Abstract
Tissue flossing aims to improve range of motion (ROM), reduce pain, and enhance injury prevention. However, evidence is lacking regarding its effects. Therefore, this study examined the effects of flossing on hamstring muscles function in comparison to dynamic stretching (DS). Seventeen healthy young men ([mean ± SD] age, 23.2 ± 1.1 years; height, 1.72 ± 0.08 m; body mass, 63.5 ± 9.3 kg) volunteered as subjects in this randomized crossover trial. The subjects received flossing, DS, and control interventions in random order at least 1 week apart to eliminate the influence of the previous intervention. Flossing involved passive twisting and active movement using a floss band (Sanctband COMPRE Floss Blueberry, Sanct Japan Co., Ltd.). DS was performed for 4 minutes in 30-second sets consisting of 15 repetitions of 2 seconds stretching. The following were measured before and after each intervention: straight leg raise (SLR) test, passive knee extension (KE) test, passive torque, passive stiffness, fascicle length in the biceps femoris long head as an indication of hamstring muscles flexibility, and maximal isometric knee flexion contraction, maximal eccentric knee extension/flexion contraction, rate of force development, and muscle activity. Flossing yielded significant improvements in the SLR test (mean difference in post-intervention changes between interventions: 5.4°, percentage change from pre- to post-value: 13.4%, p = 0.004), passive KE test (6.2°, 4.5%, p < 0.001), passive torque at end-ROM (3.8 Nm, 4.7%, p = 0.03), and maximal eccentric knee flexion contraction (14.9% body weight, 8.2%, p = 0.03) than control. Moreover, flossing yielded 2.1-fold greater improvements in the passive KE test (3.8°, 4.5%, p = 0.03) and yielded significant improvements in the maximal eccentric knee extension contraction (29.9% body weight, 13.8%, p = 0.02) than DS. Therefore, flossing on hamstring muscles is more beneficial than DS with respect to increasing ROM and muscle exertion.
Key points.
Effect of tissue flossing and dynamic stretching (DS) on hamstring muscles function was examined.
Flossing significantly increased straight leg raise, passive knee extension (KE), passive torque at end-range of motion (ROM), and maximal eccentric knee flexion contraction.
Flossing showed significantly higher increases than DS in passive KE test by 2.1 times and maximal eccentric knee extension contraction.
Flossing on hamstring muscles is more beneficial than DS with respect to increasing ROM and muscle exertion.
Key words: Floss band, Fascia, Compression, Range of motion, Flexibility, Injury prevention
Introduction
Tissue flossing is a new method that aims to improve range of motion (ROM), reduce pain, prevent injury, or enhance early return to competition in athletes. Tissue flossing involves passive twisting and active movement with a joint or muscle tightly wrapped by a floss band made from natural rubber, which is then removed within 2 minutes. This technique was popularized by the book written by Starrett and Cordoza (2013), who proposed that fascial shearing and occlusion of blood to the muscle are the mechanisms that underlie flossing. Furthermore, the compression and movement of flossing on a joint or muscle alter the relationship of the fascia with the neuromusculoskeletal system, which allows the fascia to stretch and move freely (Starrett and Cordoza, 2013). However, few reports support the alleged mechanisms that underlie the effectiveness of flossing.
Despite a lack of empirical evidence, tissue flossing is widely performed among athletes because of its subjective benefits on ROM and alleviating muscle pain. A previous study suggested that flossing on the ankle joint can increase dorsiflexion ROM and single-leg jump velocity in recreational athletes (Driller et al., 2017a; Driller and Overmayer, 2017b). In contrast, another crossover trial only indicated limited support for the use of tissue flossing to improve ankle ROM, countermovement jumping, and sprinting performance up to 30 minutes post-application in elite rugby union athletes (Mills et al., 2019). Therefore, although flossing might increase ankle ROM, few studies have reported its effectiveness on the ROM of joints or muscles other than the ankle joint.
Limited joint mobility and decreased muscle flexibility are common problems in clinical situations and athletic settings, and flexibility is important for both the prevention and rehabilitation of musculoskeletal injuries (Shadmehr et al., 2009). Lack of hamstring muscles flexibility might also result in major muscle imbalances, which predispose the individual to muscle injuries, patellar tendinopathy, patellofemoral pain, hamstring strain, and the development of low back pain (Heiderscheit et al., 2010; Lankhorst et al., 2013; Sadler et al., 2017; Van der Worp et al., 2011). Furthermore, soccer players with reduced hamstring muscles flexibility are more likely to develop hamstring injuries (Witvrouw et al., 2003). Therefore, to prevent hamstring strain, traditional stretching exercises such as static stretching, dynamic stretching (DS), ballistic stretching, or proprioceptive neuromuscular facilitation stretching is recommended prior to engaging in exercise or sports activities (Thacker et al., 2004). Several studies showed that DS improves ROM, muscle power, jump height, and sprint time (Mizuno, 2017; Perrier et al., 2011). DS has recently been recommended as a component of warm-up exercises prior to engaging in athletic activities (Behm et al., 2016; Perrier et al., 2011). Of note, the effectiveness of flossing on flexibility has not yet been compared with classical stretching methods. Therefore, in order to establish whether flossing is effective for injury prevention in athletes, it is crucial to examine its effects on hamstring muscles function. We hypothesized that flossing on the hamstring muscles would improve ROM and muscle exertion due to mechanical or sensory aspects.
Accordingly, this study examined the effects of flossing on hamstring muscles function in comparison with DS, which is commonly performed for injury prevention before exercise.
Methods
Subjects
Seventeen healthy young men ([mean ± SD] age, 23.2 ± 1.1 years; height, 1.72 ± 0.08 m; and body mass, 63.5 ± 9.3 kg) who were not involved in competitive sports or regular resistance, aerobic, or flexibility training volunteered to participate. Subjects who had latex allergy; hypertension (i.e., resting systolic blood pressure > 160 mmHg or diastolic blood pressure > 100 mmHg); venous thrombotic disease; heart disease; respiratory disease; or apparent neurological, orthopedic, dermatitis, or neuromuscular problems in their lower legs were excluded. All subjects were informed of the benefits and risks of the study and provided written informed consent before participation. The subject allowed to use his likeness in the Figures. This study was approved by our institutional ethics committee (no. 2019–013) and was conducted in accordance with the principles of the Declaration of Helsinki.
Study procedure and measurements
This study was a randomized crossover trial with three phases. Each subject performed three interventions—flossing, DS, and control—on three separate days, with a washout period of at least 1 week between interventions to eliminate the influence of the previous intervention. The subjects were randomized to a sequence of interventions based on a random table generated in Excel (2013, Microsoft, USA).
Flossing involved passive twisting and active knee flexion movement with the lower leg tightly wrapped with a floss band made from natural rubber (Sanctband COMPRE Floss Blueberry; 5.1 cm × 3.5 m; Sanct Japan Co., Ltd.). DS involved four 30-second sets of consisting of 15 repetitions of 2 seconds of stretching with 20 seconds of rest in between sets. The control involved only active knee flexion movement using the same method as that in the flossing intervention. All measurements were made before and after each intervention. All measurements and interventions were performed on the hamstring muscles of the dominant leg (i.e., the leg subjects used to kick a ball) for unilateral evaluation in order to ensure consistency in data collection among subjects (Hicks et al., 2016). All measurements were performed in an environment at room temperature of 24.9 ± 0.3°C and 62.8 ± 6.6% humidity.
Straight leg raise test
The passive straight leg raise (SLR) test was employed as an indication of hamstring muscles flexibility. The subject was placed in the supine position on an examination bed with the legs straight, and the non-tested leg was stabilized with inelastic straps to avoid compensatory movements. The subject was stabilized and instructed to remain relaxed and not offer any voluntary muscle contractions. Body markers were attached to the acromion, greater trochanter, and lateral epicondyle of the femur as well as the fibular malleolus of the dominant leg. The experimenter raised the subject’s leg, with the subject’s knee being passively extended, until the height where the subject felt a strong but tolerable stretch (i.e., slightly before the occurrence of pain) (Brusco et al., 2018). With the hip maximally flexed, the lower leg and foot were photographed from the same height and parallel to the non-tested leg of the subject. The hip flexion ROM in the obtained image was calculated using ImageJ (version 1.46r, NIH). This procedure was repeated three times, and the average of all three measurements was recorded.
Passive knee extension test
The passive knee extension (KE) test was employed as an indication of hamstring muscles flexibility (Hopper et al., 2005). The subject was placed in the supine position on an examination bed with both the hip and knee positioned in 90° of flexion, and the non-tested leg was stabilized with inelastic straps to avoid compensatory movements. Hip flexion was maintained by a stationary board on the distal thigh. The subject was stabilized and instructed to remain relaxed and to not offer any voluntary muscle contractions. Body markers were attached to the greater trochanter and lateral epicondyle of the femur as well as the fibular malleolus of the dominant leg. The experimenter extended the knee until maximal stretch within the tolerance of the hamstring muscles, with the ipsilateral hip remaining in 90° of flexion (Reurink et al., 2013). With the hip maximally flexed, the lower leg and foot were photographed from the same height and parallel to the non-tested leg of the subject. Hip flexion ROM was calculated from the obtained image by ImageJ. This procedure was repeated three times, and the average of all three measures was recorded.
Passive torque and stiffness
Passive torque was used as an index of flexibility of the hamstring muscle–tendon unit (Samukawa et al., 2011). The passive torque produced by the hamstring muscles during passive knee extension was measured by an isokinetic dynamometer (Cybex Norm, Medica Co., Ltd., Japan). The subject was seated on a seat with an attached isokinetic dynamometer and a wedge-shaped cushion inserted between their trunk and the backrest (Figure 1). The subject’s chest, pelvis, and right thigh were stabilized with inelastic straps. The knee joint was aligned with the axis of rotation of the isokinetic dynamometer, and the lever arm attachment was placed just proximal to the medial malleolus and stabilized with inelastic straps. Next, the knee was passively extended at an angular velocity of 5°/s starting from 110° of flexion to the angle of maximum knee extension just before the subjective onset of pain. Stretching at 5°/s was used, because reflexive muscle contraction does not occur at this velocity (Gajdosik et al., 1996). The subject was instructed to remain relaxed and to not voluntarily resist while the dynamometer extended their knee at 5°/s across three repetitions (Duhig et al., 2019).
Figure 1.
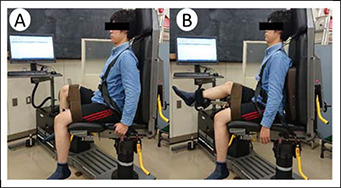
Passive torque test using an isokinetic dynamometer. (A) Starting position with both the hip and knee positioned in 110° of flexion. (B) The knee is passively extended at an angular velocity of 5°/s from 110° of knee flexion to the point of maximum knee extension just before the subjective onset of pain.
Passive knee flexion torque was analyzed at knee extension angles of –90° and –10°, and at end-ROM. Electromyography (EMG) was used to confirm that long head of the biceps femoris (BFlh) and semitendinosus (ST) did not contract during this passive knee extension. Skin preparation and electrode placement for the BFlh and ST followed the SENIAM guidelines (Hermens et al., 2000). Electrode position was carefully mapped using a transparent sheet to ensure the replication of positioning for post-intervention testing. The onset of muscle contraction was determined when the root mean square exceeded the sum of the mean and three standard deviations (SDs) for 200 ms when the muscle appeared to be relaxed just before the start of the passive torque test (Kang et al., 2012). Passive stiffness was calculated as the slope of the regression line (using the least-squares method) of the torque–angle relationship between 50% and 100% of the maximum knee extension angle (Kataura et al., 2017). The calculated knee extension angle range was defined as the angle from the 50% maximum knee extension angle to the pre-intervention maximum knee extension angle. The averages of the three values were recorded.
Fascicle length
The subject was placed in the prone position with the muscles in a relaxed state. Three longitudinal images of the muscle belly of the BFlh were obtained by B-mode ultrasonography (HI VISION Avius; Hitachi Aloka Medical Japan, Tokyo, Japan) using a high-resolution linear probe at 8.0 MHz (EUP-L65; Hitachi Aloka Medical Japan). The fascicle length of the BFlh was estimated using ImageJ, and the average of the three estimates was recorded. Fascicle length was determined as the length of the fascicle path between the superficial and deep aponeurosis. The outlined fascicle between the aponeuroses is presented in absolute terms (in mm). Because the fascicles were not entirely visible in the probe’s field of view, length was estimated using the following equation (Guilhem et al., 2011):
| Fascicle length = visible fascicle length + h / sin (pennation angle). |
where “visible fascicle length” is the length of fascicle visible in the sonographic image, h is the distance between the intersection point of the end of the visible fascicle and the edge of the image and the deep aponeurosis of the BFlh, and “pennation angle” is the angle between the fascicle and its superficial aponeurosis.
Maximal isometric voluntary contraction of knee flexion and rate of force development
Maximal isometric voluntary contraction (MIVC) of knee flexion was measured in the same position as that used to measure passive torque, with both the hip and knee positioned in 90° of flexion (Samukawa et al., 2011). MIVC was maintained for 3 seconds with the instruction, “as fast and hard as possible,” and measured twice with a 1-minute rest between the two measurements. The rate of force development (RFD) reflects the ability to rapidly increase muscle force after the onset of an explosive voluntary contraction (Rodríguez-Rosell et al., 2018). The RFD was determined as the slope of the torque–time curve over time intervals of 0–50, 0–100, 0–150, and 0–200 ms relative to the onset of muscle contraction during the MIVC test. The onset of muscle contraction was defined as the time when the moment curve exceeded the baseline moment by 2.5% of the MIVC (Aagaard et al., 2002). The sampling rate for torque measurement was 1000 Hz. The average of the two MIVC or RFD values was recorded.
Maximal eccentric voluntary knee extension/flexion contraction
Maximal eccentric voluntary knee extension/flexion contraction was measured in the same position as that used to measure MIVC. The subject was instructed to maximally resist the isokinetic action of the dynamometer that forcibly moved the knee joint from 10° to 90° of flexion and then in reverse from 90° to 10° of flexion (Figure 1). Maximal eccentric voluntary knee extension/flexion contraction was calculated according to the peak moment obtained between 10° and 90° knee flexion angles (0° indicates full knee extension). The subject received strong verbal encouragement to generate maximal force. The subject performed two maximal eccentric voluntary knee extension/flexion contractions at an angular velocity of 60°/s with a 1-minute rest between the two contractions. The average of the two values was recorded.
Muscle activity
Muscle activity was measured simultaneously with MIVC and maximal eccentric voluntary knee flexion contraction by an electromyographic apparatus (Free-EMG1000, BTS Bioengineering, Italy). Surface electrodes (SEN-12969, SparkFun Electronics, USA) were placed over the belly of the BFlh and ST of the dominant leg (20 mm inter-electrode distance). The original low EMG signals processed using a band-pass filter at 20–500 Hz were amplified and collected at a sampling rate of 2000 Hz. The average EMG activity for 2 seconds within the middle 3 seconds of the maximum voluntary contraction was calculated according to the root mean square (RMS), and full-wave rectification was performed using a RMS smoothing algorithm with a window interval of 50 ms. The average of the two values was recorded.
Intervention condition
Flossing was performed with a floss band in accordance with the following procedure; the experimenter was instructed by a person with an “Easy Flossing Instructor Course Levels 1–6” certification. First, the subject placed their dominant leg forward in the standing position. Then, the floss band was wrapped but not tightly around the area just above the distal third between the anterior superior iliac spine (ASIS) and patella as an anchor. When the band was stretched to 1.5 times its natural length with maintained tension, the experimenter wrapped the thigh distally to proximally with 50% overlap of the previous part of the band (Figure 2).
Figure 2.
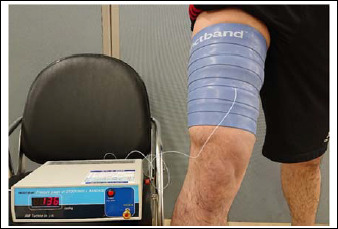
Placement of the floss band on the hamstring muscles. A contact pressure probe is placed on the anterior aspect of the thigh on the midpoint between the anterior superior iliac spine and patella.
Next, the subject performed passive twisting of the wrapped part of the leg four times and active knee flexion 20 times. The band was subsequently removed. This process was performed within 2 minutes, followed by a 2-minute break, and repeated once more. The interface pressure between the skin and floss band was measured to assess the level of compression (in mmHg) achieved by the wrapping technique. A probe of a contact pressure-measuring device (AMI-3037–SB–SET AMI Techno Co., Ltd., Japan) was placed on the anterior aspect of the thigh on the midpoint between the ASIS and patella.
For the DS intervention, the subject stood in the upright position and placed their dominant hand on the wall while placing their non-dominant hand on the ASIS of the dominant leg to fix the trunk and pelvis. The subject was instructed to actively flex their hip joints while maintaining the knees in extension once every 2 seconds such that their dominant hamstring muscles was stretched (Figure 3). The subject slowly practiced the motion five times and then performed 15 repetitions as quickly and powerfully as possible without bouncing and in synchrony with the rhythm of a digital metronome set to 30 beats/min (Yamaguchi and Ishii, 2005). The frequency or cadence of DS, which was maintained by a metronome, was approximately 1 second for hip flexion and 1 second for the return to the starting point (i.e., hip extension). This exercise emphasized achieving the greatest possible ROM and not the highest angular velocity. DS was performed for 4 minutes in 30-second sets consisting of 15 repetitions of 2 seconds stretching with a 30-second rest period between sets. The subject was instructed to avoid over-stretching with momentum and to hold their trunk upright.
Figure 3.
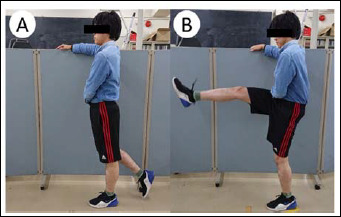
Dynamic stretching procedure for hamstring muscles. (A) The subject stands in the upright position, places their dominant hand on the wall, and places their non-dominant hand on the anterior superior iliac spine the dominant leg to fix the trunk and pelvis. (B) The subject is then instructed to actively flex their hip joints while maintaining the knees in extension once every 2 seconds such that their dominant hamstring muscles is stretched.
In the control condition, the subject only performed the active knee flexion exercise used in the flossing condition (without the band) 20 times, followed by a 2-minute break and another 20 repetitions.
Statistical analyses
The sample size was calculated using G*Power (version 3.1.9.2; University of Kiel, Kiel, Germany) to estimate the sample size required for this study (Faul et al., 2007).
Using a two-tailed test of significance with a 0.05 two-sided significance level, to achieve a power of 80%, it was estimated that a total of 17 subjects per group were required.
To examine the pre-intervention differences among the intervention conditions, one-way, repeated-measures analysis of variance (ANOVA) or the Friedman test was performed. The differences of measurements post-interventions were assessed by analysis of covariance (ANCOVA), with the pre-intervention values as a covariates. The Bonferroni post hoc test was performed if significance was detected. Effect size was calculated for each test using the Cohen’s d statistic. In addition, an effect size of 0.00–0.19 was considered as trivial, 0.20–0.49 as small, 0.50–0.79 as medium, and > 0.80 as large (Cohen, 1988). All statistical analyses were performed using SPSS version 26 (IBM, Japan). The level of statistical significance for all analyses was set at p < 0.05.
Results
The demographic characteristics of the study subjects are shown in Table 1. All subjects were male and determined to be right-leg dominant. No subjects dropped out or were excluded from the study. The pre- and post-intervention values are shown in Table 2. There were significant main effects of the interventions on passive torque at –50°, –40°, and –30° pre-intervention (p = 0.02, 0.03, and 0.03, respectively). The mean ± SD pressure applied during flossing was 134.1 ± 10.2 mmHg. The subjects reported no adverse or musculoskeletal events due to flossing or DS. The EMG activities of the BFlh and ST during passive torque were < 2% of maximum voluntary contraction, which confirmed the absence of any contribution of the contractile component to passive torque.
Table 1.
Demographic characteristics (N = 17). Data are means ± SD (range).
| Age (years) | 23.2 ± 1.1 (21.0-25.0) |
| Height (m) | 1.72 ± 0.08 (1.56-1.81) |
| Weight (kg) | 63.5 ± 9.3 (51.0-83.0) |
| BMI (kg/m²) | 21.5 ± 2.2 (18.7-27.7) |
| Leg length (cm) | 41.8 ± 2.3 (37.5-45.3) |
| Thigh length (cm) | 45.2 ± 11.7 (32.3-46.2) |
| Leg length (cm) | 87.1 ± 4.7 (76.7-93.2) |
| Thigh circumference (cm) | 52.2 ± 6.0 (45.1-66.1) |
SD: standard deviation; BMI: body mass index
Table 2.
Pre- and post-intervention values. Values are presented as mean ± SD.
| Variable | Pre-value | Post-value | ||||
|---|---|---|---|---|---|---|
| Flossing | DS | Control | Flossing | DS | Control | |
| SLR test (°) | 66.6 ± 13.6 | 67.1 ± 12.9 | 70.0 ± 17.2 | 75.5 ± 12.9 | 72.7 ± 13.8 | 73.1 ± 14.3 |
| Passive KE test (°) | 155.5 ± 8.7 | 154.1 ± 10.9 | 155.4 ± 11.2 | 162.5 ± 8.6 | 157.4 ± 10.2 | 156.1 ± 11.9 |
| Passive torque (Nm) | ||||||
| at -90 ° | 1.6 ± 1.0 | 0.9 ± 0.5 | 1.1 ± 0.9 | 0.9 ± 0.9 | 0.9 ± 0.8 | 0.9 ± 0.9 |
| at -80 ° | 3.4 ± 1.1 | 2.3 ± 1.1 | 2.8 ± 1.2 | 2.7 ± 1.0 | 2.2 ± 1.5 | 2.5 ± 0.9 |
| at -70 ° | 5.3 ± 1.3 | 4.2 ± 1.4 | 4.5 ± 1.4 | 4.4 ± 1.1 | 3.9 ± 1.6 | 4.2 ± 1.0 |
| at -60 ° | 7.2 ± 1.8 | 5.9 ± 1.7 | 6.1 ± 1.7 | 6.1 ± 1.4 | 5.7 ± 2.1 | 5.8 ± 1.2 |
| at -50 ° | 9.2 ± 2.5 | 7.5 ± 1.9 | 7.8 ± 1.9 | 7.7 ± 1.6 | 7.5 ± 2.6 | 7.4 ± 1.6 |
| at -40 ° | 11.4 ± 3.4 | 9.5 ± 2.3 | 9.6 ± 2.4 | 9.5 ± 2.0 | 9.2 ± 3.0 | 9.1 ± 2.1 |
| at -30 ° | 14.0 ± 4.6 | 11.5 ± 2.9 | 11.7 ± 3.1 | 11.5 ± 2.5 | 11.2 ± 3.6 | 11.1 ± 2.5 |
| at -20 ° | 17.8 ± 6.2 | 14.1 ± 3.3 | 14.6 ± 4.0 | 14.6 ± 3.2 | 13.8 ± 4.3 | 13.8 ± 3.3 |
| at -10 ° | 23.3 ± 8.5 | 18.4 ± 4.2 | 19.0 ± 5.3 | 19.4 ± 4.4 | 17.6 ± 5.4 | 18.0 ± 4.5 |
| at end-ROM ° | 30.8 ± 7.1 | 27.7 ± 5.2 | 28.6 ± 7.3 | 32.3 ± 7.3 | 26.9 ± 5.5 | 27.0 ± 7.1 |
| Passive stiffness (Nm/°) | 0.4 ± 0.2 | 0.3 ± 0.1 | 0.3 ± 0.1 | 0.3 ± 0.1 | 0.3 ± 0.1 | 0.3 ± 0.1 |
| Fascicle length (mm) | 49.9 ± 20.7 | 54.2 ± 13.7 | 63.3 ± 23.1 | 51.8 ± 18.7 | 57.6 ± 18.8 | 58.3 ± 20.5 |
| Maximal isometric knee flexion (%BW) | 63.8 ± 22.3 | 67.6 ± 17.5 | 64.5 ± 17.4 | 66.3 ± 21.4 | 68.1 ± 17.7 | 59.9 ± 16.0 |
| RFD (Nm/kg/s) | ||||||
| 0-50 msec | 2.8 ± 1.2 | 2.7 ± 1.2 | 2.7 ± 1.1 | 2.7 ± 1.4 | 2.5 ± 1.2 | 2.4 ± 0.9 |
| 0-100 msec | 3.0 ± 1.1 | 2.9 ± 1.0 | 2.8 ± 0.9 | 2.8 ± 1.2 | 2.7 ± 0.9 | 2.5 ± 0.8 |
| 0-150 msec | 2.7 ± 1.0 | 2.6 ± 0.8 | 2.5 ± 0.8 | 2.6 ± 0.9 | 2.5 ± 0.8 | 2.2 ± 0.7 |
| 0-200 msec | 2.3 ± 0.8 | 2.3 ± 0.7 | 2.2 ± 0.7 | 2.3 ± 0.8 | 2.2 ± 0.7 | 1.9 ± 0.6 |
| Maximal eccentric knee extension (%BW) | 200.8 ± 54.1 | 197.3 ± 58.4 | 200.5 ± 44.1 | 228.6 ± 55.6 | 195.7 ± 55.3 | 206.7 ± 45.2 |
| Maximal eccentric knee flexion (%BW) | 114.8 ± 28.4 | 116.3 ± 26.9 | 112.2 ± 26.6 | 124.3 ± 32.0 | 116.8 ± 25.9 | 107.6 ± 27.6 |
| Muscle activity (mv) | ||||||
| BFlh in isometric contraction | 0.2 ± 0.1 | 0.3 ± 0.1 | 0.3 ± 0.1 | 0.2 ± 0.1 | 0.3 ± 0.1 | 0.2 ± 0.1 |
| ST in isometric contraction | 0.4 ± 0.1 | 0.4 ± 0.2 | 0.4 ± 0.1 | 0.4 ± 0.2 | 0.4 ± 0.2 | 0.4 ± 0.2 |
| BFlh in eccentric contraction | 0.3 ± 0.2 | 0.3 ± 0.2 | 0.3 ± 0.1 | 0.3 ± 0.2 | 0.3 ± 0.2 | 0.3 ± 0.1 |
| ST in eccentric contraction | 0.4 ± 0.2 | 0.4 ± 0.2 | 0.4 ± 0.1 | 0.4 ± 0.2 | 0.4 ± 0.3 | 0.4 ± 0.1 |
DS: dynamic stretching; SLR: straight leg raise; KE: knee extension; ROM: range of motion; BW: body weight; RFD: rate of force development; BFlh: long head of biceps femoris; ST: semitendinosus.
The post-intervention changes among the three interventions are shown in Table 3. There was a significant main effect of the interventions on the SLR test (F = 5.77, p = 0.01), the passive KE test (F = 10.4, p < 0.01), passive torque at end-ROM (F = 4.05, p = 0.02), and maximal eccentric voluntary knee extension/flexion contraction (F = 4.38, p = 0.02 and F = 3.71, p = 0.03, respectively). The changes in the passive KE test results and maximal eccentric voluntary knee extension contraction were significantly greater after flossing than after DS (d = 0.54 and 0.59, respectively; all p < 0.05). Furthermore, the changes in the SLR and passive KE test results as well as passive torque at end-ROM and maximal eccentric voluntary knee flexion contraction were significantly higher after flossing than the control (d = 0.18, 0.61, 0.73, and 0.56, respectively; all p < 0.05). However, there were no significant differences post-intervention between DS and the control (p > 0.05).
Table 3.
Differences in post-intervention changes between interventions.
| Variable | Between-intervention differences # (95% simultaneous CI) † | Main effect | ||||||
|---|---|---|---|---|---|---|---|---|
| Flossing vs DS | ES | Flossing vs Control | ES | DS vs Control | ES | F-value | P-value | |
| SLR test (°) | 3.2 (-0.8 to 7.2) | 0.21 | 5.4 (1.4 to 9.4)* | 0.18 | 2.3 (-1.7 to 6.3) | 0.02 | 5.77 | 0.01 |
| Passive KE test (°) | 3.8 (0.3 to 7.2)* | 0.54 | 6.2 (2.8 to 9.7)* | 0.61 | 2.5 (-1.0 to 5.9) | 0.11 | 10.40 | < 0.01 |
| Passive torque (Nm) | ||||||||
| at -90 ° | -0.4 (-1.0 to 0.3) | 0.03 | -0.2 (-0.9 to 0.4) | 0.03 | 0.2 (-0.5 to 0.8) | 0.00 | 0.97 | 0.39 |
| at -80 ° | -0.1 (-1.0 to 0.7) | 0.42 | -0.1 (-0.9 to 0.7) | 0.29 | 0.0 (-0.8 to 0.8) | 0.02 | 0.07 | 0.93 |
| at -70 ° | -0.2 (-1.1 to 0.7) | 0.31 | -0.2 (-1.1 to 0.6) | 0.20 | 0.0 (-0.9 to 0.8) | 0.16 | 0.30 | 0.75 |
| at -60 ° | -0.5 (-1.5 to 0.5) | 0.21 | -0.4 (-1.4 to 0.6) | 0.19 | 0.1 (-0.9 to 1.0) | 0.07 | 0.82 | 0.45 |
| at -50 ° | -0.8 (-2.1 to 0.4) | 0.10 | -0.6 (-1.9 to 0.6) | 0.18 | 0.2 (-1.0 to 1.4) | 0.03 | 1.48 | 0.24 |
| at -40 ° | -1.0 (-2.4 to 0.5) | 0.10 | -0.8 (-2.2 to 0.7) | 0.19 | 0.2 (-1.2 to 1.6) | 0.05 | 1.42 | 0.25 |
| at -30 ° | -1.2 (-2.9 to 0.6) | 0.09 | -0.9 (-2.7 to 0.8) | 0.15 | 0.2 (-1.5 to 1.9) | 0.07 | 1.50 | 0.23 |
| at -20 ° | -1.2 (-3.5 to 1.2) | 0.22 | -0.9 (-3.2 to 1.4) | 0.25 | 0.3 (-2.0 to 2.5) | 0.01 | 0.83 | 0.44 |
| at -10 ° | -0.8 (-3.9 to 2.3) | 0.37 | -0.8 (-3.9 to 2.3) | 0.33 | 0.0 (-3.0 to 2.9) | 0.07 | 0.27 | 0.76 |
| at end-ROM ° | 3.1 (-0.4 to 6.6) | 0.84 | 3.8 (0.3 to 7.2)* | 0.73 | 0.6 (-2.8 to 4.1) | 0.02 | 4.05 | 0.02 |
| Passive stiffness (Nm/°) | 0.0 (-0.6 to 0.1) | 0.48 | 0.0 (-0.1 to 0.1) | 0.36 | 0.0 (-0.0 to 0.1) | 0.13 | 0.04 | 0.96 |
| Fascicle length (mm) | -5.1(-11.4 to 21.6) | 0.31 | -4.4 (-12.7 to 21.5) | 0.33 | 0.7(-17.5 to 16.0) | 0.04 | 0.34 | 0.72 |
| Maximal isometric knee flexion (%BW) | 1.2 (-8.7 to 11.1) | 0.09 | 7.0 (-2.9 to 16.9) | 0.34 | 5.8(-4.1 to 15.7) | 0.49 | 1.77 | 0.18 |
| RFD (Nm/kg/s) | ||||||||
| 0-50 msec | 0.1 (-0.5 to 0.8) | 0.17 | 0.3 (-0.4 to 0.9) | 0.26 | 0.1 (-0.6 to 0.8) | 0.10 | 0.44 | 0.65 |
| 0-100 msec | 0.1 (-0.4 to 0.6) | 0.18 | 0.2 (-0.3 to 0.8) | 0.36 | 0.1 (-0.4 to 0.6) | 0.20 | 0.72 | 0.49 |
| 0-150 msec | 0.0 (-0.4 to 0.5) | 0.13 | 0.2 (-0.2 to 0.7) | 0.43 | 0.2 (-0.3 to 0.7) | 0.33 | 0.96 | 0.39 |
| 0-200 msec | 0.1 (-0.3 to 0.5) | 0.16 | 0.2 (-0.1 to 0.6) | 0.47 | 0.2 (-0.2 to 0.6) | 0.34 | 1.29 | 0.29 |
| Maximal eccentric knee extension (%BW) | 29.9 (4.0 to 55.8)* | 0.59 | 21.6 (-4.3 to 47.4) | 0.43 | -8.4 (-34.2 to 17.5) | 0.22 | 4.38 | 0.02 |
| Maximal eccentric knee flexion (%BW) | 9.4 (-4.4 to 23.1) | 0.26 | 14.9 (1.2 to 28.6)* | 0.56 | 5.5 (-8.2 to 19.3) | 0.34 | 3.71 | 0.03 |
| Muscle activity (mv) | ||||||||
| BFlh in isometric contraction | 0.0 (-0.0 to 0.1) | 0.11 | 0.0 (-0.0 to 0.1) | 0.03 | 0.0 (-0.0 to 0.1) | 0.17 | 1.05 | 0.36 |
| ST in isometric contraction | -0.0 (-0.1 to 0.1) | 0.16 | 0.0 (-0.1 to 0.1) | 0.44 | 0.0 (-0.1 to 0.1) | 0.27 | 0.14 | 0.87 |
| BFlh in eccentric contraction | -0.0 (-0.1 to 0.0) | 0.09 | -0.0 (-0.1 to 0.0) | 0.19 | 0.0 (-0.0 to 0.1) | 0.08 | 0.16 | 0.86 |
| ST in eccentric contraction | -0.0 (-0.1 to 0.1) | 0.09 | 0.0 (-0.1 to 0.1) | 0.24 | 0.0 (-0.1 to 0.1) | 0.09 | 0.70 | 0.50 |
* P < 0.05. CI: confidence interval; DS: dynamic stretching; ES: effect size using the Cohen’s d; SLR: straight leg raise; KE: knee extension; ROM: range of motion; BW: body weight; RFD: rate of force development; BFlh: long head of biceps femoris; ST: semitendinosus.
# Mean differences in post-intervention changes between-intervention;
† Pre-intervention values were included as covariates. Mean differences in post-intervention changes between-intervention.
Discussion
The present study examined the effects of flossing on hamstring muscles function in comparison with DS. The results showed that compared to the control, flossing resulted significantly greater increases in the SLR and passive KE test results as well as passive torque at end-ROM and maximal eccentric knee flexion contraction. In addition, compared to DS, flossing resulted in a 2.1-fold greater increase in passive KE test results and an increase in maximal eccentric knee extension contraction. Therefore, flossing of the hamstring muscles is more beneficial than DS with respect to increasing ROM and muscle exertion.
The findings of this study revealed that flossing of the hamstring muscles significantly enhanced SLR, passive KE test, passive torque at end-ROM, and maximal eccentric knee flexion contraction. A previous study reported that flossing of the ankle joint increased acute dorsiflexion ROM and single-leg jump performance (Driller and Overmayer, 2017b). Furthermore, another study reported that flossing of the gastrocnemius muscle increased acute dorsiflexion ROM (Kaneda et al., 2020). Although the band was wound on a different body part in the previous study, the effect of the increased ROM is consistent with the results of this study.
The precise physiological mechanism(s) underlying flossing has not yet been determined. Previous studies suggested that increases in muscle extensibility might be due to mechanical or sensory aspects (Weppler and Magnusson, 2010); sensory aspects include the modification of sensation, which is associated with pain threshold. In addition, Starrett and Cordoza (2013) proposed that the effects of flossing on muscle exertion and flexibility might include fascial shearing and obstruction of blood to the muscle. The fascia consist of multiple fibrous layers and collagenous connective tissues that surround and interpenetrate the skeletal muscle, joints, organs, nerves, and vascular beds (Stecco et al., 2013; Stecco and Schleip, 2016). The smooth sliding between the layers of fluid fascia allows muscles to contract or elongate (Klingler et al., 2014). Furthermore, fascia change from a solid gel-like state to a fluid solution-like state in accordance with a decrease in fascial viscoelasticity when energy in the form of heat or mechanical pressure (i.e., thixotropy) is applied (Cheatham et al., 2015). A floss band provides intense mechanical pressure on the muscles, covering the limb from all directions owing to close skin contact. Muscle compression retains heat associated with the increase in intramuscular pressure and the resultant muscle contraction under compression, which can produce heat, potentially decreasing fascial viscoelasticity (Agostinucci, 2010). Therefore, heat or mechanical pressure caused by flossing might allow muscles to easily elongate by decreasing fascial viscoelasticity. In addition, the present results showing that flossing improved SLR and passive KE test results as well as passive torque at end-ROM suggest that flossing increases stretch tolerance. Stretch tolerance, which is associated with pain threshold, is reported to increase with the augmentation of ROM and passive torque at end-ROM after DS (Iwata et al., 2019). Therefore, the effect of flossing might be similar to those of DS, which increases ROM by improving stretch tolerance. Transmission of the force caused by skin stretching might activate subcutaneous mechanoreceptors and modulate pain perception (Chen et al., 2018). Thus, skin stretching caused by the tension of flossing might activate subcutaneous mechanoreceptors and increase stretch tolerance. Furthermore, compression is likely to activate both cutaneous and muscle mechanoreceptors, which could modulate sensory feedback transmission and improve muscle power output (McNair and Heine, 1999). When muscle temperature increases due to increased blood circulation, the activation of metabolic activity and decreased fascial viscoelasticity might result in smoother contraction and an increased muscle contraction rate (Yamashita et al., 1992). The key difference between flossing and DS is that the former involves target muscle contraction under compression, while the latter involves antagonist muscle contraction of the target muscle (Samukawa et al., 2011). The improvement in joint ROM after DS might be involved stretch tolerance or reciprocity suppression rather than reduced stiffness of the muscle–tendon unit (Mizuno, 2017; Samukawa et al., 2011). Thus, the increased ROM without a decrease in passive torque due to DS in this study might suggest that DS affects neuromuscular factors. Hence, the findings of this study provide insights into the mechanisms underlying the effect of flossing.
The major clinical implication of the present study is that flossing of the hamstring muscles before exercise might be effective for preventing injury and increasing physical performance. Hamstring strain injuries are an important issue in modern sports and associated with various factors such as decreased muscle flexibility, maximal eccentric knee flexion contraction weakness, muscle fatigue, and a history hamstring strain injuries (Buckthorpe et al., 2019). Considering this and the present findings showing that flossing increased the flexibility of the hamstring muscles and maximal eccentric knee flexion contraction, flossing of the hamstring muscles might help prevent hamstring strain injuries in sports. Furthermore, patellar tendonitis occurs most frequently in sports requiring repeated jumping. The triggering factors for patellar tendonitis are thought to be the overuse of the patellar tendon, and conditions such as decreased flexibility of the lower limbs, eccentric knee extension contraction weakness, and landing after jumping (Rosen et al., 2015; Van der Worp et al., 2011). Eccentric knee extension training is reported to significantly reduce tendon pain and improve function in athletes with chronic painful patellar tendonitis (Jonsson and Alfredson, 2005). Therefore, flossing of the hamstring muscles might be more effective for preventing patellar tendonitis in sports than DS.
This study has several limitations. First, the subjects were healthy, young, adult men, whereas flossing is typically used by athletes (Driller and Overmayer, 2017b). Athletes have high muscle thickness and physical functioning, and women have lower stiffness and hysteresis of tendon structures than men (Kubo et al., 2003). Therefore, flossing might yield different physical functioning outcomes in athletes or women. Second, this study did not measure physiological parameters of the mechanisms of flossing, including fascial viscoelasticity and shearing (Starrett and Cordoza, 2013). Third, this study did not measure the long-term effects of flossing and physical performance; instead, it focused on examining the acute effects of flossing on hamstring muscles function. The long-term effects of flossing on joints and muscles other than the ankle are unclear. Therefore, further studies are required to examine the long-term effects of flossing, its effects on physical performance, and the physiological mechanisms of flossing (e.g., fascial viscoelasticity and neural factors) in athletes including women.
Conclusion
This study revealed that flossing of the hamstring muscles significantly increased SLR and passive KE test results, passive torque at end-ROM, and maximal eccentric knee flexion contraction. In addition, compared to DS, flossing resulted in 2.1-fold greater improvements in passive KE test results and an increase in maximal eccentric knee extension contraction, respectively. Flossing of the hamstring muscles is more beneficial than DS with respect to increasing ROM and muscle exertion and, therefore, may lead to prevent injuries.
Acknowledgements
We thank the subjects and the study team for their participation in this study. The authors have no conflicts of interests to declare. The experiments comply with the current laws of the country in which they were performed.
Biographies
Hiroaki KANEDA
Employment
Sensory and Motor Control, Graduate School of Medical Sciences, Kitasato University, Sagamihara, Kanagawa, Japan
Degree
MSc
Research interests
Sports science, injury prevention, compression
E-mail: ap14316@st.kitasato-u.ac.jp

Naonobu TAKAHIRA
Employment
Dean, Kitasato University Graduate School of Medical Sciences. Professor, Department of Orthopaedic Surgery of Clinical Medicine, and Rehabilitation Sciences and Functional Restoration Science of Sensory and Motor Control.
Professor, Physical Therapy Course, Department of Rehabilitation, School of Allied Health Sciences, Kitasato University, Sagamihara, Kanagawa, Japan.
Kitasato University Hospital, Department of Orthopaedic Surgery.
Degree
MD, PhD
Research interests
Sports science, sports injuries, musculoskeletal disorders, orthopaedics, hip joint disease
E-mail: takahira@med.kitasato-u.ac.jp

Kouji TSUDA
Employment
Sensory and Motor Control, Graduate School of Medical Sciences, Kitasato University, Sagamihara, Kanagawa, Japan
Degree
PhD
Research interests
Exercise therapy, public health, venus thromboprophylaxis
E-mail: mm14024a@st.kitasato-u.ac.jp
Kiyoshi TOZAKI
Employment
Sensory and Motor Control, Graduate School of Medical Sciences, Kitasato University, Sagamihara, Kanagawa, Japan
Degree
MSc
Research interests
Sedentary behavior, posture,ergonomics
E-mail: ap12327@st.kitasato-u.ac.jp

Sho KUDO
Employment
Sensory and Motor Control, Graduate School of Medical Sciences, Kitasato University, Sagamihara, Kanagawa, Japan
Degree
M.S. in Physical Therapy
Research interests
Posture, exercise science, biomechanics
E-mail: ap14319@st.kitasato-u.ac.jp

Yoshiki TAKAHASHI
Employment
Sensory and Motor Control, Graduate School of Medical Sciences, Kitasato University, Sagamihara, Kanagawa, Japan
Degree
M.S. in Physical Therapy
Research interests
Sports science, injury prevention, evaluation for physical performance
E-mail: ap14328@st.kitasato-u.ac.jp
Shuichi SASAKI
Employment
Department of Rehabilitation, Kitasato University Hospital, Sagamihara, Kanagawa, Japan
Degree
PhD
Research interests
Shoulder training, sport medicine, hand orthosis
E-mail: sasakiki0821@gmail.com

Tomonori KENMOKU
Employment
Department of Orthopaedic Surgery, School of Medicine, Kitasato University, Sagamihara, Kanagawa, Japan
Degree
MD, PhD
Research interests
Sports medicine, musculoskeletal pain, motion analysis
E-mail: pseudolefty811@yahoo.co.jp
References
- Aagaard P., Simonsen E.B., Andersen J.L., Magnusson P., Dyhre-Poulsen P. (2002) Increased rate of force development and neural drive of human skeletal muscle following resistance training. Journal of Applied Physiology 93, 1318-1326. [DOI] [PubMed] [Google Scholar]
- Agostinucci J. (2010) Inhibitory effects of circumferential pressure on flexor carpi radialis H-reflex in adults with neurological deficits. Perceptual and Motor Skills 110, 89-103. [DOI] [PubMed] [Google Scholar]
- Behm D.G., Blazevich A.J., Kay A.D., McHugh M. (2016) Acute effects of muscle stretching on physical performance, range of motion, and injury incidence in healthy active individuals: a systematic review. Applied Physiology, Nutrition, and Metabolism 41, 1-11. [DOI] [PubMed] [Google Scholar]
- Buckthorpe M., Wright S., Bruce-Low S., Nanni G., Sturdy T., Gross A.S., Bowen L., Styles B., Villa S.D., Davison M., Gimpel M. (2019) Recommendations for hamstring injury prevention in elite football: translating research into practice. British Journal of Sports Medicine 53, 449-456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brusco C.M., Blazevich A.J., Radaelli R., Botton C.E., Cadore E.L., Baroni B.M., Trajano G.S., Pinto R.S. (2018) The effects of flexibility training on exercise-induced muscle damage in young men with limited hamstrings flexibility. Scandinavian Journal of Medicine & Science in Sports 28, 1671-1680. [DOI] [PubMed] [Google Scholar]
- Cheatham S.W., Kolber M.J., Cain M., Lee M. (2015) The effects of self-myofascial using a foam roll or roller massage on join range ofmotion, muscle recovery, and performance: a systematic review. International Journal of Sports Physical Therapy 10, 827-838. [PMC free article] [PubMed] [Google Scholar]
- Chen S.M., Lo S.K., Cook J. (2018) The effect of rigid taping with tension on mechanical displacement of the skin and change in pain perception. Journal of Science and Medicine in Sport 21, 342-346. [DOI] [PubMed] [Google Scholar]
- Cohen J. (1988) Statistical power analysis for the behavioral sciences. 2nd edition In. Hillsdale, New Jersey, United States of America: Lawrence Erlbaum Associates. [Google Scholar]
- Driller M., Mackay K., Mills B., Tavares F. (2017a) Tissue flossing on ankle range of motion, jump and sprint performance: A follow-up study. Physical Therapy in Sport 28, 29-33. [DOI] [PubMed] [Google Scholar]
- Driller M.W., Overmayer R.G. (2017b) The effects of tissue flossing on ankle range of motion and jump performance. Physical Therapy in Sport 25, 20-24. [DOI] [PubMed] [Google Scholar]
- Duhig S.J., Bourne M.N., Buhmann R.L., Williams M.D., Minett G.M., Roberts L.A., Timmins R.G., Sims C.K.E., Shield A.J. (2019) Effect of concentric and eccentric hamstring training on sprint recovery, strength and muscle architecture in inexperienced athletes. Journal of Science and Medicine in Sport 22, 769-774. [DOI] [PubMed] [Google Scholar]
- Faul F., Erdfelder E., Lang A.G., Buchner A. (2007) G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods 39, 175-191. [DOI] [PubMed] [Google Scholar]
- Gajdosik R.L., Vander Linden D.W., Williams A.K. (1996) Influence of age on concentric isokinetic torque and passive extensibility variables of the calf muscles of women. European Journal of Applied Physiology and Occupational Physiology 74, 279-286. [DOI] [PubMed] [Google Scholar]
- Guilhem G., Cornu C., Guével A. (2011) Muscle architecture and EMG activity changes during isotonic and isokinetic eccentric exercises. European Journal of Applied Physiology 111, 2723-2733. [DOI] [PubMed] [Google Scholar]
- Heiderscheit B.C., Sherry M.A., Silder A., Chumanov E.S., Thelen D.G. (2010) Hamstring strain injuries: recommendations for diagnosis, rehabilitation, and injury prevention. The Journal of Orthopaedic and Sports Physical Therapy 40, 67-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hermens H.J., Freriks B., Disselhorst-Klug C., Rau G. (2000) Development of recommendations for SEMG sensors and sensor placement procedures. Journal of Electromyography and Kinesiology 10, 361-374. [DOI] [PubMed] [Google Scholar]
- Hicks K.M., Onambélé G.L., Winwood K., Morse C.I. (2016) Muscle damage following maximal eccentric knee extensions in males and females. Plos One 11, e0150848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopper D., Conneely M., Chromiak F., Canini E., Berggren J., Briffa K. (2005) Evaluation of the effect of two massage techniques on hamstring muscle length in competitive female hockey players. Physical Therapy in Sport 6, 137-145. [Google Scholar]
- Iwata M., Yamamoto A., Matsuo S., Hatano G., Miyazaki M., Fukaya T., Fujiwara M., Asai Y., Suzuki S. (2019) Dynamic stretching has sustained effects on range of motion and passive stiffness of the hamstring muscles. Journal of Sports Science and Medicine 18, 13-20. [PMC free article] [PubMed] [Google Scholar]
- Jonsson P., Alfredson H. (2005) Superior results with eccentric compared to concentric quadriceps training in patients withjumper’s knee: a prospective randomised study. British Journal of Sports Medicine 39, 847-850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaneda H., Takahira N., Tuda K., Tozaki K., Sakai K., Kudo S., Takahashi Y., Sasaki S., Fukushima K., Kenmoku T. (2020) The effects of tissue flossing and static stretching on gastrocnemius exertion and flexibility. Isokinetics and Exercise Science 28, 205-213. [Google Scholar]
- Kang SY., Jeon HS., Kwon O., Cynn H.S., Choi B. (2012) Activation of the gluteus maximus and hamstring muscles during prone hip extension with knee flexion in three hip abduction positions. Manual Therapy 18, 303-307. [DOI] [PubMed] [Google Scholar]
- Kataura S., Suzuki S., Matsuo S., Hatano G., Iwata M., Yokoi K., Tsuchida W., Banno Y., Asai Y. (2017) Acute effects of the different intensity of static stretching on flexibility and isometric muscle force. Journalof Strength and Conditioning Research 31, 3403-3410. [DOI] [PubMed] [Google Scholar]
- Klingler W., Velders M., Hoppe K., Pedro M., Schleip R. (2014) Clinical relevance of fascial tissue and dysfunctions. Current Pain and Headache Reports 18, 439. [DOI] [PubMed] [Google Scholar]
- Kubo K., Kanehisa H., Fukunaga T. (2003) Gender differences in the viscoelastic properties of tendon structures. European journal of applied physiology 88, 520–526. [DOI] [PubMed] [Google Scholar]
- Lankhorst N.E., Bierma-Zeinstra S.M., van Middelkoop M. (2013) Factors associated with patellofemoral pain syndrome: a systematic review. British Journal of Sports Medicine 47, 193-206. [DOI] [PubMed] [Google Scholar]
- McNair P.J., Heine P.J. (1999) Trunk proprioception: enhancement through lumbar bracing. Archives of Physical Medicine and Rehabilitation 80, 96-99. [DOI] [PubMed] [Google Scholar]
- Mills B., Mayo B., Tavares F., Driller M. (2019) The effect of tissue flossing on ankle range of motion, jump and sprint performancein elite rugby union athletes. Journal of Sport Rehabilitation 12, 1-5. [DOI] [PubMed] [Google Scholar]
- Mizuno T. (2017) Changes in joint range of motion and muscle-tendon unit stiffness after varying amounts of dynamic stretching. Journal of Sports Sciences 35, 2157-2163. [DOI] [PubMed] [Google Scholar]
- Perrier E.T., Pavol M.J., Hoffman M.A. (2011) The acute effects of a warm-up including static or dynamic stretching on countermovement jump height, reaction time, and flexibility. Journal of Strength and Conditioning Research 25, 1925-1931. [DOI] [PubMed] [Google Scholar]
- Reurink G., Goudswaard G.J., Oomen H.G., Moen M.H., Tol J.L., Verhaar J.N.V., Weir A. (2013) Reliability of the active and passive knee extension test in acute hamstring injuries. The American Journal of Sports Medicine 41, 1757-1761. [DOI] [PubMed] [Google Scholar]
- Rodríguez-Rosell D., Pareja-Blanco F., Aagaard P., González-Badillo J.J. (2018) Physiological and methodological aspects of rate of force development assessment in human skeletal muscle. Clinical Physiology and Functional Imaging 38, 743-762. [DOI] [PubMed] [Google Scholar]
- Rosen A.B., Ko J., Simpson K.J., Kim S.H., Brown C.N. (2015) Lower extremity kinematics during a drop jump in individuals with patellar tendinopathy. Orthopaedic Journal of Sports Medicine 3, 2325967115576100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadler S.G., Spink M.J., Ho A., De Jonge X.J., Chuter V.H. (2017) Restriction in lateral bending range of motion, lumbar lordosis, and hamstring flexibility predicts the development of low back pain: a systematic review of prospective cohort studies. BMC Musculoskeletal Disorders 18, 179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samukawa M., Hattori M., Sugama N., Takeda N. (2011) The effects of dynamic stretching on plantar flexor muscle-tendon tissue properties. Manual Therapy 16, 618-622. [DOI] [PubMed] [Google Scholar]
- Shadmehr A., Hadian M.R., Naiemi S.S., Jalaie S. (2009) Hamstring flexibility in young women following passive stretch and muscle energy technique. Journal of Back and Musculoskeletal Rehabilitation 22, 143-148. [DOI] [PubMed] [Google Scholar]
- Stecco C., Schleip R. (2016) A fascia and thefascial system. Journal of Bodywork and Movement Therapies 20, 139-140. [DOI] [PubMed] [Google Scholar]
- Stecco A., Gesi M., Stecco C., Stern R. (2013) Fascial components of the myofascial pain syndrome. Current Pain and Headache Reports. 17, 352. [DOI] [PubMed] [Google Scholar]
- Starrett K., Cordoza G. (2013) Becoming a Supple Leopard 2nd Edition: The Ultimate Guide to Resolving Pain, Preventing Injury, and Optimizing Athletic Performance. Las Vegas, NV: Victory Belt Publishing. [Google Scholar]
- Thacker S.B., Gilchrist J., Stroup D.F., Kimsey C.D., Jr. (2004) The impact of stretching on sports injury risk: a systematic review of the literature. Medicine and Science in Sports and Exercise 36, 371-378. [DOI] [PubMed] [Google Scholar]
- Van der Worp H., Van Ark M., Roerink S., Pepping G.J., van den Akker-Scheek I., Zwerver J. (2011) Risk factors for patellar tendinopathy: a systematic review of the literature. British Journal of Sports Medicine 45, 446-452. [DOI] [PubMed] [Google Scholar]
- Weppler C.H., Magnusson S.P. (2010) Increasing muscle extensibility: a matter of increasing length or modifying sensation? Physical Therapy 90, 438-449. [DOI] [PubMed] [Google Scholar]
- Witvrouw E., Danneels L., Asselman P., D’Have T., Cambier D. (2003) Muscle flexibility as a risk factor for developing muscle injuries in male professional soccer players. A prospective study. The American Journal of Sports Medicine 31, 41-46. [DOI] [PubMed] [Google Scholar]
- Yamaguchi T., Ishii K. (2005) Effects of static stretching for 30 seconds and dynamic stretching on leg extension power. Journal of Strength and Conditioning Research 19, 677-683. [DOI] [PubMed] [Google Scholar]
- Yamashita T., Ishii S., Oota I. (1992) Effect of muscle stretching on the activity of neuromuscular transmission. Medicine and Science in Sports and Exercise 24, 80-84. [PubMed] [Google Scholar]


