Abstract
Background
A large number of the population experienced panic during the pandemic of the coronavirus disease 2019 (COVID‐19) in China. The current study explored the trajectory of panic and its associated factors to develop promising strategies for controlling the global spread of COVID‐19 and improving the mental health emergency management.
Methods
A total of 812 unmarried adults (aged from 18 to 42 years, M = 23.3, SD = 3.45) from all over China participated online in our investigation. A Growth Mixture Model (GMM) was developed and analysed.
Results
Three classes of trajectories for panic were identified: the “continuous decline group (CDG)”, the “continuous low group (CLG),” and the “continuous high group (CHG)”. With reference to the CDG, people in the CHG were more sensitive to social factors. With reference to the CDG, people in the CLG were more likely to possess some of the following traits: being men, in Hubei Province (center of the pandemic), with a lower income, and less sensitive towards social factors and individual factors. With reference to the CLG, people in the CHG were more likely to be women, located outside of Hubei Province, and more sensitive to social factors, family factors, and individual factors.
Conclusion
Social factors, family factors, and individual factors predicted the different trajectories of panic.
Keywords: COVID‐19, family factors, individual factors, panic, social factors, trajectory
INTRODUCTION
The Coronavirus Disease 2019 (COVID‐19) has been spreading since December 2019. The number of confirmed cases and deaths has been rising since its discovery (Song et al., 2020). Outbreaks of infectious diseases usually bring a great deal of panic and fear throughout society (Okeyo & Dowse, 2018). The COVID‐19 may cause severe pneumonia with clusters of illness onsets (Zhao et al., 2020) that expand on the symptoms. People are more likely to panic about diseases when coupled with a high risk of infection (Wang & Lin, 2003; Xu et al., 2020). During the COVID‐19 pandemic, the data from the Psychological Assistance Hotline of Beijing Normal University indicated that almost 44 per cent of clients suffered with panic and panic‐related issues. Moreover, panic may cause both behavioral (e.g. irrational behavior) and physical damages (e.g. impair the immune system), increasing the risk of infection (Arafat, Kar, Marthoenis, Sharma, & Kabir, 2020; Sim, Chua, Vieta, & Fernandez, 2020; Wang & Lin, 2003; Yu, 2020). Therefore, in the time of the COVID‐19 pandemic, it is urgent to explore the mechanism of public panic to alleviate the harm from the perspective of mental health.
Studies on mental health in China indicated that married people suffered fewer mental problems than unmarried people (e.g. Feng et al., 2018; Song et al., 2020). Feng and his colleagues selected 2,396 residents in Wuxi city (a city in the Jiangsu province) to investigate the influencing factors on mental health status, and found that being unmarried, divorced, or widowed were risk factors for mental health. Univariate analysis in this study showed that the prevalence of psychological problems among unmarried people was significantly higher than that among married people. Song and his colleagues’ study during the COVID‐19 period also found the same results. The explanation might be that unmarried people could not get help in time when they encountered difficulties, and there was no emotional support when they needed to be heard, which might easily lead to anxiety, depression, and other mental problems (Fu et al., 2017; Li, 2015). On the bases of these studies and the actual situation of COVID‐19, unmarried adults deserve more attention.
Previous research has explored the emergence of panic and its stages. In an unprecedented emergency, a psychological crisis could emerge. Unless the crisis was alleviated in time, it might result in panic due to physical, emotional, cognitive, or behavioral dysfunctions (Wu, 2006). One study summed up the stages of panic as anxiety stage, calm stage, and problem‐solving stage (Wu, 2009). Nevertheless, the trajectory of panic needs to be further explored with data and taking individual differences into account.
Many of the previous studies on panic involved its influencing factors (e.g. Kelley, Condry, Dahlke, & Hill, 1965; Liao, Li, Zhao, Yan, & Chen, 2003; Wang, 2003). One study presented the associated factors for the degree, the duration, and the manifestation of panic (Wu, 2009). First, the characteristics of emergencies are the basic inducement to panic. People tend to be more panic when faced with a greater degree of destruction. The second influencing factor is the authenticity and emotional implication of information. When people receive incomplete information, their judgment and decision‐making are limited, leaving an incomplete description and unreasonable evaluation of the crisis to cause panic. Additionally, people often experience a higher degree of panic when receiving negative information. Third, the social supports, such as proper information disclosure and unified medical treatment, effectively control the spread of infection and greatly alleviate panic. Finally, individual characteristics, including physical state, age, gender, cognition, and perception, constitute an influencing factors of panic. The effect of panic perception could be explained by constructivism theory (Speier & Price, 1998). To be more specific, emergencies might impinge on the cognitive schema and appear the cognitive bias of risk, which leads to more panic.
Ecological systems theory mainly refers to the relationship between individual development and the social environment (Bronfenbrenner, 1977). Each environment, such as family or society, plays an important and distinct role in the individual's life. Moreover, family, as an important factor in the mezzo system of ecological systems theory (e.g. Cassarino & Murphy, 2018; Friesen, 2012), has not been given enough attention in previous studies on panic in public health emergency settings. To the best of our knowledge, a study during the SARS pandemic pointed out that relying on family was a predictor of panic (Xie, Zheng, Xie, & Wang, 2005). Recently, studies have shown that quarantine and “stay at home” measures during the COVID‐19 pandemic might have a negative psychological impact on people (Brooks, Webster, Smith, Woodland, & Rubin, 2020), while insufficient attention to family relations during the epidemic was reported (Liu et al., 2020). Previous research and the current situation suggested that family factors should be considered to further clarify how family factors affect the trajectory of panic.
Hence, a comprehensive consideration of social factors, family factors, and individual factors could contribute to a deeper understanding of the mechanisms underlying different trajectories of panic. The purpose of the present study was to investigate the different trajectories of panic and its predictors among Chinese population during the COVID‐19 pandemic. In this study, the degrees of panic at different times were measured during the COVID‐19 pandemic. The resulting trajectories and the predictive factors were discussed. Among the predictive factors, we focused on social factors, family factors, and individual factors. We postulated that there was individual heterogeneity in the trajectory of panic, which was predicted by social factors, family factors, and individual factors, as well as demographic factors such as gender, age, location, and income.
METHOD
Participants
The online questionnaire was used to explore the different trajectories of panic and the associated factors among Chinese population during the COVID‐19 pandemic. During April 2020, 812 unmarried Chinese adults from all over China participated in this research through Wenjuanxing (questionnaire star), an online survey platform. The participants varied in age from 18 to 42 years (M = 23.3, SD = 3.45), of which 28.4 per cent were men and 71.6 per cent were women. Location during the time of pandemic was considered to be a determining factor regarding its influence on panic level. In all, 35.8 per cent of the participants were from Hubei province and 64.2 per cent were from Hubei province. Hubei province, the center of the epidemic area with above 80 per cent of confirmed cases and 90 per cent of the deaths during the COVID‐19 pandemic in China, was categorised as high risk, while the rest of China, with a small number of confirmed cases and deaths, was categorised as low risk. In terms of family income, the individual average monthly income in China is 8,572 CNY (1,239 USD). In the current sample, 3.7 per cent of families had more than 30,001 CNY (4,306 USD), 25.2 per cent had 10,001–30,000 CNY (1,436–4,306 USD), 37.1 per cent had 5,001–10,000 CNY (718–1,435 USD), 27.6 per cent had 2,001–5,000 CNY (287–717 USD), and 6.4 per cent had less than 2,000 CNY (287 USD).
Survey Procedure
First, we prepared the initial questionnaire according to the relavant literature and the specific circumstances of the epidemic. Then, one professor and five students majored in psychology were invited to evaluate and revise the initial version. Taking their opinions into account, the items in the questionnaire were adjusted, including incorrect words, unreasonable questions, unreasonable options, and irrelevant items. Finally, the questionnaires were uploaded onto Wenjuanxing to collect the survey data. In addition, informed consent was presented at the beginning of the questionnaire, and quality control items were set up in the questionnaire system (e.g. a simple mathematical calculation, a missing item reminder). Payment of 10 CNY (1.43 USD) was given to the participants after the questionnaire was completed. The research protocol was approved by the Institutional Review Board of Beijing Normal University.
Measures
Regarding the development of COVID‐19, three crucial messages marked changes in the perception of the disease in China. T1 was at the end of January 2020. This time point was signified by (1) Zhong Nanshan, the Chinese representative pulmonologist during the COVID‐19 pandemic, who affirmed that the virus could spread from person to person in close contact, and by (2) the Wuhan lockdown shortly after Zhong’s announcement. T2 was at mid‐February 2020. This time point was signified by (1) the fact that new confirmed cases were over 10,000 in China (including clinical diagnosis), and by (2) the proposal of aerosol transmission. T3 was during mid‐late March. This time point was signified by (1) the global outbreak of COVID‐19 leading to a pandemic classification from WHO and by (2) an increase in confirmed cases from abroad when many regions of China began to gradually lift the blockade.
At each time, participants were asked to recall the object of panic (e.g. What do you panic about?) using a multiple‐choice format (e.g. (a) Fear of infection from the virus; (b) Shortage of supplies for living and epidemic prevention; (c) Shortage of medical supplies; (d) Isolated from home; (e) Request for return to work; (f) Others). Participants were then asked to evaluate the extent of that recall (e.g. Please evaluate the extent of the recall for the signs of panic using a 5‐point Likert scale ranging from 1 (No recollection at all) to 5 (Complete recollection). Then, participants were asked to assess their own degree of panic using a 7‐point Likert scale ranging from 1 (No panic at all) to 7 (Extreme panic).
Finally, we measured the predictive factors of panic from social, family, and individual perspectives. We directly asked participants the degree of agreement with causes for panic using a 5‐point Likert scale ranging from 1 (Totally disagree) to 5 (Totally agree). For social factors, we directly asked participants how much they agreed that the social causes of panic were the highly contagious virus, the large number of infections, the insufficient supply of medical materials, and a lot of negative information. For family factors, we directly asked the participants how much they agreed with the family cause of panic as the lack of understanding and communication between parents and children. For individual factors, we used four adapted items (e.g. “I think the COVID‐19 impacts me deeply”) from a study during the SARS pandemic to measure the perception of COVID‐19 (Xie, Zheng, Xie, & Wang, 2005).
Data Analyses
SPSS 22.0 and Mplus7.4 were adopted to analyse data. The descriptive analysis and Pearson correlation analysis of participants’ demographic variables, independent variables, and dependent variables were carried out first. Then, the Growth Mixture Model (GMM) was used to identify subclasses corresponding to distinct patterns of growth (Muthén & Muthén, 2000) for panic. This is different from the Latent Class Growth Model (LGCM) without consideration of individual differences, and LCGM required homogeneity within a class. On the other hand, the GMM allows all individuals within the category to estimate freely (Feldman, Masyn & Conger, 2009; Muthén & Asparnuhov, 2008). It has been argued that once the optimum unconditional model has been established, it would be necessary to examine the parameters through the conditional model (Muthén, 2003). In addition, previous studies have also shown that the accuracy of classification could be improved when covariates are included in the GMM (Petras & Masyn, 2010). Therefore, the demographic variables (gender, age, location, income) together with social factors, family factors, and individual factors were included in the optimal trajectory subclass of panic. Finally, the R3STEP was used to further investigate the predictive effects of time‐invariant and time‐varying covariates on panic subclass trajectories.
To evaluate the accuracy of classification, several fit indices including the Akaike Information Criterion (AIC), Bayesian information criterion (BIC), adjusted BIC (aBIC), Entropy, Lo‐Mendell‐Rubin Likelihood ratio test (LMR), Bootstrapped Likelihood ratio test (BLRT) were adopted (e.g. Dias, 2007; Gomez, Skilbeck, Thomas, & Slatyer, 2017; Nylund et al, 2007; Yang, 2006). Generally, the smaller statistical values of AIC, BIC, aBIC indicate a better fit. The value of entropy ranges from 0 to 1; the larger value indicates the more accurate classification. For example, when the entropy is <0.6, it means that 20 per cent of individuals have classification errors, and when the entropy is ≥0.8, the accuracy of classification is as high as 90 per cent (Nylund et al., 2007). Due to the limitations of simulation conditions, entropy may only be used as a reference (He, 2019). Both Bootstrapped Likelihood Ratio Teas (BLRT; McLachlan & Peel, 2000) and Lo‐Mendell‐Rubin (LMR; Lo, Mendell, & Rubin, 2001) test a model with K classes versus a model with K‐1 classes. A significant p‐value indicates that the model with K classes is better than the model with K‐1 classes (Gomez, Skilbeck, Thomas, & Slatyer, 2017).
RESULTS
Descriptions and Correlations of Variables
The means, standard deviations of each variable, and bivariate correlations among variables are listed in Table 1. For the average degree of panic, the overall score was on the medium side with a trend of first rising and then decreasing. Except for family factors at T1 that was not significantly correlated with the degree of panic at T2, it showed that social factors, family factors, and individual factors were all positively correlated with the degree of panic at all three time points (ps < .05). These results generally indicated that a higher degree of approval of negative social factors, worse parent‐child relationship, and higher negative perception were associated with a higher degree of panic across the time points. As for the demographic variables, except for age and income that were not significantly correlated with the degree of panic at T3, it showed that gender, age, location, and income were significantly positively correlated with the degree of panic at all three time points (ps < .05). These results generally indicated that these demographic traits were more associated with a higher degree of panic: being women, older age, out of Hubei province during the pandemic, and with a higher income. On the other hand, these demographic traits were more associated with a lower degree of panic accordingly: men, younger age, people locating in Hubei province during the pandemic, and having a lower income.
TABLE 1.
Correlation between Demographic and Observed Variables (N = 812)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 71 Gender | – | |||||||||||||||
| 2 Age | −.09** | − | ||||||||||||||
| 3 Location | .08* | −.04 | – | |||||||||||||
| 4 Income | .03 | .20*** | .23*** | – | ||||||||||||
| 5T1 Social factors | .16*** | .07* | .05 | .15*** | – | |||||||||||
| 6T2 Social factors | .12*** | .10** | .03 | .14*** | .59*** | – | ||||||||||
| 7T3 Social factors | .11** | .10** | .04 | .10** | .37*** | .47*** | – | |||||||||
| 8T1 Family factors | .05 | −.09** | .03 | −.07 | .02 | −.003 | .09* | – | ||||||||
| 9T2 Family factors | .01 | −.07 | .02 | −.04 | .02 | .01 | .10** | .77*** | – | |||||||
| 10T3 Family factors | −.01 | −.06 | .02 | −.07* | −.02 | −.07* | .13*** | .72*** | .75*** | – | ||||||
| 11T1 Individual factors | .10** | .04 | .08* | .05 | .30*** | .27*** | .24*** | .19*** | .23*** | .19*** | – | |||||
| 12T2 Individual factors | .06 | −.02 | .06 | .03 | .23*** | .31*** | .26*** | .22*** | .30*** | .27*** | .74*** | – | ||||
| 13T3 Individual factors | .06 | .03 | .04 | .04 | .11** | .14*** | .32*** | .23*** | .27*** | .34*** | .61*** | .73*** | – | |||
| 14T1 Degree of panic | .14*** | .09* | .12*** | .12*** | .31*** | .31*** | .22*** | .07* | .12** | .07* | .44*** | .40*** | .30*** | – | ||
| 15T2 Degree of panic | .11** | .07* | .12** | .12*** | .31*** | .38*** | .25*** | .06 | .12** | .10** | .37*** | .44*** | .31*** | .79*** | – | |
| 16T3 Degree of panic | .07* | .05 | .16*** | .06 | .14*** | .18*** | .33*** | .13*** | .17*** | .21*** | .31*** | .35*** | .40*** | .60*** | .65*** | – |
| M | – | 23.3 | – | – | 3.65 | 3.57 | 3.25 | 2.34 | 2.38 | 2.23 | 2.86 | 2.83 | 2.23 | 4.03 | 4.15 | 3.64 |
| SD | – | 3.45 | – | – | .92 | 1.01 | 1.03 | 1.12 | 1.14 | 1.09 | .65 | .77 | 1.09 | 1.26 | 1.35 | 1.31 |
p < .05;
p < .01;
p < .001.
The 3‐Class Unconditional Model
The Growth Mixture Model contains different classes for determining the best trajectory classes. Table 2 provides the AIC, BIC, aBIC, entropy, LMR, BLRT for the 1‐, 2‐, 3‐, 4‐, 5‐, and 6‐class solutions. The AIC, BIC, and aBIC decreased from the 1‐ to the 4‐class. LMR (p < .01) and BLRT (p < .01) and the proportion of each class consistently indicated that the 3‐class was the optimum one. Although the classification accuracy of 2‐class (entropy = .86), 4‐class (entropy = .71), 5‐class (entropy = .73), and 6‐class (entropy = .69) were higher than the 3‐class (entropy = .64), according to the practical meaning of categories (no <5% of each class) (Nylund et al., 2007; Zhou, 2018), the class probabilities were more reasonable in the 3‐class.
TABLE 2.
Fit Indices for Unconditional 1‐ to 6‐class Growth Mixture Models (N = 812)
| GMM | K | AIC | BIC | aBIC | Entropy | LMR | BLRT | Proportion of each class |
|---|---|---|---|---|---|---|---|---|
| 1C | 8 | 7063.96 | 7101.56 | 7076.15 | 1.00 | |||
| 2C | 11 | 7032.59 | 7084.28 | 7049.35 | .86 | .03 | <.01 | .04/.96 |
| 3C | 14 | 7001.80 | 7067.59 | 7023.13 | .64 | .01 | <.01 | .06/.41/.53 |
| 4C | 17 | 6973.37 | 7053.26 | 6999.28 | .71 | .06 | <.01 | .02/.39/.08/.51 |
| 5C | 20 | 6959.59 | 7053.58 | 6990.07 | .73 | .01 | <.01 | .12/.47/.39/.00/.02 |
| 6C | 23 | 6959.24 | 7067.33 | 6994.29 | .69 | .39 | .67 | .11/.44/ .37/.06/.02/.00 |
The three trajectory classes of panic are presented in Figure 1. In Class 1, the trajectory started at the highest level and continued to decline. Thus, it was named the “Continuous Decline Group (CDG)”, consisting of 46 people and accounting for 5.67 per cent of the total. In Class 2, the trajectory started at the lowest level and remained stable. Therefore, it was named the “Continuous Low Group (CLG)”, consisting of 335 people, and accounting for 41.25 per cent of the total population. In Class 3, the trajectory started at a relatively high level and remained stable. Therefore, it was named the “Continuous High Group (CHG)”, consisting of 431 people and accounting for 53.08 per cent of the total population.
FIGURE 1.
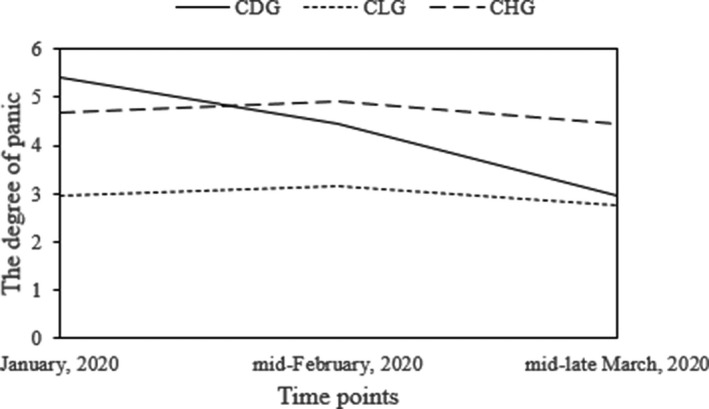
Trajectories of 3‐class models. Note: CDG is the “continuous decline group”, CLG is the “continuous low group”, and CHG is the “continuous high group”.
The 3‐Class Conditional Model
Time‐invariant covariates (gender, age, location, and income) and time‐varying covariates (social factors, family factors, and individual factors at T1) were included in the GMM. The classification accuracy of the GMM was improved from .64 to .72 after the addition of the covariates. Additionally, the AIC, BIC, and aBIC decreased from the 3‐class unconditional model to the 3‐class conditional model. There was also an impact on the number of people in each class. The probability of the CDG increased from 5.67 per cent (n = 46) to 6.41 per cent (n = 52), the CLG decreased from 41.25 per cent (n = 335) to 33.37 per cent (n = 271), and the CHG increased from 53.08 per cent (n = 431) to 60.22 per cent (n = 489).
Predictors in the Trajectory of Panic
According to R3STEP, there was no significant predictive effect of age, while gender, location, income, social factors, family factors, and individual factors significantly predicted the trajectory class of panic. As shown in Table 3, with reference to the CDG, people in the CHG were more vulnerable to social factors; people in the CLG were more likely to be men, be in Hubei Province during the pandemic, have a low income, and were more vulnerable to social factors and individual factors. With reference to the CLG, people in the CHG were more likely to be women, be outside of Hubei Province during the pandemic, and were more vulnerable to social factors, family factors, and individual factors.
TABLE 3.
Predictors in the Trajectory Class of Panic
| Predictors | CDG vs. CHG | CDG vs. CLG | CLG vs. CHG | |||
|---|---|---|---|---|---|---|
| B | p | B | p | B | p | |
| Gender | −.27 | .51 | −.86 | <.05 | .60 | <.01 |
| Place | −.40 | .13 | −.91 | <.01 | .52 | <.05 |
| Age | .03 | .26 | −.03 | .37 | .07 | .07 |
| Income | −.25 | .08 | −.46 | <.01 | .21 | .05 |
| Social factors | −1.26 | <.05 | −1.94 | <.01 | .68 | <.01 |
| Family factors | .14 | .49 | −.11 | .58 | .25 | <.01 |
| Individual factors | .03 | .97 | −2.05 | <.01 | 2.07 | <.01 |
DISCUSSION
The current study used the GMM to examine the trajectory of panic and its associated factors during the COVID‐19 pandemic in China. Three trajectory classes of panic were identified: the “Continuous Decline Group (CDG)”, the “Continuous Low Group (CLG)”, and the “Continuous High Group (CHG)” with an individual‐centered approach. The different classes of trajectory helped to extend previous findings of variable‐centered research (e.g. Craske, DeCola, Sachs, & Pontillo, 2003; Liu, 2019; Sun, 2006; Xie, Zheng, Xie, & Wang, 2005). It also showed that these three trajectory classes of panic were related to social factors, family factors, and individual factors as well as gender, income, and location.
Based on ecological systems theory, this study focused on social factors, family factors, and individual factors and discovered that all three levels significantly predicted profiles of people in the CHG. Previous studies revealed social factors, such as the characteristics of the emergency itself and the state of supplies and information, were associated with panic (Liu, 2019; Wang, 2009). Extending these findings, we found that people were more likely to belong to the CHG when they agreed that the predictive factors were the highly contagious virus, the big number of infections, the insufficient supply of medical materials, and a lot of negative information. At the family level, there was a high correlation between strained parent‐child relations and mental health problems in preceding studies (e.g. Bentley et al, 2016; Wang et al, 2019; Wu & Zhang, 2004). The present study also demonstrated that people with strained parent‐child relationships were more likely to belong to the CHG. As for individual factors, perception deviation was an assignable predictive factor of panic in a previous study (Xu et al., 2020). Our study confirmed similar results by finding that the perception deviation was a predictor of different trajectory classes of panic. Specifically, people with more perception deviation were more likely to belong to the CHG.
Besides the above three levels, the present study uncovered that individuals in the CHG were more likely to be women, be outside of Hubei Province during the pandemic with the CLG as the reference class. According to a previous study (Xie, Zheng, Xie, & Wang, 2005), women’s panic level was higher than men’s because women tended to be more sensitive than men. Thus, women’s panic level was more likely to be continuously higher than that of men. Moreover, people outside of Hubei province were more likely to belong to the CHG than people in Hubei province during the pandemic. This might be explained through the moderating effect of risk locus center, which refers to the phenomenon that people at the center of the high‐risk area would experience lower panic (Wiegman & Gutteling, 1995; Xie, Zheng, Xie, & Wang, 2005). People in Hubei Province had more direct experience of and identified information about the pandemic, which could alleviate their panic level.
Last but not the least, people in the CLG were more likely to have a lower income compared to people in the CDG. This is inconsistent with the research during the pandemic by Song and colleagues, who found that the impact of income on mental health was not significant (Song et al., 2020). According to the regional differences of income among Chinese residents, small towns usually have lower incomes (Yin & Wang, 2020). Thus, people with a lower income were more likely to be in the CLG probably because they were in a relatively familiar and safe environment, living a life of self‐sufficiency.
Nevertheless, there are some limitations that need to be addressed. First, with respect to uneven sampling, the number of women was significantly larger than that of men, and people in Hubei Province were significantly fewer than people outside of Hubei Province. Second, there were fewer items in the questionnaire due to the online survey limitations, which was not as comprehensive as a set of questionnaires. Further study should improve measurement for more accurate data. Finally, this study failed to explore the effect of the interaction between the predictive factors and the trajectory of panic. Future studies should improve measurements for more accurate data and expand the model to further examine the interactions between variables.
Implications
Despite these limitations, the current study extended the prior literature on panic during public health emergencies with a growth mixture model. Our findings emphasised the important role of social factors, family factors, and individual factors as well as demographic profiles including gender, income, and location in the different trajectory classes of panic. The resulting Growth Mixture Model indicated three levels of trajectories and identified multiple predictive factors. These results also highlighted the attention to women and individuals outside of Hubei province regarding their panic level as they were more identified with the CHG, providing implications for psychological intervention and public policy. Therefore, interventions and policies might work at three levels (social, family, and individual) with comprehensive consideration of multiple aspects (such as gender, income, and location). For instance, the government could improve the transparency of information and give economic subsidies to people with economic difficulties; family members could learn parent‐child communication skills to improve their relationships; individuals could modify unreasonable perceptions about the pandemic through scientific knowledge to alleviate panic. This study also provides a more specific group profiling regarding clinical practices on panic and public health emergencies, targeting women, people located outside the center of the pandemic, and people with higher income. Clinical practices should also focus on decreasing the negative effects of social factors, family factors, and individual factors to alleviate panic.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.
AUTHOR CONTRIBUTIONS
All authors have participated in the study and have read and approved the submitted version of the manuscript. Xiuyun Lin conceived the idea and acquired the fund, Yuxin Tan, hui Chen, Yongqiang Jiang, Ting He, Jinxiu Yin and Yingying Tang performed the experiment, Yuxin Tan analysed the data and wrote the manuscript, Xiuyun Lin and Dazhou Wu reviewed and edited the manuscript.
ETHICAL APPROVAL
Prior to conducting the study, the Institutional Review Board of Beijing Normal University in China approved the research protocol, including the consent procedure. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
INFORMED CONSENT
In the current study, participants were aged from 18 to 42 years old. Before the study, participants signed informed consent forms.
ACKNOWLEDGEMENTS
The study described in this report was funded by the National Key R&D Program of China, the COVID‐19 Prevention and Research Emergency Project of Beijing Normal University, and the COVID‐19 Mental Health Support Project of the Department of Psychology of Beijing Normal University. The content is solely the responsibility of the authors and does not necessarily represent the official views of Administration for Reacher and Development, Beijing Normal University. We are appreciative of the participants in our study and the many people who assisted in data collection.
REFERENCES
- Arafat, S.M. , Kar, S.K. , Marthoenis, M. , Sharma, P. , & Kabir, R. (2020). Psychological underpinning of panic buying during pandemic (COVID‐19). Psychiatry Research, 289, 1–2. 10.1016/j.psychres.2020.113061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentley, E. , Millman, Z.B. , Thompson, E. , Demro, C. , Kline, E. , Pitts, S.C. , & Schiffman, J. (2016). High‐risk diagnosis, social stress, and parent‐child relationships: A moderation model. Schizophrenia Research, 174(1–3), 65–70. 10.1016/j.schres.2016.04.014 [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner, U. (1977). Toward an experimental ecology of human development. American Psychologist, 32(7), 513–531. 10.1037/0003-066X.32.7.513 [DOI] [Google Scholar]
- Brooks, K.S. , Webster, R.K. , Smith, L.E. , Woodland, L. , & Rubin, G.J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet, 395(10227), 912–920. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassarino, M. , & Murphy, G. (2018). Reducing young drivers' crash risk: Are we there yet? An ecological systems‐based review of the last decade of research. Transportation Research Part F: Traffic Psychology and Behaviour, 56, 54–73. 10.1016/j.trf.2018.04.003 [DOI] [Google Scholar]
- Craske, M.G. , DeCola, J.P. , Sachs, A.D. , & Pontillo, D.C. (2003). Panic control treatment for agoraphobia. Journal of Anxiety Disorders, 17(3), 321–333. 10.1016/S0887-6185(02)00203-7 [DOI] [PubMed] [Google Scholar]
- Dias, J.C. (2007). Model selection criteria for model‐based clustering of categorical time series data: A Monte Carlo study. In Decker R. & Lenz H.J. (Eds.), Advances in data analysis: Studies in classification, data analysis, and knowledge organization (pp. 23–30). Berlin and Heidelberg: Springer. [Google Scholar]
- Feldman, B.J. , Masyn, K.E. , & Conger, R.D. (2009). New approaches to studying problem behaviors: A comparison of methods for modeling longitudinal, categorical adolescent drinking data. Developmental Psychology, 45(3), 652–676. 10.1037/a0014851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng, W. , Yao, J.J. , Li, S.M. , Wu, Y. , Zhou, D.X. , Zhang, Z.J. , & Yang, Q.P. (2018). Influencing factors and survey of mental health of community residents in Wuxi City. Journal of Public Health and Preventive Medicine, 29(6), 133–137. CNKI:SUN:FBYF.0.2018-06-035 [Google Scholar]
- Friesen, J.D. (2012). An ecological systems approach to family counselling. Canadian Counsellor, 17, 98–104. [Google Scholar]
- Fu, A.L. , Bo, L. , Yu, J. , Zhang, G.G. , & Liu, J.W. (2017). A mental health survey of different ethnic and occupational groups in Xinjiang, China. International Journal of Environmental Research & Public Health, 14(1), 46–57. 10.3390/ijerph14010046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomez, R. , Skilbeck, C. , Thomas, M. , & Slatyer, M. (2017). Growth mixture modeling of depression symptoms following traumatic brain injury. Frontiers in Psychology, 8, 1–14. 10.3389/Fpsyg.2017.01320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He, Z.X. (2019). Trajectory of bullying in preschool children: Prediction of peer relationship. Master's Degree, Ludong University. [Google Scholar]
- Kelley, H.H. , Condry, J.C. , Dahlke, A.E. , & Hill, A.H. (1965). Collective behavior in a simulated panic situation. Journal of Experimental Social Psychology, 1(1), 20–54. 10.1016/0022-1031(65)90035-1 [DOI] [Google Scholar]
- Li, B. (2015). Assessment on the mental health and its influencing factors among the retired elderly from the universities of Guangdong province. Journal of Public Health and Preventive Medicine, 26(3), 30–32. CNKI:SUN:FBYF.0.2015-03-009 [Google Scholar]
- Liao, F. , Li, D.U. , Zhao, J. , Yan, Y.R. , & Chen, H. (2003). Social psychology analysis of fear derived from severe acute respiratory syndrome. Academic Journal of Second Military Medical University, 24(6), 621–624. 10.1007/BF02838801 [DOI] [Google Scholar]
- Liu, S. , Yang, L.L. , Zhang, C.X. , Xiang, Y.T. , Liu, Z.C. , Hu, S.H. , & Zhang, B. (2020). Online mental health services in China during the COVID‐19 outbreak. The Lancet Psychiatry, 7(3), 228–229. 10.1016/S2215-0366(20)30077-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, Y. (2019). Study on the influence of group panic psychology on the unsafe evacuation behavior of subway passengers. Master’s Degree, Xi’an University of Science and Technology. [Google Scholar]
- Lo, Y.T. , Mendell, N.R. , & Rubin, D.B. (2001). Testing the number of components in a normal mixture. Biometrika, 88(3), 767–778. 10.1093/biomet/88.3.767 [DOI] [Google Scholar]
- McLachlan, G.J. , & Peel, D. (2000). Finite mixture model. New York: Wiley. [Google Scholar]
- Muthén, B. (2003). Statistical and substantive checking in growth mixture modeling: Comment on Bauer and Curran. Psychological Methods, 8(3), 369–377. 10.1037/1082-989X.8.3.369 [DOI] [PubMed] [Google Scholar]
- Muthén, B.O. , & Asparnuhov, T. (2008). Growth mixture modeling: Analysis with non‐Gaussian random effects. In Fitzmaurice G., Davidian M., Verbeke C., & Molenberghs C. (Eds.), Advances in longitudinal data analysis (pp. 143–165). Boca Raton, FL: Chapman & Hall/CRC Press. [Google Scholar]
- Muthén, B. , & Muthén, L.K. (2000). Integrating person‐centered and variable‐centered analyses: Growth mixture modeling with latent trajectory classes. Alcoholism: Clinical & Experimental Research, 24(6), 882–891. 10.1111/j.1530-0277.2000.tb02070.x [DOI] [PubMed] [Google Scholar]
- Nylund, K.L. , Asparoutiov, T. , & Muthen, B.O. (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling: A Multidisciplinary Journal, 14(4), 535–569. 10.1080/10705510701575396 [DOI] [Google Scholar]
- Okeyo, I.L.A. , & Dowse, R. (2018). An illustrated booklet for reinforcing community health worker knowledge of tuberculosis and facilitating patient counselling. African Journal of Primary Health Care & Family Medicine, 10(1), 1–7. 10.4102/Phcfm.V10i1.1687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petras, H. , & Masyn, K. (2010). General growth mixture analysis with antecedents and consequences of change. New York; Springer. [Google Scholar]
- Sim, K. , Chua, H.C. , Vieta, E. , & Fernandez, G. (2020). The anatomy of panic buying related to the current COVID‐19 pandemic. Psychiatry Research, 288. 10.1016/j.psychres.2020.113015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song, F.F. , Wand, X. , Ju, Z.Y. , Liu, A.X. , Liu, J.J. , & Wang, T. (2020). Mental health status and related influencing factors during the epidemic of coronavirus disease 2019(COVID–19). Journal of Public Health and Preventive Medicine, 31(2), 23–27. 10.3969/j.issn.1006-2483.2020.02.006 [DOI] [Google Scholar]
- Speier, C. , & Price, M.F. (1998). Using aggregated data under time pressure: A mechanism for coping with information overload. Paper presented at the Proceedings of the Thirty‐First Hawaii International. [Google Scholar]
- Sun, D.Y. (2006). A quantitative model about panic perception of the individual based on logit modeling and its empirical research. Management Review, 18(10), 48–53. 10.1631/jzus.2006.B0099 [DOI] [Google Scholar]
- Wang, F. , Lin, L. , Xu, M. , Li, L. , & Zhou, X. (2019). Mental health among left‐behind children in rural China in relation to parent‐child communication. International Journal of Environmental Research and Public Health, 16(10), 1855. 10.3390/ijerph16101855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, H. (2003). The cause of the group panic and its removal: Interpretation of group mentality from the spread of SARS. Journal of Beijing University of Posts and Telecommunications (Social Sciences Edition), 5(3), 1–4. 10.3969/j.issn.1008-7729.2003.03.001 [DOI] [Google Scholar]
- Wang, X.H. , & Lin, C. (2003). The psychological mechanism and self adjust of SARS panic. Academic Journal of PLA Postgraduate Medical School, 24(2), 173–174. 10.3969/j.issn.1005-1139.2003.03.005 [DOI] [Google Scholar]
- Wang, Y. (2009). Thoughts on the strategy of crisis communication based on the public psychology. Master's Degree, Hengyang Normal University. [Google Scholar]
- Wiegman, O. , & Gutteling, J.M. (1995). Risk appraisal and risk communication: Some empirical data from the Netherlands reviewed. Basic & Applied Social Psychology, 16(2), 227–249. 10.1080/01973533.1995.9646111 [DOI] [Google Scholar]
- Wu, K.J. (2006). Psychosocial panic in disaster. Contemporary Manager, 11(2006), 216–217. CNKI:SUN:DDJR.0.2006-11-115 [Google Scholar]
- Wu, N.Y. , & Zhang, D.Y. (2004). A study on the correlation between parent‐child relation and mental health level of teenagers. Psychological Science, 27(4), 812–816. https://www.cnki.net/kcms/doi/10.16719/j.cnki.1671‐6981.2004.04.011.html [Google Scholar]
- Wu, X.W. (2009). Research of panic in crisis based on time constraints. Master's Degree, Shanghai Jiao Tong University. [Google Scholar]
- Xie, X.F. , Zheng, R. , Xie, D.M. , & Wang, H. (2005). Analysis on psychological panic phenomenon of SARS. Acta Scicentiarum Naturalum Universitis Pekinesis, 41(4), 628–639. 10.13209/j.0479-8023.2005.082 [DOI] [Google Scholar]
- Xu, M.X. , Zheng, R. , Rao, L.L. , Kuang, Y. , Yang, S.W. , Ding, Y. , & Li, S. (2020). Proposals for coping with "Psychological typhoon eye" effect detected in COVID‐19. Bulletin of Chinese Academy of Sciences, 35(3), 273–282. 10.16418/j.issn.1000-3045.20200226001 [DOI] [Google Scholar]
- Yang, C. (2006). Evaluating latent class analyses in qualitative phenotype identification. Computational Statistics & Data Analysis, 50, 1090–1104. 10.1016/j.csda.2004.11.004 [DOI] [Google Scholar]
- Yin, X.B. , & Wang, Q. (2020). The study on financial development, urbanization and urban & rural residents' income gap in China. Economic Geography, 40(3), 84–91. 10.15957/j.cnki.jjdl.2020.03.010 [DOI] [Google Scholar]
- Yu, X. (2020). Strategies for overcoming panic during the COVID‐19 epidemic. Chinese Mental Health Journal, 34(3), 278–279. 10.3969/j.issn.1000-6729.2020.3.032 [DOI] [Google Scholar]
- Zhao, D.H. , Yao, F.F. , Wang, L.J. , Zheng, L. , Gao, Y.J. , Ye, J. , & Gao, R.B. (2020). A comparative study on the clinical features of COVID‐19 pneumonia to other pneumonias. Clinical Infectious Diseases, 71(15), 756–761. 10.1093/cid/ciaa247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou, Y.Y. (2018). Adolescent internet addiction: Longitudinal associations with adjustment outcomes and interpersonal factors. Master's Degree, Central China Normal University. [Google Scholar]


