Abstract
Concerns have been expressed that persons with a pre‐existing mental disorder may represent a population at increased risk for COVID‐19 infection and with a higher likelihood of adverse outcomes of the infection, but there is no systematic research evidence in this respect. This study assessed the impact of a recent (within past year) diagnosis of a mental disorder – including attention‐deficit/hyperactivity disorder (ADHD), bipolar disorder, depression and schizophrenia – on the risk for COVID‐19 infection and related mortality and hospitalization rates. We analyzed a nation‐wide database of electronic health records of 61 million adult patients from 360 hospitals and 317,000 providers, across 50 states in the US, up to July 29, 2020. Patients with a recent diagnosis of a mental disorder had a significantly increased risk for COVID‐19 infection, an effect strongest for depression (adjusted odds ratio, AOR=7.64, 95% CI: 7.45‐7.83, p<0.001) and schizophrenia (AOR=7.34, 95% CI: 6.65‐8.10, p<0.001). Among patients with a recent diagnosis of a mental disorder, African Americans had higher odds of COVID‐19 infection than Caucasians, with the strongest ethnic disparity for depression (AOR=3.78, 95% CI: 3.58‐3.98, p<0.001). Women with mental disorders had higher odds of COVID‐19 infection than males, with the strongest gender disparity for ADHD (AOR=2.03, 95% CI: 1.73‐2.39, p<0.001). Patients with both a recent diagnosis of a mental disorder and COVID‐19 infection had a death rate of 8.5% (vs. 4.7% among COVID‐19 patients with no mental disorder, p<0.001) and a hospitalization rate of 27.4% (vs. 18.6% among COVID‐19 patients with no mental disorder, p<0.001). These findings identify individuals with a recent diagnosis of a mental disorder as being at increased risk for COVID‐19 infection, which is further exacerbated among African Americans and women, and as having a higher frequency of some adverse outcomes of the infection. This evidence highlights the need to identify and address modifiable vulnerability factors for COVID‐19 infection and to prevent delays in health care provision in this population.
Keywords: COVID‐19, mental disorders, risk of infection, mortality, hospitalization, depression, schizophrenia, ADHD, bipolar disorder, ethnic disparity, gender disparity, access to care, discrimination
COVID‐19 infection has rapidly escalated into a global pandemic, with more than 33 million cases and one million deaths worldwide as to September 30, 2020 1 . Socioeconomic deprivation, older age, and several medical conditions are associated with increased risk for severe COVID‐19 disease2, 3, 4, 5.
Mental disorders are estimated to affect 20‐25% of the adult population (450 million globally, 47 million in US) 6 , and their incidence is likely to have increased during the pandemic, due to a variety of factors7, 8. Concerns have been expressed that persons with a pre‐existing mental disorder may represent a population with an increased risk for COVID‐19 infection, and in which the outcomes of the infection are worse7, 8, 9, 10.
Multiple factors have been described that could increase the risk of persons with mental disorders to get COVID infection, or make the outcomes of the infection worse. These include challenges in appraising health information and complying with preventive behaviors, limitations in access to health care, homelessness or living in settings where the risk for contagion is higher 10 , and the higher prevalence of comorbid medical conditions that are associated with increased risk for COVID‐19 severe illness (such as cardiovascular diseases, cancers, and chronic obstructive pulmonary disease). Despite the recognition of these multiple vulnerability factors, the risk for COVID‐19 infection and its outcomes among patients with mental disorders have not been investigated systematically.
Ethnic disparities in mental health and mental health care have been repeatedly documented, especially among minority populations in the US, such as African Americans11, 12, 13. Gender is also a critical determinant of mental health, due to the differential power and control of men and women over the socioeconomic determinants of their lives, and the different exposure and susceptibility to specific mental health risks 14 .
Data from the general population across the US have revealed that COVID‐19 infection disproportionately affects African Americans and people with poorer socioeconomic status 15 . Men might have a higher COVID‐related mortality, whereas women might be more vulnerable to the socioeconomic and emotional effects of the infection16, 17, 18.
In this study, we analyzed a nation‐wide database of electronic health records of 61 million adult patients in the US, aiming to assess the impact of a recent (within past year) diagnosis of a mental disorder – including attention‐deficit/hyperactivity disorder (ADHD), bipolar disorder, depression and schizophrenia – on the risk for COVID‐19 infection and related mortality and hospitalization rates. We also evaluated how these risks were affected by ethnicity and gender.
METHODS
Design and study population
We conducted a case‐control study using de‐identified population‐level electronic health records data collected by the IBM Watson Health Explorys from 360 hospitals and 317,000 providers across 50 states in the US, representing 20% of US population 19 .
The electronic health records were de‐identified according to the Health Insurance Portability and Accountability Act, and the Health Information Technology for Economic and Clinical Health Act standards, so that the approval by an institutional review board was not needed. After the de‐identification process, curation process normalized the data through mapping key elements to widely‐accepted biomedical terminologies and standards 20 , including the Systematized Nomenclature of Medicine‐Clinical Terms (SNOMED‐CT) for disease coding21, 22.
More than 160 published studies have used this large‐scale and standardized database and the cloud‐based Explorys Cohort Discovery informatics tools to study a variety of conditions, including cardiovascular diseases, cancers, neurological diseases, infectious diseases, and substance use disorders 23 . Recently, we have used this database for drug discovery24, 25 and for COVID‐19 research in patients with substance use disorders 26 .
In the present study, the status of COVID‐19 was based on the concept “coronavirus infection (disorder)” (SNOMED‐CT code 186747009), while that of mental disorder was based on the diagnosis of “mental disorder (disorder)” (74732009). The status of type of disorder was based for ADHD on the diagnosis of “attention deficit hyperactivity disorder (disorder)” (406506008); for bipolar disorder on the diagnosis of “bipolar disorder (disorder)” (13746004); for depression on the diagnosis of “depressive disorder (disorder)” (35489007); and for schizophrenia on the diagnosis of “schizophrenia (disorder)” (58214004). The SNOMED‐CT concept “hospital admission (procedure)” (32485007) was used to obtain hospitalization status. The status of “death” was based on the Social Security Death index that Explorys regularly imports.
We examined the impact of mental disorders on the risk of COVID‐19 infection, adjusted for age, gender, ethnicity, and common medical comorbidities. The exposure groups were patients diagnosed with a mental disorder; the unexposed groups were patients without the mental disorder; and the outcome measure was the diagnosis of COVID‐19.
We then explored how demographic factors affected COVID‐19 infection risk among patients with mental disorders. The case groups were patients with a mental disorder and one of the following factors: female, senior (i.e., >65 years), African American. The comparison groups were patients with a mental disorder and one of the following corresponding factors: male, adult (i.e., 18 to 65 years), Caucasian. The outcome measure was the diagnosis of COVID‐19.
We finally investigated the rates of death and hospitalization among patients with COVID‐19 infection and a mental disorder, compared to patients with COVID‐19 infection but no mental disorder, and to patients with a mental disorder but no COVID‐19 infection.
Statistical analysis
The adjusted odds ratio (AOR), 95% CI and p values were calculated using the Cochran‐Mantel‐Haenszel method 27 , controlling for age groups (adults, seniors), gender (female, male), ethnicity (Caucasian, African American), and medical comorbidities such as cancers, cardiovascular diseases, type 2 diabetes, obesity, chronic kidney diseases, chronic obstructive pulmonary disease, asthma, and substance use disorders.
Two‐sided, two‐sample tests for equality of proportions with continuity correction were used to compare outcomes. Statistical tests were conducted with significance set at p<0.05 (two‐sided). All analyses were done using R, version 3.6.3.
RESULTS
Patient characteristics
The demographic characteristics of the study population are presented in Table 1. Among 61,783,950 patients (age ≥18), 11,240,580 had a lifetime diagnosis of a mental disorder (within past year or prior) and 1,307,720 had a recent diagnosis (within past year) (lifetime diagnosis: 18.2%, recent diagnosis: 2.1% of study population).
Table 1.
Characteristics of the sample
| Study population | With mental disorder (lifetime) | With mental disorder (recent) | With COVID‐19 | With COVID‐19 + mental disorder (lifetime) | With COVID‐19 + mental disorder (recent) | |
|---|---|---|---|---|---|---|
| Total | 61,783,950 | 11,240,580 | 1,307,720 | 15,110 | 5,450 | 3,430 |
| Gender | ||||||
| Female | 33,654,480 (54%) | 6,899,010 (61%) | 838,380 (64%) | 8,980 (59%) | 3,730 (68%) | 2,380 (70%) |
| Male | 27,758,960 (45%) | 4,301,060 (38%) | 449,290 (34%) | 6,090 (40%) | 1,710 (32%) | 1,040 (30%) |
| Unknown | 371,040 (<1%) | 40,590 (<1%) | 20,060 (2%) | 30 (<1%) | 10 (<1%) | 0 |
| Age | ||||||
| Adult (18‐65 years) | 43,933,300 (71%) | 7,684,520 (68%) | 934,500 (71%) | 11,290 (75%) | 3,680 (68%) | 2,240 (65%) |
| Senior (>65 years) | 17,896,950 (29%) | 3,570,470 (32%) | 374,950 (29%) | 3,820 (25%) | 1,770 (32%) | 1,190 (35%) |
| Ethnicity | ||||||
| Caucasian | 35,096,550 (57%) | 8,506,170 (76%) | 990,000 (76%) | 7,550 (50%) | 3,150 (58%) | 1,980 (58%) |
| African American | 6,389,510 (10%) | 1,238,820 (11%) | 160,480 (12%) | 6,310 (42%) | 2,030 (37%) | 1,280 (37%) |
| Asian | 1,008,180 (2%) | 139,810 (1%) | 14,260 (1%) | 150 (1%) | 40 (1%) | 20 (1%) |
| Hispanic/Latino | 859,970 (1%) | 101,120 (1%) | 7,970 (<1%) | 10 (<1%) | 0 | 0 |
| Unknown | 7,959,570 (12%) | 1,361,290 (12%) | 111,090 (8%) | 790 (5%) | 330 (6%) | 230 (7%) |
The specifics for lifetime and recent diagnosis were as follows: lifetime 1,030,790, recent 99,230 (1.7% and 0.2% of study population, respectively) for ADHD; lifetime 930,280, recent 87,270 (1.5% and 0.1%, respectively) for bipolar disorder; lifetime 6,237,350, recent 610,710 (10.1% and 1.0%, respectively) for depression; lifetime 275,950, recent 26,510 (0.5% and 0.04%, respectively) for schizophrenia.
Among 15,110 COVID‐19 patients in the database, 5,450 had a lifetime diagnosis of a mental disorder (past year or prior, but prior to COVID‐19 diagnosis), and 3,430 had a recent diagnosis of a mental disorder (past year, but prior to COVID‐19) (lifetime: 36.1%, recent: 22.7% of COVID‐19 population). Lifetime and recent diagnosis for specific disorders in the COVID‐19 population were highest for depression (lifetime: 18.0%, N=2,720; recent: 9.7%, N=1,460); followed by ADHD (lifetime: 2.7%, N=400; recent: 1.5%, N=220); bipolar disorder (lifetime: 2.1%, N=310; recent: 1.2%, N=180); and schizophrenia (lifetime: 0.8%, N=120; recent: 0.5%, N=80).
Associations between mental disorders and COVID‐19
Patients with a recent diagnosis of a mental disorder had significantly higher odds of COVID‐19 infection than patients without a mental disorder, after adjusting for age, gender and ethnicity, with the strongest effect for depression (AOR=10.43, 95% CI: 10.10‐10.76, p<0.001) and schizophrenia (AOR=9.89, 95% CI: 8.68‐11.26, p<0.001) (see Figure 1). The trend was similar for patients with a lifetime diagnosis of a mental disorder, but the risk associations were lower (e.g., AOR=2.01, 95% CI: 1.96‐2.06, p<0.001 for depression; AOR=1.48, 95% CI: 1.33‐1.65, p<0.001 for schizophrenia). For the rest of the analyses, we focused on patients with a recent diagnosis.
Figure 1.
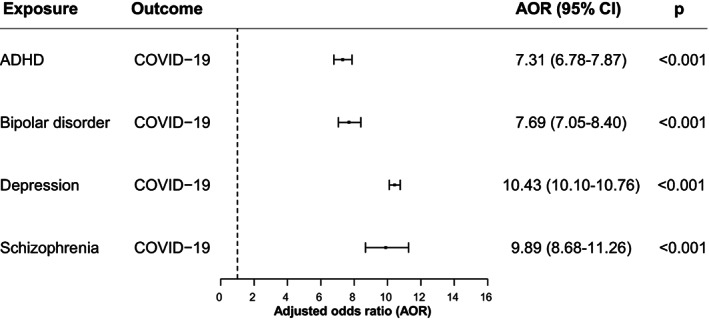
Association of recent (within past year) diagnosis of a mental disorder and COVID‐19 infection after adjusting for age, gender and ethnicity. ADHD – attention‐deficit/hyperactivity disorder
After adjusting for medical comorbidities (cancers, cardiovascular diseases, type 2 diabetes, obesity, chronic kidney diseases, chronic obstructive pulmonary disease, asthma, and substance use disorders), in addition to age, gender and ethnicity, the odds of COVID‐19 infection among patients with a mental disorder decreased, but remained highly significant (see Figure 2). Once again, the strongest effect was for depression (AOR=7.64, 95% CI: 7.45‐7.83, p<0.001), followed by schizophrenia (AOR=7.34, 95% CI: 6.65‐8.10, p<0.001), ADHD (AOR=5.82, 95% CI: 5.46‐6.20, p<0.001), and bipolar disorder (AOR=5.72, 95% CI: 5.35‐6.10, p<0.001).
Figure 2.

Association of recent (within past year) diagnosis of a mental disorder and COVID‐19 infection after adjusting for age, gender, ethnicity, and medical comorbidities (cancers, cardiovascular diseases, type 2 diabetes, obesity, chronic kidney diseases, chronic obstructive pulmonary disease, asthma, and substance use disorders). ADHD – attention‐deficit/hyperactivity disorder
Demographic disparity of risk for COVID‐19 infection among patients with recent diagnosis of a mental disorder
Among patients with a recently diagnosed mental disorder, African Americans had a higher risk for COVID‐19 than Caucasians, after adjusting for age, gender and medical comorbidities, with the strongest ethnic disparity for depression (AOR=3.78, 95% CI: 3.58‐3.98, p<0.001), followed by schizophrenia (AOR=2.33, 95% CI: 1.84‐2.97, p<0.001), bipolar disorder (AOR=2.23, 95% CI: 1.90‐2.61, p<0.001), and ADHD (AOR=2.00, 95% CI: 1.64‐2.43, p<0.001) (see Figure 3).
Figure 3.
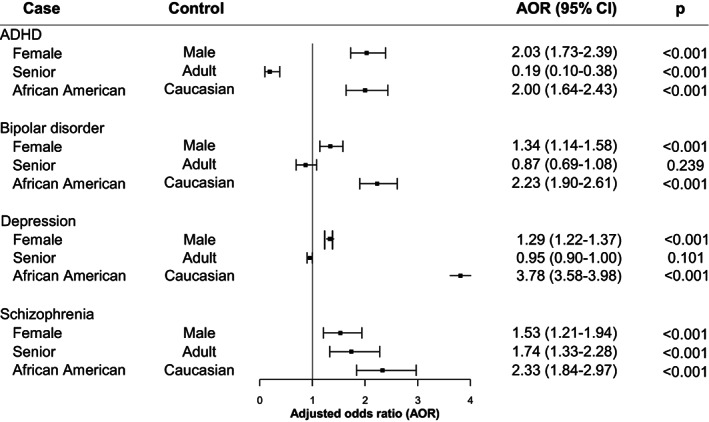
Effects of demographics on odds of COVID‐19 infection among patients with a recently diagnosed mental disorder after adjusting for medical comorbidities (cancers, cardiovascular diseases, type 2 diabetes, obesity, chronic kidney diseases, chronic obstructive pulmonary disease, asthma, and substance use disorders). ADHD – attention‐deficit/hyperactivity disorder
Women with a recent diagnosis of a mental disorder had higher odds of COVID‐19 infection than men after adjusting for age, ethnicity and medical comorbidities, with the strongest gender disparity for ADHD (AOR=2.03, 95% CI: 1.73‐2.39, p<0.001), followed by schizophrenia (AOR=1.53, 95% CI: 1.21‐1.94, p<0.001), bipolar disorder (AOR=1.34, 95% CI: 1.14‐1.58, p<0.001) and depression (AOR=1.29, 95% CI: 1.22‐1.37, p<0.001).
Age had significant effects on COVID‐19 risk, after adjusting for gender, ethnicity and medical comorbidities, among patients with a recent diagnosis of ADHD (patients >65 years had a lower risk than those aged 18‐65 years; AOR=0.19, 95% CI: 0.10‐0.38, p<0.001), and schizophrenia (patients >65 years had a higher risk than those aged 18‐65 years; AOR=1.74, 95% CI: 1.33‐2.28, p<0.001) (see Figure 3).
Rates of death and hospitalization among COVID‐19 patients with a recent diagnosis of a mental disorder
The death rate in the 15,120 COVID‐19 patients was 5.7%, being higher for African Americans (6.2%) than for Caucasians (3.7%) (p<0.001), and higher for men (6.6%) than for women (3.4%) (p<0.001).
Among the 3,430 adults with both COVID‐19 and a recent diagnosis of a mental disorder, 290 died (death rate of 8.5%), with similar rates for African Americans (8.6%) and Caucasians (8.6%), but higher rates for men (12.5%) than for women (6.7%) (p<0.001).
Among the 1,460 patients with both COVID‐19 and a recent diagnosis of depression, 120 died (death rate of 8.2%), with similar rates for African Americans (9.6%) and Caucasians (8.1%), and higher rates for men (13.9%) than women (6.4%) (p<0.001).
The death rate for patients with both a recent diagnosis of a mental disorder and COVID‐19 infection (8.5%) was higher than for patients with COVID‐19 infection but no mental disorder (4.7%) (p<0.001), and for patients with a mental disorder but no COVID‐19 infection (1.4%) (p<0.001).
The overall hospitalization rate in the 15,120 COVID‐19 patients was 20.8%, being higher for African Americans (27.3%) than Caucasians (12.7%) (p<0.001), and higher for men (21.6%) than women (16.5%) (p<0.001).
Among the 3,430 patients with both COVID‐19 and a recent diagnosis of a mental disorder, 940 were hospitalized (27.4%). The rate was higher for African Americans (33.6%) than for Caucasians (24.8%), and for men (36.5%) than for women (23.5%) (p<0.001).
Among the 1,460 patients with both COVID‐19 and a recent diagnosis of depression, 380 were hospitalized (26.0%), and the rate was higher for African Americans (32.7%) than for Caucasians (23.3%) (p<0.001), and for men (33.3%) than for women (23.6%) (p<0.001).
Overall, the hospitalization rate for patients with both a recent diagnosis of a mental disorder and COVID‐19 infection (27.4%) was higher than for patients with COVID‐19 infection but no mental disorder (18.6%) (p<0.001) and for patients with a mental disorder but no COVID‐19 infection (13.8%) (p<0.001).
DISCUSSION
Based on an analysis of a nation‐wide database of electronic health records in the US, we document that patients with a recent (within past year) diagnosis of a mental disorder have a significantly higher risk for COVID‐19 infection as compared to patients without mental disorders, and also present a worse outcome as evidenced by higher rates of hospitalization and death. The risk for COVID‐19 infection among those with a recent diagnosis of a mental disorder is further increased among African Americans and women, though death and hospitalization rates are higher in men. These findings identify individuals with mental disorders as a highly vulnerable population for COVID‐19 infection and its adverse outcomes, and confirm the ethnic and gender disparities already observed in the general population.
A variety of factors are likely to contribute to the higher risk for COVID‐19 infection and worse outcomes of the infection in people with mental disorders. These people may have problems to appraise health information and to comply with preventive behaviors 10 . Their life circumstances place them at higher risk for living in crowded hospitals or residences, or even in prisons, and these are environments where infections can disseminate rapidly 10 . People with serious mental illness are likely to be socioeconomically disadvantaged, which might force them to work and live in unsafe environments. Homelessness and unstable housing may affect their ability to quarantine. Stigma may result in barriers to access health care for patients who are infected with COVID‐19, or make them reluctant to seek medical attention for fear of discrimination 28 .
Specific manifestations of individual mental disorders might influence risk differently. For example, in the case of patients with ADHD, their inattention might place them at higher risk for forgetting to wear face masks or maintaining social distancing, whereas in individuals suffering from depression their amotivation might lead them to neglect protecting themselves or seeking medical attention when indicated, and in a patient with schizophrenia the delusional thinking might lead him/her to reject the use of a face mask. On the other hand, the higher sensitivity to stress, which is common among patients with mental disorders, will make it harder for them to cope with the uncertainties, isolation and economic challenges linked with the COVID‐19 pandemic, increasing their risk for relapse and disease exacerbation7, 10.
Individuals with mental disorders are also at higher risk for taking drugs and for suffering from a substance use disorder than the general population. In particular, tobacco smoking is highly prevalent among those with schizophrenia, bipolar disorder and depression compared to the general population29, 30. Moreover, patients with mental disorders who are smokers smoke more heavily than those who do not have a mental disorder 31 , which accentuates their risk for pulmonary pathology, making them more vulnerable to severe COVID‐19 disease. Indeed, a higher risk for adverse outcomes related to the association of COVID‐19 and smoking has been reported32, 33. In a recent study based on an analysis of electronic health records data, we documented that patients with a recent history of tobacco smoking had increased odds (AOR=8.22) for COVID‐19 infection 26 .
People with severe mental disorders are more likely to suffer from comorbid medical conditions associated with higher risk for severe COVID‐19 illness 10 . Indeed, our analyses showed that medical comorbidities (cancers, cardiovascular diseases, obesity, chronic kidney diseases, asthma, chronic obstructive pulmonary disease, type 2 diabetes, and substance use disorders) contributed to the higher COVID‐19 infection risk in patients with a recent mental disorder, as evidenced by the reduction of risk after adjusting for these comorbidities. However, even after this adjustment, the risk for COVID‐19 infection in patients with recent mental disorders was still increased, indicating that these disorders directly affect COVID‐19 susceptibility.
Overlapping biological factors among mental disorders and COVID‐19 infection could also be implicated. An example of a common biological factor that contributes to various mental disorders and to COVID‐19 pathology is inflammation, which is reported to play a role in the pathogenesis of depression 34 , schizophrenia 35 and bipolar disorder 36 , as well as in the systemic manifestations of COVID‐19 infection 37 .
Our analyses revealed that African Americans with depression, bipolar disorder, schizophrenia and ADHD had higher risk for COVID‐19 infection than Caucasians even after controlling for medical comorbidities, indicating that social, behavioral and lifestyle factors also contribute to this profound ethnic inequality. Women with ADHD, bipolar disorder, depression and schizophrenia had higher risk for COVID‐19 infection, though lower rates of death and hospitalizations than men, which could reflect either a higher risk for infection or a higher likelihood of being tested. However, socioeconomic factors contribute to gender disparities in health and are likely to have also influenced gender disparities in COVID‐19 infection rates. The much higher risk of death for men than women in general, but prominently for patients with depression and COVID‐19 infection, could similarly reflect biological as well socioeconomic factors.
Patients with both COVID‐19 infection and a recent diagnosis of a mental disorder had an increased risk of death (8.5% versus 5.7% for all COVID‐19 patients and 4.7% for COVID‐19 patients without a recent mental disorder), which again may result from delays in getting medical attention, medical comorbidities, and a variety of socioeconomic and disease‐related factors. The difference in death rate of COVID‐19 patients with mental disorders compared to all COVID patients (48% higher) is similar in magnitude to the difference we recently reported for COVID‐19 patients with substance use disorder (45% higher) 26 . However, in that prior study, using electronic health records data up to June 15, 2020, we reported a higher death rate from COVID‐19 infection than in the current study, which used data up to July 29, 2020 (6.6% vs. 5.7%), which is likely to reflect the decline in COVID‐19 mortality attributed in part to better disease management, increased testing and shifts in the patient population 38 .
Patient electronic health records data may have limitations when used for research purposes, including limited information on time‐series, socioeconomic and lifestyle determinants39, 40, 41. Moreover, COVID‐19 is regularly tested at drive‐up and pop‐up sites, so it is likely that many cases, particularly asymptomatic ones, were not captured by electronic health records. Third, findings from this study are correlational, not causal, and need to be validated in other patient databases or populations.
Despite these limitations, our analysis of a large nation‐wide database provided evidence of an increased COVID‐19 infection risk among patients with mental disorders, exacerbated by ethnic and gender disparities, and of higher mortality and hospitalization rates in COVID‐19 patients with a recent diagnosis of a mental disorder. Our results identify mental disorders as a health risk factor for COVID‐19 infection and its adverse outcomes, emphasizing the need to recognize and address modifiable vulnerability factors and to prevent delays in health care provision in this population.
ACKNOWLEDGEMENTS
R. Xu is supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the US National Institutes of Health (NIH), the US NIH National Institute on Aging, the American Cancer Society Research, and the Clinical and Translational Science Collaborative of Cleveland.
REFERENCES
- 1. World Health Organization . WHO coronavirus disease (COVID‐19) dashboard. https://covid19.who.int.
- 2. Centers for Disease Control and Prevention . Groups at higher risk for COVID‐19 severe illness. https://www.cdc.gov/coronavirus. [PubMed]
- 3. Richardson S, Hirsch JS, Narasimhan M et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID‐19 in the New York City area. JAMA 2020;323:2052‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Myers LC, Parodi SM, Escobar GJ et al. Characteristics of hospitalized adults with COVID‐19 in an integrated health care system in California. JAMA 2020;323:2195‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zhou F, Yu T, Du R et al. Clinical course and risk factors for mortality of adult inpatients with COVID‐19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. World Health Organization . Mental disorders. https://www.who.int.
- 7. Adhanom Ghebreyesus T. Addressing mental health needs: an integral part of COVID‐19 response. World Psychiatry 2020;19:129‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Li J, Yang Z, Qiu H et al. Anxiety and depression among general population in China at the peak of the COVID‐19 pandemic. World Psychiatry 2020;19:249‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Yao H, Chen JH, Xu YF. Patients with mental health disorders in the COVID‐19 epidemic. Lancet Psychiatry 2020;7:e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Shinn AK, Viron M. Perspectives on the COVID‐19 pandemic and individuals with serious mental illness. J Clin Psychiatry 2020;81:20com13412. [DOI] [PubMed] [Google Scholar]
- 11. McGuire TG, Miranda J. New evidence regarding racial and ethnic disparities in mental health: policy implications. Health Aff 2008;27:393‐403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Alegría M, Chatterji P, Wells K et al. Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatr Serv 2008;59:1264‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Alegría M, Falgas‐Bague I, Fong H. Engagement of ethnic minorities in mental health care. World Psychiatry 2020;19:35‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. World Health Organization . Gender and women’s mental health. Geneva: World Health Organization, 2020. [Google Scholar]
- 15. Yancy CW. COVID‐19 and African Americans. JAMA 2020;323:1891‐2. [DOI] [PubMed] [Google Scholar]
- 16. Burki T. The indirect impact of COVID‐19 on women. Lancet Infect Dis 2020;20:904‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. The Lancet. The gendered dimensions of COVID‐19. Lancet 2020;395:1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. United Nations . The impact of COVID‐19 on women. https://www.unwomen.org.
- 19. International Business Machines (IBM). Explorys EHR solutions. https://www.ibm.com.
- 20. Bodenreider O. The unified medical language system (UMLS): integrating biomedical terminology. Nucleic Acids Res 2004;32:D267‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. SNOMED International . The systematized nomenclature of medicine – clinical terms (SNOMED CT). http://www.snomed.org.
- 22. Kaelber DC, Foster W, Gilder J et al. Patient characteristics associated with venous thromboembolic events: a cohort study using pooled electronic health record data. J Am Med Inform Assoc 2012;19:965‐72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. International Business Machines (IBM). IBM Explorys EHR database bibliography categorized by therapeutic area. https://www.ibm.com.
- 24. Zhou M, Xu R, Kaelber DC et al. Tumor necrosis factor (TNF) blocking agents are associated with lower risk for Alzheimer’s disease in patients with rheumatoid arthritis and psoriasis. PLoS One 2020;15:e0229819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Zhou M, Zheng CL, Xu R. Combining phenome‐driven drug target prediction with patients? Electronic health records‐based clinical corroboration towards drug discovery. Bioinformatics 2020;36(Suppl. 1):i436‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Wang Q, Kaelber D, Xu R et al. COVID‐19 risk and outcomes in patients with substance use disorders: analyses from electronic health records in the United States. Mol Psychiatry (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kuritz SJ, Landis JR, Koch GG. A general overview of Mantel‐Haenszel methods: applications and recent developments. Annu Rev Public Health 1988;9:123‐60. [DOI] [PubMed] [Google Scholar]
- 28. Wasserman D, Iouse M, Wuestefeld A et al. Adaptation of evidence‐based suicide prevention strategies during and after the COVID‐19 pandemic. World Psychiatry 2020;19:294‐306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Dickerson F, Schroeder J, Katsafanas E et al. Cigarette smoking by patients with serious mental illness, 1999‐2016: an increasing disparity. Psychiatr Serv 2018;69:147‐53. [DOI] [PubMed] [Google Scholar]
- 30. Weinberger AH, Kashan RS, Shpigel DM et al. Depression and cigarette smoking behavior: a critical review of population‐based studies. Am J Drug Alcohol Abuse 2017;43:416‐31. [DOI] [PubMed] [Google Scholar]
- 31. Prochaska JJ, Das S, Young‐Wolff KC. Smoking, mental illness, and public health. Annu Rev Public Health 2017;38:165‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Vardavas CI, Nikitara K. COVID‐19 and smoking: a systematic review of the evidence. Tob Induc Dis 2020;18:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Patanavanich R, Glantz SA. Smoking is associated with COVID‐19 progression: a meta‐analysis. Nicotine Tob Res 2020;22:1653‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Beurel E, Toups M, Nemeroff CB. The bidirectional relationship of depression and inflammation: double trouble. Neuron 2020;107:234‐56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Müller N. Inflammation in schizophrenia: pathogenetic aspects and therapeutic considerations. Schizophr Bull 2018;44:973‐82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Benedetti F, Aggio V, Pratesi ML et al. Neuroinflammation in bipolar depression. Front Psychiatry 2020;11:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Steardo L Jr, Steardo L, Verkhratsky A. Psychiatric face of COVID‐19. Transl Psychiatry 2020;10:261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Centers for Disease Control and Prevention . COVIDView. A weekly surveillance summary of U.S. COVID‐19 activity. https://www.cdc.gov.
- 39. Cowie MR, Blomster JI, Curtis LH et al. Electronic health records to facilitate clinical research. Clin Res Cardiol 2017;106:1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Coorevits P, Sundgren M, Klein GO et al. Electronic health records: new opportunities for clinical research. J Intern Med 2013;274:547‐60. [DOI] [PubMed] [Google Scholar]
- 41. Ahmad FS, Chan C, Rosenman MB et al. Validity of cardiovascular data from electronic sources: the Multi‐Ethnic Study of Atherosclerosis and HealthLNK. Circulation 2017;136:1207‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]


