Abstract
Background
Lockdown is one of the prevalent tools that are used to control the spread of COVID‐19 virus in India. Under the circumstances created during lockdown period, children are deprived from the social interaction and companionship; because of which, they are susceptible to psychiatric disorders. Therefore, in this study, efforts were to understand the impacts of lockdown on the mental status of the children of India and their specific causes.
Study Design
It is a questionnaire‐based study.
Methods
A web‐based questionnaire was prepared, and 400 parents from four districts of Punjab, India, namely, Ludhiana, Sahibzada Ajit Singh (SAS) Nagar, Sangrur and Ferozepur, were telephonically interviewed. Further, the information collected from the interviews was statistically analysed using Statistical Package for the Social Sciences (SPSS) software.
Results
Findings from this study revealed that 73.15% and 51.25% of the children were having signs of increased irritation and anger, respectively; 18.7% and 17.6% of the parents also mentioned the symptoms of depression and anxiety, respectively, among their children, which were also augmented by the changes in their diet, sleep, weight and more usage of the electronic equipment. Children (~76.3%) persistently urge to go outdoors and play with their friends; therefore, they could lag in social development. Further, observations from Pearson's correlation revealed that during lockdown, children's mental health is significantly related to the area of their house, number of children in the family, qualification of their mother and socio‐economic status of their family.
Conclusions
This study made it evident that the mental health of the children residing in Punjab, India, was compromised during the lockdown period induced by the COVID‐19 pandemic. Findings of this study may also trigger the international authorities to frame the guidelines of lockdown in the interest of mental health of their native children.
Keywords: children, COVID‐19, Kuppuswamy's socio‐economic status, lockdown, mental health
Key messages.
Lockdown may impact the diet, weight and sleeping pattern of children.
Lockdown may inhibit the social development of the children.
Approximately 73.15% and 51.25% of the children showed increased irritation and anger.
Qualification of mother is one of the factors that affect children's mental health.
Therefore, it is important to spread awareness about the importance of mental health of the children during lockdown.
1. INTRODUCTION
Natural disaster is an event that can pose regional or global loss to human life, economy and infrastructure. Such calamitous events generally occur in three ways, that is, (a) meteorological, (b) geophysical and (c) biological. Among these three natural disasters, the lattermost does not cause much direct harm to the infrastructure; however, consequences of its impacts on human life and economy remain for a longer period of time. Biological disasters are generally caused by certain bioactive substances, pathogenic microorganisms and biotoxins. The risks associated with biological disasters are mainly dependent on certain characteristics of the microorganism, namely, the reproduction number, the number of species it is impacting, death rate and mode of transmission. On the basis of the severity of the biological disaster, different preventive measures are implemented into the society to suppress and mitigate the consequences of the biological disaster.
In case of epidemic and pandemic situations caused by certain communicable disease, lockdown is one of the primary steps that are taken to bring down the reproduction rate of the microorganism to <1 (Zhang, Zhao, & Hu, 2020). For example, in 2003, several areas of China and Canada were locked down due to the spread of SARS infection. Similarly, Ebola virus impacted a large area of Africa; due to which, many cities of West Africa were put into lockdown (Wang, Zhang, Zhao, Zhang, & Jiang, 2020). Therefore, in today's unprecedented times, when COVID‐19 has caused a pandemic situation in the world, almost all the affected countries have announced complete lockdown (Arshad Ali, Baloch, Ahmed, Arshad Ali, & Iqbal, 2020; Khan et al., 2020; Yang et al., 2020). Also, on 22 March 2020, the authorities of India announced a complete nationwide lockdown in the country. The impacts of these measures on the normal lifestyle of the citizens of India are very sudden and unexpected (Parmet & Sinha, 2020). Such an uncertain condition has caused distressful situation among people of all ages, that is, elders, adults, adolescents and children. Therefore, citizens of India, which are now living an interrupted lifestyle under lockdown, are prone to confront distressful moods, namely, depression, sleeplessness and anxiety (Breslau, 2001).
While evaluating the impacts of COVID‐19‐induced lockdown on mental health of human beings, Satcher and Kenned (2020) observed that anxiety and increased fear are the common symptoms that were reported among people living under lockdown. To understand the compromised mental health in lockdown situation, Brooks et al. (2020) conducted a systematic review of 3166 published articles, findings of which presented the seriousness of the psychological impacts of lockdown. This study revealed that lockdown may lead to anxiety, anger, sleep disorder, depression and post‐traumatic stress disorder (PTSD) among the children. Sprang and Silman (2013) also observed four times higher PSTD score among the children who had lived under lockdown than those who had not. However, the level of psychological impacts of lockdown is related to various factors such as lifestyle, society and culture. Therefore, the present study aimed to understand the impacts of the 42‐day nationwide lockdown on the behaviour of the children living in Punjab, India. An ad hoc questionnaire was used to record the assessment of children's parents. The findings of this study will synthesize evidences, with respect to compromised mental health of the children during lockdown. This will further assist policymakers in reducing the negative effects of lockdown and increasing its efficiency as a public health measure.
2. METHODS
2.1. Questionnaire
Considering that psychology of a child is highly influenced by several factors such as parents' health, relation among the family members, child's medical history, financial status of the family and qualification of the parents, the questionnaire (Table S1) used in this study was divided into four sections, which are as follows (Cohen, Kelleher, & Mannarino, 2008; Dehon & Scheeringa, 2006):
Details of respondent: In this section, contact details of the interviewee were noted.
Details of respondent's family: Socio‐economic status and size of the family are important factors affecting the mental growth of the children. Therefore, in this section, details of the family were recorded. In Indian societies, there are two types of families, that is, nuclear and joint. In such families, head of the family may either be the father of the child or some elder family member. Therefore, while deciding the Kuppuswamy socio‐economic status of the family, qualification and gross income of the two types of the families were considered (Wani, 2019).
Details of the residence: In this section, information regarding area of the house and facilities available was noted.
Details of the child's family: Habits of the child's parents, their qualification, relationship and medical history are some of the characteristics of a family that largely influence the behaviour of the child.
Details about the children: In this section, complete information about the child's habits, changes in behaviour and medical history was recorded.
Questionnaire was firstly prepared on Google Docs, and then, the link of the questionnaire was shared with all the interviewees before discussing and filling the questionnaire over phone. Finally, a relation among the different factors was analysed and correlated to derive conclusions. The brief layout of the methodology, followed in this study, is explained in Figure 1.
FIGURE 1.
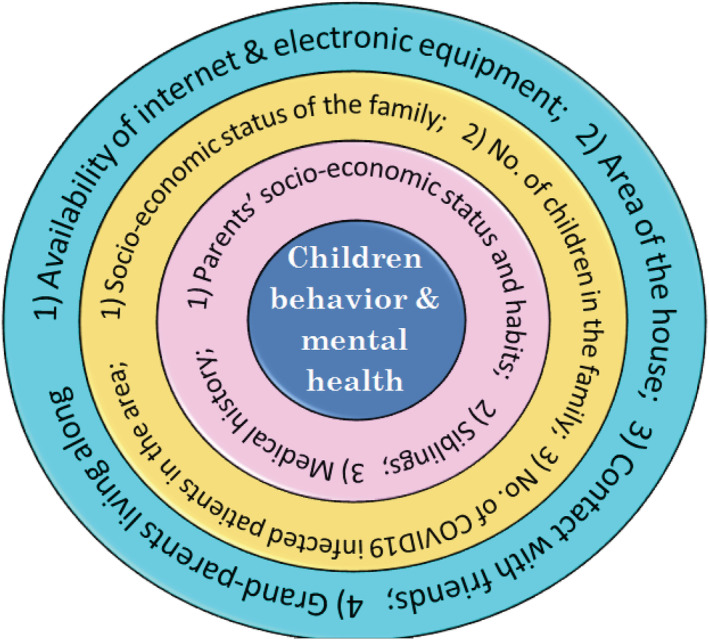
Brief layout of the methodology [Colour figure can be viewed at wileyonlinelibrary.com]
2.2. Study area and sampling
Study area chosen for conducting the survey was Punjab state in North India. Occupation of the residents of Punjab is mainly agriculture, and people with different economic status and qualification are easily available. Including all the states of India, Punjab also went under 42 days of strict lockdown, due to COVID‐19, since 25 March 2020. Till 3 May 2020, Punjab had 964 active cases, 117 recovered case and 21 deceased cases. Almost all the districts of Punjab were having COVID‐19‐infected patients. For the present study, only four districts, that is, Ludhiana, Sahibzada Ajit Singh (SAS) Nagar Mohali, Ferozepur and Sangrur, were chosen for the survey. Among these four districts, the first two were having the highest number of COVID‐19‐infected patients, and the rest were having the minimum number of infected patients. Therefore, implementation of COVID‐19‐induced lockdown was also lenient in Sangrur and Ferozepur. The brief demographic and COVID‐19‐related details of the four districts are mentioned in Figure 2.
FIGURE 2.
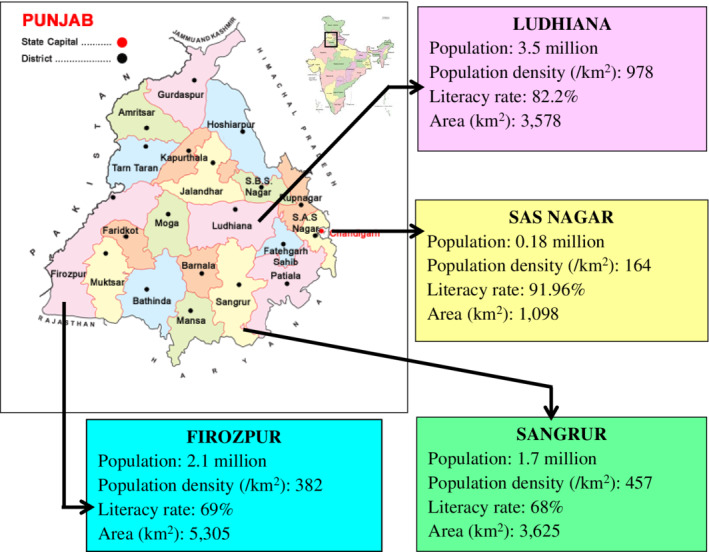
Demographics of the study area [Colour figure can be viewed at wileyonlinelibrary.com]
Sample size for the study was calculated using Equation 1.
| (1) |
where N denotes the population size; e represents the margin of error; and z is the z score. In the present study, the value of confidence level, margin of error and z score were calculated as 95%, 5% and 1.96, respectively. From Equation 1, the samples size of the study area was calculated to be 400 interviewees. Therefore, 100 interviewees were contacted telephonically, on the basis of convenient sampling, from each district.
3. RESULTS AND DISCUSSION
3.1. Response rate of the interviewees
A description of the attitudes of the interviewees from all the four districts of the study area towards participating in the questionnaire is mentioned in Table 1.
TABLE 1.
Response rate of the interviewees
| No. of interviewees approached | Did not participate | Incomplete | Complete | |
|---|---|---|---|---|
| Ludhiana | 100 | 21 | 9 | 70 |
| Sangrur | 100 | 10 | 5 | 85 |
| Ferozepur | 100 | 11 | 7 | 82 |
| SAS Nagar | 100 | 16 | 11 | 73 |
| Total (%) | 400 | 58 (14.5) | 32 (8) | 310 (77.5) |
Abbreviation: SAS, Sahibzada Ajit Singh.
From Table 1, it was observed that out of 400, a total of 310 interviews were successful, leading the response rate to 77.5%. Highest inputs were observed from Ferozepur and Sangrur, as compared with Ludhiana and SAS Nagar. This could possibly be because of fear of interaction among the residents of Ludhiana and SAS Nagar, due to higher reporting of COVID‐19‐infected patients from the region.
3.2. Analysis of the responses
The information extracted out of the questionnaire was segregated into three sections, which are as follows:
details of the family and household;
mental health of the children; and
factors affecting the mental health of the children.
An elaborated discussion on each section is done in the following sections:
-
1
Details of the family and household: This section represents the findings about child's family and the type of lifestyle they are living. In addition, it also describes the household and type of facilities available to the residents. The responses of the interviewees for this section are described in Table 2.
TABLE 2.
Details of the respondents' families and households
| S. No. | Details of questions asked | Ludhiana | Sangrur | Ferozepur | SAS Nagar |
|---|---|---|---|---|---|
| 1 | Gender of the child | ||||
| M | 41 (58.5) | 48 (56.5) | 51 (62.2) | 39 (53.4) | |
| F | 29 (41.5) | 37 (43.5) | 31 (37.8) | 34 (46.6) | |
| 2 | School/kindergarten‐going child | 61 (87) | 53 (62.4) | 47 (57.3) | 59 (80.8) |
| 3 | Type of families | ||||
| Joint | 20 (28.6) | 32 (37.6) | 25 (30.5) | 14 (19.2) | |
| Nuclear | 50 (71.4) | 53 (62.4) | 57 (69.5) | 59 (80.8) | |
| 4 | Socio‐economic status of the joint families (%) | ||||
| Upper (26–29) | 3 (4.3) | 2 (2.4) | 1 (1.2) | 4 (5.5) | |
| Upper middle (16–25) | 6 (8.6) | 5 (5.9) | 3 (3.7) | 1 (1.4) | |
| Lower middle (11–15) | 7 (10) | 13 (15.3) | 11 (13.4) | 8 (11) | |
| Upper lower (5–10) | 2 (2.9) | 7 (8.2) | 6 (7.3) | 0 (0) | |
| Lower (01–04) | 2 (2.9) | 5 (5.9) | 4 (4.9) | 1 (1.4) | |
| 5 | Socio‐economic status of the nuclear families | ||||
| Upper (26–29) | 9 (12.9) | 6 (7.1) | 7 (8.5) | 9 (12.3) | |
| Upper middle (16–25) | 9 (12.9) | 7 (8.2) | 7 (8.5) | 14 (19.2) | |
| Lower middle (11–15) | 17 (24.3) | 21 (24.7) | 18 (22) | 20 (27.4) | |
| Upper lower (5–10) | 11 (15.7) | 15 (17.6) | 18 (22) | 10 (13.7) | |
| Lower (01–04) | 4 (5.7) | 4 (4.7) | 7 (8.5) | 6 (8.2) | |
| 6 | Number of families residing together in joint families | ||||
| 2 | 17 (24.3) | 26 (30.6) | 19 (23.2) | 11 (15.1) | |
| 3 | 2 (2.9) | 4 (4.7) | 4 (4.9) | 2 (7) | |
| 4 | 1 (1.4) | 2 (2.4) | 2 (2.4) | 1 (1.4) | |
| >4 | 0 (0) | 0 (0) | 0 (0) | 0 (0) | |
| 7 | Number of children in the family | ||||
| 1 | 30 (42.9) | 32 (37.6) | 30 (36.6) | 38 (52.1) | |
| 2 | 28 (40) | 38 (44.7) | 30 (36.6) | 18 (24.7) | |
| 3 | 7 (10) | 9 (10.6) | 12 (14.6) | 10 (13.7) | |
| >3 | 5 (7.1) | 6 (7.1) | 10 (12.2) | 7 (9.6) | |
| 8 | Stress level of parents' increased | 33 (47.1) | 23 (27.1) | 26 (31.7) | 20 (27.4) |
| 9 | Father addicted to drugs | 10 (14.3) | 16 (18.8) | 21 (25.6) | 8 (11) |
| 10 | Type of electronic equipment available | ||||
| TV | 69 (98.6) | 77 (90.6) | 78 (95.1) | 72 (98.6) | |
| Mobile (smart phone) | 66 (94.3) | 80 (94.1) | 75 (91.5) | 69 (94.5) | |
| Internet (mobile based) | 62 (88.6) | 74 (87.1) | 70 (85.4) | 63 (86.3) | |
| Laptop/desktop | 27 (38.6) | 35 (41.2) | 31 (37.8) | 28 (38.4) | |
| 11 | Area of the house (%) | ||||
| <2000 sq. ft | 24 (34.3) | 43 (50.6) | 39 (47.6) | 32 (43.8) | |
| >2000 sq. ft | 46 (65.7) | 42 (49.4) | 43 (52.4) | 41 (56.2) | |
From Table 2, it can be inferred that in all the four districts, the major respondents were having male children. Gender gap among the children of the different districts was in the order Ferozepur > Ludhiana > Sangrur > SAS Nagar, which can be augmented by the respective literacy rates of the districts.
Similarly, children who are pursuing education in schools or kindergartens and the number of nuclear families were observed more in Ludhiana and SAS Nagar. As influence of the parents may vary with the type of family, a separate column was mentioned for Kuppuswamy's socio‐economic status of the joint and nuclear families. Socio‐economic status of the joint families revealed that the cumulative proportion of the upper‐ and upper‐middle‐class families was higher in Ludhiana (13.1%) and SAS Nagar (6.9%). However, the cumulative proportion of the upper‐lower and lower‐class joint families was comparatively higher in Sangrur (14.1%) and Ferozepur (12.2%). Similar observations were reported for the socio‐economic status of the nuclear families in all the four districts. In joint families, it was found that larger number of families was the ones where only two families were living together. Other than that, there were joint families where the number of families was three or four. However, none of the joint families were observed to be living with more than four families together. The families of the respondents were mostly having either one or two children living along. However, there were families where the number of children was three or even more than that, but such families were very few (~3.4%). Single‐child families were proportionately more among the districts of Ludhiana and SAS Nagar. The proportion of rest of the families having two, three or more than three children was almost same among the respondents of the four districts. Stress level of the parents residing in Ludhiana was reported highest (47.1%) among all the parents of the other districts. Fathers of the children living in Sangrur and Ferozepur were the most drug addicted, which can again be attributed to the literacy rate of specific districts.
-
2
Mental health of the children: In this section, discussion on the information collected during the interviews concerning the mental health of the child is done. It points out the issues with which the children of the study area are suffering from during the lockdown period. Such issues could deliberately disturb the mental health of the children who spend a lot of their daily life indoors. The observations made during this analysis are summarized in Table 3.
TABLE 3.
Description of the mental health of the children
| Ludhiana (%) | Sangrur (%) | Ferozepur (%) | SAS Nagar (%) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| S. no. | Questions | Y | N | DK | Y | N | DK | Y | N | DK | Y | N | DK |
| 1 | Is child suffering from | ||||||||||||
| Anxiety | 15 (21.4) | 46 (65.7) | 09 (12.9) | 20 (23.5) | 46 (54.1) | 11 (18.8) | 10 (12.2) | 54 (65.9) | 21 (25.6) | 21 (28.8) | 47 (64.4) | 05 (6.8) | |
| Depression | 16 (22.9) | 46 (65.7) | 08 (11.4) | 18 (21.2) | 50 (58.8) | 14 (16.5) | 09 (11) | 56 (68.3) | 20 (24.4) | 22 (30.1) | 45 (61.6) | 06 (8.2) | |
| Anger | 56 (80) | 10 (14.3) | 04 (5.7) | 50 (58.8) | 21 (24.7) | 11 (12.9) | 44 (53.7) | 25 (30.5) | 16 (19.5) | 55 (75.3) | 14 (19.2) | 04 (5.5) | |
| Irritation | 60 (85.7) | 8 (11.4) | 02 (2.9) | 58 (68.2) | 06 (7.1) | 18 (21.2) | 52 (63.4) | 12 (14.6) | 21 (25.6) | 55 (75.3) | 12 (16.4) | 06 (8.2) | |
| 2 | Diet of child affected | 50 (71.4) | 16 (22.9) | 04 (5.7) | 61 (71.8) | 12 (14.1) | 09 (10.6) | 52 (63.4) | 21 (25.6) | 12 (14.6) | 44 (60.3) | 22 (30.1) | 07 (9.6) |
| 3 | Weight of child changed | 58 (82.9) | 07 (10) | 05 (7.1) | 70 (82.4) | 05 (5.9) | 07 (8.2) | 63 (76.8) | 14 (17.1) | 08 (9.8) | 55 (75.3) | 13 (17.8) | 05 (6.8) |
| 4 | Sleep of child disturbed | 40 (57.1) | 14 (20) | 16 (22.9) | 51 (60) | 08 (9.4) | 13 (15.3) | 43 (52.4) | 24 (29.3) | 18 (22) | 37 (50.7) | 25 (34.2) | 11 (15.1) |
| 5 | Child spend more time using TV, mobile phone | 50 (71.4) | 11 (15.7) | 09 (12.9) | 65 (76.5) | 13 (15.3) | 04 (4.7) | 60 (73.2) | 17 (20.7) | 08 (9.8) | 45 (61.6) | 16 (21.9) | 12 (16.4) |
| 6 | Urge to play outdoors | 64 (91.4) | 06 (8.6) | 00 (0) | 51 (60) | 31 (36.5) | 00 (0) | 55 (67.1) | 30 (36.6) | 00 (0) | 68 (93.2) | 05 (6.8) | 00 (0) |
| 7 | Child missing his/her friends | 22 (31.4) | 36 (51.4) | 12 (17.1) | 30 (35.3) | 30 (35.3) | 22 (25.9) | 25 (30.5) | 31 (37.8) | 29 (35.4) | 29 (39.7) | 22 (30.1) | 22 (30.1) |
| 8 | Quarrels increased | 28 (70) | 09 (22.5) | 03 (7.5) | 36 (68) | 16 (30.2) | 01 (1.8) | 33 (63.5) | 17 (32.7) | 02 (3.8) | 27 (77) | 04 (11.5) | 04 (11.5) |
| 9 | Impact on social development of child | 61 (87.1) | 00 (0) | 09 (12.9) | 74 (87.1) | 00 (0) | 14 (16.5) | 70 (85.4) | 04 (4.9) | 11 (13.4) | 61 (83.6) | 05 (6.8) | 07 (9.6) |
| 10 | Child knows about COVID‐19 | 42 (60) | 19 (27.1) | 09 (12.9) | 35 (41.2) | 31 (36.5) | 16 (18.8) | 33 (40.2) | 42 (51.2) | 10 (12.2) | 49 (67.1) | 15 (20.5) | 09 (12.3) |
| 11 | Child needs counselling | 50 (71.4) | 12 (17.1) | 08 (11.4) | 42 (49.4) | 25 (29.4) | 15 (17.6) | 41 (50) | 27 (32.9) | 17 (20.7) | 49 (67.1) | 14 (19.2) | 10 (13.7) |
Abbreviations: DK, do not know; N, no; Y, yes.
From Table 3, it is evidently clear that after the lockdown period, several children of the study area were suffering from initial symptoms of disturbed mental health, that is, irritation and anger. Some parents have also reported serious psychological symptoms among their children such as depression and anxiety. Among the four districts, respondents from Ludhiana and SAS Nagar reported comparatively high (>75%) psychological symptoms among their children.
Psychological symptoms may also be augmented by disturbances in daily activities of the children such as diet, weight, sleep of the children and usage of electronic equipment. Changes in diet, weight and sleep of the children were reported almost similar among the children of all the districts. Variations in diet intake of the children were reported by almost 60%–72% of the respondents, and children with change in body weight were almost in the range of 75%–83%. Ludhiana district again led in these changes of the children's activities. With 60% and 71.4% of the children showing disturbances in the sleeping hours and increased usage of the electronic equipment, Sangrur district showed the highest impacted children.
During lockdown, several normal indoor and outdoor activities of the children are severely affected, which may alter the mental health of the children. For an instance, in the present study, it was indicated that children urge to play outdoors during the lockdown period. In Ludhiana and SAS Nagar, almost 92% of the children wanted to play outdoor games; because of which, some of them (~30%–35%) also miss playing and talking to their friends. Consequently, when siblings stayed indoors during the lockdown, they quarrel among each other, which can also lead to stress among the children. On an average, 69.5% of the parents of the study area mentioned that the quarrels among their children have increased since the lockdown is imposed. Moreover, parents also pointed that under the circumstances created due to lockdown, the social development of their children may also get compromised.
Several measures were taken by the families to make their children understand the situation during the COVID‐19 pandemic and its importance. Therefore, the parents should keep informing their children in a calm way. However, it was reported that in Ludhiana and SAS Nagar, 60% and 67.1% of the children, respectively, were having brief knowledge about the COVID‐19 situation. Condition was even worse among the children of Sangrur and Ferozepur, where on an average, only 34% of the children were having an understanding about the COVID‐19 situation. Moreover, from Table 3, it is also evident that the parents also stressed on the need of professional counselling of their children in order to keep their mental health intact. Almost 50% of the parents agreed that their children need a professional help, which could assist them in understanding the alterations made in the normal lifestyle of their children due to COVID‐19 induced lockdown.
-
3
Factors affecting the mental health of the children: Finally, using Pearson's correlation, an association among the activities going around the children and its own mental health was tried to develop. The results of this analysis are shown in Table 4.
TABLE 4.
Factors affecting the mental health of the children
| Area of the house | Socio‐economic status of the joint family | Socio‐economic status of the nuclear family | Qualification of the father | Qualification of the mother | Mental health of the parents | Number of children in the family | |
|---|---|---|---|---|---|---|---|
| Child's anxiety/depression/anger/irritation | +0.6 | +0.5 | +0.3 | −0.2 | −0.6 | −0.2 | +0.4 |
| Quarrel among children of the family | −0.5 | +0.1 | +0.2 | −0.3 | −0.7 | −0.3 | +0.8 |
| Diet of the child disturbed | −0.2 | −0.7 | −0.8 | −0.4 | −0.1 | +0.4 | −0.1 |
| Weight of the child disturbed | −0.1 | 0.0 | +0.1 | −0.2 | −0.6 | +0.5 | +0.2 |
| Usage of TV, mobile phones, laptop | −0.3 | +0.1 | +0.3 | −0.4 | −0.6 | +0.5 | +0.6 |
| Sleep disorder | +0.2 | +0.2 | +0.3 | −0.2 | −0.4 | +0.4 | −0.7 |
| Child insists to go outdoors | −0.4 | −0.3 | −0.1 | −0.3 | −0.6 | +0.1 | −0.5 |
| Child gets sick more often | −0.1 | −0.6 | −0.2 | −0.3 | −0.8 | +0.8 | −0.6 |
Note: + and − denote the positive and negative correlation.
Table 4 indicated that symptoms of degraded mental health of the children such as anxiety, depression, anger and irritation are significantly related with the area of the house, socio‐economic status of the joint family and qualification of the mother. These parameters were also highly correlated with other similar factors of mental health such as disturbances in the diet and weight of the children and, moreover, increased usage of the electronic equipment such as TV, mobile phones and laptop.
Quarrels among children were reported to increase with decrease in the area of the house and with poor qualification of the mother. However, increase in the number of the children in the family could lead to enhanced quarrels among the children in the house.
Number of the children in the family was also observed to be significantly related to the increased usage of electronic equipment among the children, their sleep disorders, their willingness to play outdoors and getting sick from time to time. Qualification of the mother was observed to be playing a crucial role in maintaining the mental health of the children, with it having significant correlation with certain other factors such as child getting sick and its zeal to go out of the home.
AUTHOR CONTRIBUTIONS
It is declared that during the study, authors contributed in the following specific tasks:
Bhupinder Kaur Sama designed the study, contributed to the original draft and writing of the manuscript and arranged the resources.
Palakpreet Kaur designed the questionnaire and contributed to conceptualizing the study, formatting the manuscript and data mining.
Parteek Singh Thind performed the statistical analysis and contributed to the writing, reviewing and editing of the manuscript.
Manpreet Kaur Verma interviewed the subjects, reviewed the manuscript and compiled the data.
Mandeep Kaur and Dapinder Deep Singh interviewed the subjects and reviewed the manuscript.
Supporting information
TABLE S1 Supporting Information
Sama BK, Kaur P, Thind PS, Verma MK, Kaur M, Singh DD. Implications of COVID‐19‐induced nationwide lockdown on children's behaviour in Punjab, India. Child Care Health Dev. 2021;47:128–135. 10.1111/cch.12816
REFERENCES
- Arshad Ali, S. , Baloch, M. , Ahmed, N. , Arshad Ali, A. , & Iqbal, A. (2020). The outbreak of coronavirus disease 2019 (COVID‐19)—An emerging global health threat. Journal of Infection and Public Health, 13, 644–646. 10.1016/j.jiph.2020.02.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau, N. (2001). The epidemiology of posttraumatic stress disorder: What is the extent of the problem? Journal of Clinical Psychiatry, 62(17), 16–22. [PubMed] [Google Scholar]
- Brooks, S. K. , Webster, R. K. , Smith, L. E. , Woodland, L. , Wessely, S. , Greenberg, N. , & Rubin, G. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet, 395, 912–920. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen, J. A. , Kelleher, K. J. , & Mannarino, A. P. (2008). Identifying, treating, and referring traumatized children: The role of pediatric providers. Archives of Pediatrics and Adolescent Medicine, 162(5), 447–452. 10.1001/archpedi.162.5.447 [DOI] [PubMed] [Google Scholar]
- Dehon, C. , & Scheeringa, M. S. (2006). Screening for preschool posttraumatic stress disorder with the Child Behavior Checklist. Journal of Pediatric Psychology, 31(4), 431–435. 10.1093/jpepsy/jsj006 [DOI] [PubMed] [Google Scholar]
- Khan, S. , Siddique, R. , Ali, A. , Bai, Q. , Li, Z. , Li, H. , … Nabi, G. (2020). The spread of novel coronavirus has created an alarming situation worldwide. Journal of Infection and Public Health, 13, 469–471. 10.1016/j.jiph.2020.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parmet, W. E. , & Sinha, M. S. (2020). Covid‐19—The law and limits of quarantine. New England Journal of Medicine, 382, 28. [DOI] [PubMed] [Google Scholar]
- Satcher, D. , & Kenned, P. J. (2020). Failure to address coronavirus mental health issues will prolong impact. https://thehill.com/opinion/healthcare/488370-failure-to-address-coronavirus- mental‐health‐issues‐will‐prolong‐impact.
- Sprang, G. , & Silman, M. (2013). Posttraumatic stress disorder in parents and youth after health‐related disasters. Disaster Medicine and Public Health Preparedness, 7, 105–110. 10.1017/dmp.2013.22 [DOI] [PubMed] [Google Scholar]
- Wang, G. , Zhang, Y. , Zhao, J. , Zhang, J. , & Jiang, F. (2020). Mitigate the effects of home confinement on children during theCOVID‐19 outbreak. Lancet, 395(10228), 945–947. 10.1016/S0140-6736(20)30547-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wani, R. T. (2019). Socioeconomic status scales—Modified Kuppuswamy and Udai Pareekh's scale updated for 2019. Journal of Family Medicine and Primary Care, 8(6), 1846–1849. 10.4103/jfmpc.jfmpc_288_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang, M. C. , Hung, P. P. , Wu, Y. K. , Peng, M. Y. , Chao, Y. C. , & Su, W. L. (2020). A three generation family cluster with COVID‐19 infection: Should quarantine be prolonged? Public Health, 185, 31–33. 10.1016/j.puhe.2020.05.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang, Y. , Zhao, Q. , & Hu, B. (2020). Community‐based prevention and control of COVID‐19: Experience from China. American Journal of Infection Control, 48, 716–727. 10.1016/j.ajic.2020.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
TABLE S1 Supporting Information


