Abstract
Objective
To assess the experience, views, and opinions of rheumatology providers at Veterans Affairs (VA) facilities about rheumatic disease health care issues during the COVID‐19 pandemic.
Methods
We performed an anonymized cross‐sectional survey, conducted from April 16 to May 18, 2020, of VA rheumatology providers. We assessed provider perspectives on COVID‐19 issues and resilience.
Results
Of the 153 eligible VA rheumatologists, 103 (67%) completed the survey. A significant proportion of providers reported a ≥50% increase related to COVID‐19 in visits by telephone (53%), video‐based VA video connect (VVC; 44%), and clinical video telehealth with a facilitator (29%). A majority of the responders were somewhat or very comfortable with technology for providing health care to established patients during the COVID‐19 pandemic using telephone (87%), VVC (64%), and in‐person visits (54%). A smaller proportion were comfortable with technology providing health care to new patients. At least 65% of rheumatologists considered telephone visits appropriate for established patients with gout, osteoporosis, polymyalgia rheumatica, stable rheumatoid arthritis, stable spondyloarthritis, or osteoarthritis; 32% reported a rheumatology medication shortage. Adjusted for age, sex, and ethnicity, high provider resilience was associated with significantly higher odds ratios (ORs) of comfort with technology for telephone (OR 3.1 [95% confidence interval (95% CI) 1.1–9.7]) and VVC visits for new patients (OR 4.7 [95% CI 1.4–15.7]).
Conclusion
A better understanding of COVID‐19 rheumatic disease health care issues using a health‐system approach can better inform providers, improve provider satisfaction, and have positive effects on the care of veterans with rheumatic disease.
INTRODUCTION
COVID‐19 is highly infectious, with significant associated mortality (1). Not surprisingly, its effects on people and societies are multiple. To combat this pandemic, several measures for infection prevention have been implemented. Stay at home (shelter‐in‐place), social distancing, and other measures to reduce transmission have been adopted by many countries worldwide, including the US (2).
SIGNIFICANCE & INNOVATIONS.
A majority of the rheumatologists were somewhat or very comfortable with technology for providing health care to established patients during the COVID‐19 pandemic, but not to new patients.
Rheumatologists reported some shortages of hydroxychloroquine and of interleukin‐6 inhibitors for their patients with rheumatic diseases.
At least 65% of rheumatologists considered telephone visits appropriate for established patients with gout, osteoporosis, polymyalgia rheumatica, stable rheumatoid arthritis, stable spondyloarthritis, and osteoarthritis.
High provider resilience was independently associated with significantly higher odds of more comfort with technology for telephone‐assisted or video‐assisted telemedicine visits.
The COVID‐19 pandemic has had a significant impact on health care and health care delivery systems. Three major changes have involved the conversion of regular in‐person clinic visits to telephone/video health care visits, the use of personal protective equipment by both patients and health care providers during in‐person health care visits, and the performance of some work duties by health care providers while working from home (3). The reduced in‐person access to health care providers and health information is worrisome for people with rheumatic diseases, who require close long‐term monitoring. Provision of optimal health care in these suboptimal circumstances is very challenging.
The Veterans Affairs (VA) is the largest integrated health care system in the US, with 1,255 health facilities that provide care to >9 million veterans annually (4). The VA has had a state‐of‐the‐art electronic health care record system since 1998 that has helped to improve quality of health care. The VA pioneered telehealth more than a decade ago (5). VA telemedicine visits, including using telephone or video (with a facilitator for examination [clinical video telehealth (CVT)] or without a facilitator [VA video connect (VVC)], direct‐to‐patient), were performed for 702,000 veterans in the fiscal year 2016 (6). In 2019, more than 900,000 veterans received care through VA telemedicine (5).
Most VA facilities switched from in‐person outpatient visits to telemedicine, using telephone or video (CVT or VVC) visits, between March 16 and 20, 2020, with many facilities prohibiting routine in‐person outpatient visits. Our study objective was to conduct a cross‐sectional survey of a nationally representative sample of rheumatologists at the VA during the first few months of the COVID‐19 pandemic, to assess their experience, views, and opinions about rheumatic disease health care issues, and to understand the impact of the pandemic on VA rheumatologists and their patients.
MATERIALS AND METHODS
This study was approved by the human ethics committee at the University of Alabama at Birmingham. We obtained a list of email addresses of VA rheumatologists from the VA Rheumatology Consortium (VARC). VARC is a volunteer work group of VA rheumatologists who practice across the US. These data are available from the authors after appropriate approvals have been obtained from the Ethics Committee at the University of Alabama at Birmingham and meeting all privacy policies and regulations. After prepiloting with 6 rheumatologists, we finalized the survey. We used Qualtrics survey software to send an anonymous survey to all VA rheumatologists who were VARC members on April 16, 2020. Nonresponders received reminders to complete the survey from April 21 to May 18, 2020.
The survey assessed providers’ views and opinions about the new health care delivery methods, including the best health care delivery modality (in‐person, telephone, or video visit) for the management of each rheumatic disease, diseases appropriate for alternative methods, the perceived risk of COVID‐19 in rheumatic diseases, rheumatic disease medication shortages, and the safety of a future COVID‐19 vaccine with rheumatic disease medications. Only a few, but not all questions included CVT with a facilitator, since CVT is used much less frequently compared to a telephone visit or VVC. Provider resilience, or stress coping ability, was measured with a validated 2‐item Connor‐Davidson Resilience Scale (7), scored from 0 to 8, higher scores corresponding with higher resilience, with a general population mean of 6.9. Physicians have higher resilience scores compared to the general employed population (8).
Summary statistics were assessed as proportions. Since the number of people completing the surveys was close to 100, the actual numbers in the tables were close to the percentages, which are presented in the Results section. Logistic regression assessed whether provider age, sex, years of experience, and provider resilience (categorized as high resilience, score of 7 or 8, i.e., scores at par with the general population or higher) were independently associated with comfort with technology in providing virtual care to new or established clinic patients. We obtained the information on sex and age for all potential participants from Healthgrades and other publicly available search websites. Analyses were done using IBM SPSS, version 25. The University of Alabama at Birmingham’s Institutional Review Board (IRB) approved this study, and all investigations were conducted in conformity with ethical principles of research (UAB X120207004). The IRB waived the need for an informed consent for this anonymized study.
RESULTS
Of the 153 eligible VA rheumatologists, 103 completed the survey (67% response rate). Of these, 26% each were in the age groups 45–54 years and 55–64 years; 56% were White, 27% Asian, 6% African American, and 5% Hispanic; and 63% were female. More than two‐thirds had practiced rheumatology for 10 years or more (see Supplementary Table 1, available on the Arthritis Care & Research website at http://onlinelibrary.wiley.com/doi/10.1002/acr.24487/abstract). Nonresponders were slightly older (16% versus 11% were age ≥65 years) and more likely to be male compared to the survey responders (45% versus 38%).
Rheumatic diseases and adjudicated appropriateness of health care delivery methods early in the COVID‐19 pandemic
Two‐thirds or more of the rheumatologists chose a telephone follow‐up visit as the best modality for gout, osteoporosis, polymyalgia rheumatica, stable rheumatoid arthritis, stable spondyloarthritis, and osteoarthritis (Figure 1). One‐third or more chose a video‐based VVC follow‐up visit as the best modality for local musculoskeletal conditions, tendinitis, rheumatoid arthritis with active medication (disease‐modifying antirheumatic drug [DMARD]/biologic) changes, and patients with stable lupus, scleroderma, or vasculitis (Figure 1). In contrast, 41–53% of responders selected an in‐person follow‐up visit as the best modality for people with lupus, scleroderma, or vasculitis with immunosuppressive or glucocorticoid dose changes and rheumatoid arthritis or spondyloarthritis with active medication (DMARD/biologic) changes (Figure 1). A total of 43% of responders agreed or strongly agreed that they were able to provide health care efficiently, 68% were able to provide it safely, and >50% spent a lot of extra time providing this care.
Figure 1.
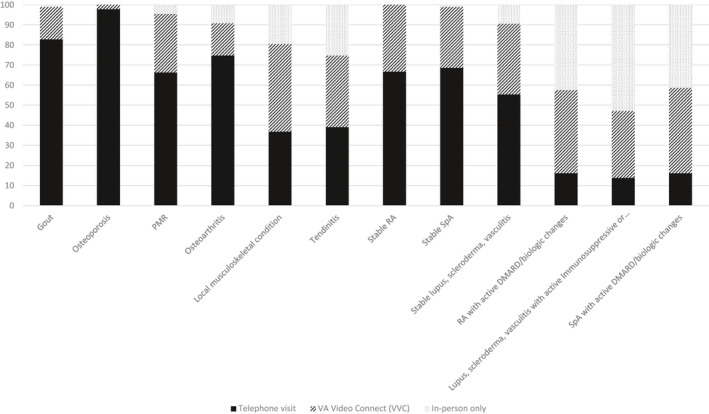
Provider‐preferred clinic follow‐up appointment modality for established patients due to COVID‐19 by the type of rheumatic disease. The y‐axis represents the percent of all valid nonmissing responses. The number of missing responses for each condition varied (n =16 to 18). Providers responded to the question: “Which of the following conditions in established patients do you feel are best suited for telephone or video‐based visits during follow‐up during the COVID‐19 pandemic? Choose the single best response.” This was followed by listing each rheumatic condition in a separate row. Response options included telephone, Veterans Administration (VA) video connect, and in‐person visit. DMARD = disease‐modifying antirheumatic drug; PMR = polymyalgia rheumatica; RA = rheumatoid arthritis; SpA = spondyloarthritis.
Provider technology use and comfort for VA health care delivery methods early in the COVID‐19 pandemic
Of the responders, 50% reported using their personal desktop and laptop, 69% were using a VA desktop, and 18% were using a VA laptop for providing VA health care during the COVID‐19 pandemic (providers could choose multiple responses). Of these, 31% were working entirely from the VA hospital or VA clinic, 14% from a non‐VA location (or home), and the rest were working from both non‐VA and VA locations. Survey responders reported providing VA health care to veterans with rheumatic disease using multiple methods during the COVID‐19 pandemic: 91% used telephone visits, 59% used video‐based VVC visits, 7% used CVT visits with a facilitator, and 59% used in‐person visits. A significant proportion of providers reported a 50% or more increase in the following types of visits related to COVID‐19: telephone visits (53%), video‐based VVC visits (44%), and CVT visits with a facilitator (29%) (see Supplementary Table 2, available on the Arthritis Care & Research website at http://onlinelibrary.wiley.com/doi/10.1002/acr.24487/abstract).
The proportion of responders who were somewhat or very comfortable while providing health care to established clinic patients using each of these methods was as follows: telephone visits (87%), video‐based VVC visits (64%), and in‐person visits (54%) (Figure 2). The proportion of responders who were somewhat or very comfortable providing health care to new clinic patients was as follows: telephone visits (25%), video‐based VVC visits (34%), and in‐person visits (58%) (Figure 2). More than two‐thirds of responders reported that evaluating a new patient scheduled in their clinic was feasible during the COVID‐19 pandemic.
Figure 2.
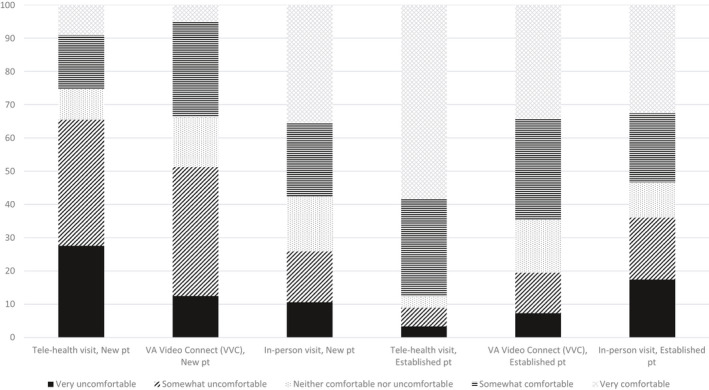
Provider comfort with technology in providing care to new or established patients using each of the modalities during the COVID‐19 pandemic. The y‐axis represents the percent of all valid nonmissing responses. Providers responded to 2 questions: “What is your level of comfort with technology with providing health care to new patients in your clinic during the COVID‐19 pandemic? What is your level of comfort with technology with providing health care to established patients in your clinic during the COVID‐19 pandemic?” Each question was followed by listing telephone, Veterans Administration (VA) video connect, and in‐person visit in a separate row. The response option was a 5‐point ordinal scale: very uncomfortable, somewhat uncomfortable, neither comfortable nor uncomfortable, somewhat comfortable, and very comfortable. As an example, 87% of respondents were somewhat or very comfortable while providing health care to established clinic patients with telephone visits versus only 25% of respondents for new patient evaluations. pt = patient.
Risk of COVID‐19 infection in veterans with rheumatic diseases
Among respondents, a majority agreed or strongly agreed that veterans with autoimmune rheumatic diseases were at a higher risk of COVID‐19 infection even in the absence of immunosuppressive drugs (54%) and when currently using immunosuppressive drugs (71%). Similarly, only a small proportion (23%) agreed or strongly agreed that veterans with nonautoimmune rheumatic diseases were at a higher risk of COVID‐19 infection.
Rheumatic disease medications: shortages and risks with a future COVID‐19 vaccine or convalescent sera
Approximately 32% of responders reported a medication shortage. Responders indicated some (little or extreme) shortage for the following: hydroxychloroquine (45%), interleukin (IL)‐6 inhibitors (15%), non–tumor necrosis factor (TNF) biologics (1%), TNF‐biologics (0%), Janus‐inhibitors (1%), and other immunosuppressives (1%).
Most responders would not withhold hydroxychloroquine (95%) or sulfasalazine (74%) for a future, live attenuated COVID‐19 vaccine. A majority would withhold methotrexate or leflunomide (66%) and glucocorticoids of 20 mg/day or higher (52%) for 2 weeks or less, and would withhold anti TNF‐biologics (85%), anti‐IL‐17/23 biologics (82%), Janus‐kinase inhibitors (78%), belimumab (77%), non‐TNF biologics (76%), and immunosuppressive drugs such as azathioprine (64%), for 3–8 weeks for administering a future, live attenuated COVID‐19 vaccine. A majority of responders (55–100%) would not withhold these drugs for administering a killed COVID‐19 vaccine; another 5–30% would hold them off for <2 weeks. A majority of responders (≥50%) would not withhold any of these drugs for a convalescent sera treatment of COVID‐19.
Perceived increase in health care disparities in veterans during COVID‐19
A significant proportion of responders perceived an increase in health care disparities during the COVID‐19 pandemic in the following groups: African Americans (40%), Hispanics (31%), other racial minorities (19%), low socioeconomic groups (47%), females (8%), rural residents (23%), and those with nonservice‐connected illnesses (12%). Of responders, 24% had had a family member or friend with a COVID‐19–positive test. Three responders had been tested for COVID‐19, 1 reported a negative test result, and 2 received care for COVID‐19 at home.
Responder resilience and comfort with technology for virtual health care visits
Resilience was high among responders. The mean ± SD Connor‐Davidson Resilience Scale score was 6.35 ± 1.260; scores were 6 or higher for >80% of people: 46%, 16%, and 23% of the responders had high resilience scores of 6, 7, and 8, respectively.
Adjusted for age, sex, and ethnicity, a high provider resilience score was independently associated with a significantly higher odds ratio (OR) of more comfort with technology (somewhat or very comfortable) for telephone health care visits (OR 3.1 [95% confidence interval (95% CI) 1.1–9.7]) and video‐based VVC visits (OR 4.7 [95% CI 1.4–15.7]) for new patients, with no difference for in‐person visits (OR 1.8 [95% CI 0.7–5.0]). No significant associations of provider resilience were noted with comfort with technology for established patients for telephone (OR 1.7 [95% CI 0.3–8.0]), VVC (OR 1.7 [95% CI 0.6–5.0]), or in‐person visits (OR 2.8 [95% CI 1.0–7.8]).
DISCUSSION
We performed a national cross‐sectional study of rheumatologists at the VA, the largest integrated health care system in the US. The survey response rate was 67%, higher than the average 61% response rate for physician surveys (9). Survey responders were similar in age and sex distribution to all potential participants, with slight differences. The survey was conducted 1 month after COVID‐19–associated outpatient health care delivery changes at the VA. Therefore, findings mostly represent provider experience and practice patterns early in the COVID‐19 pandemic. Several study findings deserve further discussion.
During the COVID‐19 pandemic, telemedicine has emerged as one of the main ways to deliver health care. Telemedicine is an acceptable alternative to an in‐person visit from the patient perspective. It can ameliorate the economic burden of clinic visits for people traveling long distances, and patients are satisfied with telemedicine visits in these situations (10). In an observational study of 85 patients with inflammatory arthritis at a single VA Medical Center, patient‐reported outcomes for care delivered via telemedicine were similar to usual care, with a significant cost and distance savings (11).
In a meta‐analysis of telemedicine studies in rheumatology, feasibility and patient satisfaction rates were high or very high for various telemedicine interventions, and effectiveness was similar to a standard in‐person approach (12). On the other hand, the majority of people preferred an in‐person over telemedicine visit for pediatric rheumatology care, despite travel and inconvenience (13). These articles highlight the contrast in patient preference for telemedicine versus in‐person visits. High rates of patient satisfaction with telemedicine care (when offered and provided to selected patients) and higher patient preference for in‐person over telemedicine visits can coexist in an ideal world. Telemedicine is a viable alternative to in‐person rheumatology follow‐up visits during the COVID‐19 pandemic.
Our study is the first national study of VA rheumatologists to examine which rheumatic conditions were considered appropriate for virtual visits using the telephone during the COVID‐19 pandemic. Survey responders made a clear distinction between conditions that were appropriate for telemedicine versus in‐person visits. More than 90% of rheumatologists surveyed considered gout, osteoporosis, osteoarthritis, and polymyalgia rheumatica to be appropriate for telephone visits or video‐based health care visits for established patients. Active systemic autoimmune rheumatic conditions (rheumatoid arthritis, spondyloarthritis, lupus, vasculitis, scleroderma, etc.) with ongoing changes to disease‐modifying, immunosuppressive, or biologic medications were considered most appropriate for in‐person visits during the COVID‐19 pandemic by the majority of responders. However, one‐third favored video visits. These patterns may change over time.
Our study found that most respondents were comfortable with telemedicine technology to provide health care to established patients with rheumatic diseases. In contrast, less than one‐third of responders were comfortable with telemedicine technology in providing care to new patients. Previous studies have shown that physicians are satisfied with telemedicine when providing care in specific specialties, including cardiology (14), neurology (15), and primary care (16). Our national study is among the first to assess this comfort for various rheumatic diseases. Our study describes VA rheumatology providers’ views and preferences 4–8 weeks after the switch from in‐person regular outpatient visits to telemedicine at VA facilities due to the COVID‐19 outbreak in the US.
We found that a high provider resilience score was associated with a 3‐ to 5‐fold higher odds of comfort with technology for telephone and video visits for new patients, with no difference for in‐person visits. To our knowledge, there are no published studies of the relationship between provider resilience and higher comfort levels with using telemedicine. Our study provides new data that will need confirmation in other studies. A mean resilience score of 6.35 for VA rheumatologists was similar to 6.49 for US physicians from a recent survey (8).
We found that 55–100% of VA rheumatology providers would not withhold 1 or more treatments for rheumatic diseases or withhold it for <2 weeks to administer an inactivated/killed COVID‐19 vaccine. In contrast, >75% would withhold biologic therapy for 2–8 weeks for administering a live attenuated COVID‐19 vaccine. The VA rheumatology providers reported some shortages of hydroxychloroquine (45%) and IL‐6 inhibitors (16%) for their VA patients with rheumatic diseases. Due to the potential for hydroxychloroquine and IL‐6 inhibitors to be treatments for COVID‐19, shortages have been reported by patients with rheumatic diseases (17). Poor outcomes in African Americans with COVID‐19 point to racial health care disparities in the US (18). VA rheumatologists, however, perceived a potential increase in health care disparities not only in African Americans and Hispanics, but also in people in the low socioeconomic groups and those living in the rural areas.
Our study findings must be interpreted considering limitations. These findings cannot be generalized to non‐VA settings without an additional similar study. Even though our study responders were similar to the overall sample in age and sex, we do not have information on other characteristics (since the survey was anonymous), and therefore nonresponse bias is a limitation. Several outcomes represent VA rheumatology provider views and opinions, which might change as the COVID‐19 epidemic evolves. However, given the nature of health care delivery changes related to COVID‐19, examining provider views and opinions was our study goal. Prior experience with telemedicine was not assessed, which might have influenced comfort with technology and the likelihood of using telemedicine visits. Providers could only choose 1 best modality for follow‐up visits; for some conditions, 2 modalities could perhaps be equally good, which our survey is unable to detect.
In conclusion, we conducted a study of experiences, views, and opinions of VA rheumatology providers. The VA is the largest integrated health care system in the US; therefore these findings are important and have implications for the VA system. The knowledge of barriers to the use of telemedicine, medication shortage, increasing health care disparities, and considerations for future COVID‐19 vaccines can inform future delivery of health care to patients with rheumatic diseases.
AUTHOR CONTRIBUTIONS
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be submitted for publication. Dr. Singh had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design
Singh, Richards, Chang, Joseph, Ng.
Acquisition of data
Singh.
Analysis and interpretation of data
Singh, Richards, Chang, Joseph, Ng.
Supporting information
Table S1‐S2
Acknowledgments
The authors thank all of the participating Veterans Affairs Rheumatology Consortium members who responded to the survey. We also thank the members of the Veterans Affairs Field Advisory Committee for their support.
Supported by the University of Alabama at Birmingham and the Birmingham Veterans Affairs Medical Center, Birmingham, Alabama.
Dr. Singh has received consulting fees from Medisys, Fidia, UBM LLC, Trio Health, Medscape, WebMD, Clinical Care Options, Clearview Healthcare Partners, Putnam Associates, Spherix, and Practice Point Communications (less than $10,000 each) and from Crealta/Horizon (more than $10,000), and owns stock options in Amarin Pharmaceuticals and Viking Therapeutics. No other disclosures relevant to this article were reported.
References
- 1. Weiss P, Murdoch DR. Clinical course and mortality risk of severe COVID‐19. Lancet 2020;395:1014–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gostin LO, Wiley LF. Governmental public health powers during the COVID‐19 pandemic: stay‐at‐home orders, business closures, and travel restrictions. JAMA 2020;323:2137–8. [DOI] [PubMed] [Google Scholar]
- 3. Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid‐19. N Engl J Med 2020;383:1679–81. [DOI] [PubMed] [Google Scholar]
- 4. Perlin JB, Kolodner RM, Roswell RH. The Veterans Health Administration: quality, value, accountability, and information as transforming strategies for patient‐centered care. Am J Manag Care 2004;10 Pt 2:828–36. [PubMed] [Google Scholar]
- 5. Department of Veterans Affairs . VA telehealth. 2020. URL: https://telehealth.va.gov/.
- 6. Department of Veterans Affairs . VA telehealth services: fact sheet. 2020. URL: https://www.va.gov/COMMUNITYCARE/docs/news/VA_Telehealth_Services.pdf.
- 7. Vaishnavi S, Connor K, Davidson JR. An abbreviated version of the Connor‐Davidson Resilience Scale (CD‐RISC), the CD‐RISC2: psychometric properties and applications in psychopharmacological trials. Psychiatry Res 2007;152:293–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. West CP, Dyrbye LN, Sinsky C, Trockel M, Tutty M, Nedelec L, et al. Resilience and burnout among physicians and the general US working population. JAMA Netw Open 2020;3:e209385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cummings SM, Savitz LA, Konrad TR. Reported response rates to mailed physician questionnaires. Health Serv Res 2001;35:1347–55. [PMC free article] [PubMed] [Google Scholar]
- 10. Poulsen KA, Millen CM, Lakshman UI, Buttner PG, Roberts LJ. Satisfaction with rural rheumatology telemedicine service. Int J Rheum Dis 2015;18:304–14. [DOI] [PubMed] [Google Scholar]
- 11. Wood PR, Caplan L. Outcomes, satisfaction, and costs of a rheumatology telemedicine program: a longitudinal evaluation. J Clin Rheumatol 2019;25:41–4. [DOI] [PubMed] [Google Scholar]
- 12. Piga M, Cangemi I, Mathieu A, Cauli A. Telemedicine for patients with rheumatic diseases: systematic review and proposal for research agenda. Semin Arthritis Rheum 2017;47:121–8. [DOI] [PubMed] [Google Scholar]
- 13. Bullock DR, Vehe RK, Zhang L, Correll CK. Telemedicine and other care models in pediatric rheumatology: an exploratory study of parents’ perceptions of barriers to care and care preferences. Pediatr Rheumatol Online J 2017;15:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Oliveira GL, Cardoso CS, Ribeiro AL, Caiaffa WT. Physician satisfaction with care to cardiovascular diseases in the municipalities of Minas Gerais: Cardiosatis‐TEAM Scale. Rev Bras Epidemiol 2011;14:240–52. [DOI] [PubMed] [Google Scholar]
- 15. Harper K, McLeod M, Brown SK, Wilson G, Turchan M, Gittings EM, et al. Teleneurology service provided via tablet technology: 3‐year outcomes and physician satisfaction. Rural Remote Health 2019;19:4743. [DOI] [PubMed] [Google Scholar]
- 16. Waterman AD, Banet G, Milligan PE, Frazier A, Verzino E, Walton B, et al. Patient and physician satisfaction with a telephone‐based anticoagulation service. J Gen Intern Med 2001;16:460–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Peschken CA. Possible consequences of a shortage of hydroxychloroquine for patients with systemic lupus erythematosus amid the COVID‐19 pandemic. J Rheumatol 2020;47:787–90. [DOI] [PubMed] [Google Scholar]
- 18. Yancy CW. COVID‐19 and African Americans. JAMA 2020;323:1891–2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1‐S2


