Abstract
BACKGROUND
It is crucial that nursing homes have adequate personal protective equipment (PPE) and staff to protect residents and staff from COVID‐19. Some states have taken actions to mitigate shortages of PPE and staffing in nursing homes, including creating dedicated long‐term care (LTC) teams and supporting staffing capacity.
OBJECTIVE
To examine whether state actions and nursing home characteristics are associated with shortages of PPE and staffing.
DESIGN AND SETTING
Facility‐level data, released July 31, 2020, from the Nursing Home COVID‐19 Public File, were combined with data from other sources. Our sample was the 13,445 facilities with information about PPE and staffing shortages for each of the 5 weeks between the week ending June 21, 2020, and the week ending July 19, 2020. Associations between facility characteristics and shortages were examined using descriptive statistics and logistic regression models.
MEASUREMENTS
Outcome variables were whether or not a facility lacked a 1‐week supply of PPE (“PPE shortage”) and whether or not a facility had a staffing shortage during 1 or more weeks over the 5‐week study period.
RESULTS
Over the 5‐week study period, 27.6% of facilities reported 1 or more weeks of PPE shortage, 30.2% of facilities reported at least 1 week of staffing shortage, and 46.5% of facilities lacked PPE and/or staff. Facilities located in states in the Northeast PPE Consortium or with LTC teams were modestly less likely to have had a PPE shortage, and facilities located in states that implemented processes to match job seekers with LTC facilities were marginally significantly less likely to have had a staffing shortage.
CONCLUSION
Given that nearly half of U.S. nursing homes recently faced a shortage of PPE and/or staff, and that state budget deficits may limit further state actions, ongoing federal assistance with PPE and staffing of nursing homes is needed.
Keywords: nursing homes, COVID‐19, personal protective equipment, staffing
INTRODUCTION
As of early September 2020, over 75,000 COVID‐19–related deaths had occurred in U.S. nursing homes and other long‐term care (LTC) facilities. 1 There is substantial variation across states in the percentage of COVID‐19 deaths linked to nursing homes, assisted living centers, and other LTC facilities. Three‐quarters or more of COVID‐19 deaths in Rhode Island and New Hampshire were in LTC facilities compared with only 16% in Nevada. 1 This level of variation suggests that policies and practices may influence the extent to which COVID‐19 impacts facilities.
Key to protecting nursing homes, according to both the Centers for Disease Control and Prevention (CDC) and the Centers for Medicare and Medicaid Services (CMS), is having adequate supplies of personal protective equipment (PPE), staffing, and COVID‐19 tests. 2 , 3 Shortages of PPE, staffing, and testing have likely exacerbated transmission of COVID‐19 in nursing homes. 4 Using the most recent week of information available for each Medicare‐ or Medicaid‐certified skilled nursing home from the Nursing Home COVID‐19 Public File for the period between June 24, 2020, and July 19, 2020, McGarry et al found that 19.1% of nursing homes had less than a 1‐week supply of at least one type of PPE and 21.9% reported staffing shortages. 2 , 5
Federal and state efforts have sought to reduce shortages of PPE, staffing, and testing in nursing homes. In May 2020, the federal government began sending nursing homes two 1‐week shipments of PPE, although there were reports that the supplies were inadequate in number and in quality. 6 In late August 2020, the federal government authorized the provision of a 1‐week supply of N95 masks to approximately 3,330 nursing homes that reported having less than a 3‐day supply of N95 masks. 7 Additionally, in March 2020, the federal government waived the training requirement for nurseʼs aides and in mid‐July 2020 began shipping rapid point‐of‐care diagnostic test instruments and tests to nursing homes in areas that the CDC has designated as COVID‐19 hot spots. 8 , 9 , 10
At the state level, seven states in the Northeast formed a consortium to develop a regional supply chain for PPE, other medical equipment, and testing. 11 Almost half of all states (n = 22) have created dedicated teams to support LTC facilities. According to the National Governors Association, “the specific charge and composition of teams vary, but typically involve support with infection control, staffing, testing, PPE and other supply needs.” 9 Twenty‐three states have implemented policies to support staffing capacity, including increasing pay for staff, enabling individuals to serve in critical roles without certification, and developing systems to match job seekers with LTC providers. 8 , 9 Twenty‐two states have provided additional funding to LTC facilities through Medicaid or other mechanisms. 9
This article builds on McGarry et al by considering whether state actions are associated with shortages of PPE and staffing in U.S. nursing homes. 5 Additionally, this article examines whether and how often nursing homes had a shortage of PPE or staffing over a 5‐week period from mid‐June to mid‐July 2020, offering insight into the extent of shortages faced by facilities over time. Although CMS requires nursing homes to report whether residents have access to on‐site testing, testing shortages are not considered in this article because CMS does not collect information about whether facilities have access to an adequate supply of tests.
METHODS
Data
Skilled nursing home facility‐level data from the Nursing Home COVID‐19 Public File 2 (data released July 31, 2020) were combined with facility‐level data from Nursing Home Compare (data released June 4, 2020) 12 and Brown Universityʼs LTCFocus.org (2017 data), 13 county‐level data from the 2019 Area Health Resources File and the New York Times Coronavirus Case Data, 14 and state‐level information from the National Governors Association. 15 Our sample was the set of facilities with information about shortages of five types of PPE (N95 masks, surgical masks, gowns, gloves, and eye protection) and four types of staff (nursing staff, clinical staff, healthcare aides, and other types of staff) for each of the 5 weeks between the week ending June 21, 2020, and the week ending July 19, 2020, and that reported information about the number of COVID‐19 cases among residents for the weeks of May 24 and June 14, 2020 (n = 13,445 of 15,388 Medicare‐ or Medicaid‐certified nursing homes in the Nursing Home COVID‐19 Public File).
Measures
The main outcome variables were whether or not a facility lacked a 1‐week supply of any type of PPE (“PPE shortage”) and whether or not a facility had any type of staffing shortage during 1 or more weeks over the 5‐week period. Hand sanitizer was included in the definition of PPE in supplemental analyses. Explanatory variables for state policy actions included whether or not a facility was located in one of the seven states that are part of the Northeast PPE Consortium, 11 one of the 13 states that created dedicated LTC support teams with responsibilities in addition to testing, 9 one of the 23 states that developed enhanced LTC workforce supports, 9 and one of the 22 states that expanded Medicaid payments or other funding to LTC facilities. 9 LTC workforce supports were further characterized as adjustments to licensing, certification, and training requirements (nine states), increased payments and other incentives for staff (nine states), and systems or processes to match job seekers to LTC facilities with staffing needs (10 states). 9 Other key explanatory variables included facility size, ownership, share of facility revenue from Medicaid, whether greater than 25% of residents were Black, and the CMS Overall Five Star Rating. 15 , 16 , 17 The full set of explanatory variables is listed in Table 2.
Table 2.
Logistic Regression Models of Nursing Homes with PPE Shortage and Staffing Shortage, June 15 through July 19, 2020 (n = 13,445)
| Variable | Short PPE at Least 1 wk | Short staff at least 1 wk | ||
|---|---|---|---|---|
| Odds Ratio | P value | Odds Ratio | P value | |
| State in which facility is located | ||||
| In Northeast PPE Consortium | ||||
| No | [1.00] | |||
| Yes | 0.82 | .021 | ||
| Has LTC teams with a focus beyond testing | ||||
| No | [1.00] | [1.00] | ||
| Yes | 0.82 | .035 | 0.72 | .170 |
| Expanded Medicaid payments to LTC | ||||
| No | [1.00] | [1.00] | ||
| Yes | 1.20 | .108 | 1.01 | .939 |
| Adjusted LTC licensing or training requirements | ||||
| No | [1.00] | |||
| Yes | 0.89 | .473 | ||
| Increased payments or incentives for LTC staff | ||||
| No | [1.00] | |||
| Yes | 0.89 | .623 | ||
| Offers LTC job match assistance | ||||
| No | [1.00] | |||
| Yes | 0.70 | .064 | ||
| County in which facility is located | ||||
| Change in COVID‐19 cases per 100,000 population between May 24, 2020, and June 14, 2020 | 1.00 | .184 | 1.00 | .435 |
| Population >75% urban | ||||
| No | [1.00] | [1.00] | ||
| Yes | 0.95 | .493 | 0.70 | <.000 |
| Nursing home characteristics | ||||
| Nursing home size | ||||
| Small (<50 beds) | [1.00] | [1.00] | ||
| Medium (≥50 and ≤150 beds) | 0.94 | .495 | 0.99 | .960 |
| Large (>150 beds) | 0.97 | .792 | 1.02 | .834 |
| Ownership | ||||
| Nonprofit | [1.00] | [1.00] | ||
| Government | 0.86 | .306 | 1.22 | .149 |
| For profit | 1.46 | <.001 | 1.05 | .619 |
| Chain status | ||||
| Not part of a chain | [1.00] | [1.00] | ||
| Part of a chain | 1.03 | .600 | 0.90 | .058 |
| In‐hospital status | ||||
| Free standing | [1.00] | [1.00] | ||
| Part of a hospital | 0.67 | .015 | 0.80 | .109 |
| Share of revenue from Medicaid (quartiles) | ||||
| 1 (Lowest) | [1.00] | [1.00] | ||
| 2 | 1.03 | .673 | 1.08 | .259 |
| 3 | 0.98 | .853 | 1.09 | .385 |
| 4 (Highest) | 0.96 | .653 | 1.28 | .001 |
| Black residents >25% of all residents | ||||
| No | [1.00] | [1.00] | ||
| Yes | 0.89 | .068 | 1.36 | .003 |
| CMS overall five‐star rating | ||||
| Missing rating | 0.79 | .239 | 1.16 | .447 |
| 1 (Lowest) | 0.95 | .676 | 1.57 | <.001 |
| 2 | 1.02 | .837 | 1.32 | <.001 |
| 3 | 0.99 | .900 | 1.20 | <.001 |
| 4 | 1.06 | .394 | 1.10 | .104 |
| 5 (Highest) | [1.00] | [1.00] | ||
| Change in COVID‐19 cases per bed between May 24, 2020, and June 14, 2020 | 0.68 | .318 | 4.45 | <.001 |
| Information from LTCFocus.org missing | ||||
| No | [1.00] | [1.00] | ||
| Yes | 1.12 | .493 | 0.99 | .978 |
Note: The logistic regression models were estimated using robust standard errors clustered at the state level. Information from LTCfocus.org (chain status, in‐hospital status, Medicaid revenue quartile, and Black resident share) was missing for 754 facilities. Facilities missing LTCfocus information were assigned a value of zero for these variables, and the models included an indicator variable for missing LTCfocus information.
Abbreviations: CMS, Centers for Medicare and Medicaid Services; LTC, long‐term care; PPE, personal protective equipment.
Statistical Analyses
The percentage of facilities with a shortage in each week of the 5‐week study period was calculated for facilities included in the sample and for facilities excluded from the sample that reported shortage information in at least 1 week over the 5‐week period. Other characteristics of facilities included and excluded from the sample were also compared. Associations between nursing home characteristics and whether or not a facility had a shortage during at least 1 week over the 5‐week study period were examined using descriptive statistics and logistic regression models with robust standard errors clustered at the state level.
RESULTS
In each week of the 5‐week study period, between 16.8% and 18.8% of facilities included in the sample had a PPE shortage, between 20.2% and 21.8% had a staffing shortage, and between 32.4% and 34.3% had a shortage of PPE and/or staff (Figure 1). The percentage of facilities with a shortage of each type in each week was similar for facilities excluded from the sample, with the exception of the percentage of facilities reporting a PPE shortage during the week ending July 19 (Supplementary Table S1). Additionally, excluded facilities were more likely to be small, to be for profit or government owned, to have a higher percentage of Black residents and lower five‐star quality ratings, and to be located in highly urban areas and in states that did not increase payments or incentives for LTC staff or expand Medicaid payments.
Figure 1.
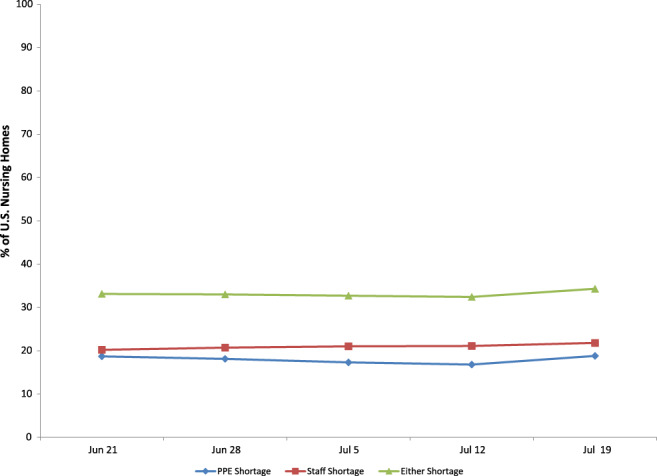
Percentage of U.S. nursing homes with weekly personal protective equipment (PPE) and staffing shortages over the weeks ending June 21 through July 19, 2020 (n = 13,445).
There was variation over time in which facilities had shortages; 27.6% of facilities were missing a weekʼs supply of PPE during at least 1 week over the 5‐week study period, and 30.1% of facilities reported a staffing shortage during at least 1 week (Table 1). PPE shortages were most likely for N95 masks and gowns, and staffing shortages were most common for health aides and nursing staff. Of facilities, 46% had a PPE shortage and/or a staffing shortage in at least 1 week over the 5‐week period and 11.7% had a PPE shortage and 14.8% had a staffing shortage in every week of the study period.
Table 1.
Shortages of PPE and Staff in Nursing Homes in the United States, June 15 through July 19, 2020 (n = 13,445)
| Variable | No. of weeks nursing home has shortage of PPE or staff | |||
|---|---|---|---|---|
| 0 | 1 | 2–4 | 5 | |
| Personal protective equipment and hand sanitizer | ||||
| N95 masks | 79.4 | 5.9 | 6.4 | 8.3 |
| Surgical masks | 87.2 | 6.3 | 3.2 | 3.2 |
| Gowns | 81.9 | 5.9 | 5.8 | 6.4 |
| Gloves | 91.9 | 3.8 | 2.4 | 1.9 |
| Eye protection | 88.0 | 6.1 | 2.8 | 3.1 |
| Hand sanitizer | 91.5 | 4.0 | 2.3 | 2.2 |
| Any type of PPE | 72.4 | 7.7 | 8.2 | 11.7 |
| Any type of PPE or hand sanitizer | 71.4 | 8.1 | 8.5 | 12.0 |
| Staff | ||||
| Nursing staff | 76.6 | 6.7 | 7.2 | 9.5 |
| Clinical staff | 92.6 | 5.0 | 1.7 | 0.7 |
| Aides | 73.7 | 6.8 | 7.8 | 11.7 |
| Other staff | 83.4 | 6.9 | 5.4 | 4.3 |
| Any type of staff | 69.9 | 7.2 | 8.1 | 14.8 |
Note: Data are given as percentages. Shortage of PPE means not having enough for 1 week. Nursing staff includes registered nurses, licensed practical nurses, and vocational nurses. Clinical staff includes physicians, physician assistants, and advanced practice nurses. Aides include certified nursing assistants, nurse aides, medication aides, and medication technicians.
Abbreviation: PPE, personal protective equipment.
Descriptive statistics are shown in Supplementary Table S2. In the PPE shortage logistic regression model (Table 2), nursing homes were less likely to have a shortage if they were located in a state in the Northeast PPE Consortium (odds ratio (OR) = 0.82; 3.7 percentage points (pp) less than facilities in states not in the Northeast PPE Consortium; P = .021) or in a state with LTC teams (OR = 0.82; 3.9 pp less than facilities in states without LTC teams; P = .035). Expanded Medicaid payments were not significantly associated with PPE shortages. For‐profit ownership and location outside of a hospital were also associated with a significantly higher likelihood of a PPE shortage.
In the staffing shortage regression model (Table 2), location in a state that implemented a process to match job seekers with LTC facilities was associated with a marginally significantly lower likelihood of a shortage (OR = 0.70; 7.1 pp less than facilities in states without a matching process; P = .064). State LTC teams, other workforce supports, and expanded Medicaid payments were not significantly associated with staffing shortages. Location in a less urban county, being in the highest quartile of revenue from Medicaid, and having greater than 25% of residents who were Black, a five‐star rating lower than four stars, and a greater recent increase in COVID‐19 cases per bed were also associated with a significantly higher likelihood of a staffing shortage.
DISCUSSION
Almost half of facilities reported a shortage of PPE and/or staffing during at least 1 week over the 5‐week study period. This percentage is substantially higher than the roughly 33% of facilities that reported a shortage of PPE and/or staffing in a given week, and it demonstrates the sizeable variation over time in which facilities face shortages. However, there is some persistence in shortages, as more than 1 in 10 facilities faced shortages of PPE or staffing during each week of the 5‐week study period. These findings suggest that the recent federal government shipment of a 1‐week supply of N95 masks to nursing homes with a severe N95 shortage will provide only a partial and temporary remedy to the shortages facing nursing homes.
The most direct measure of nursing home quality used in this study, the CMS Overall Five Star Rating, was not associated with PPE shortages but was associated with staffing shortages. High concentrations of residents who were Black or who had Medicaid as the primary payer were also associated with staffing shortages. Although for‐profit status was associated with PPE shortages, other nursing home characteristics associated with lower quality in prior research were not significant predictors of PPE shortages. 15 , 16 , 17 The findings suggest that difficulty acquiring PPE is a problem faced by a range of facilities, not solely those with quality‐of‐care issues, and that difficulty maintaining staffing levels is more closely linked to lower‐quality facilities. These findings are similar to those of McGarry et al for their June 24, 2020, to July 19, 2020, study period, which is encompassed by the study period used in this article. 5
We find that state actions were associated with slightly lower PPE and staffing shortages in nursing homes. Nursing homes located in states in the Northeast PPE Consortium or with LTC teams were statistically significantly less likely to have had a PPE shortage compared with facilities in other states, although the difference was modest. Facilities located in states that implemented processes to match job seekers with LTC facilities were less likely to have had a staffing shortage, although the association was marginally significant. It is important to note the preliminary nature of these estimates given that a substantial number of facilities did not report complete shortage information and that facility characteristics differed between facilities included and excluded from the sample. Additionally, information was not included in the analyses on other actions that have been taken by states, local governments, or other actors, such as professional associations and nonprofit organizations, to help alleviate PPE or staffing shortages in nursing homes, which could bias associations between the measured state actions and the shortage outcomes.
CONCLUSION
Nearly half of the nursing homes across the country continue to struggle to secure PPE and adequately staff their facilities, both of which are essential to keeping residents and staff protected from COVID‐19. Several state actions to help nursing homes prevent shortages of PPE and staff are associated with modest reductions in the likelihood of these types of shortages. However, the COVID‐19 pandemic has left states facing enormous budget deficits. 18 In such an environment, it is likely to be difficult for states to sustain or additional states to replicate these efforts. These findings provide support for the need for ongoing federal assistance with PPE and staffing to help ensure the safety of nursing home residents and staff.
Supporting information
Supplementary Table S1: Characteristics of Nursing Homes by Completeness of Data on Personal Protective Equipment and Staffing Shortages
Supplementary Table S2: Characteristics of Nursing Homes by Shortages of Personal Protective Equipment and Staff
ACKNOWLEDGMENTS
Conflict of Interest
The authors have no conflicts.
Author Contributions
Both authors contributed equally to the study concept and design, acquisition of data, analysis and interpretation of data, and preparation of the manuscript.
Sponsorʼs Role
This study did not receive financial support.
REFERENCES
- 1. Kaiser Family Foundation . State data and policy actions to address coronavirus. September 14. https://www.kff.org/health-costs/issue-brief/state-data-and-policy-actions-to-address-coronavirus/#long-term-care-cases-deaths. Published 2020. Accessed September 14, 2020.
- 2. Centers for Disease Control and Prevention . Preparing for COVID‐19 in nursing homes. https://www.cdc.gov/coronavirus/2019-ncov/hcp/long-term-care.html. Published May 19, 2020. Accessed September 14, 2020.
- 3. Director Quality, Safety & Oversight Group . Nursing home reopening recommendations for state and local officials. Centers for Medicare and Medicaid Services. https://www.cms.gov/files/document/qso-20-30-nh.pdf. Published May 18, 2020. Accessed September 14, 2020.
- 4. Berklan J. McKnightʼs COVID survey reveals vast PPE, staffing shortages. McKnightʼs Long Term Care News . https://www.mcknights.com/news/mcknights-covid-survey-reveals-vast-ppe-staffing-shortages/. Published March 30, 2020. Accessed September 14, 2020.
- 5. McGarry BE, Grabowski DC, Barnett ML. Severe staffing and personal protective equipment shortages faced by nursing homes during the COVID‐19 pandemic. Health Aff August. 2020;39(10):1812‐1821. 10.1377/hlthaff.2020.01269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Abbasi J. “Abandoned” nursing homes continue to face critical supply and staff shortages as COVID‐19 toll has mounted. JAMA. 2020;324:123. 10.1001/JAMA.2020.10419. [DOI] [PubMed] [Google Scholar]
- 7. HHS Press Office . Trump Administration to release 1.5 million N95 respirators from the strategic national stockpile for distribution to nursing homes. 2020. https://www.hhs.gov/about/news/2020/08/25/trump‐administration‐release‐1‐5‐million‐n95‐respirators‐from‐strategic‐national‐stockpile‐distribution‐nursing‐homes.html. Accessed September 14, 2020.
- 8. Hauslohner A, Sacchetti M. Nursing homes turn to quick fix training to meet pandemic staffing needs. The Washington Post . https://www.washingtonpost.com/national/nursing‐homes‐turn‐to‐quick‐fix‐training‐to‐meet‐pandemic‐staffing‐needs/2020/05/28/418c3802‐a020‐11ea‐9590‐1858a893bd59_story.html. Published May 28, 2020. Accessed September 14, 2020.
- 9. McBride B. Strategies for COVID‐19 response for populations receiving long‐term care. https://www.nga.org/wp-content/uploads/2020/06/Strategies-for-COVID-19-Response-for-Populations-Receiving-Long-Term-Care.pdf. Published July 13, 2020. Accessed September 14, 2020.
- 10. HHS Press Office . Trump Administration announces initiative for more and faster COVID‐19 testing in nursing homes. https://www.hhs.gov/about/news/2020/07/14/trump-administration-announces-initiative-more-faster-covid-19-testing-nursing-homes.html. Published 2020. Accessed September 14, 2020.
- 11. Governor Andrew M. Cuomo. Amid ongoing COVID‐19 pandemic, Governor Cuomo announces joint multi‐state agreement to develop regional supply chain. https://www.governor.ny.gov/news/video-audio-photos-rush-transcript-amid-ongoing-covid-19-pandemic-governor-cuomo-announces-18. Published 2020. Accessed September 14, 2020.
- 12. Centers for Medicare and Medicaid Services . Nursing Home Compare datasets. 2020. https://data.medicare.gov/data/nursing-home-compare. Accessed September 14, 2020.
- 13. Brown University . Shaping Long Term Care in America Project at Brown University funded in part by the National Institute on Aging (1P01AG027296). LTCFocus.org. Published 2020. Accessed September 14, 2020.
- 14. The New York Times . Weʼre sharing coronavirus case data for every U.S. county. The New York Times . https://www.nytimes.com/article/coronavirus-county-data-us.html?action=click&module=Spotlight&pgtype=Homepage. Published March 28, 2020. Accessed September 14, 2020.
- 15. Boccuti C, Casillas G, Neuman T. Reading the stars: nursing home quality star ratings, nationally and by state; 2015. https://www.kff.org/medicare/issue‐brief/reading‐the‐stars‐nursing‐home‐quality‐star‐ratings‐nationally‐and‐by‐state/. Accessed September 14, 2020.
- 16. You K, Li Y, Intrator O, et al. Do nursing home chain size and proprietary status affect experiences with care? Med Care. 2016;54(3):229‐234. 10.1097/MLR.0000000000000479. Accessed September 14, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mor V, Zinn J, Angelelli J, Teno JM, Miller SC. Driven to tiers: socioeconomic and racial disparities in the quality of nursing home care. Milbank Q. 2004;82(2):227‐256. 10.1111/j.0887-378X.2004.00309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mulvihill G. No federal relief leaves states, cities facing big deficits. Associated Press . https://apnews.com/da0b410202ef725cc9a32c41d5ac810e. Published August 10, 2020. Accessed September 14, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1: Characteristics of Nursing Homes by Completeness of Data on Personal Protective Equipment and Staffing Shortages
Supplementary Table S2: Characteristics of Nursing Homes by Shortages of Personal Protective Equipment and Staff


