Abstract
Objectives
The current COVID‐19 outbreak in conjunction with the need to provide safe dental treatments and the limited knowledge on the efficacy of protective measures has posed dentists into a challenging situation. Therefore, the present article aimed at collecting experiences and recommendations of frontline clinical experts on critical aspects of dental treatment provision during pandemic.
Material & Methods
From a total of 32 European countries, one leading academic expert in Oral and Maxillofacial Surgery or Oral Surgery per country was asked to participate in an anonymous online 10‐item survey on COVID‐19 covering the topics of safety of dental settings, personal protective equipment (PPE), and patient‐related measures to reduce transmission risk. Data collection took place from April 12th to May 22nd, 2020.
Results
A total of 27 experts from different European countries completed the survey. The transmission risk of SARS‐CoV‐2 in dental settings for aerosol‐generating procedures was considered high by all experts except two. For aerosol‐free and aerosol‐generating procedures, more than 80% of the experts recommended face protection and caps for every single treatment. For aerosol‐generating procedures, additional measures (FFP2/FFP3 masks and gowns) were suggested by the vast majority of the experts. To reduce transmission risk, all experts recommended limiting aerosol‐generating procedures and reducing the number of patients in waiting areas as well as hand hygiene for the patients.
Conclusion
The limitation of aerosol‐generating procedures along with the usage of adequate personal protection equipment was considered to be crucial to protect dental healthcare providers and patients, thus reducing the transmission risk of COVID‐19.
Keywords: coronavirus, COVID‐19, expert opinion, pandemic, patient triage, personal protective equipment
1. INTRODUCTION
The spread of coronavirus disease 2019 (COVID‐19) has posed significant challenges for dentistry and medicine. The risk of nosocomial transmission led the routine dental care to be temporally suspended in several European countries experiencing COVID‐19 (Coulthard, 2020), and it was restricted to emergency treatments (Gurzawska‐Comis et al., 2020). Various measures, including the use of additional personal protective equipment (PPE), have been proposed by national and international guidelines to minimize infection risks (Pan et al., 2020; Ren et al., 2020). However, due to an extremely large demand worldwide, limited protection measures were available for the provision of dental treatments (Coulthard, 2020).
The lack of scientific evidence on the efficacy of preventive measures accelerated research tremendously, which, however, has not become comprehensive so far (Majumder & Mandl, 2020; Zimmermann & Nkenke, 2020). In addition, due to fast track review and time pressure, publications appeared online before thorough peer‐review process. This made assessing the quality of the available evidence more challenging and also more relevant than ever. Therefore, our research group reviewed the current evidence and recommendations recently (Gurzawska‐Comis et al., 2020). It was reported that literature and recommendations were mainly based on severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS).
Another approach to collect evidence is a survey of experts, that allows fast and high‐quality data collection (Atkins et al., 2004). Due to the urgent need for reliable recommendations, the authors hypothesized that research gaps might be filled by asking international experts at the frontline for their opinions.
The purpose of this study was to survey European experts about their opinion on PPE, patient triage and additional measures in dental settings during COVID‐19 pandemic.
2. MATERIAL AND METHODS
A survey was designed to identify the opinions and the experience of academic European experts in Oral and Maxillofacial Surgery or Oral Surgery, involved in the dental emergency care during the outbreak of COVID‐19. The study protocol was submitted to and approved by the Ethical Committee of the University of Dusseldorf (Protocol no. 2020–926). The recognized standards were followed (Declaration of Helsinki; European Medicines Agency Guidelines for Good Clinical Practice). The present study was also conducted and reported according to the “Good practice in the conduct and reporting of survey research” criteria (Kelly et al., 2003).
2.1. Study population
For each of the 27 member countries of the EU and for 5 additional European countries (Iceland, Norway, Moldova, Switzerland, UK), a survey invitation was sent by email to one academic expert in Oral and Maxillofacial Surgery or Oral Surgery (preferably head of the department). The selection of the participants was based on word‐of‐mouth communication and by hand search of University websites. The invitation email explained the aim of the study and included the link to the consent form and online survey. If the answer was not provided within the given deadline, a second expert from the respective country was contacted. If the second expert did not reply in time, a third expert was asked. If no response was retrieved, the country was labelled as not‐responding.
The participation in the survey was voluntary and without any incentive. All responders signed an informed consent form before accessing the questionnaire through an online survey platform (SurveyMonkey®). Data collection took place between 12th April and 22nd May 2020. Data were assessed, stored and processed anonymously.
2.2. Questionnaire
A structured questionnaire including 10 items was developed (Attachment 1). The survey was evaluated in a pilot phase by five Oral Surgeons affiliated to European universities that were selected based on the professional network of the authors. The questionnaire was amended based on their feedback, to avoid redundancies and ambiguities in the final survey. The COVID‐19 risk classification according to Gurzawska‐Comis et al. [2020] was provided: Unknown risk: (no flu‐like symptoms) AND (no contact with COVID‐19‐positive patients); High risk: (flu‐like symptoms + no contact with COVID‐19‐positive patient) OR (no flu‐like symptoms + contact with COVID‐19‐positive patient); Very high risk: COVID‐19 positive or flu‐like symptoms + contact with COVID‐19‐positive patients.
The questionnaire covered the following areas:
Participant working environment (2 items, single choice);
Infection risk of dental health professionals (2 items, single choice);
Recommended PPE for dental health professionals (2 items, matrix/multiple select);
Facilities for dental treatment of COVID‐19‐positive patients (1 item single choice);
Measures to prevent infection of health professionals and nosocomial transmission in dental clinics (2 items, matrix/single choice per row);
Information about where dental care was provided for patients with a high risk of COVID‐19 (1 item, multiple select).
The issues on the working environment included two questions. The experts were asked whether they treated patients in the private and/or university dental clinic settings (question 1) and about the number of staff members working in their departments was also investigated (question 2). The infection risk of dental health professionals had to be scored for aerosol‐free and aerosol‐generating procedures (questions 3 and 4).
Questions 5 and 6 investigated experts’ recommendation regarding PPE for dental health professionals during the pandemic for aerosol‐free or aerosol‐generating procedures.
In question 7, it was asked where COVID‐19‐positive patients should be treated in case of urgency. The relevance of various measures to prevent infection transmission in dental settings was investigated in questions 8 and 9. Information on the dental setting where patients with (high) risk of COVID‐19 were treated during pandemic was obtained in question 10.
2.3. Statistical analysis
The data analysis was performed using Microsoft Excel® for Mac version 16.37 (Microsoft®, USA). For each question, the absolute number of votes and the relative agreement (%) were calculated. As only one group was surveyed (experts in oral surgery), no comparative analyses were performed.
3. RESULTS
In total, experts from 27 (84%) countries out of 32 responded to the survey (Figure 1). To the first round of invitation, 13 experts from the respective countries responded, while to the second round 10 remaining countries replied. A total of 4 countries responded to the third round. The mean duration of answering the questionnaire was seven minutes. Details on the adhere to the “Good practice in the conduct and reporting of survey research” criteria for questionnaire studies are reported in attachment 2 (Kelly et al., 2003).
Figure 1.
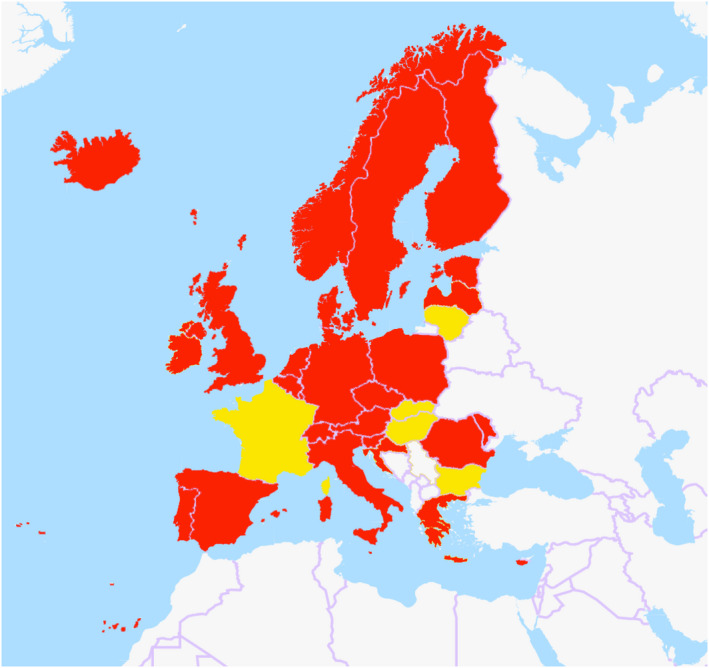
Map of European countries whose experts were contacted: in red the countries of the responders (Austria, Belgium, Croatia, Cyprus, Czech Republic, Denmark, Estonia, Finland, Germany, Greece, Iceland, Ireland, Italy, Lithuania, Luxembourg, Malta, Moldova, Netherlands, Norway, Poland, Portugal, Romania, Slovenia, Spain, Sweden, Switzerland and UK) and in yellow the countries of experts who did not reply to the survey (Bulgaria, France, Hungary, Latvia and Slovakia). (The original map was retrieved from openstreetmap.org (Open Database License))
3.1. A) Participant working environment
Eleven respondents (40.5%) stated to treat patients at the Dental University Hospital, and another eleven (40.5%) indicated treatment in both private practice and Dental University Hospital. Five participants (18.5%) reported to be working clinically in private practice only. The number of staff members working in their department was heterogeneous: 0–10 (5 participants,18.5%), 11–20 (6 participants, 22.2%), 21–30 (5 participants, 18.5%), 31–50 (4 participants 14.8%), 51–100 (6 participants, 22.2%), >100 (1 participant, 3.7%).
3.2. B) infection risk of dental health professionals
For aerosol‐free treatments, four experts (14.8%) found the risk to be low, whereas eleven rated the risk to be neutral (40.7%) and twelve (44.4%) considered the risk to be high. For aerosol‐generating procedures, two experts scored the risk to be neutral (7.4%) whereas 25 (92.6%) to be high.
3.3. C) Recommended ppe for dental health professionals
For aerosol‐free procedures, the recommendations varied for the different PPE measures (Table 1). The majority of experts recommended FFP2/FFP3 masks for treating patients at unknown (66.7%), high (88.9%) and very high (96.3%) risk, while only one expert found FFP2/FFP3 not relevant for aerosol‐free procedures.
Table 1.
Percentage (%) and number of experts agreeing that the respective PPE measure should be used during aerosol‐free procedures for patients with unknown/high/very high COVID‐19 risk/none of them. The number of experts is provided in brackets (…).
| Unknown COVID−19 risk | High COVID−19 risk | Very high COVID−19 risk only | None | |
|---|---|---|---|---|
| FFP2/FFP3 mask | 66.7% (18) | 88.9% (24) | 96.3% (26) | 3.7% (1) |
| Face shield/goggle | 81.5% (22) | 88.9% (24) | 96.3% (26) | 3.7% (1) |
| Overshoes | 40.7% (11) | 66.7% (18) | 70.4% (19) | 29.6% (8) |
| Gown | 66.7% (18) | 85.2% (23) | 92.6% (25) | 7.4% (2) |
| Cap | 85.2% (23) | 92.6% (25) | 100% (27) | 0% (0) |
| Double gloves | 40.7% (11) | 63.0% (17) | 74.1% (20) | 25.9% (7) |
Risk classification: Unknown risk: (no flu‐like symptoms) AND (no contact with COVID‐19‐positive patients); High risk: (flu‐like symptoms + no contact with COVID‐19‐positive patient) OR (no flu‐like symptoms + contact with COVID‐19‐positive patient); Very high risk: COVID‐19 positive or flu‐like symptoms + contact with COVID‐19‐positive patients
Similar replies were observed for face shields and goggles. However, there was a trend towards recommending face protection for dental staff regardless of the patients’ individual risk (22 experts, 81,5%). Overshoes were less appreciated and were not recommended at all by 29.6% of the experts. Gowns were recommended by comparable numbers of experts for patients with unknown (18 experts, 66.6%), high (23 experts, 85.2%) and very high risk (25 experts, 92.6%). In contrast, caps were frequently recommended for every treatment regardless of the individual risk (23 experts, 85.9%), whereas no experts found this measure useless for aerosol‐free procedures (Table 1).
When considering aerosol‐generating procedures, FFP2/FFP3 masks, face shields, overshoes, gowns and double gloves were recommended by the majority of participants. In contrast to aerosol‐free procedures, most of the PPE was also recommended when treating patients with unknown COVID‐19 risk (Table 2).
Table 2.
Percentage (%) and number of experts agreeing that the respective PPE measure should be used during aerosol‐generating procedures for patients with unknown/high/very high COVID‐19 risk/none of them
| Unknown COVID−19 risk | High COVID−19 risk | very high COVID−19 risk | None | |
|---|---|---|---|---|
| FFP2/FFP3 mask | 77.8% (21) | 96.3% (26) | 100% (27) | 0% (0) |
| Face shield/goggle | 92.6% (25) | 100% (27) | 100% (27) | 0% (0) |
| Overshoes | 55.6% (15) | 74.1% (20) | 77.8% (21) | 22.2% (6) |
| Gown | 81.5% (22) | 88.9% (24) | 88.9% (24) | 11.1% (3) |
| Cap | 88.9% (24) | 96.3% (26) | 100% (27) | 0% (0) |
| Double gloves | 51.8% (14) | 66.7% (18) | 74.1% (20) | 25.9% (7) |
The number of experts is provided in brackets (…).
3.4. D) Facilities for dental treatment of COVID‐19‐positive patients
A total of 18 experts (66.7%) responded that dental treatments of COVID‐19‐positive patients should be performed at Dental University Hospitals. The remaining 9 participants (33.3%) suggested private practice and Dental University Hospitals as eligible. Private practices, in contrast, were not found to be the only setting for urgent treatment of COVID‐19‐positive patients.
3.5. E) Measures to prevent infection of health professionals and nosocomial transmission in dental clinics
The wide majority of experts (25 experts, 92.6%) recommended treating COVID‐19‐positive patients in separate isolation rooms and minimizing aerosol‐generating procedures (27 experts, 100%). Furthermore, limiting the contact between staff members was found relevant by most of the experts (23 experts, 85.2%). The majority of participants also found the use of rubber dam, extraoral radiographs, air disinfection and natural air ventilation relevant (Figure 2).
Figure 2.
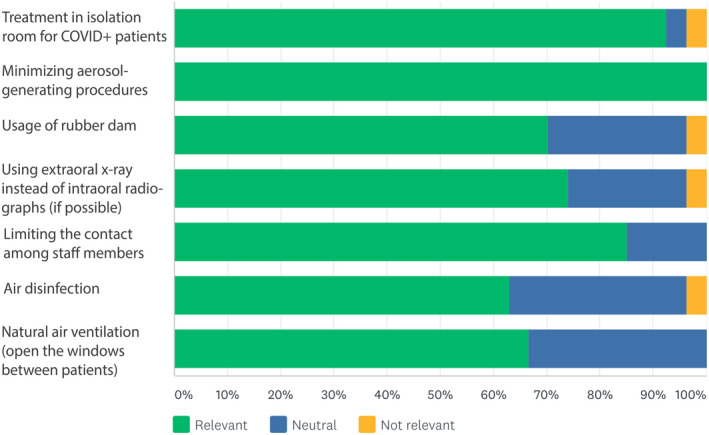
Relevance scoring for the use of different measures to decrease transmission risk of COVID‐19 in dental settings
The majority of patient‐related measures were found relevant to limit the risk of COVID‐19 transmission. All the experts agreed that the number of patients in waiting area and the time they spend there should be minimized. Phone interviews to assess the health status (COVID‐19 risk assessment) were scored to be highly relevant (81.5%). In contrast, assessing patient treatment needs via phone was approved by 66.7% of the experts only. The hand hygiene was considered to be crucial (100%), while surgical mask wear inside the clinic was slightly less approved (70.4%) (Figure 3).
Figure 3.
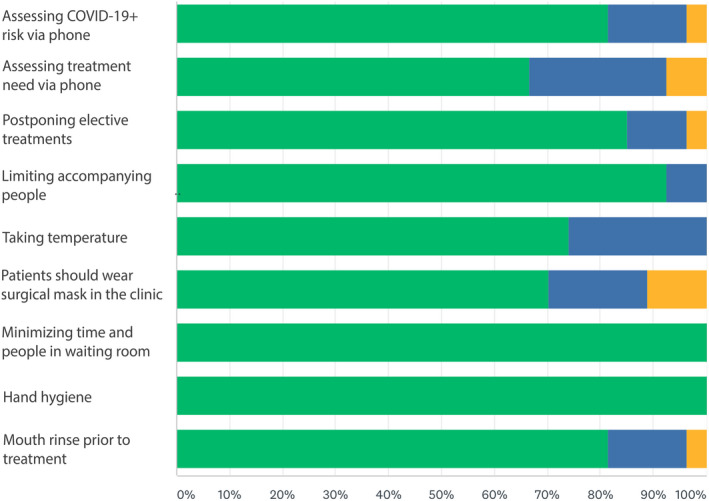
Relevance of applied patient‐related measures to decrease transmission risk of COVID‐19 in dental settings
3.6. F) Information about where dental care was provided for patients with a high risk of COVID‐19
In the majority of countries (70.4%), the Department of Oral Surgery was providing emergency dental care during data collection. The Department of Oral and Maxillofacial Surgery was reported to be involved in 55.6% of the countries. In 37.0%, private practices were providing dental treatment for COVID‐19‐positive patients or patients being at high risk. Emergency units offered dental care in 22.2% of the countries. No treatment was performed on the affected patients in 3.7% of the countries.
4. DISCUSSION
Provision of dental care during this pandemic is challenging because of the high transmission risk in dental settings (Ather et al., 2020; Izzetti et al., 2020; Meng et al., 2020). As dental care cannot be postponed for longer episodes, eligible precautionary measures have to be implemented rapidly to ensure safety in dental settings (Gurzawska‐Comis et al., 2020). At this time (May 2020), controlled clinical trials on COVID‐19 in dentistry are not yet available and they are not likely to be feasible owing to ethical reasons. To provide interim evidence‐based medicine recommendations, the research gaps can be filled with expert opinions (World Health, 2014). Therefore, the present study aimed to collect the opinion of experts working at the frontline involved in emergency dental care during the pandemic. These experts’ statements are supposed to supplement our previous review of the available literature and national as well as international guidelines (Gurzawska‐Comis et al., 2020). All experts selected to participate in this study were based at European Universities.
The transmission risk for aerosol‐free procedures in dental settings was considered to be low or neutral by approximately 55% of the experts, whereas for aerosol‐generating procedures, the vast majority (93%) agreed that the risk was high. Despite of the heterogenic responses related to aerosol‐free procedures, metadata (working environment) could only partially explain the diverse answers. Experts working not exclusively at university hospitals tended to rate the risk of aerosol‐free procedures higher. In contrast, 64% of the experts working at university hospitals considered the risk to be low or neutral. As data could not be matched with the experts’ home country, the association with national COVID‐19 prevalence could not be evaluated.
Among recommended PPE, face shields, gowns, and caps were scored the highest for patients of unknown COVID‐19 risk. FFP2/3 masks were recommended by almost 80% of experts for aerosol‐generating procedures for patients of unknown risk, and experts agreed that FFP2/3 masks, face shields and caps should be used for aerosol‐generating procedures in patients at high or very high risk. Experts suggested that patients with high and very high risk should be treated with FFP2/3 masks, face shields and caps no matter on the type of procedure.
Overshoes and double gloves were judged not useful by the majority of the respondents, and this appraisal may be related to the limited evidence available (Verbeek et al., 2020).
However, proposed PPE measures were more homogenous for aerosol‐generating procedures, whereas higher disagreement was found for aerosol‐free procedures. This might reflect a lack of scientific evidence and unclarity towards the transmission risk during aerosol‐free procedures.
Two thirds of the experts suggested to treat COVID‐19‐positive patients during pandemic only in University Hospitals, while one third suggested to treat them also in private offices. None of the participants considered private practice as the only setting for treating infected patients.
All experts agreed on the importance of reducing aerosol‐generating procedures and 92% of the experts suggested treating COVID‐19‐positive patients in isolation rooms. In contrast, air disinfection was suggested by 60%.
To reduce the number of potentially infected patients in dental settings, a telephone risk assessment was found to be beneficial. However, about one third of the experts did not suggest assessing treatment needs via phone, thus emphasizing the importance of face to face contact during clinical examination. None of the experts suggested that dental care during pandemic should be limited to private practices, and the majority found only dental hospitals to be appropriate. This may be related to the lockdown of dental offices in several European countries when the survey was conducted.
A high percentage of experts recommended wearing of masks by patients in dental settings, even though this preventive measure was not yet recommended by World Health Organization (WHO) during data collection. This may reflect the yearlong experience of dentists being exposed to several infectious disease.
Previous studies related to SARS‐CoV‐1 reported implementation of universal precautions, whenever an aerosol is produced (e.g. preprocedural mouth rinse) (Harrel & Molinari, 2004). The application of infection control strategies is widespread in dentistry and it is a milestone in dental education at universities nowadays (Heinzerling et al., 2020; Oosthuysen et al., 2014).
Since June 5th 2020, community mask wear is recommended by WHO (World Health, 2020). As wearing mask by patients during dental treatment is impossible, mouth wash may reduce the viral load. Indeed, 80% of experts recommended this measure even before it was recommended by WHO. However, very few studies exist on the efficacy and substantivity of mouth rinses to eliminate viral load during treatment (Carrouel et al., 2020; Peng et al., 2020).
In summary, experts’ recommendations revealed high agreement, especially for PPE measures during aerosol‐generating procedures. This underlines the importance of face protection using FFP2/3 masks, shields and caps as well as reduction of aerosol‐generating procedures.
The survey population was intended to represent the opinion of European experts facing dental emergencies during pandemic. As the majority of the emergencies are provided by Oral Surgery or Oral and Maxillofacial Surgery departments (Scottish Dental Clinical Effectiveness Programme, 2007), the respective heads or professors were selected to be included. Some countries had very few dental schools. Thus, considering more than one expert vote per country would have required aggregation to prevent imbalance. In addition, the respective question for the origin would have been in conflict with our anonymous approach in small countries (i.e. making it impossible to allocate experts and answers). Therefore, to ensure homogenous representativity, one expert vote was permitted per country only. In addition, all experts were selected independently of age and gender.
Limitations associated with the present study include that the impact of national guidelines and local regulations on experts’ answers could not be assessed owing to the anonymous approach. Moreover, the survey was performed during an exponential growth phase (6 weeks), in which experts might have adapted to the situation. Furthermore, the present recommendations were collected when only emergency care was provided in most of the countries. Due to the similarity between emergency and other elective oral surgery treatments, the present recommendations can be applied in implant dentistry. As general dental practitioners and specialists (endodontists, orthodontists, periodontists, prosthodontics) providing elective treatments are now re‐opening their offices, larger‐scaled surveys will be possible in the near future. They may include further questions on the relevance of qualitative and quantitative testing for COVID‐19, novel high‐efficiency particulate air (HEPA) filtration devices for dental offices, or high‐power suction.
In conclusion, the infection and transmission risk in dental settings was scored to be particular high. For aerosol‐generating procedures and patients at high/very high risk, maximum PPE use was recommended. Whereas the proposed measures (i.e. FFP2/3 masks, caps, gowns and face protection) may reduce the transmission risk in dental hospitals, future survey should be conducted among a larger population of dentists as well as among experts in virology and infection control. In the future, also in vitro experiments and epidemiological studies would reveal valuable information about the transmission risk associated with the specific dental procedures. Finally, future risk assessment might include additional factors, such as the current prevalence per 100,000 inhabitants, age distribution of the patients, and social and economical status.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest related to this study.
AUTHOR CONTRIBUTION
Kathrin Becker: Conceptualization (equal); Data curation (equal); Formal analysis (equal); Investigation (equal); Methodology (equal); Project administration (lead); Resources (equal); Writing‐original draft (equal); Writing‐review & editing (equal). Giulia Brunello: Conceptualization (equal); Data curation (equal); Investigation (equal); Methodology (equal); Resources (equal); Writing‐original draft (equal); Writing‐review & editing (equal). Katarzyna Gurzawska‐Comis: Conceptualization (equal); Data curation (equal); Investigation (equal); Methodology (equal); Project administration (equal); Resources (equal); Writing‐original draft (equal); Writing‐review & editing (equal). Stefano Sivolella: Methodology (equal); Supervision (equal); Writing‐review & editing (equal). Frank Schwarz: Conceptualization (equal); Supervision (equal); Writing‐review & editing (equal). Bjorn Klinge: Conceptualization (equal); Methodology (equal); Supervision (equal); Validation (equal); Writing‐review & editing (equal).
Supporting information
Supplementary Material
ACKNOWLEDGEMENTS
The authors would like to acknowledge Dr. Agata Gurzawska (Trilateral Research Ireland, Dublin, Ireland) and Prof. Thomas Dietrich (University of Birmingham, Birmingham, UK) who helped during survey preparation, and the authors also like to thank the following experts (in alphabetic order) for their participation in the survey: Prof. Massimo Albanese (University of Verona, Verona, Italy); Prof. Ricardo F. Almeida (University of Porto, Porto, Portugal); Prof. Athanasios E. Athanasiou (European University Cyprus, Nicosia, Cyprus); Prof. Jonas P. Becktor (Malmö University, Malmö, Sweden); Prof. Dr. Fred Bergmann (University for Digital Technologies in Medicine and Dentistry, Wiltz, Luxembourg); Prof. Alexandru Bucur (Carol Davila University of Medicine and Pharmacy, Bucharest, Romania); Dr. Alex Cassar (University of Malta, Msida, Malta); Prof. Titiaan Dormaar (Universitair Ziekenhuis Leuven, Leuven, Belgium); Dr. Veronica Fisher (Trinity College Dublin, Dublin, Ireland); Dr. Cecilia Gjerde (University of Bergen, Bergen, Norway); Prof. Klaus Gotfredsen (University of Copenhagen, Copenhagen, Denmark); Prof. Natasa I. Hren (University of Ljubljana, Ljubljana, Slovenia); Prof. Oksana Ivask (University of Tartu, Tartu, Estonia); Prof. Jochen Jackowski (Witten‐Herdecke University, Witten, Germany); Prof. Ricardas Kubilius (Lithuanian University of Health Sciences, Kaunas, Lithuania); Prof. Darko Macan (University of Zagreb, Zagreb, Croatia); Prof. Radovan Mottl (Charles University in Prague, Prague, Czech Republic); Prof. Nikolaos Nikitakis (National and Kapodistrian University of Athens, Athens, Greece); Dr. Victor Palarie (State University for Medicine and Pharmaceutics, Chisinau, Moldova); Dr. Vinod Patel (King's College London, London, UK); Prof. Michael Payer (Medical University of Graz, Graz, Austria); Prof. Miguel Peñarrocha (University of Valencia, Valencia, Spain); Prof. Bjarni E. Pjetursson (University of Iceland, Reykjavík, Iceland); Prof. Pawel Plakwicz (Medical University of Warsaw, Warsaw, Poland); Prof. Tero Soukka (University of Turku, Turku, Finland); Prof. Ali Tahmaseb (Academisch Centrum Tandheelkunde Amsterdam – ACTA, Amsterdam, Netherlands); Prof. Florian Thieringer (University of Basel, Switzerland). Open access funding enabled and organized by ProjektDEAL.
Becker K, Brunello G, Gurzawska‐Comis K, et al. Dental care during COVID‐19 pandemic: Survey of experts’ opinion. Clin Oral Impl Res. 2020;31:1253–1260. 10.1111/clr.13676
Kathrin Becker, Giulia Brunello, Katarzyna Gurzawska‐Comis contributed equally to this work.
Stefano Sivolella, Frank Schwarz, and Björn Klinge contributed equally to this work.
REFERENCES
- Ather, A. , Patel, B. , Ruparel, N. B. , Diogenes, A. , & Hargreaves, K. M. (2020). Coronavirus Disease 19 (COVID‐19): Implications for Clinical Dental Care. Journal of Endodontics, 46(5), 584–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkins, D. , Best, D. , Briss, P. A. , Eccles, M. , Falck‐Ytter, Y. , Flottorp, S. , & Zaza, S. (2004). Grading quality of evidence and strength of recommendations. BMJ, 328(7454), 1490. 10.1136/bmj.328.7454.1490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrouel, F. , Conte, M. P. , Fisher, J. , Gonçalves, L. S. , Dussart, C. , Llodra, J. C. , & Bourgeois, D. (2020). COVID‐19: A Recommendation to Examine the Effect of Mouthrinses with β‐Cyclodextrin Combined with Citrox in Preventing Infection and Progression. J Clin Med, 9(4) , 1126. 10.3390/jcm9041126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coulthard, P. (2020). Dentistry and coronavirus (COVID‐19) ‐ moral decision‐making. British Dental Journal, 228(7), 503–505. 10.1038/s41415-020-1482-1 [DOI] [PubMed] [Google Scholar]
- Gurzawska‐Comis, K. , Becker, K. , Brunello, G. , Gurzawska, A. , & Schwarz, F. (2020). Recommendations for Dental Care during COVID‐19 Pandemic. J Clin Med, 9(6), 1833. 10.3390/jcm9061833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrel, S. K. , & Molinari, J. (2004). Aerosols and splatter in dentistry: A brief review of the literature and infection control implications. Journal of the American Dental Association, 135(4), 429–437. 10.14219/jada.archive.2004.0207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinzerling, A. , Stuckey, M. J. , Scheuer, T. , Xu, K. , Perkins, K. M. , Resseger, H. , Magill, S. , Verani, J. R. , Jain, S. , Acosta, M. , & Epson, E. (2020). Transmission of COVID‐19 to health care personnel during exposures to a hospitalized patient ‐ solano County, California, february 2020. MMWR. Morbidity and Mortality Weekly Report, 69(15), 472–476. 10.15585/mmwr.mm6915e5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Izzetti, R. , Nisi, M. , Gabriele, M. , & Graziani, F. (2020). COVID‐19 transmission in dental practice: brief review of preventive measures in Italy. Journal of Dental Research, 99(9), 1030–1038. 10.1177/0022034520920580 [DOI] [PubMed] [Google Scholar]
- Kelly, K. , Clark, B. , Brown, V. , & Sitzia, J. (2003). Good practice in the conduct and reporting of survey research. International Journal for Quality in Health Care, 15(3), 261–266. 10.1093/intqhc/mzg031 [DOI] [PubMed] [Google Scholar]
- Majumder, M. , & Mandl, K. D. (2020). Early Transmissibility Assessment of a Novel Coronavirus in Wuhan, China SSRN . 10.2139/ssrn.3524675 [DOI] [Google Scholar]
- Meng, L. , Hua, F. , & Bian, Z. (2020). Coronavirus disease 2019 (COVID‐19): emerging and future challenges for dental and oral medicine. Journal of Dental Research, 99(5), 481–487. 10.1177/0022034520914246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oosthuysen, J. , Potgieter, E. , & Fossey, A. (2014). Compliance with infection prevention and control in oral health‐care facilities: A global perspective. International Dental Journal, 64(6), 297–311. 10.1111/idj.12134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan, Y. , Liu, H. , Chu, C. , Li, X. , Liu, S. , & Lu, S. (2020). Transmission routes of SARS‐CoV‐2 and protective measures in dental clinics during the COVID‐19 pandemic. American Journal of Dentistry, 33(3), 129–134. [PubMed] [Google Scholar]
- Peng, X. , Xu, X. , Li, Y. , Cheng, L. , Zhou, X. , & Ren, B. (2020). Transmission routes of 2019‐nCoV and controls in dental practice. Int J Oral Sci, 12(1), 9. 10.1038/s41368-020-0075-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren, Y. F. , Rasubala, L. , Malmstrom, H. , & Eliav, E. (2020). Dental Care and Oral Health under the Clouds of COVID‐19. JDR Clin Trans Res, 5(3), 202–210. 10.1177/2380084420924385 [DOI] [PubMed] [Google Scholar]
- Scottish Dental Clinical Effectiveness Programme (2007). Emergency Dental Care. Retrieved from http://www.sdcep.org.uk/wp‐content/uploads/2013/03/EDC+Guidance.pdf. [Google Scholar]
- Verbeek, J. H. , Rajamaki, B. , Ijaz, S. , Sauni, R. , Toomey, E. , Blackwood, B. , Tikka, C. , Ruotsalainen, J. H. , & Kilinc Balci, F. S. (2020). Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff. Cochrane Database Systematic Review, 4(4), Cd011621. 10.1002/14651858.CD011621.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health, O (2014). WHO handbook for guideline development (2nd, ed.). World Health Organization. [Google Scholar]
- World Health, O (2020). Advice on the use of masks in the context of COVID‐19: Interim guidance, 5 June 2020. Retrieved from Geneva: https://apps.who.int/iris/handle/10665/332293. [Google Scholar]
- Zimmermann, M. , & Nkenke, E. (2020). Approaches to the management of patients in oral and maxillofacial surgery during COVID‐19 pandemic. Journal of Cranio‐Maxillo‐Facial Surgery, 48(5), 521–526. 10.1016/j.jcms.2020.03.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


