Abstract
Aim
Proctology is one of the surgical specialties that has suffered the most during COVID‐19 pandemic. Using a cross‐sectional non‐incentivised World Wide Web survey, we aimed to snapshot the current status of proctological practice in six world regions.
Method
Surgeons affiliated to renowned scientific societies with an interest in coloproctology were invited to join the survey. Members of the ProctoLock Working Group enhanced recruitment by direct invitation. The predictive power of respondents’ and hospitals’ demographics on the change of status of surgical and outpatient activities was calculated.
Results
Respondents (n = 1050) were mostly men (79%), with a mean age of 46.9 years, at consultant level (79%), practising in academic hospitals (53%) offering a dedicated proctology service (68%). A total of 119 (11%) tested positive for SARS‐CoV‐2. The majority (54%) came from Europe. Participants from Asia reported a higher proportion of unaltered practice (17%), while those from Europe had the highest proportion of fully stopped practice (20%). The likelihood of ongoing surgical practice was higher in men (OR 1.54, 95% CI 1.13–2.09; P = 0.006), in those reporting readily availability of personal protective equipment (PPE) (OR 1.40, 1.08–1.42; P = 0.012) and in centres that were partially or not at all involved in COVID‐19 care (OR 2.95, 2.14–4.09; P < 0.001). This chance decreased by 2% per year of respondent’s age (P = 0.001).
Conclusion
Several factors including different screening policies and resource capacity affected the current status of proctological practice. This information may help health authorities to formulate effective preventive strategies to limit curtailment of care of these patients during the pandemic.
Keywords: COVID‐19, Europe, Italy, Lockdown, ProctoLock2020, Proctology, SARS‐COV‐2, Worldwide
What does this paper add to the literature?
A worldwide survey of 1050 respondents showed that proctological practice has been seriously affected by the COVID‐19 pandemic. Age, gender and level of hospital preparedness were associated with the change of status of surgical and outpatient activities (i.e. from fully stopped to ongoing).
1. INTRODUCTION
Since the first human cases of severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2)[1, 2] were reported in Wuhan in December 2019, the attention of the scientific community has risen hand in hand with the diffusion of the novel coronavirus. The rapid worldwide spread of the disease, later named as COronaVIrus Disease 2019 (COVID‐19), led the World Health Organization to reconsider the initial status of the outbreak by declaring a pandemic on 11 March 2020.
The potential life‐threatening consequences of COVID‐19 in symptomatic patients have put a strain on healthcare systems worldwide [3]. In Italy, with the exception of oncological and urgent cases, all elective procedures and outpatient clinics have been suspended [4, 5, 6].
In this unprecedented healthcare crisis, scientific societies and experts in the field are committing to develop recommendations with the aim of steering clinical practice [7, 8, 9].
Proctology is one of the subspecialties that has suffered the most during the COVID‐19 pandemic [6, 10, 11, 12]. The social, psychological and economic consequences of curbing proctological practice should be carefully considered [6, 10, 11, 12]. In fact, serious diagnostic delays may arise from deferring a comprehensive first visit (anamnesis, physical examination and anoscopy) – an alarming concern, particularly for patients with neoplastic diseases. Although oro‐faecal spread does not seem to be a principal route of COVID‐19 infection, proctologists are also warned about stool isolation of SARS‐CoV‐2 viral RNA [13, 14]. In this context, personal protective equipment (PPE) plays a major role in curbing viral spread, despite resource constraints [15, 16].
The current impact of COVID‐19 on global health systems is difficult to assess, but concerted efforts are being made to avoid detrimental effects on oncological outcomes and limit surgical morbidity. Indeed, a rearrangement of clinical and surgical activities is compulsory to achieve full and adequate patient care [17].
The ProctoLock 2020 survey sought to obtain a snapshot of the impact of COVID‐19 on proctological practice worldwide to inform the development of strategies that best guarantee access to treatment.
2. METHOD
Experts in the field who joined a previous qualitative study [18] (n = 492) were invited to complete a web survey (participants could be identified only via their valid email address; no other identifying information was collected). The survey link was sent to scientific societies of interest to coloproctologists (i.e. Italian Society of Colorectal Surgery, Russian Association of Coloproctologists, Mediterranean Society of Coloproctology) and disseminated to their members. All collaborators (the ProctoLock 2020 Working Group) committed to further recruitment of participants by direct invitation. Participation was entirely voluntary with no compensation offered. Informed consent was obtained from all those agreeing to complete a survey.
2.1. Survey
A 27‐item survey (namely, ‘ProctoLock 2020’; Appendix 1) was designed and developed by the authors using an online platform [‘Online surveys’, formerly BOS (Bristol Online Survey) developed by the University of Bristol] in accordance with the Consolidated Criteria for Reporting Qualitative Research (COREQ) and the Checklist for Reporting Results of Internet E‐Surveys (the CHERRIES statement; Appendix 2) [19]. Proprietary survey software and local servers were used to ensure data protection. The fully de‐identified dataset was kept on password‐protected computers. The authors piloted the survey, assessed the design and checked the feasibility and validity of the questions. The estimated mean time needed to complete the survey was 8 min. The finalised online survey was made available from 15 to 26 April 2020.
The survey aimed to capture the current status of proctological practice worldwide, first exploring the overall changes in terms of resource allocation and secondly assessing in more detail the various fields of application for both proctological surgery [i.e. elective (oncological and nononcological) and urgent] and outpatient practice, with a focus on sexually transmitted disease (STD) and pelvic floor clinics. The availability of anorectal physiology testing was also assessed.
All questions were set as mandatory fields with real‐time validation and automated skip logic to prevent missing data and avoid illogical or incompatible responses. No randomisation of items was used. Quantitative data were automatically collected by the software and exported to a tabulated format.
The study was registered at ClinicalTrials.gov (NCT 04392245).
2.2. Statistical analysis
Continuous variables were summarised by means and standard deviations (SDs), whilst categorical variables were assessed by proportions. Comparisons of categorical variables across groups were made by Pearson's chi‐square tests. A series of hierarchical binary and ordinal logistic models for binary or ordinal variables were performed to assess the association between respondents' preferences and their characteristics, with geographical area as a random effect [adjusted odds ratio (OR)]. The Brant test was performed to assess the proportional odds assumption in the ordinal logistic model. Uni‐ and multivariable models were fitted using a predefined set of covariates which included respondents' and hospitals' demographics (i.e. age, gender, type of hospital, hospital rearrangement, external facilities for proctological surgery, use of PPE, preoperative testing policies for SAR‐CoV‐2).
The denominator of the percentages of respondents was the total number of respondents who eventually completed the survey. Adjustment to the P‐values was not performed. However, considering the number of tests performed, P‐values <0.05 were critically appraised in order to take into account the risk of false positives. All analyses were performed using STATA 16 (StataCorp LLC).
3. RESULTS
3.1. Demographics
A total of 1079 subjects completed the survey, taking a mean time of 8.6 min (SD 3.8 min) each. Of these, 1050 (97%) were unique respondents and contributed to the final analysis.
Among the invited experts who joined a previous qualitative study [18], 420/492 (85.4%) responded to the survey, accounting for 40% of participants. The remaining 630 (60%) were recruited through advertising to other scientific societies and direct invitation by members of the ProctoLock 2020 Working Group. A total of 570 (54%) came from Europe, 200 (19%) and 68 (6%) from North and South America, respectively, 186 (18%) from Asia, 16 (2%) from Africa and only 10 (1%) from Australia and New Zealand, with a total of 69 countries being involved (Appendix 3).
At the time of survey completion, Europe was the most affected region, with more than 1 million confirmed cases and 100 000 deaths [20].
Respondents were mostly men (79%), with a mean age of 46.9 years (12.1), at consultant level (79%), practising in academic hospitals (53%) with a dedicated proctologist performing surgery (68%). A total of 119 (11%) tested positive for SARS‐CoV‐2 (Table 1). A logistic regression model showed that the chance of SARS‐CoV‐2 positivity was 74% higher in men (P = 0.044), 91% higher in those from centres with external COVID‐19‐free facilities (P = 0.003) and 73% higher in those reporting preoperative SARS‐CoV‐2 screening for all patients (P = 0.015) (Appendix 4). A total of 310 (30%) and 497 (47%) participants came from centres providing dedicated pathways for STD and pelvic floor disorders (PFD), respectively.
TABLE 1.
Demographics and geographical distribution of survey respondents
| Total responses (n = 1050) | Asia (n = 186) | Europe (n = 570) | North America (n = 200) | South America (n = 68) | Africa (n = 16) | Oceania (n = 10) | |
|---|---|---|---|---|---|---|---|
| Gender | |||||||
| Male | 824 (78.5) | 144 (77.4) | 434 (76.1) | 161 (80.5) | 61 (89.7) | 16 (100) | 8 (80.0) |
| Female | 226 (21.5) | 42 (22.6) | 136 (23.9) | 39 (19.5) | 7 (10.3) | 0 (0) | 2 (20.0) |
| Age (years), mean (SD) | 46.9 (12.1) | 43.2 (11.7) | 46.5 (12.0) | 52.9 (11.4) | 46.2 (10.2) | 38.9 (8.8) | 53.5 (13.0) |
| Training level | |||||||
| Consultant | 829 (79.0) | 129 (69.4) | 429 (75.3) | 193 (96.5) | 55 (80.9) | 13 (81.3) | 10 (100) |
| Resident | 168 (16.0) | 33 (17.7) | 126 (22.1) | 6 (3.0) | 2 (2.9) | 1 (6.3) | 0 (0) |
| Fellow | 53 (5.0) | 24 (12.9) | 15 (2.6) | 1 (0.5) | 11 (16.2) | 2 (12.5) | 0 (0) |
| Type of hospital | |||||||
| Academic | 560 (53.3) | 132 (71.0) | 273 (47.9) | 87 (43.5) | 48 (70.6) | 13 (81.3) | 7 (70.0) |
| Nonacademic teaching | 307 (29.2) | 29 (15.6) | 183 (32.1) | 72 (36.0) | 17 (25.0) | 3 (18.8) | 3 (30.0) |
| Nonteaching | 183 (17.4) | 25 (13.4) | 114 (20.0) | 41 (20.5) | 3 (4.4) | 0 (0) | 0 (0) |
| Dedicated clinical pathways | |||||||
| Sexually transmitted diseases | 310 (29.5) | 72 (38.7) | 184 (32.3) | 23 (11.5) | 24 (35.3) | 3 (18.8) | 4 (40) |
| Pelvic floor disorders | 497 (47.3) | 99 (53.2) | 299 (28.5) | 58 (29.0) | 29 (42.6) | 6 (37.5) | 6 (60) |
| Anorectal physiology testing | 669 (63.7) | 112 (60.2) | 381 (66.8) | 125 (62.5) | 36 (52.9) | 7 (43.8) | 8 (80) |
| Type of surgeon performing urgent cases | |||||||
| Dedicated proctologist | 710 (67.6) | 137 (73.7) | 336 (58.9) | 172 (86.0) | 47 (69.1) | 10 (62.5) | 8 (80) |
| General surgeon | 340 (32.4) | 49 (26.3) | 234 (41.1) | 28 (14.0) | 21 (30.9) | 6 (37.5) | 2 (20) |
| Tested SARS‐CoV‐2‐positive | 119 (11.3) | 22 (11.8) | 90 (15.8) | 6 (3) | 1 (1.5) | 0 (0) | 0 (0) |
Figures in brackets are percentages or SD where stated.
3.2. Hospital preparedness for the COVID‐19 pandemic
Most respondents came from centres that were rearranged to fully (n = 161, 15%) or partially (n = 746, 71%) assist COVID‐19 patients, with only a minority (n = 143, 14%) not being involved in COVID‐19 care (Table 2). Surgical patients were referred to external COVID‐19‐free facilities according to nearly a quarter (n = 251, 24%) of respondents.
TABLE 2.
Hospital preparedness for COVID‐19 pandemic
| Total responses (n = 1050) | Asia (n = 186) | Europe (n = 570) | North America (n = 200) | South America (n = 68) | Africa (n = 16) | Oceania (n = 10) | |
|---|---|---|---|---|---|---|---|
| Hospital rearrangement | |||||||
| Fully dedicated to COVID‐19 | 161 (15.3) | 40 (21.5) | 70 (12.3) | 38 (19.0) | 12 (17.6) | 1 (6.3) | 0 (0) |
| Partially dedicated to COVID‐19 | 746 (71.0) | 106 (57.0) | 417 (73.2) | 153 (76.5) | 51 (75.0) | 10 (62.5) | 9 (90.0) |
| Not involved in COVID‐19 care | 143 (13.6) | 40 (21.5) | 83 (14.6) | 9 (4.5) | 5 (7.4) | 5 (31.3) | 1 (10.0) |
| External facilities for proctological surgery | |||||||
| Available for benign and oncological cases | 69 (6.6) | 32 (17.2) | 18 (3.2) | 9 (4.5) | 7 (10.3) | 2 (12.5) | 1 (10.0) |
| Available for oncological cases only | 182 (17.3) | 39 (21.0) | 105 (18.4) | 20 (10.0) | 12 (17.6) | 3 (18.8) | 3 (30.0) |
| Unavailable | 799 (76.1) | 115 (61.8) | 447 (78.4) | 171 (85.5) | 49 (72.1) | 11 (68.8) | 6 (60.0) |
| Surgical consent form redesigned for | |||||||
| SARS‐CoV‐2+ patients | 598 (57.0) | 122 (65.6) | 327 (57.4) | 93 (46.5) | 42 (61.8) | 9 (56.3) | 5 (50.0) |
| SARS‐CoV‐2– patients | 623 (59.3) | 132 (71.0) | 334 (58.6) | 102 (51.0) | 41 (60.3) | 9 (56.3) | 5 (50.0) |
| Use of personal protective equipment in theatre with | |||||||
| SARS‐CoV‐2+ patients | |||||||
| Always | 921 (87.7) | 142 (76.3) | 508 (89.1) | 191 (95.5) | 59 (86.8) | 11 (68.8) | 10 (100) |
| Case‐by‐case | 107 (10.2) | 34 (18.3) | 55 (9.6) | 7 (3.5) | 8 (11.8) | 3 (18.8) | 0 (0) |
| Never | 22 (2.1) | 10 (5.4) | 7 (1.2) | 2 (1.0) | 1 (1.5) | 2 (12.5) | 0 (0) |
| SARS‐CoV‐2– or untested patients | |||||||
| Always | 556 (53.0) | 95 (51.1) | 276 (48.4) | 139 (69.5) | 36 (52.9) | 4 (25.0) | 6 (60.0) |
| Case‐by‐case | 399 (38.0) | 71 (38.2) | 234 (41.1) | 52 (26.0) | 30 (44.1) | 8 (50.0) | 4 (40.0) |
| Never | 95 (9.0) | 20 (10.8) | 60 (10.5) | 9 (4.5) | 2 (2.9) | 4 (25.0) | 0 (0) |
| Personal protective equipment readily available | 745 (71.0) | 131 (70.8) | 388 (68.1) | 162 (81.0) | 45 (66.2) | 10 (62.5) | 9 (90.0) |
| All patients are tested for SARS‐CoV‐2 prior to surgery | 541 (51.5) | 87 (46.8) | 369 (64.7) | 71 (35.5) | 10 (14.7) | 1 (6.3) | 3 (30.0) |
| Experience with patients refusing surgery | 381 (36.3) | 78 (41.9) | 186 (32.6) | 84 (42.0) | 29 (42.6) | 2 (12.5) | 2 (20.0) |
| 1–5 patients | 176 (16.8) | 38 (20.4) | 85 (14.9) | 39 (19.5) | 14 (20.6) | 0 (0) | 0 (0) |
| 6–10 patients | 90 (8.6) | 13 (7.0) | 44 (7.7) | 20 (10.0) | 10 (14.7) | 2 (12.5) | 1 (10.0) |
| 11–20 patients | 45 (4.3) | 10 (5.4) | 23 (4.0) | 9 (4.5) | 3 (4.4) | 0 (0) | 0 (0) |
| >20 patients | 70 (6.7) | 17 (9.1) | 34 (6.0) | 16 (8.0) | 2 (2.9) | 0 (0) | 1 (10.0) |
| Current outcome of patients waiting for surgery or visits | |||||||
| Rescheduled until the end of pandemic | 223 (21.2) | 47 (25.3) | 122 (21.4) | 37 (18.5) | 12 (17.6) | 4 (25.0) | 1 (10) |
| Rescheduled upon balance of risks and benefits | 319 (30.4) | 56 (30.1) | 180 (31.6) | 54 (27.0) | 22 (32.4) | 3 (18.8) | 4 (40.0) |
| Rescheduled in 1–3 months according to the waiting list | 252 (24.0) | 44 (23.7) | 116 (20.4) | 64 (32.0) | 21 (30.9) | 4 (25.0) | 3 (30.0) |
| Yet to be established | 256 (24.4) | 39 (21.0) | 152 (26.7) | 45 (22.5) | 13 (19.1) | 5 (31.3) | 2 (20.0) |
Figures in brackets are percentages or SD where stated.
More than a half of interviewees had redesigned the surgical informed consent for both SARS‐CoV‐2‐positive (n = 598, 57%) and ‐negative patients (n = 623, 59%), by mentioning a higher risk of postoperative morbidity.
Only 541 (52%) respondents reported that patients were routinely tested for SARS‐CoV‐2 preoperatively. More than a third (n = 381, 36%) had had experience of patients refusing surgery, with the fear of being infected as the most commonly reported reason (>99%).
A quarter (n = 256) of respondents had yet to reschedule patients waiting for surgery or outpatient visits. Among the possible factors associated with the chance of rescheduling, only a respondent’s age (chance decreased by 1% per year of respondent's age; P = 0.045) and current status of proctological practice [58% higher from ‘fully stopped’ to ‘emergency only’ (P =0.035), and from ‘emergency only’ to ‘ongoing elective’ (P =0.005)] were statistically significant (Appendix 5).
3.3. Current status of proctological practice
Figure 1 shows the status of proctological practice across the world at the time of survey completion. This was more likely to be unaltered in Asia (n = 32, 17%) and fully stopped in Europe (n = 114, 20%).
FIGURE 1.

Current status of proctological surgical practice across the six world regions. (A) Light to dark colour scale represents a low to high prevalence of respondents across countries. (B) Number of COVID‐19 cases per million people on 26 April 2020
Logistic regression models were fitted to explore the association between the status of proctological practice and a number of respondent and hospital characteristics, taking into account the variability across geographical provenance (Table 3). The likelihood of ongoing surgical practice was higher in men (OR 1.54, 95% CI 1.13–2.09; P = 0.006), in those reporting ready availability of PPE (OR 1.40, 1.08–1.42; P = 0.012) and in centres that were partially or not at all involved in COVID‐19 care (OR 2.95, 2.14–4.09; P < 0.001). The chance decreased by 2% per year of respondent's age (P = 0.001).
TABLE 3.
Mixed‐effects logistic regression models exploring the current status of proctological surgery (ordinal) and outpatient practice (binary) with geographical distribution as a random effect
| Odds ratio | 95%CI | P | ||
|---|---|---|---|---|
| Lower | Upper | |||
| Fully stopped vs. Emergency vs. Elective | ||||
| Surgery | ||||
| Age | 0.981 | 0.970 | 0.992 | 0.001 |
| Gender | ||||
| Female (reference) | ||||
| Male | 1.540 | 1.134 | 2.090 | 0.006 |
| Type of hospital | ||||
| Nonteaching (reference) | ||||
| Academic or teaching | 1.304 | 0.951 | 1.787 | 0.100 |
| Hospital rearrangement | ||||
| Fully dedicated to COVID‐19 (reference) | ||||
| Partially dedicated or not involved | 2.954 | 2.136 | 4.086 | <0.001 |
| External facilities for proctological surgery | ||||
| Unavailable (reference) | ||||
| Available | 1.215 | 0.907 | 1.628 | 0.192 |
| Personal protective equipment | ||||
| Unavailable (reference) | ||||
| Readily available | 1.400 | 1.076 | 1.822 | 0.012 |
| Fully stopped vs. Ongoing | ||||
| Outpatients | ||||
| Age | 1.005 | 0.994 | 1.017 | 0.376 |
| Gender | ||||
| Female (reference) | ||||
| Male | 0.625 | 0.452 | 0.866 | 0.005 |
| Type of hospital | ||||
| Nonteaching (reference) | ||||
| Academic or teaching | 0.954 | 0.680 | 1.338 | 0.785 |
| Hospital rearrangement | ||||
| Fully dedicated to COVID‐19 (reference) | ||||
| Partially dedicated or not involved | 0.467 | 0.327 | 0.668 | <0.001 |
| External facilities for proctological surgery | ||||
| Unavailable (reference) | ||||
| Available | 0.752 | 0.554 | 1.020 | 0.068 |
| Personal protective equipment | ||||
| Unavailable (reference) | ||||
| Readily available | 0.908 | 0.687 | 0.1.202 | 0.501 |
3.4. Surgical practice
3.4.1. Elective oncological surgery
A total of 550 (52%) respondents stated elective oncological surgery to be reduced and 286 (27%) fully stopped, with the two main reasons being diminished referrals and/or hospital directions. Figure 2A shows the status of oncological surgery across world regions.
FIGURE 2.
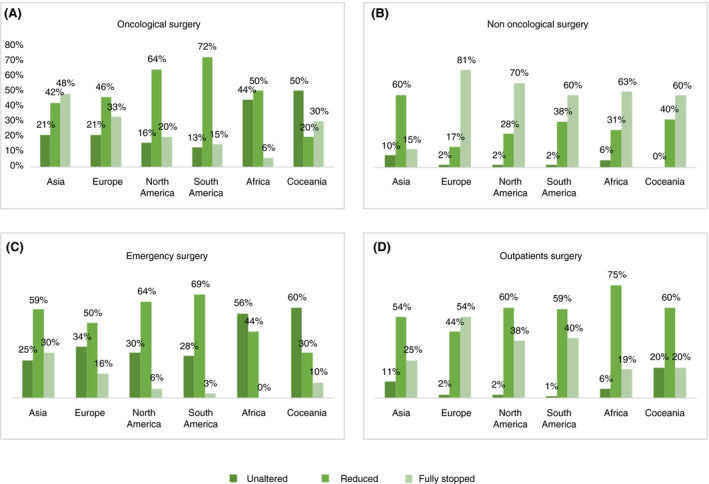
Current status of the single fields of application of proctology across the six world regions
In case of SARS‐CoV‐2 positivity, an equal proportion of participants (32%) either rescheduled operations or performed surgery in accordance with local protocols and then transferred the patient to a dedicated SARS‐CoV‐2+ (84%) or mixed SARS‐CoV‐2+/− (16%) ward. Among respondents who had tested positive for SARS‐CoV‐2, a higher proportion was practising in mixed (20%) rather than dedicated wards (12%) (P < 0.001).
A total of 472 (62%) participants felt that there were flaws or delay in the management of oncological patients, with the main reasons being the temporary suspension of multidisciplinary team meetings and/or reduction of theatre sessions, followed by a delay in performing endoscopic/radiological investigations.
Only 136 (18%) had recently treated a high‐grade squamous intra‐epithelial lesion, with the majority (58%) only in selected high‐risk patients.
3.4.2. Elective nononcological surgery
Up to 71% (n = 750) of respondents reported that elective nononcological surgery fully stopped at their centres, with the main reasons being hospital directions and/or reduced referrals. Figure 2B shows the status of nononcological surgery across world regions.
Among those still performing these operations (n = 303, 29%), the most used setting was theatre (57%), followed by outpatient clinic (13%), with 30% of participants using both.
3.4.3. Emergency surgery
Overall, 587 (56%) participants stated that emergency surgery was reduced and only 131 (13%) reported a fully stopped practice. Figure 2C shows the status of emergency surgery across world regions.
Among respondents reporting an ongoing activity (n = 919, 88%), 548 (60%) stated that patients were routinely tested for SARS‐CoV‐2 preoperatively, with only a minority reporting postoperative (4%) or pre‐ and postoperative (5%) testing. Two thirds (n = 710, 68%) of participants stated that emergency surgery at their centre was performed by a dedicated proctologist.
3.5. Outpatient practice
Outpatient practice was reduced or fully stopped according to 51% (n = 537) or 45% (n = 476) of respondents, respectively, typically as a result of national or local hospital directions. Figure 2D shows the status of outpatient practice across world regions.
A lower chance of ongoing activity was observed in men (OR 0.63, 0.45–0.87; P = 0.005) and in centres that were partially or not at all involved in COVID‐19 care (OR 0.47, 0.33–0.67; P < 0.001) (Table 3).
In centres where this had not fully stopped (n = 574, 55%), an increased time interval between visits was set in two thirds of cases to allow for social distancing. Furthermore, 371 (65%) participants reported that patient history was taken over the phone prior to the visit. Alternatively, a specific anamnestic evaluation for COVID‐19 was performed prior to consultation according to only 113 (56%) participants. Slightly more than a third (35%) declared that all patients were routinely screened for COVID‐19 prior to the visit. However, only 409 (71%) reported regular use of PPE during the consultation.
The likelihood of delayed diagnosis of anorectal cancer resulting from a decreased outpatient practice or specific diagnostic procedures (e.g. high‐resolution anoscopy) concerned up to 86% of respondents.
Among participants from centres where anorectal physiology testing was available before the outbreak (669, 64%), only 10% were still performing investigations at the time of survey completion.
Overall, 78% and 86% of respondents from centres with dedicated pathways for STD and PFD, respectively, reported a postoutbreak curb on referrals. These pathways were statistically significantly more prevalent in centres where a dedicated proctologist was available (STD, 33% vs. 23%, P = 0.001; PFD, 53% vs. 36%, P < 0.001).
4. DISCUSSION AND CONCLUSION
The ProctoLock 2020 survey unexpectedly exceeded 1000 participants. Such massive participation within a relatively short time period reflects the high attention given to a subspecialty that has always been considered the ‘Cinderella’ of general surgery [21].
Of note, the geographical distribution of participants by and large mirrored the areas of highest prevalence of COVID‐19 [20].
Male gender was predominant and in line with previous reports within general surgery [22, 23], suggesting that coloproctology has not largely met women's ambitions over the last two decades. Four out of five participants were consultants, underlining an average high level of professional experience among interviewees. Two thirds of respondents confirmed the presence of a dedicated proctologist performing surgery at their centre, with a peak of 86% in North America, where general and colorectal surgery are two known distinct specialties [24]. Moreover, the presence of a proctologist correlated with the coexistence of third‐level care pathways (e.g. STD, PFD, anorectal physiology testing) in the centre.
The substantial prevalence of SARS‐CoV‐2‐positive subjects among participants (11%) was an alarming figure, highlighting that healthcare workers are at great risk of contagion [25]. Two main factors may explain this observation: first that, as surgeons, proctologists have proved their resilience in continuing their practice while facing the emergency. In some instances, this has translated into alternating shifts in surgical wards and intensive care units [26, 27]. Secondly, proctologists may have been exposed to further potential drivers of transmission (i.e. direct/indirect contact and the oro‐faecal route) [28, 29], thus stressing the need to ensure an adequate reserve of PPE for effective reprocessing and distribution. Furthermore, the observation that participants from centres rearranged so as to keep performing surgery were more at risk may even suggest the limited accuracy of screening instruments [3].
Despite the curb on surgical practice, almost 60% of participants used a redesigned consent form to meet current needs, especially for COVID‐19 patients, reaching its upper peak in Asia and lower peak in Oceania.
Surprisingly, PPE were deemed readily available by only 71% of respondents worldwide, ranging from <33% in Africa and South America to >80% in North America. Whilst 88% of interviewees confirmed the regular use of PPE during surgery on SARS‐CoV‐2‐positive patients, the percentage dropped to 53% for SARS‐CoV‐2‐negative or untested patients. Such a finding may reflect resource management policies that do not always meet risk prevention and up to date scientific evidence on the spread of SARS‐CoV‐2.
The evidence that 36% of participants had had experience with patients who refused surgery underlines a high sense of fear in the population concerning health systems [30].
The three times greater chance of rescheduling patients' procedures among respondents confirming the readily availability of PPE highlights different levels of preparedness for the emergency between centres.
Oncological surgery has greatly been challenged by the pandemic as it was suspended in a third of European and almost half of Asian centres. A reduction in the number of new diagnoses is likely to have resulted from the shutdown and adherence to national directives in many countries. Despite efforts to reallocate resources, only a quarter of respondents confirmed the presence of external facilities for cancer referrals.
Predictably, nononcological surgery has suffered the most among proctological practices as a result of shortage of personnel and operative spaces. Apart from the Asian continent, a reduction of more than 90% in this practice was observed in the other world regions. Among those still practising nononcological surgery, the outpatient/office setting was chosen by 42% of respondents. Although claimed by other authors [6, 9], this option was likely to be influenced by the need to preserve health resources while facing the outbreak. It might be a fertile ground for future development.
With regard to emergency surgery, our results showed that a complete suspension of all activities runs in tandem with the epidemiological evolution of the pandemic. Indeed, the subequatorial countries have shown a smaller chance of stopping in line with the slower spread of SARS‐CoV‐2.
The curb on outpatient practice ranged from 19% in Africa to 54% in Europe. As recently argued, the next decade will prove whether this has had an impact on patients' oncological outcomes [31].
The study has some limitations that are common to all survey‐based studies (e.g. recall and selection bias) [32, 33, 34]. Although we attempted to control for the potential confounding effects of respondents’ characteristics and take into account geographical variations by fitting hierarchical multivariable models, some unobserved and latent factors (e.g. the different timing and magnitude of spread of the virus across the globe) might have played a role and potentially biased some of our exploratory conclusions.
In conclusion, the results of this survey highlight that several factors have affected the global status of proctological practice. This information may help health authorities and decision makers formulate effective preventive strategies to limit curtailment of care of patients during the pandemic.
CONFLICT OF INTEREST
None.
5. Ethical approval
This article does not contain any studies with animals performed by any of the authors.
Appendix 1.
PROCTOLOCK 2020 SURVEY
| Q1 | The information provided in this questionnaire will be exclusively used for research purposes. It will not be used in a manner which would allow identification of your individual responses |
| 1 | Accept |
| Q2 | |
| Q3 | Gender |
| Q4 | Year of birth |
| Q5 | Country |
| Q5_a | Italian region |
| Q6 | Training level |
| 1 | Consultant |
| 2 | Resident |
| 3 | Research Fellow or PhD student |
| Q7 | Type of hospital |
| 1 | Academic |
| 2 | Non academic teaching |
| 3 | Non teaching |
| Q8 | How has your hospital been preparing for the COVID‐19 emergency? |
| 1 | Fully dedicated to COVID‐19 patients |
| 2 | By creating dedicated pathways and wards to COVID‐19 patients |
| 3 | Not involved at all in COVID‐19 patients’ care |
| Q9 | Do you still perform proctologic surgery at your unit? |
| 1 | Not at all |
| 2 | Yes, but only urgent cases |
| 3 | Yes, but only urgent and oncologic cases |
| 4 | Yes, in any case including elective surgery for benign disease |
| Q10 | Did your hospital create external connections to keep performing proctologic surgery in COVID‐free centres? |
| 1 | No |
| 2 | Yes, but only for elective oncologic disease |
| 3 | Yes, for both oncologic and benign disease |
| Q11 | Did you amend your informed consent for COVID‐19 positive patients undergoing surgery by mentioning the augmented risk of complications and mortality? |
| 1 | Yes |
| 2 | No |
| Q12 | Did you amend your informed consent for COVID‐19 negative patients undergoing surgery by mentioning the augmented risk of contagion? |
| 1 | Yes |
| 2 | No |
| Q13 | In case of surgery for COVID‐19 positive patients (either performed in the operating room or outpatient clinic), do you use PPE (Personal Protective Equipment)? |
| 1 | Always |
| 2 | On a case‐by‐case basis |
| 3 | Never |
| Q14 | In case of surgery for COVID‐19 negative or untested patients (either performed in the operating room or outpatient clinic), do you use PPE? |
| 1 | Always |
| 2 | On a case‐by‐case basis |
| 3 | Never |
| Q14_a | Are these patients always tested for COVID‐19 before surgery? |
| 1 | Yes |
| 2 | No |
| Q14_a_i | How? |
| 1 | Chest‐CT |
| 2 | Nasopharyngeal swab |
| 3 | Serology |
| Q15 | Is PPE readily available (adequate for quantity and quality) at your workplace? |
| 1 | Yes |
| 2 | No |
| Q16 | Did any patient refuse proctologic surgery (elective or urgent) at your centre after COVID‐19 outbreak? |
| 1 | Not applicable – proctologic surgery has fully stopped |
| 2 | No |
| 3 | Yes |
| Q16_a | How many, approximately? |
| 1 | 1–5 |
| 2 | 6–10 |
| 3 | 11–20 |
| 4 | >20 |
| Q16_b | For what reason(s)? |
| 1 | Fear of being infected |
| 2 | Other |
| Q16_b_i | If you selected Other, please specify: |
| Q17 | Have you ever tested positive for COVID‐19? |
| 1 | Yes |
| 2 | No |
| Q18 | To what extent has the elective proctologic surgery reduced at your centre for oncologic disease? |
| 1 | 0% – unaltered |
| 2 | Less than 50% |
| 3 | More than 50% |
| 4 | 100% – fully stopped |
| Q18_a | For what reason(s)? |
| 1 | Reduced number of patients |
| 2 | Unavailability of operative rooms |
| 3 | Lack of nurses |
| 4 | Lack of anaesthetists |
| 5 | Lack of surgeons |
| 6 | Hospital directions |
| 7 | Other |
| Q18_a_i | If you selected Other, please specify: |
| Q18_b | Are patients undergoing oncological proctologic surgery tested for COVID‐19? |
| 1 | Prior to surgery |
| 2 | Prior and after surgery |
| 3 | After surgery |
| 4 | Never |
| Q18_c | In case of COVID‐19 positivity prior to surgery? |
| 1 | The operation is rescheduled |
| 2 | Surgery is performed in accordance to local protocols thence transferring the patient to a dedicated COVID‐19 ward |
| 3 | Surgery is performed in accordance to local protocols thence transferring the patient to a mixed COVID‐19 positive/negative ward |
| Q18_d | Do you find flaws or delay in the management of oncological patient? |
| 1 | Yes |
| 2 | No |
| Q18_d_i | For what reason(s)? |
| 1 | Impossibility to operate |
| 2 | Delay in performing endoscopic procedures |
| 3 | Delay in getting radiological imaging |
| 4 | Delay in getting histopathological reports |
| 5 | Suspension of multidisciplinary team meetings |
| 6 | Other |
| Q18_d_i_a | If you selected Other, please specify: |
| Q18_e | Have you recently treated any HSIL (high‐grade squamous intraepithelial neoplasia)? |
| 1 | Yes without case selection criteria |
| 2 | Yes but only in high‐risk patients |
| 3 | No |
| Q19 | To what extent has the elective proctologic surgery reduced at your centre for benign disease? |
| 1 | 0% – unaltered |
| 2 | Less than 50% |
| 3 | More than 50% |
| 4 | 100% – fully stopped |
| Q19_a | For what reason(s)? |
| 1 | Reduced number of patients |
| 2 | Unavailability of operative rooms |
| 3 | Lack of nurses |
| 4 | Lack of anaesthetists |
| 5 | Lack of surgeons |
| 6 | Hospital directions |
| 7 | Other |
| Q19_a_i | If you selected Other, please specify: |
| Q19_b | In which setting are you currently performing elective surgery for benign disease? |
| 1 | Operative room |
| 2 | Outpatients clinic |
| 3 | Both |
| Q20 | To what extent has the urgent proctologic surgery reduced at your centre? |
| 1 | 0% – unaltered |
| 2 | Less than 50% |
| 3 | More than 50% |
| 4 | 100% – fully stopped |
| Q20_a | For what reason(s)? |
| 1 | Reduced number of patients |
| 2 | Unavailability of operative rooms |
| 3 | Lack of nurses |
| 4 | Lack of anaesthetists |
| 5 | Lack of surgeons |
| 6 | Hospital directions |
| 7 | Other |
| Q20_a_i | If you selected Other, please specify: |
| Q21 | Are patients undergoing urgent proctologic surgery tested for COVID‐19? |
| 1 | Prior to surgery |
| 2 | Prior and after surgery |
| 3 | After surgery |
| 4 | Never |
| Q22 | Are urgent proctologic procedures usually performed by a proctologist at your unit? |
| 1 | Yes |
| 2 | No |
| Q23 | To what extent has the outpatient proctologic activity reduced at your centre? |
| 1 | 0% – unaltered |
| 2 | Less than 50% |
| 3 | More than 50% |
| 4 | 100% – fully stopped |
| Q23_a | For what reason(s)? |
| 1 | Local hospital directions |
| 2 | National directions |
| 3 | Other |
| Q23_a_i | If you selected Other, please specify: |
| Q23_b | Have you managed to increase in‐between visits’ time interval? |
| 1 | Yes |
| 2 | No |
| Q23_b_i | For what reason(s)? |
| 1 | Social distance in waiting rooms |
| 2 | Need time to clean the rooms |
| 3 | Time spent for wearing personal protective equipment |
| Q23_c | Have the patients been called for preliminary anamnesis before coming to the visit? |
| 1 | Yes |
| 2 | No |
| Q23_c_i | Do you perform anamnestic evaluation for COVID‐19 before starting the visit? |
| 1 | Yes |
| 2 | No |
| Q23_d | Have the patients been screened for COVID‐19 before attending the visit? |
| 1 | Yes |
| 2 | No |
| Q23_e | Do you regularly use personal protective equipment (PPE) during the visit? |
| 1 | Yes |
| 2 | No |
| Q23_f | Do you think that a decreased outpatient activity may lead to diagnostic delay of rectal/anal cancer? |
| 1 | Yes |
| 2 | No |
| Q23_g | Have you discontinued HRA (high resolution anoscopy) and related procedures (i.e. biopsy) at all? |
| 1 | Yes |
| 2 | No |
| Q24 | To what extent have the visits/procedures for sexually transmitted disease (STD) reduced at your centre? |
| 1 | 0% – unaltered |
| 2 | Less than 50% |
| 3 | More than 50% |
| 4 | 100% – fully stopped |
| Q24_a | Is there a dedicated STD pathway in your hospital? |
| 1 | Yes |
| 2 | No |
| Q25 | To what extent have the visits/procedures for pelvic floor disorders reduced at your centre? |
| 1 | 0% – unaltered |
| 2 | Less than 50% |
| 3 | More than 50% |
| 4 | 100% – fully stopped |
| Q25_a | Is there a dedicated pathway for the management of pelvic floor disorders in your hospital? |
| 1 | Yes |
| 2 | No |
| Q26 | Before the COVID‐19 emergency, were anorectal physiology tests (manometry, EAUS, etc.) performed at your centre? |
| 1 | Yes |
| 2 | No |
| Q26_a | Are you still performing anorectal physiology tests? |
| 1 | Yes |
| 2 | No |
| Q26_a_i | Which of the following anorectal physiology tests are still performed at the moment? |
| 1 | Anorectal manometry |
| 2 | Endorectal ultrasound |
| 3 | Neurophysiology tests |
| 4 | X‐ray defecography |
| 5 | MRI defecography |
| Q27 | Have patients with pre‐booked visit or surgery been rescheduled? |
| 1 | Not yet |
| 2 | Yes, in 1–3 months according to the waiting list |
| 3 | Yes, after balancing the urgency of the case with the risks related to COVID‐19 |
| 4 | Yes, until the end of pandemic |
Appendix 2.
CHECKLIST FOR REPORTING RESULTS OF INTERNET E‐SURVEYS (CHERRIES) [19]
| Item category | Checklist item | Page no. | Description |
|---|---|---|---|
| Design | Study design | Page 2 | The target population were colorectal surgeons with an interest in coloproctology |
| Ethics | Ethics approval | Page 2 | This study was exempt from review board approval at authors’ institutions |
| Informed consent | Page 2 | All participants, as members of a web‐based panel, had already provided informed consent to participate in online surveys. Informed consent for the present survey was obtained from all those agreeing to complete a survey, with participants informed on the welcome page that the survey concerned the current status of proctology, that it would take approximately 8 min to complete, that all responses were confidential and anonymous and that reporting would be on an aggregate level only. Consent was indicated when respondents clicking the ‘Accept’ button from this page | |
| Data protection | Page 3 | Proprietary survey software and local servers were used to ensure data protection. No personal information was linked to survey results in any way. The fully de‐identified dataset is kept on password‐protected computers | |
| Development and pretesting | Page 3 | Co‐authors (GG, AS, VDS, IG, UG) piloted the survey, assessed the design and checked the feasibility and validity of the questions. Estimated mean time to complete the survey was 8 min | |
| Recruitment process | Open versus closed survey | Page 2 | This was an open survey. Participants were recruited through dedicated scientific societies advertisement and social media. A closed number of participants belonging to two of the most renowned scientific societies in the field was also recruited via email invitation |
| Contact mode | Page 2 | The initial contact with the potential participants was made on the Internet | |
| Recruitment process (cont'd) | Advertising the survey | Page 2 | The survey was advertised on social media and among members of scientific societies in the field of coloproctology |
| Survey administration | Web/email | Pages 2–3 | This was a web‐based survey, with respondents channelled to ‘Online surveys’ (formerly BOS – Bristol Online Survey) site, developed by the University of Bristol. Responses were collected through the online survey platform and stored on secure local servers. Responses were single or multiple choice, numeric, and open text |
| Context | Pages 2–3 | The online survey platform is licensed by the Queen Mary University of London for research projects | |
| Mandatory/volun tary | Page 2 | Voluntary | |
| Incentives | Page 2 | No compensation offered | |
| Time/date | Page 3 | Responses were collected between 15 and 26 April 2020 | |
| Item randomisation | Page 3 | No randomisation of items was used | |
| Adaptive questioning | Page 3 | Adaptive questioning (branched) was used. Relevant survey items were displayed based on previous responses | |
| Number of items | Page 2 | A maximum of five items were displayed on any one survey page. The full survey comprised a total of 27 items, although because of the adaptive nature of the questionnaire, not all respondents answered all items | |
| Number of screens | Page 2 | The full survey was distributed over nine pages | |
| Completeness check | Page 3 | All survey items were deemed to be mandatory, and respondents prompted to complete outstanding items before leaving the survey page on which the item was contained | |
| Review step | Page 3 | Respondents were unable to change their responses once submitted | |
| Response rates | Unique site visitor | Page 2 | Determination of unique visitors was only possible for the closed group of participants who received an email invitation based on IP addresses |
| View rate | Page 2 | Not applicable | |
| Participation rate | Page 2 | Not applicable | |
| Completion rate | Page 3 | 100% | |
| Preventing multiple entries from same individual | Cookies used | Page 3 | No |
| IP check | Page 3 | No | |
| Log file analysis | Page 3 | Not used | |
| Registration | Page 3 | Not applicable | |
| Analysis | Handling of incomplete questionnaires | Page 3 | Not applicable |
| Questionnaires with atypical timestamp | Page 3 | No respondents were removed from the survey for completing the items too quickly. The minimum completed survey was timed at approximately 5 min | |
| Statistical correction | Page 3 | Not applicable |
Appendix 3.
LIST OF PARTICIPATING COUNTRIES
| Frequency | Per cent | Valid per cent | Cumulative per cent | |
|---|---|---|---|---|
| Italy | 299 | 28.5 | 28.5 | 28.5 |
| United States | 165 | 15.7 | 15.7 | 44.2 |
| Spain | 67 | 6.4 | 6.4 | 50.6 |
| Turkey | 57 | 5.4 | 5.4 | 56.0 |
| Portugal | 52 | 5.0 | 5.0 | 61.0 |
| Russian Federation | 51 | 4.9 | 4.9 | 65.8 |
| China | 36 | 3.4 | 3.4 | 69.2 |
| United Kingdom | 25 | 2.4 | 2.4 | 71.6 |
| Brazil | 23 | 2.2 | 2.2 | 73.8 |
| France | 18 | 1.7 | 1.7 | 75.5 |
| Canada | 16 | 1.5 | 1.5 | 77.0 |
| Argentina | 15 | 1.4 | 1.4 | 78.5 |
| Chile | 15 | 1.4 | 1.4 | 79.9 |
| Greece | 15 | 1.4 | 1.4 | 81.3 |
| Belgium | 14 | 1.3 | 1.3 | 82.7 |
| Egypt | 14 | 1.3 | 1.3 | 84.0 |
| Mexico | 14 | 1.3 | 1.3 | 85.3 |
| Germany | 13 | 1.2 | 1.2 | 86.6 |
| Netherlands | 11 | 1.0 | 1.0 | 87.6 |
| Australia | 9 | 0.9 | 0.9 | 88.5 |
| Romania | 9 | 0.9 | 0.9 | 89.3 |
| Switzerland | 9 | 0.9 | 0.9 | 90.2 |
| Denmark | 8 | 0.8 | 0.8 | 91.0 |
| Japan | 6 | 0.6 | 0.6 | 91.5 |
| United Arab Emirates | 5 | 0.5 | 0.5 | 92.0 |
| Bulgaria | 4 | 0.4 | 0.4 | 92.4 |
| Ireland | 4 | 0.4 | 0.4 | 92.8 |
| Singapore | 4 | 0.4 | 0.4 | 93.1 |
| Belarus | 3 | 0.3 | 0.3 | 93.4 |
| Bolivia, Plurinational State of | 3 | 0.3 | 0.3 | 93.7 |
| Finland | 3 | 0.3 | 0.3 | 94.0 |
| India | 3 | 0.3 | 0.3 | 94.3 |
| Iraq | 3 | 0.3 | 0.3 | 94.6 |
| Israel | 3 | 0.3 | 0.3 | 94.9 |
| Pakistan | 3 | 0.3 | 0.3 | 95.1 |
| Serbia | 3 | 0.3 | 0.3 | 95.4 |
| Venezuela, Bolivarian Republic of | 3 | 0.3 | 0.3 | 95.7 |
| Colombia | 2 | 0.2 | 0.2 | 95.9 |
| Ecuador | 2 | 0.2 | 0.2 | 96.1 |
| Guatemala | 2 | 0.2 | 0.2 | 96.3 |
| Iran, Islamic Republic of | 2 | 0.2 | 0.2 | 96.5 |
| Jordan | 2 | 0.2 | 0.2 | 96.7 |
| Korea, Republic of | 2 | 0.2 | 0.2 | 96.9 |
| Latvia | 2 | 0.2 | 0.2 | 97.0 |
| Panama | 2 | 0.2 | 0.2 | 97.2 |
| Peru | 2 | 0.2 | 0.2 | 97.4 |
| Philippines | 2 | 0.2 | 0.2 | 97.6 |
| Poland | 2 | 0.2 | 0.2 | 97.8 |
| Saudi Arabia | 2 | 0.2 | 0.2 | 98.0 |
| Sweden | 2 | 0.2 | 0.2 | 98.2 |
| Algeria | 1 | 0.1 | 0.1 | 98.3 |
| Aruba | 1 | 0.1 | 0.1 | 98.4 |
| Austria | 1 | 0.1 | 0.1 | 98.5 |
| Azerbaijan | 1 | 0.1 | 0.1 | 98.6 |
| Bangladesh | 1 | 0.1 | 0.1 | 98.7 |
| Cameroon | 1 | 0.1 | 0.1 | 98.8 |
| Cyprus | 1 | 0.1 | 0.1 | 98.9 |
| Czech Republic | 1 | 0.1 | 0.1 | 99.0 |
| Hong Kong | 1 | 0.1 | 0.1 | 99.0 |
| Jersey | 1 | 0.1 | 0.1 | 99.1 |
| Lebanon | 1 | 0.1 | 0.1 | 99.2 |
| Lithuania | 1 | 0.1 | 0.1 | 99.3 |
| New Zealand | 1 | 0.1 | 0.1 | 99.4 |
| Norway | 1 | 0.1 | 0.1 | 99.5 |
| Paraguay | 1 | 0.1 | 0.1 | 99.6 |
| Puerto Rico | 1 | 0.1 | 0.1 | 99.7 |
| Senegal | 1 | 0.1 | 0.1 | 99.8 |
| Taiwan, Province of China | 1 | 0.1 | 0.1 | 99.9 |
| Trinidad and Tobago | 1 | 0.1 | 0.1 | 100.0 |
| Total | 1050 | 100.0 | 100.0 |
Appendix 4.
Mixed‐effects logistic regression models exploring the chance of COVID‐19 positivity with geographic distribution as random effect.
| COVID‐19 positivity | ||||
|---|---|---|---|---|
| Odds ratio | 95% CI | P | ||
| Lower | Upper | |||
| Age | 0.991 | 0.972 | 1.010 | 0.341 |
| Gender | ||||
| Female (reference) | ||||
| Male | 1.741 | 1.015 | 2.988 | 0.044 |
| Type of hospital | ||||
| Nonteaching (reference) | ||||
| Academic or teaching | 0.863 | 0.509 | 1.461 | 0.582 |
| Hospital rearrangement | ||||
| Fully dedicated to COVID‐19 (reference) | ||||
| Partially dedicated or not involved | 0.718 | 0.421 | 1.223 | 0.223 |
| External facilities for proctological surgery | ||||
| Unavailable (reference) | ||||
| Available | 1.915 | 1.244 | 2.949 | 0.003 |
| PPE | ||||
| Unavailable (reference) | ||||
| Readily available | 0.748 | 0.483 | 1.159 | 0.194 |
| Status of proctological activities | ||||
| Fully stopped (reference) | ||||
| Emergency | 0.648 | 0.360 | 1.167 | 0.149 |
| Elective | 0.700 | 0.417 | 1.174 | 0.177 |
| Use of PPE in theatre with SARS‐CoV‐2+ Pts | ||||
| Not always (reference) | ||||
| Always | 0.680 | 0.390 | 1.186 | 0.175 |
| Preoperative SARS‐CoV‐2 testing for Pts | ||||
| No (reference) | ||||
| Yes | 1.729 | 1.111 | 2.691 | 0.015 |
| Training level | ||||
| Other (reference) | ||||
| Consultant | 0.779 | 0.477 | 1.272 | 0.318 |
Abbreviations: PPE, personal protective equipment; Pts, patients.
Appendix 5.
Mixed‐effects logistic regression models exploring the chance of rescheduling patients on the waiting list for surgery or an outpatient visit, with geographic distribution as random effect.
| Patients rescheduled | ||||
|---|---|---|---|---|
| Odds ratio | 95% CI | P | ||
| Lower | Upper | |||
| Age | 0.987 | 0.975 | 0.999 | 0.045 |
| Gender | ||||
| Female (reference) | ||||
| Male | 0.887 | 0.607 | 1.298 | 0.538 |
| Type of hospital | ||||
| Nonteaching (reference) | ||||
| Academic or teaching | 1.241 | 0.862 | 1.788 | 0.246 |
| Hospital rearrangement | ||||
| Fully dedicated to COVID‐19 (reference) | ||||
| Partially dedicated or not involved | 0.914 | 0.608 | 1.372 | 0.663 |
| External facilities for proctological surgery | ||||
| Unavailable (reference) | ||||
| Available | 1.060 | .754 | 1.489 | .739 |
| PPE | ||||
| Unavailable (reference) | ||||
| Readily available | 0.919 | 0.668 | 1.266 | 0.608 |
| Status of proctological activities | ||||
| Fully stopped (reference) | ||||
| Emergency | 1.579 | 1.032 | 2.417 | 0.035 |
| Elective | 1.747 | 1.188 | 2.571 | 0.005 |
Abbreviation: PPE, personal protective equipment.
Appendix 6.
PROCTOLOCK2020 WORKING GROUP
Collaborators to be indexed
Italian Society of Colorectal Surgery (SICCR) Steering Committee: Domenico Aiello, Francesco Bianco, Andrea Bondurri, Gaetano Gallo, Marco La Torre, Giovanni Milito, Roberto Perinotti, Renato Pietroletti, Alberto Serventi, Marina Fiorino.
Young Group of the Italian Society of Colorectal Surgery (Y‐SICCR): Veronica De Simone, Ugo Grossi, Michele Manigrasso, Alessandro Sturiale, Gloria Zaffaroni.
Mediterranean Society of Coloproctology (MSCP): Ferruccio Boffi.
Dissemination Committee. Italy: Francesco Cantarella, Simona Deidda, Salomone Di Saverio, Fabio Marino, Jacopo Martellucci, Marco Milone, Francesco Pata, Arcangelo Picciariello. Spain: Ana Minaya Bravo, Vincenzo Vigorita; Portugal: Miguel Fernandes Cunha; Turkey: Sezai Leventoglu; Russia Tatiana Garmanova, Petr Tsarkov; Denmark: Alaa El‐Hussuna; France: Alice Frontali; Greece: Argyrios Ioannidis; Belgium Gabriele Bislenghi; Egypt: Mostafa Shalaby; Chile: Felipe Celedon Porzio; China: Jiong Wu; The Netherlands: David Zimmerman.
External Advisors: Claudio Elbetti, Julio Mayol, Gabriele Naldini, Mario Trompetto, Giuseppe Sammarco, Giulio Aniello Santoro.
Gaetano Gallo, Alessandro Sturiale, Veronica De Simone, Gian Luca Di Tanna, Iacopo Giani and Ugo Grossi shared first author position.
Contributor Information
Gaetano Gallo, Email: gaethedoctor@alice.it, @Gae_Gallo.
the ProctoLock 2020 Working Group:
Domenico Aiello, Francesco Bianco, Andrea Bondurri, Marco La Torre, Giovanni Milito, Roberto Perinotti, Renato Pietroletti, Alberto Serventi, Marina Fiorino, Michele Manigrasso, Gloria Zaffaroni, Ferruccio Boff, Francesco Cantarella, Simona Deidda, Salomone Di Saverio, Fabio Marino, Jacopo Martellucci, Marco Milone, Francesco Pata, Arcangelo Picciariello, Ana Minaya Bravo, Vincenzo Vigorita, Miguel Fernandes Cunha, Sezai Leventoglu, Tatiana Garmanova, Petr Tsarkov, Alaa El‐Hussuna, Alice Frontali, Argyrios Ioannidis, Gabriele Bislenghi, Mostafa Shalaby, Felipe Celedon Porzio, Jiong Wu, David Zimmerman, Claudio Elbetti, Julio Mayol, Gabriele Naldini, Mario Trompetto, Giuseppe Sammarco, and Giulio Aniello Santoro
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Wu Y, Ho W, Huang Y, Jin DY, Li S, Liu SL, et al. SARS‐CoV‐2 is an appropriate name for the new coronavirus. Lancet. 2020;395:949‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. https://coronavirus.jhu.edu.
- 3. COVIDSurg Collaborative . Global guidance for surgical care during the COVID‐19 pandemic. Br J Surg. 2020. 10.1002/bjs.11646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Gagliano A, Villani PG, Co FM, Manelli A, Paglia S, Bisagni PAG, et al. COVID‐19 epidemic in the middle province of northern Italy: impact, logistics, and strategy in the first line hospital. Disaster Med Public Health Prep. 2020;1‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gallo G, Trompetto M. The effects of COVID‐19 on academic activities and surgical education in Italy. J Invest Surg. 2020;33:687‐9. [DOI] [PubMed] [Google Scholar]
- 6. Giani I, Elbetti C, Trompetto M, Gallo G. Proctology in the COVID‐19 era: handle with care. Br J Surg. 2020;107:e243. 10.1002/bjs.11676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. https://www.facs.org/covid‐19/clinical‐guidance/triage
- 8. Gallo G, La Torre M, Pietroletti R, Bianco F, Altomare DF, Pucciarelli S, et al. Italian society of colorectal surgery recommendations for good clinical practice in colorectal surgery during the novel coronavirus pandemic. Tech Coloproctol. 2020;24:501‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Di Saverio S, Pata F, Gallo G, Carrano F, Scorza A, Sileri P, et al. Coronavirus pandemic and Colorectal surgery: practical advice based on the Italian experience. Colorectal Dis. 2020;22:625‐34. [DOI] [PubMed] [Google Scholar]
- 10. Mascagni D, Eberspacher C, Mascagni P, Arezzo A, Selvaggi F, Sturiale A, et al. From high volume to "zero" proctology: Italian experience in the COVID era. Int J Colorectal Dis. 2020;35:1777‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gallo G, Sturiale A, De Simone V, Mancini S, Di Tanna GL, Milito G, et al. Deadlock of proctologic practice in Italy during COVID‐19 pandemic: a national report from ProctoLock2020. Updates Surg. 2020;1–7: 10.1007/s13304-020-00860-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gallo G, Sturiale A, De Simone V, Di Tanna GL, Bianco F, Perinotti R, et al. The impact of COVID‐19 on proctologic practice in Italy. Tech Coloproctol. 2020;24:1103–1104. 10.1007/s10151-020-02319-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wu Y, Guo C, Tang L, Hong Z, Zhou J, Dong X, et al. Prolonged presence of SARS‐CoV‐2 viral RNA in faecal samples. Lancet Gastroenterol Hepatol. 2020;5:434‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gupta S, Parker J, Smits S, Underwood J, Dolwani S. Persistent viral shedding of SARS‐CoV‐2 in faeces ‐ a rapid review. Colorectal Dis. 2020;22:611‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Stewart CL, Thornblade LW, Diamond DJ, Fong Y, Laleh G, Melstrom LG. Personal protective equipment and COVID‐19 – a review for surgeons. Ann Surg. 2020;272:e132‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Livingston EH. Surgery in a time of uncertainty: a need for universal respiratory precautions in the operating room. JAMA. 2020;323:2254‐5. [DOI] [PubMed] [Google Scholar]
- 17. Fu SJ, George EL, Maggio PM, Hawn M, Nazerali R. The consequences of delaying elective surgery: surgical perspective. Ann Surg. 2020;272:e79–e80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ratto C, Grossi U, Litta F, Di Tanna GL, Parello A, De Simone V, et al. Contemporary surgical practice in the management of anal fistula: results from an international survey. Tech Coloproctol. 2019;23:729‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Eysenbach G. Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E‐Surveys (CHERRIES). J Med Internet Res. 2004;6:e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. https://www.who.int/docs/default‐source/coronaviruse/situation‐reports/20200420‐sitrep‐91‐covid‐19.pdf?sfvrsn=fcf0670b_10
- 21. Colorectal surgery–the Cinderella specialty. Br Med J. 1981;283:557‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wallis CJ, Ravi B, Coburn N, Nam RK, Detsky AS, Satkunasivam R. Comparison of postoperative outcomes among patients treated by male and female surgeons: a population based matched cohort study. BMJ. 2017;359:j4366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. https://www.aamc.org/news‐insights/where‐are‐all‐women‐surgery.
- 24. https://www.facs.org/education/resources/medical‐students/faq/specialties.
- 25. The Lancet . COVID‐19: protecting health‐care workers. Lancet. 2020;395:922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Giulio M, Maggioni D, Montroni I, Ugolini G, Capelli P, Ceppi L, et al. Being a doctor will never be the same after the COVID‐19 pandemic. Am J Med. 2020;133:652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Coons BE, Tam SF, Okochi S. Rapid development of resident‐led procedural response teams to support patient care during the coronavirus disease 2019 epidemic: a surgical workforce activation team. JAMA Surg. 2020: 10.1001/jamasurg.2020.1782. [DOI] [PubMed] [Google Scholar]
- 28. Guo YR, Cao QD, Hong ZS, Tan YY, Chen SD, Jin HJ, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID‐19) outbreak ‐ an update on the status. Mil Med Res. 2020;7:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Tian Y, Rong L, Nian W, He Y. Review article: gastrointestinal features in COVID‐19 and the possibility of faecal transmission. Aliment Pharmacol Ther. 2020;51:843‐51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID‐19. Lancet Child Adolesc Health. 2020;4:e10‐1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Pellino G, Spinelli A. How COVID‐19 outbreak is impacting colorectal cancer patients in Italy: a long shadow beyond infection. Dis Colon Rectum. 2020;63:720‐2. [DOI] [PubMed] [Google Scholar]
- 32. Andreassen CS, Pallesen S, Griffiths MD. The relationship between addictive use of social media, narcissism, and self‐esteem: findings from a large national survey. Addict Behav. 2017;64:287‐93. [DOI] [PubMed] [Google Scholar]
- 33. Capretti G, Boggi U, Salvia R, Belli G, Coppola R, Falconi M, et al. Application of minimally invasive pancreatic surgery: an Italian survey. Updates Surg. 2019;71:97‐103. [DOI] [PubMed] [Google Scholar]
- 34. Yao K, Belkora J, Sisco M, Rosenberg S, Bedrosian I, Liederbach E, et al. Survey of the deficits in surgeons’ knowledge of contralateral prophylactic mastectomy. JAMA Surg. 2016;151:391‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


