Introduction
In this report, we describe the development of an outpatient severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2; known as coronavirus disease 2019 [COVID‐19]) clinical recovery program, including demographic and clinical characteristics of patients referred to programs in New York City (NYC) and Boston during the early phase of the novel coronavirus pandemic. On 13 May 2020 the United States was reported to have 1.3 million COVID‐19 cases, representing nearly one third of confirmed cases worldwide. 1 Cumulative COVID‐19‐associated hospitalization rates in the United States were approximately 68 per 100 000. 2 Both morbidity and mortality statistics from COVID‐19 are likely underestimated, as there are significant barriers to accurate tracking and reporting.
Patients who become seriously ill because of COVID‐19, whether hospitalized or not, frequently have short‐term rehabilitation needs 3 and a subset of this population have longer‐term rehabilitation needs. In response, multidisciplinary teams led by physiatrists at three different academic institutions developed clinical programs for patients recovering from COVID‐19. Here we describe a clinical quality improvement program designed to evaluate and treat the physical, cognitive, psychological, and functional sequelae following hospitalization for COVID‐19.
New York and Massachusetts were two of the states hit hardest early in the pandemic when initial infection surges occurred. On 22 May 2020 in New York there were nearly 360 000 positive cases and over 23 000 fatalities, and in Massachusetts, there were more than 90 000 confirmed cases and just over 6200 deaths. 4 , 5 The initial acute care medical response focused on managing hospitalized patients, with many requiring intensive care unit (ICU) level care and mechanical ventilation. The needs of patients surviving acute hospital stays for COVID‐19 were not clearly understood early in the course of the pandemic. However, many hospitalized patients, especially those with prolonged stays, have been found to exhibit residual pulmonary compromise, muscular deconditioning, mobility impairments, fatigue, as well as cognitive, sleep, and mood complaints. 6
There is limited guidance on how to build a clinical recovery program for patients hospitalized with COVID‐19. Nevertheless, the urgency to design and quickly implement a follow‐up program grew as exponential numbers of patients contracted the illness. There have been calls to action to provide a coordinated response for patients exhibiting persistent symptoms following COVID‐19 infection. 6 Thus, our teams worked together to design and implement clinical quality improvement programs in NYC and Boston aimed at identifying and treating the rehabilitative needs of survivors. Telehealth visits were initially used because of public health safety measures that were in place in both states. To our knowledge, this is the first report describing a cohort of U.S.‐based rehabilitation ambulatory referrals and interventions for previously hospitalized COVID‐19 patients.
Methods
Ethics
This study was conducted at Weill Cornell Medical Center (NYC1), Columbia University Medical Center (NYC2), and Spaulding Rehabilitation Hospital (Boston). This study was approved by the respective institution's quality improvement program, and thus deemed exempt from institutional review board approval. The quality improvement report followed the revised Standards for Quality Improvement Reporting Excellence (SQUIRE 2.0).
Program Description
Our teams developed a robust outpatient rehabilitation program addressing functional impairments, with focus on physical symptoms, for patients discharged following hospitalization for COVID‐19. In all institutions, patients underwent an initial physiatry evaluation via a telemedicine platform. Two of the institutions created a Home Rehabilitation Recovery Guide for patients to assist with at‐home pulmonary rehab (eg, instructions in use of an incentive spirometer, breathing exercises) and graded, phased exercise program for endurance, strength, and range of motion training. The guide also reports specific oxygenation parameters for those discharged with a pulse oximeter and use of the Borg Rate of Perceived Exertion scale to guide exercise. This guide was made available in English and Spanish and can be accessed online (see Appendix). Virtual therapy services, including physical, occupational, and speech therapy, were coordinated based on identified patient needs. Psychologist telehealth appointments were also facilitated in select cases.
NYC1 and NYC2
The primary team at both NYC centers included physiatrists, neuropsychologists, and physical therapists with a cardiopulmonary and musculoskeletal background.
At NYC1, key groups facilitating program referrals were hospitalist physicians and physician assistants, social workers, inpatient physical therapists, and medical record programming teams enabling appropriate electronic referral orders. The senior member of the physician team presented the program as a Department of Internal Medicine Grand Rounds and also provided an interview to the press to further disseminate program information.
To obtain referrals at NYC2, the rehabilitation team established connections and made discharge materials available to the lead hospitalists, chief medicine residents, care coordinators of discharging medical teams, and inpatient therapists in order to allow patients easy transition to home upon discharge. For patients identified by these care providers as having persistent rehabilitation needs, virtual physiatry visits were arranged for detailed screening and evaluation within 7 days of referral.
In both NYC programs, physician visits occurred approximately 7 days following hospital discharge and subsequently at 1‐2‐week intervals until patients had no additional rehabilitation needs. Physical therapy visits occurred two to three times per week.
Boston Location
In Boston, both physiatry generalists and specialists were involved in the development and implementation of the recovery program. The Boston program assembled following a series of discussions among clinicians, clinic managers, and case coordinators across the inpatient and outpatient sites. Initially, patients referred to the program included those recently discharged from a long‐term acute care hospital (LTACH) or inpatient rehabilitation facility (IRF) within the same hospital network. Just prior to discharge from inpatient rehabilitation, patients were scheduled for a telemedicine physiatry virtual visit in the upcoming 2 to 4 weeks. Home care and rehabilitation services were also typically arranged at the time of discharge from inpatient rehabilitation or acute care. Consequently, a second referral source included referrals through home care. A third source of referrals came from a field hospital in Boston, a temporary 1000‐bed rehabilitative field hospital.
Eligible Participants
For NYC, screening criteria for the COVID‐19 telemedicine rehabilitation program included (1) prolonged weaning of supplemental oxygen, (2) shortness of breath with basic activities of daily living (ADLs), (3) muscle weakness/fatigue with basic ADLs, or (4) continuation of therapies following an ICU or IRF stay. In Boston, criteria for participating was broader and included anyone hospitalized for COVID‐19 with ongoing physical symptoms and/or functional changes. No funding was received for any of the programs, and the majority of patients had insurance coverage. All institutions accepted major healthcare plans including private, public, and combination plans.
Telemedicine
In compliance with government‐issued physical distancing guidelines put in place to reduce contagion, routine outpatient rehabilitation services at all three academic centers were closed to in‐person visits except for urgent cases. Thus, the recovery programs were designed to initially utilize telemedicine for physician evaluations. The expansion of telemedicine reimbursement during the initial stages of the pandemic provided the means to increase access to patients. 7 Patients were assisted via support staff to help connect to the telemedicine platform, which most often included Epic, Epic‐integrated Zoom, or in rare cases of technical difficulty, another Health Insurance Portability and Accountability Act compliant platform such as Doxy.me or Doximity.
Assessments and Metrics
During the virtual visits at all institutions, physiatrists performed a comprehensive assessment of functional status, including mobility, endurance, cognition, mental health, and sleep. Data on demographics, medical and psychiatric comorbidities, and variables relating to hospitalization such as acute hospital length of stay or days on mechanical ventilation were extracted from medical records and can be seen in Table 1. The NYC and Boston teams also collaborated to assemble standardized metrics that included validated measures (Figure 1). If available, oxygen saturation was monitored at rest and following the 2‐minute step test and 30‐second sit to stand using pulse oximeters.
Table 1.
Baseline demographic and clinical data for patients hospitalized with COVID‐19
| NYC1 n = 35 | NYC2 n = 31 | Boston n = 36 | Total n = 102 | P value | |
|---|---|---|---|---|---|
| Age (y) | 56.3 (12.1) | 59.1 (12.6) | 63.1 (15.5) | 59.5 (13.7) | .11 |
| Gender, Female | 15 (42.9%) | 17 (54.8%) | 12 (33.3%) | 44 (43.1%) | .21 |
| Race | <.001 | ||||
| Asian | 7 (20%) | 1 (3.2%) | 2 (5.9%) | 10 (10%) | |
| Black | 9 (25.7%) | 3 (9.7%) | 3 (8.8%) | 15 (15%) | |
| Hispanic | 11 (31.4%) | 19 (61.3%) | 5 (14.7%) | 35 (35%) | |
| White | 8 (22.9%) | 3 (9.7%) | 22 (64.7%) | 33 (33%) | |
| Other | 0 (0%) | 5 (16.1%) | 2 (5.9%) | 7 (7%) | |
| Comorbidities | |||||
| Hypertension | 15 (42.9%) | 21 (67.7%) | 20 (55.6%) | 56 (54.9%) | .13 |
| Coronary artery disease | 6 (17.1%) | 3 (9.7%) | 5 (13.9%) | 14 (13.7%) | .68 |
| Congestive heart failure | 2 (5.7%) | 0 (0%) | 5 (13.9%) | 7 (6.9%) | .077 |
| Chronic lung disease | 9 (25.7%) | 2 (6.5%) | 5 (13.9%) | 16 (15.7%) | .093 |
| History of smoking | 8 (22.9%) | 7 (22.6%) | 13 (36.1%) | 28 (27.5%) | .35 |
| Chronic kidney disease | 3 (8.6%) | 6 (19.4%) | 6 (16.7%) | 15 (14.7%) | .43 |
| Liver disease | 1 (2.9%) | 0 (0%) | 0 (0%) | 1 (1.0%) | .38 |
| Cancer | 2 (5.7%) | 1 (3.2%) | 2 (5.6%) | 5 (4.9%) | .87 |
| Immunosuppression | 3 (8.6%) | 3 (9.7%) | 3 (8.3%) | 9 (8.8%) | .98 |
| Dementia | 1 (2.9%) | 0 (0%) | 1 (2.8%) | 2 (2.0%) | .64 |
| Stroke | 1 (2.9%) | 1 (3.2%) | 3 (8.3%) | 5 (4.9%) | .49 |
| Depression | 4 (11.4%) | 6 (16.1%) | 5 (13.9%) | 14 (13.7%) | .86 |
| Other mental health | 4 (11.4%) | 4 (12.9%) | 4 (11.4%) | 12 (11.9%) | .98 |
| Obesity | 13 (37.1%) | 17 (54.8%) | 20 (55.6%) | 50 (49%) | .22 |
| Acute hospital LOS (days) | 12.8 (10.3) | 12.6 (8.9) | 19.8 (11.4) | 15.2 (10.8) | .006 |
| ICU stay | 9 (25.7%) | 5 (16.1%) | 22 (66.7%) | 38 (37.3%) | <.001 |
| Mechanical ventilation | 9 (25.7%) | 5 (16.1%) | 22 (61.1%) | 36 (35.3%) | <.001 |
| Duration (days) | 12.8 (5.3) | 15.2 (4.0) | 15.7 (7.2) | 14.9 (6.4) | .53 |
| Discharge disposition | |||||
| Home | 31 (88.6%) | 30 (96.8%) | 1 (2.8%) | 62 (60.8%) | |
| IRF | 4 (11.4%) | 1 (3.2%) | 1 (2.8%) | 6 (5.9%) | |
| LTACH | 0 (0%) | 0 (0%) | 33 (91.7%) | 33 (32.4%) | |
| SNF | 0 (0%) | 0 (0%) | 1 (2.8%) | 1 (1.0%) | |
| Rehab LOS (days) | 6.1 (7.7) | 6 (−) | 16.9 (8.9) | 14.6 (9.6) | .008 |
| Insurance | |||||
| Commercial | 10 (28.6%) | 13 (41.9%) | 16 (44.4%) | 39 (38.2%) | |
| Medicaid | 15 (42.9%) | 10 (32.3%) | 4 (11.1%) | 29 (28.4%) | |
| Medicare | 9 (25.7%) | 7 (22.6%) | 16 (44.4%) | 32 (31.4%) | |
| Uninsured | 0 (0%) | 1 (3.2%) | 0 (0%) | 1 (1%) | |
| Other | 1 (2.9%) | 0 (0%) | 0 (0%) | 1 (1%) |
Data are presented as mean (SD) for continuous variables, and n (%) for categorical measures.
COVID‐19 = coronavirus disease 2019; ICU = intensive care unit; IRF = inpatient rehabilitation facility; LOS = length of stay; LTACH = long‐term acute care hospital; NYC1 = Weill Cornell Medical Center; NYC2 = Columbia University Medical Center; SNF = skilled nursing facility.
Figure 1.
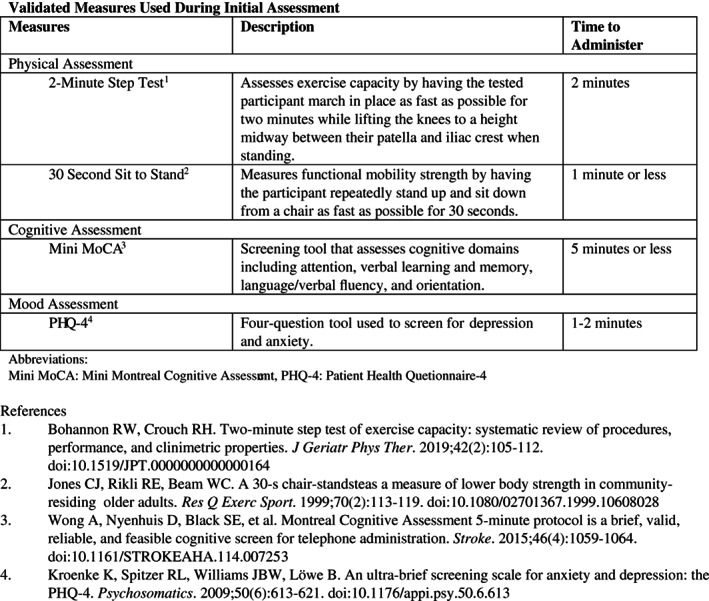
Validated measures used during initial assessment. Mini MoCA = Mini Montreal Cognitive Assessment; PHQ‐4 = Patient Health Questionnaire‐4.
Statistics
Data were analyzed using summary statistics both in total and by site for a number of variables. For quantitative variables (eg, age), analysis of variance was used to detect any differences between the sites. For categorical variables (eg, gender), the frequency of occurrence of each value and the percentage of responses within a site were reported. In addition, similarity of distribution across sites was tested by chi‐square. For each variable, one overall P value was presented as a compilation test of whether there were any differences across the three sites.
Results
As of 22 May 2020, 35 patients had been referred to NYC1, 31 to NYC2, and 36 to Boston location. The mean age of patients was 59.5 years with 43.1% female. In terms of race/ethnicity, in the combined cohorts 10% identified as Asian, 15% Black, 35% Hispanic, 33% White, and 7% Other. Racial/ethnic diversity was greater in the NYC cohorts. For instance, at NYC1, 20% of the population identified as Asian and 25.7% as Black, and at NYC2 61.3% identified as Hispanic.
The most common premorbid medical comorbidities included hypertension (54.9%) and obesity (49.0%). In total, 13.7% had a history of depression and 11.9% had a mental health illness other than depression. The comorbidities of the NYC and Boston cohorts did not significantly differ.
Average hospital length of stay (LOS) was 15.2 days, with 37.3% requiring an ICU stay and 35.3% needing mechanical ventilation (Table 1). On average, the Boston program cohort had a significantly greater acute hospital LOS—Boston location 19.8 (11.4) days, versus NYC1 12.8 (10.3) or NYC2 12.6 (8.9); P = .006. The Boston cohort also more often required an ICU stay (Boston 67% vs NYC1 26% or NYC2 16%; P < .001) and mechanical ventilation (Boston 61% vs NYC1 26% or NYC2 16%; P < .001).
Discussion
This study focused on the implementation of an ambulatory post‐COVID‐19 rehabilitation program for hospitalized patients in New York and Boston during the early months of the pandemic. Several key findings emerged: (1) teams were able to rapidly develop physiatry‐run outpatient COVID‐19 recovery clinics via telehealth to safely address rehabilitation‐related needs of patients who had become severely ill from COVID‐19, (2) institutions differed in mechanisms for patient flow and referrals to the recovery clinic, and (3) patient demographics differed among institutions. To our knowledge this is the only article published to date describing implementation of a physiatry‐led outpatient COVID‐19 recovery program.
As the number of COVID‐19‐associated hospitalizations grew, an increased burden of critical illness‐related morbidity and associated functional limitations were anticipated. Although long‐term rehabilitation needs are yet unknown, prior literature evaluating ICU hospitalization reveals that many survivors experience persistent physical, cognitive, and mental impairments. 8 Complications including critical illness myopathy, critical illness polyneuropathy, muscle atrophy, and delirium among others may contribute to rehabilitation needs. 6 Recent data also suggest a burden of COVID‐19 neurologic complications, including ischemic and hemorrhagic stroke, encephalopathy, seizure, impaired consciousness, anosmia, dysgeusia, and nerve pain. 9 The outpatient COVID‐19 recovery program was developed to address rehabilitation needs from these potential complications. In order to preserve the continuation of care following discharge home, programs sought to provide rehabilitation services while operating within physical distancing confines. Given the novelty of the SARS‐CoV‐2 pandemic, there is no one accepted model for delivery of care after discharge home.
Other interdisciplinary models of care have been proposed and employed for slightly different populations including post‐ICU survivors. 10 Existing literature describing the design of these clinics is limited. A survey of post‐ICU clinics in the United Kingdom found that half were nurse led, one third offered prenegotiated access to psychology and physical therapy, and the majority utilized a locally devised screening tool to assess functional recovery. 10 Although these clinics have shown mixed effectiveness on various outcomes, 11 prior studies demonstrate interdisciplinary post‐ICU follow‐up can identify untreated physical and psychological problems. 12 The COVID‐19 recovery program described here borrows elements from other interdisciplinary team clinic models; however, our clinics were all physiatrist led.
In terms of demographic information, the majority of the patient cohort in the NYC sample were Black/African American and Hispanic/Latino whereas the Boston cohort was predominantly White. Preliminary data from NYC suggests Black and Hispanic individuals are disproportionately affected by COVID‐19 including increased hospitalization and death rates. 13 The NYC cohort demographics may be reflective of disproportionate morbidity resulting in more rehabilitation referrals. In Boston, although Black and Hispanic individuals are also affected disproportionately, 14 recent data suggest clinically relevant hospitalization outcomes including mortality are not significantly associated with race/ethnicity. 15 It is not clear why the racial makeup of the Boston cohort is incongruent with higher infection rates among Black and Hispanic residents but may reflect a difference in access to care. Further exploration is warranted in regard to race/ethnicity, particularly as understanding of racial disparities and access to care emerge.
In total, across the three cohorts, approximately one third of patients required ICU care and mechanical ventilation. Patients seen in the Boston recovery program were more likely than NYC counterparts to have been discharged to an inpatient rehabilitation facility with the majority of these discharged from acute care to LTACH. NYC patients were more likely to be discharged directly to home without inpatient rehabilitation. Differences in utilization of Centers for Medicare & Medicaid Service's emergent expansion of acute care beds into alternative inpatient space may explain the discharge disposition discrepancy between NYC and Boston cohorts. 16 Boston operated LTACH facilities as an expansion of acute care to accommodate a surge in cases. There were also differences in program processes between sites. NYC physiatrists who developed the program were recruited to front‐line acute care units during the surge of the pandemic and established connections and a referral basis with acute care medicine teams. In contrast, the Boston team predominantly continued work within various rehabilitation settings and referrals were made between these facilities.
Limitations
The applicability of our findings to other health delivery systems is limited by the qualitative improvement design focusing on local patient populations and institutions. This study captures a relatively small number of patient experiences and does not provide data on the effectiveness of a recovery clinic intervention. The patient populations were from two major cities and their surrounding suburbs, the demographics and risk factors of which may not be comparable to other communities. This study group may not be representative of the entire post COVID‐19 population to the extent that those without insurance may experience barriers to access services in addition to previously documented disproportionate effects of COVID‐19 in lower socioeconomic populations. 13 Although both institutions were able to successfully implement multidisciplinary follow‐up clinics, the generalizability of this program may be limited in other health care systems lacking access to specialists, home care services, or telehealth platforms. Different institutions may have varying degrees of communication between acute care hospitals, rehabilitation hospitals, and outpatient clinics, which may affect recruitment of patients for clinics.
Conclusion
As numbers of individuals surviving COVID‐19 hospitalization grow, the need for rehabilitation is increasingly important. During the early part of the novel coronavirus pandemic, our teams were able to develop a clinical program to evaluate and treat patients with ongoing rehabilitation needs following hospitalization for COVID‐19. This study describes the population of COVID‐19 survivors that utilized outpatient rehab services at two metropolitan areas affected early by the pandemic and may benefit from such a program. To date, 61, 45, and 92 patients have been seen at NYC1, NYC2, and Boston sites, respectively. Further research is needed to identify the long‐term sequelae in this population and assess the benefit of rehabilitation interventions.
Supporting information
Appendix
Appendix
Acknowledgments
The authors would like to acknowledge the many clinicians, educators, and administrators involved at each site who helped to facilitate this work. No funding was received for this work.
Disclosures: Hannah K. Steere, MD ‐ no disclosures related to this work. Ginger Polich, MD ‐ no disclosures related to this work. Julie K. Silver, MD ‐ no disclosures related to this work. Dr. Silver reports participation in research funded by the Arnold P. Gold Foundation and the Binational Scientific Foundation outside the submitted work. Farah Hameed, MD ‐ no disclosures related to this work. Alfred C. Gellhorn, MD ‐ no disclosures related to this work. Joanne Borg‐Stein, MD ‐ no disclosures related to this work. Jeffrey C. Schneider, MD ‐ no disclosures related to this work. Dr. Schneider reports grants from Department of Defense, grants from Department of Health and Human Services, National Institute on Disability, Independent Living, and Rehabilitation Research, outside the submitted work.
References
- 1. Coronavirus Disease (COVID‐19) Situation Report‐114 Situation in Numbers (by WHO Region); 2020.
- 2. Virus Outpatient and Emergency Department Visits Severe Disease Public Health . Commercial and clinical laboratories outpatient influenza‐like illness network (ILINet) and National Syndromic Surveillance Program (NSSP) hospitalizations. Mortality. 2020. [Google Scholar]
- 3. Kiekens C, Boldrini P, Andreoli A, et al. Rehabilitation and respiratory management in the acute and early post‐acute phase. “Instant paper from the field” on rehabilitation answers to the COVID‐19 emergency. Eur J Phys Rehabil Med. 2020;56:323‐326. 10.23736/S1973-9087.20.06305-4. [DOI] [PubMed] [Google Scholar]
- 4. New York State Department of Health . NYSDOH COVID‐19 Tracker; 2020.
- 5. Massachusetts Department of Public Health . Public Health COVID‐19 Dashboard May 22; 2020.
- 6. Simpson R, Robinson L. Rehabilitation after critical illness in people with COVID‐19 infection. Am J Phys Med Rehabil. 2020. Jun;99(6):470‐474. 10.1097/PHM.0000000000001443. PMID: 32282359; PMCID: PMC7253039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Tenforde A, Iaccarino M, Borgstrom H, et al. Telemedicine during COVID‐19 for outpatient sports and musculoskeletal medicine physicians. PM R. 2020;12(9):926‐932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fuke R, Hifumi T, Kondo Y, et al. Early rehabilitation to prevent postintensive care syndrome in patients with critical illness: a systematic review and meta‐analysis. BMJ Open. 2018;8(5):e019998. 10.1136/BMJOPEN-2017-019998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Helms J, Kremer S, Merdji H, et al. Neurologic features in severe SARS‐CoV‐2 infection. 2020;382(23):2268‐2270. 10.1056/NEJMC2008597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Griffiths JA, Barber VS, Cuthbertson BH, Young JD. A national survey of intensive care follow‐up clinics. Anaesthesia. 2006;61(10):950‐955. 10.1111/j.1365-2044.2006.04792.x. [DOI] [PubMed] [Google Scholar]
- 11. Teixeira C, Rosa RG. Post‐intensive care outpatient clinic: is it feasible and effective? A literature review TT ‐ Ambulatório pós‐unidade de terapia intensiva: é viável e efetivo? Uma revisão da literatura. Rev Bras Ter intensiva. 2018;30(1):98‐111. 10.5935/0103-507x.20180016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Schandl AR, Brattström OR, Svensson‐Raskh A, Hellgren EM, Falkenhav MD, Sackey PV. Screening and treatment of problems after intensive care: a descriptive study of multidisciplinary follow‐up. Intensive Crit Care Nurs. 2011;27:94‐101. 10.1016/j.iccn.2011.01.006. [DOI] [PubMed] [Google Scholar]
- 13. Wadhera RK, Wadhera P, Gaba P, et al. Variation in COVID‐19 hospitalizations and deaths across New York City boroughs. JAMA. 2020;323(21):2192‐2195. 10.1001/jama.2020.7197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Racial Data On Boston Resident COVID‐19 Cases. COVID‐19 Health Inequities Task Force ‐ Boston Mayor's Office. https://www.boston.gov/departments/mayorsoffice/racial-data-boston-resident-covid-19-cases. Accessed September 1, 2020
- 15. McCarty TR, Hathorn KE, Redd WD, Rodriguez NJ, Zhou JC, Bazarbashi AN, Njie C, Wong D, Trinh Q‐D, Shen L, Stone VE, Chan WW. How do presenting symptoms and outcomes differ by race/ethnicity among hospitalized patients with covid‐19 infection? experience in massachusetts. Clinical Infectious Diseases. 2020. 10.1093/cid/ciaa1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Centers for Medicare and Medicaid Services . Long Term Care Facilities (Skilled Nursing Facilities and/or Nursing Facilities): CMS Flexibilities to Fight COVID‐19; 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix
Appendix


