The United Kingdom National Health Service (NHS) response to the coronavirus pandemic (COVID‐19) involved far‐reaching service reconfigurations to release clinical capacity, including staff redeployment and whole department relocations. Rapid development of novel ways of working followed to provide care for people with bleeding‐disorders and their families and ensure provision of safety‐netting systems during a period of severely restricted face‐to‐face consultations.
UK hospitals adapted to deal with the repercussions of the pandemic, and it is possible that haemophilia services may not return to their previous form. Funding pressures are likely to be renewed, and individual hospital organizations will recognize that some of the initiatives introduced offer opportunities to rationalize services whilst maintaining standards of care.
A virtual meeting of UK NHS haemophilia physiotherapists took place on 3rd June 2020 to share how services had been affected during the pandemic and review potential implications for physiotherapy in the future. Following an unstructured discussion of experiences, an analysis of strengths, weaknesses, opportunities and threats analysis (SWOT) was undertaken to prioritize strategies for the reopening of haemophilia physiotherapy services (Figure 1). Nine physiotherapists from centres in the UK London [2], Canterbury, Basingstoke, Leeds [2], Newcastle, Cardiff and Belfast participated in this meeting.
Figure 1.
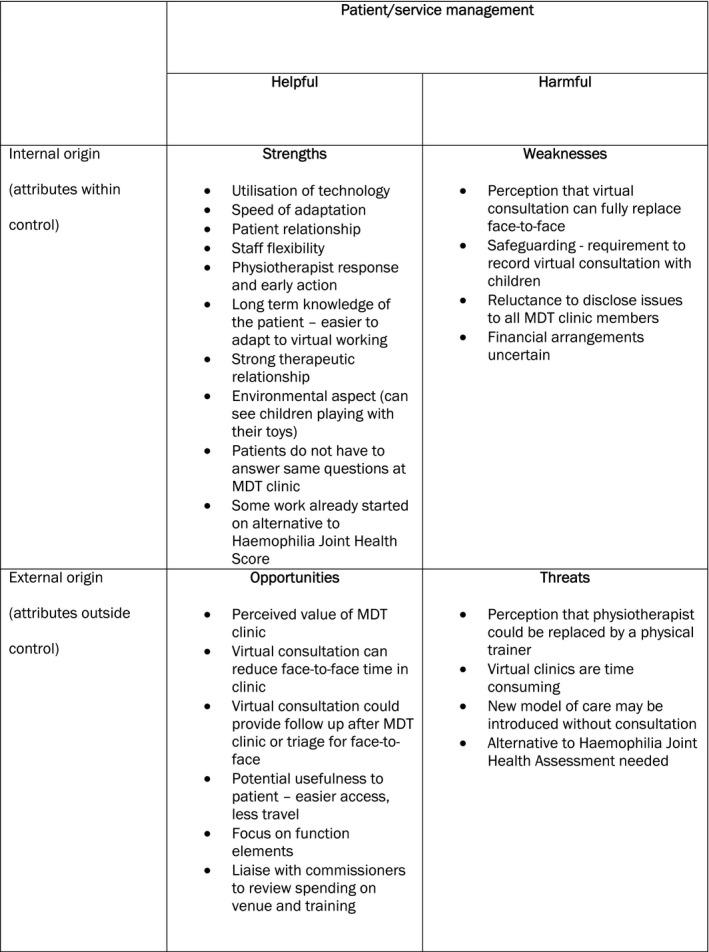
SWOT analysis
The immediate response to the pandemic focussed on freeing acute hospital beds and support services for the expected influx of patients with COVID‐19, reducing or closing nonessential clinics and relocating nonacute services. The impact on haemophilia services depended on local circumstances. Centres were moved to shared premises, and other sites or other services moved into the haemophilia centre. Environmental factors were particularly significant in such decisions. For example, one centre was adjacent to a car park served by an entrance isolated from the rest of the hospital, thereby reducing risk of exposure.
Pre‐COVID, all centres routinely provided face‐to‐face consultations with members of the multi‐disciplinary team (MDT) for people with severe or moderate haemophilia and telephone clinics for those with a mild bleeding disorder. Use of video consultations was not utilized in any of the centres pre‐COVID, and only one had considered virtual consultations prior to the pandemic.
During COVID, centres operated on ‘skeleton’ staff with colleagues shielding, self‐isolating, redeployed to COVID‐19 wards/intensive care units, seconded to support COVID research activity, medical staff redeployed to main hospital rota and nurses to general wards, where possible centre nurses and physiotherapists delivered their haemophilia service remotely from home using ‘telehealth’ (telephone, video‐consultations).
Routine face‐to‐face clinics were cancelled, and patients advised against visiting the hospital unless an urgent need was identified during a telehealth consultation (e.g. enhanced bleed management or the patient/family had specific concerns that could not be dealt with remotely). Planned hospital appointments had constraints such as attending with only one other person. Shared clinic rooms required enhanced cleaning and even where the layout of the premises allowed for direct access clinic appointments were drastically reduced.
Telehealth included routine consultations, triage and rehabilitation. For example, a young person with a bleeding‐disorder sustained an iliopsoas bleed secondary to increasing their exercise level during lockdown; however, a telephone review with a Haematologist did not lead to improvement. During a follow‐up video consultation by the physiotherapist, they were able to assess how severe the bleed was, realize the level of distress the patient felt and offer focussed treatment. Similarly, when a parent had expressed concern about their child with haemophilia, the physiotherapist was able to observe them at play and provide reassurance.
An array of digital technology was used for video consultations depending on individual hospital policies including: Zoom; Microsoft Teams; Google Meet; Google Duo and Attend Anywhere. Choice was largely influenced by local governance directives; however, prior to these being established, accessible platforms like WhatsApp had been used in early acute scenarios. Challenges to telehealth implementation included outdated computer operating systems, software and browsers and insufficient access to suitable hardware for video consultations. Ease of implementing platforms varied with reports of frequent crashing of systems to no issues at all. The latter experience enabled some centres to quickly offer several clinics per week. Good support from local Information Technology departments appeared to enhance uptake of video consultations. Most members of the MDT were supportive of video consultations; however, more than one centre noted disinterest/lack of engagement particularly among medical staff.
Rapid adoption of telehealth was not always smooth. Notifications from one hospital conflicted with those sent by the centre resulting in patients being unaware of a telehealth appointment and so not being available. As lockdown in the UK eases, unavailability of patients for video consultation appears to have increased.
Child safeguarding was highlighted as an area of concern. Video consultations should always have a parent or guardian visible and should never take place with a child in an inappropriate setting/room such as a bedroom/bathroom. One centre reported that no video consultations with children were currently permitted, whilst another had a policy that all paediatric consultations had to be accessed through the hospitals portal to ensure security. Maintaining confidentiality of patient information was a further concern. The group agreed that only systems approved by the NHS should be used, and users should apply relevant professional standards as they would normally, ensuring personal information stored on their own device, or obtained through a video or conversation, is safely transferred to the appropriate health and care record and personal information, including back‐up data deleted as soon as possible.
Although video consultations had proved to be a valuable means of patient contact, several physiotherapists expressed concerns about future use. Physical contact is a key aspect to physiotherapy assessment. The group acknowledged pitfalls of attempting a diagnosis from a video image; however, this was a rapidly evolving situation with limited guidance/options being available. Equally, considering the patient's perspective, they may be prepared to disclose something to an individual but may not if all members of MDT were on the call. Thought and care is required to reduce or avoid the loss of such vital communications between an individual/family and their care team.
Video would not routinely be an acceptable substitute for a face‐to‐face consultation, because UK physiotherapists are required to assess and record the Haemophilia Joint Health Score as a service quality indicator. Performance indicators will require adaptation to take account of the limitations of telehealth and to reflect the growing need for functional measures to be incorporated in physiotherapy management.
Some centres had virtual MDT meetings although acknowledging difficulties involving patients and in engaging all team members. The reasons for this are likely to be multifactorial but are considered important to understand when developing future service provisions inclusive of all stakeholders.
Pre‐existing therapeutic relationships with patients appeared to be an important factor in the success of therapy remote consultations. In general, physiotherapists believed patients and families were coping well during this time. Telehealth consultations were perceived to be acceptable, and there appeared to be value in having contact with the physiotherapist during this time. Remote consultation could act as a triaging mechanism to avoid unnecessary visits to hospital or confirm need to attend. Whilst therapists agreed that children were able to use the technology for consultations, engagement was more difficult with them than with adults, but no such difficulties were reported with engaging older patients.
As we emerge from the pandemic with the gradual reopening of face‐to‐face clinics, it remains unclear whether individuals will be willing to use public transport or travel to a hospital setting for nonacute appointments. Our experience demonstrated that a reduction in nonacute, centre‐based care could be positively supported by developing telehealth physiotherapy. Published research on the value of telehealth in haemophilia care is available; however, its widespread use in the NHS is lacking. 1 , 2 , 3 Proposed models included face‐to‐face physiotherapy and nurse led clinics to evaluate musculoskeletal health complemented by follow‐up virtual consultations led by medical staff. Physiotherapists could provide immediate telehealth triage for new musculoskeletal concerns, provide timely postbleed follow‐up and support remote rehabilitation. 4 , 5 Telehealth consultations may also provide greater access for people with mild bleeding disorders, who would otherwise not be in regular contact with the centre. 4
Models of telehealth will be a feature of the post‐COVID landscape, and the involvement of patients in service redesign alongside robust evaluation of the impact on their health outcomes is required. To facilitate telehealth models of care, there is a need to collect accurate data on telehealth and patient outcomes and develop quality formal assessment tools with remote delivery capabilities, that will engage both adults and children, to measure clinical endpoints. Furthermore, most haemophilia services in the UK are funded by block contract, and it remains to be seen if funding models change as face‐to‐face contact is replaced by virtual consultations in the future.
ACKNOWLEDGEMENTS
The authors stated that they had no interests which might be perceived as posing a conflict or bias. Haemnet—for providing logistical support for the meeting, transcription and first draft.
REFERENCES
- 1. Boccalandro EA, Dallari G, Mannucci PM. Telemedicine and telerehabilitation: current and forthcoming applications in haemophilia. Blood Transfus. 2019;17(5):385‐390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Qian W, Lam TT, Lam HHW, Li CK, Cheung YT. Telehealth Interventions for Improving Self‐Management in Patients with Hemophilia: Scoping Review of Clinical Studies. J Med Internet Res. 2019;21(7):e12340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mateo F, Soria‐Olivas E, Carrasco JJ, Bonanad S, Querol F, Pérez‐Alenda S. HemoKinect: A microsoft kinect V2 based exergaming software to supervise physical exercise of patients with hemophilia. Sensors (Basel). 2018;18(8):2439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kulkarni R. Use of telehealth in the delivery of comprehensive care for patients with haemophilia and other inherited bleeding disorders. Haemophilia. 2018;24(1):33‐42. [DOI] [PubMed] [Google Scholar]
- 5. Jacobson K, Hooke MC. Telehealth videoconferencing for children with hemophilia and their families: a clinical project. J Pediatr Oncol Nurs. 2016;33(4):282‐288. [DOI] [PubMed] [Google Scholar]


