates are provided to facilitate surgical decision-making and informed consent.
Graphical Abstract.

Estimated risks
Introduction
The SARS-CoV-2 pandemic represents a critical challenge to the safe delivery of surgical care. Early data highlighted an alarmingly high risk of postoperative death among patients undergoing surgery during the incubation period of COVID-19, with 44·1 per cent admitted to intensive care for progressive organ dysfunction and an overall mortality rate of 20·5 per cent1. This high mortality risk has now been confirmed in a large multicentre collaborative study2, with an overall 30-day mortality rate of 23·8 per cent. However, emergency surgical presentations continue despite the pandemic, while many authors have highlighted the importance of mitigating the impact of the pandemic on provision of timely and safe urgent elective and cancer surgery3–9. This has led to difficulty with respect to clinical decision-making and informed consent for surgery in both the emergency and elective contexts.
Minimization of nosocomial transmission is critical to the safe delivery of surgical care. SARS-CoV-2 is a particularly virulent pathogen with prolonged viral shedding10, aerosol transmission and prolonged detection on environmental surfaces11, and asymptomatic or minimally symptomatic carriage12,13, posing major challenges in terms of hospital infection prevention and control.
The aim of the present study was to use national administrative data (National Quality Assurance Improvement System (NQAIS) data set) to estimate perioperative SARS-CoV-2 infection and mortality risk, relative to nosocomial transmission rates. This will allow effective surgical decision-making and informed consent. A second aim was to highlight the impact of procedure-specific factors, such as complexity, acuity, operative subspecialty and surgical access, on the risk of postoperative SARS-CoV-2 infection and mortality.
Methods
The aim was to estimate the impact of a range of potential nosocomial transmission rates, and length of hospital stay (LOS) on the risk of postoperative SARS-CoV-2 infection. To achieve this, pooled estimates for 30-day mortality according to nosocomial transmission rates were calculated as the product of the cumulative nosocomial transmission risk and postoperative mortality rates derived from the COVIDSurg Collaborative Study2. These definitions have been designed as easily adaptable to mature morbidity and mortality rates as they become available later in the pandemic.
National Quality Assurance Improvement System data
Data were retrieved from the NQAIS for all general and vascular surgery admissions from October 2018 to September 2019. Patients undergoing a surgical procedure classified as general, colorectal, hepatobiliary (HPB), upper gastrointestinal (GI), breast, endocrine or vascular surgery were included. Endoscopic procedures and those commonly performed at the beside or in interventional radiology were excluded. All operations with a mean hospital stay of less than 2 days were excluded from the analysis.
Definitions
The nosocomial transmission rate was defined as the overall new hospital-level incidence of SARS-CoV-2 detection per 7 inpatient days. The nosocomial transmission risk was defined as:
where n is number of susceptible individuals (7-day mean number of inpatients) in the group and x is the number of nosocomial SARS-CoV-2 cases per 7 inpatient days. The cumulative nosocomial transmission risk was calculated as:
Procedure-specific nosocomial transmission rates were generated using the mean NQAIS LOS in the weeks from October 2018 to September 2019 and the 7-day nosocomial transmission rate. Included procedures were chosen to reflect the most commonly performed 95 per cent of procedures in the NQAIS database.
Statistical analysis
Data are reported as mean(s.d.) unless specified otherwise. Univariable comparisons were performed using Student's t or Mann–Whitney U tests for continuous variables. Repeated-measures one-way ANOVA with post hoc Tukey multiple comparisons testing was used to study the impact of nosocomial transmission on postoperative SARS-CoV-2 infection risk. Two-way ANOVA and mixed-effects analysis with post hoc Tukey multiple comparisons testing were used to determine the relative impact of nosocomial transmission and surgical factors with respect to perioperative SARS-CoV-2 infection and 30-day mortality. Sensitivity analyses were undertaken to assess the impact of minimally invasive surgery, including: major and complex colorectal procedures; major and complex upper GI and HPB procedures; and matched procedures performed via a laparoscopic or open approach. The threshold of significance was set at P < 0·050. Data were analysed using GraphPad Prism® version 6.0 for Windows® (GraphPad Software, San Diego, California, USA) and SPSS® version 23.0 (IBM, Armonk, New York, USA).
Results
NQAIS procedure-level data are summarized in Table S1 (supporting information). Of 122 582 surgical admissions from October 2018 to September 2019, 14 798 met the inclusion criteria, comprising 5103 elective and 9695 emergency procedures within 220 distinct procedure codes.
SARS-CoV-2 infection
Procedural complexity and emergency surgery were significantly associated with the risk of perioperative SARS-CoV-2 (both P < 0·001) (Fig. 1). Surgical subspecialty was a significant factor in terms of the risk of perioperative SARS-CoV-2 (P < 0·001), with patients undergoing colorectal, upper GI/HPB and vascular procedures at greatest risk, and a lower risk observed after breast and endocrine surgery.
Fig. 1.
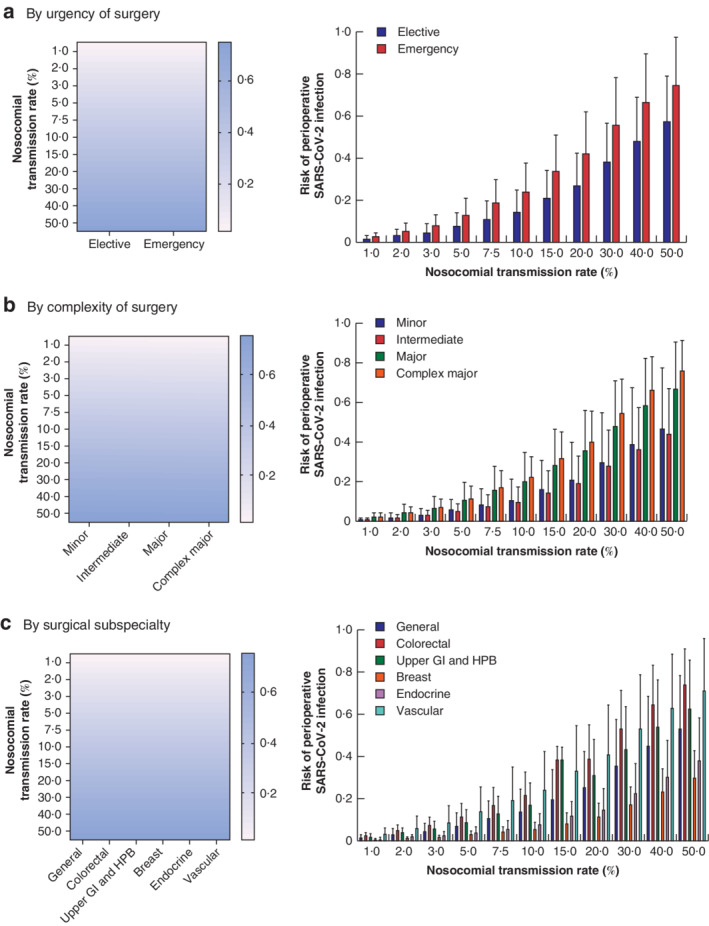
Nosocomial transmission rate and estimated postoperative SARS-CoV-2 infection risk
a By urgency of surgery, b by complexity of surgery and c by surgical subspecialty. a Emergency procedures were associated with an increased risk of nosocomial SARS-CoV-2 infection compared with elective procedures (P < 0·001), with the greatest risk at higher nosocomial transmission rates (P < 0·001 for interaction). b The risk of postoperative SARS-CoV-2 infection was significantly associated with procedural complexity, with the greatest risk following major surgery (P < 0·001 versus intermediate, P = 0·044 versus minor) and complex major surgery (P = 0·033 versus major, P < 0·001 versus intermediate, P < 0·001 versus minor). The impact of procedural complexity was greater at increased nosocomial transmission rates (P < 0·001 for interaction). c Surgical subspecialty was a significant factor in terms of risk of perioperative SARS-CoV-2 (P < 0·001). The greatest risk of SARS-CoV-2 infection was observed for general, colorectal, vascular and upper gastrointestinal (GI) and hepatobiliary (HPB) procedures. Breast and endocrine procedures were associated with a significantly reduced risk of nosocomial SARS-CoV-2 infection compared with all other subspecialties (P < 0·050) (mixed-effects analysis with post hoc Tukey multiple comparisons test).
SARS-CoV-2-related mortality
The estimated risk of postoperative death was greater after emergency compared with elective procedures (P < 0·001) (Figs S1, S2, supporting information). Subgroup analysis of major and complex major colorectal (P < 0·001) operations, and upper GI and HPB (P = 0·008) procedures, confirmed this effect. Subspecialty and increasing procedural complexity were associated with increased estimates of postoperative mortality risk adjusted for nosocomial transmission (both P < 0·001).
SARS-CoV-2 infection risk and operative approach
Operative approach was associated with estimated postoperative SARS-CoV-2 infection risk, with patients undergoing laparoscopic procedures at reduced risk (P = 0·011) (Fig. S3, supporting information). In the sensitivity analyses, laparoscopic surgery was associated with a reduced risk of perioperative SARS-CoV-2 infection among patients undergoing major or complex major upper GI/HPB procedures (P = 0·040), an effect that was most evident at higher transmission rates (P < 0·001 for interaction).
Procedure-specific risk
Procedure-specific risk estimates for nosocomial SARS-CoV-2 infection were generated for general, colorectal and upper GI/HPB procedures (Tables S2–S4, supporting information). For emergency open versus laparoscopic appendicectomy, for example, perioperative infection rates and associated mortality risk were similar in a low nosocomial transmission risk environment; however, the estimated relative increase in perioperative SARS-CoV-2 infection according to nosocomial transmission risk, and associated mortality, was greater following open compared with laparoscopic appendicectomy (both P < 0·001) (Fig. 2).
Fig. 2.
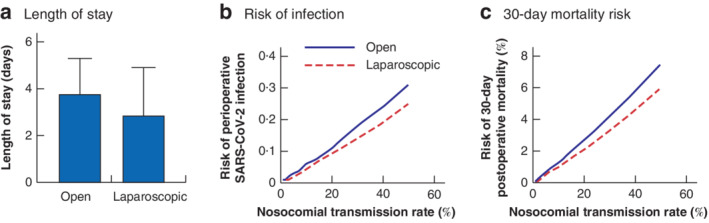
Length of hospital stay, and estimated SARS-CoV-2 and mortality risk in relation to nosocomial transmission rate after laparoscopic versus open appendicectomy in the National Quality Assurance Improvement System database
a Mean(s.d.) length of hospital stay after open (724 patients) versus laparoscopic (4896 patients) appendicectomy; P < 0·001 (Mann–Whitney U test). Risk of b postoperative SARS-CoV-2 infection and c 30-day mortality in relation to nosocomial transmission rate for open compared with laparoscopic appendicectomy; both P < 0·001 (logistic regression analysis).
Discussion
This study estimated the impact of nosocomial transmission rates on postoperative SARS-CoV-2 infection and associated mortality, using NQAIS data. It also investigated the role of factors such as complexity, acuity, operative subspecialty and surgical access in terms of postoperative SARS-CoV-2 infection risk and mortality.
Accurate and timely estimation of local nosocomial transmission rates is essential in informing decision-making around consenting and providing surgical services during the SARS-CoV-2 pandemic14. For the present study, a nationally agreed definition of the local nosocomial transmission rate was adopted, representing the 7-day hospital nosocomial infection number relative to the mean bed occupancy over the same interval. Sample estimates undertaken across academic centres in Ireland in late April and early May 2020 indicated a nosocomial transmission rate of less than 5 per cent. As such, a range of transmission rates and their relative effect on morbidity and mortality rates are provided, aiming to inform corporate decision-making with respect to resumption of scheduled inpatient operations.
A major impact of LOS on nosocomial transmission risk was found. Laparoscopic procedures overall were associated with a reduced risk of perioperative transmission and mortality. The example of laparoscopic versus open appendicectomy highlights the marginal but significantly increased risk associated with greater LOS following an open approach. These data may influence the discussion regarding the risks and potential benefits associated with minimally invasive emergency surgery in the COVID-19 era; however, further study is needed to determine the risks associated with aerosol generation during laparoscopy15, and the impact of mitigating strategies such as use of gas extraction systems16 and enhanced personal protective equipment by operating room staff4.
The strength of this study lies in the provision of overall and procedure-specific risk estimates to inform surgical planning and shared decision-making, and to facilitate real-time monitoring of nosocomial risk, promoting an adaptive strategy for the delivery of essential surgical services. The study uses real-world data to inform bespoke estimates of nosocomial infection risk, providing a useful tool for clinicians and patients, and highlights the importance of strategies to minimize LOS, which may include use of minimally invasive approaches, enhanced recovery protocols and timely discharge planning.
A number of limitations are acknowledged. The use of administrative data limits granularity at an individual-patient level. The present data represent contemporary outcomes in a national public health service, so their generalizability to private health systems internationally is uncertain. The strategy proposed here relies on access to accurate and timely testing for SARS-CoV-2 among hospital inpatients, which may limit the transferability of this approach to resource-constrained settings. The estimates presented assume a cumulative risk associated with increased inpatient exposure, but future studies may challenge this assumption. In addition, overall- and category-specific mortality estimates derived from the COVIDSurg data set were used, which may overestimate the mortality risk for minor procedures, and underestimate for higher-risk operations. Nonetheless, estimates based on operative complexity and acuity were incorporated to minimize this effect. The present analysis determined estimates of pure risk, a hypothetical risk of developing SARS-CoV-2 in the perioperative period and associated mortality over a defined time interval, without adjusting for competing mortality. This may overestimate risk compared with absolute risk estimates, particularly in high-risk operative contexts or those with prolonged LOS17.
The nosocomial transmission rate is an important determinant of surgical outcome, and the impact of nosocomial transmission is greatest after major, complex major and emergency surgery, whereas laparoscopic surgery may be protective as a result of reduced LOS. The procedure-specific risk estimates provided here may facilitate surgical planning and shared decision-making, and enhance informed consent.
Supplementary Material
Appendix S1: Supporting information
Acknowledgements
The authors acknowledge the NQAIS for collaborating on this project; the National Healthcare Pricing Office, clinicians, nursing and administrative staff; and Hospital In-Patient Enquiry coders, responsible for registration and coding of NQAIS data.
Disclosure: The authors declare no conflict of interest.
References
- 1. Lei S, Jiang F, Su W, Chen C, Chen J, Mei Wet al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine 2020; 21: 100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. COVIDSurg Collaborative . Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet 2020; 396: 27–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Di Marzo F, Sartelli M, Cennamo R, Toccafondi G, Coccolini F, La Torre Get al. Recommendations for general surgery activities in a pandemic scenario (SARS-CoV-2). Br J Surg 2020; 107: 1104–1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Welsh Surgical Research Initiative (WSRI) Collaborative . Surgery during the COVID-19 pandemic: operating room suggestions from an international Delphi process. Br J Surg 2020; 107: 1450–1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cai M, Wang G, Zhang L, Gao J, Xia Z, Zhang Pet al. Performing abdominal surgery during the COVID-19 epidemic in Wuhan, China: a single-centred, retrospective, observational study. Br J Surg 2020; 107: e183–e185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cano-Valderrama O, Morales X, Ferrigni CJ, Martín-Antona E, Turrado V, García Aet al. Reduction in emergency surgery activity during COVID-19 pandemic in three Spanish hospitals. Br J Surg 2020; 107: e239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Chen WC, Teckie S, Somerstein G, Adair N, Potters L. Guidelines to reduce hospitalization rates for patients receiving curative-intent radiation therapy during the COVID-19 pandemic: report from a multicenter New York area institution. Adv Radiat Oncol 2020; 5: 621–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. COVIDSurg Collaborative . Global guidance for surgical care during the COVID-19 pandemic. Br J Surg 2020; 107: 1097–1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gong Y, Cao X, Mei W, Wang J, Shen L, Wang Set al. Anesthesia considerations and infection precautions for trauma and acute care cases during the COVID-19 pandemic. Anesth Analg 2020; 131: 326–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Zet al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020; 395: 1054–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BNet al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med 2020; 382: 1564–1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JXet al. Clinical characteristics of Coronavirus Disease 2019 in China. N Engl J Med 2020; 382: 1708–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Li C, Ji F, Wang L, Wang L, Hao J, Dai Met al. Asymptomatic and human-to-human transmission of SARS-CoV-2 in a 2-family cluster, Xuzhou, China. Emerg Infect Dis 2020; 26: 1626–1628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bryan AF, Milner R, Roggin KK, Angelos P, Matthews JB. Unknown unknowns: surgical consent during the COVID-19 pandemic. Ann Surg 2020; 272: e161–e162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Schwarz L, Tuech JJ. Is the use of laparoscopy in a COVID-19 epidemic free of risk? Br J Surg 2020; 107: e188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Yeo D, Kaushal S, Ahmed S. Clearing the air: an accessible system for suction and safe evacuation of pneumoperitoneum during laparoscopy in patients with COVID-19. Br J Surg 2020; 107: e200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gail MH. Twenty-five years of breast cancer risk models and their applications. J Natl Cancer Inst 2015; 107: djv042. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1: Supporting information


