Abstract
On April 2, 2020, we received a maternal transport from a local city hospital of a pregnant woman (38 weeks and 0 days of gestation) in her 20s, who had the 2019 novel coronavirus disease (COVID‐19). We performed an emergency cesarean section with spinal anesthesia because of an abnormal fetal heart rate pattern. A healthy 3106‐g male baby was delivered. All the severe acute respiratory syndrome coronavirus 2 polymerase chain reaction tests of nasal and oral discharges, anal swabs and blood samples of the neonate at 9 h, 30 h and 4 days after birth were negative. Because the mother was diagnosed as having COVID‐19 pneumonia, the neonate was given formula milk. The mother's nasal discharge samples at 20 and 21 days were negative. The mother first held her baby in her arms on the 22nd day after birth, and they were discharged on the following day. To the best of our knowledge, this is the first report in Japan of a delivery of a baby from a woman infected with COVID‐19.
Keywords: 2019 novel coronavirus disease, severe acute respiratory syndrome coronavirus 2, infection transmission, pregnancy, cesarean section
Introduction
In December 2019, a novel coronavirus was first reported in Wuhan, in the Hubei province of China. 1 The first case of the novel coronavirus disease 2019 (COVID‐19) in Japan was reported mid‐January 2020, and the number of infected people ran up to approximately 2000 by April 1. Since then, data regarding the COVID‐19 have rapidly accumulated, now on a daily worldwide basis, increasing our understanding of this disease, including pregnancy‐related outcomes. 2 , 3 , 4 , 5 However, the optimal management protocol of pregnancies complicated by maternal COVID‐19 has not yet been established. There are worldwide, country‐to‐country variations in each country's perinatal healthcare system due to cultural, religious and socioeconomic reasons. In Japan, real‐time reverse transcriptase‐polymerase chain reaction (RT‐PCR) tests for COVID‐19 are handled through local public health centers. The necessary preconditions for these tests are severe malaise, breathing difficulty and/or continuous high fever. Under these circumstances, we, at our tertiary center of obstetric and perinatal medicine in Sagamihara City, Kanagawa Prefecture, adjacent to the southern border of the Tokyo Metropolitan area, experienced the first delivery in Japan of a baby from a woman complicated with COVID‐19.
Case Report
On the night of April 1, the Center for Perinatal, Pediatric and Developmental Medicine, Kitasato University Hospital was requested to accept a maternal transport from a local city hospital of a pregnant woman (37 weeks and 6 days of gestation) in her 20s, who had tested positive for severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2). The patient had had a past history of an uncomplicated vaginal delivery in her early 20s. The current pregnancy had been uneventful until she experienced a watery discharge on March 30 and was admitted to a local hospital, at which time her body temperature was 38.1°C. A diagnosis of premature rupture of the membranes was confirmed. Obstetric examinations revealed a cephalic presentation of a normally grown fetus with a reassuring fetal heart rate (FHR) pattern. The cervical os was 2.5‐cm open with 30% effacement. Antibiotic therapy was initiated on suspicion of intrauterine infection. The following day, March 31, the maternal body temperature was 38.9°C, so labor was induced with oxytocin. At that stage, the delivery ward staff members had no idea of the possibility of the mother being positive for COVID‐19 in this case. The labor progress was slow and the patient complained of an increase in nasal discharge and dysgeusia. Although a chest X‐ray did not provide any suspicious findings, COVID‐19 was suspected, so a nasopharyngeal mucous specimen was obtained and sent to pathology for a real‐time RT‐PCR test of SARS‐CoV‐2. From that point on, full protection for all of the delivery ward staff members against COVID‐19 was initiated.
On the third day, April 1, the maternal body temperature remained high (38.9°C), and the SARS‐CoV‐2 RT‐PCR test result via the local public health center came back positive. Because many delivery ward staff members were categorized as close contacts, the hospital directors decided to discontinue the delivery and transfer the patient to another hospital. Before the actual transport, we performed a meticulous simulation in our hospital to ensure a safe patient transport and a vaginal or cesarean delivery in a negative pressure operating room. Upon admission to Kitasato University Hospital in the early morning of April 2, the patient's condition was stable (body temperature, 37.8°C; blood pressure, 128/60 mmHg; and oxygen saturation [SpO2], 98%), although the FHR patterns (nearly 200 bpm at baseline with markedly decreased FHR variability and intermittent mild variable decelerations) indicated a non‐reassuring fetal condition.
We decided to perform an emergency cesarean section with spinal anesthesia because of her chest X‐ray showing very mild pneumonia (Fig. 1a). All staff members in operation rooms wore full personal protective equipment (PPE) with N95 masks and surgeons put on double gloves. Two hours after the admission, a cesarean section was performed, and a 3106‐g male baby was delivered with Apgar scores of 8 at both 1 and 5 min. The umbilical artery blood pH was 7.32. After the cesarean, the mother's SpO2 was maintained above 96% with oxygen supplementation for 28 h. Her postoperative course was uneventful.
Figure 1.
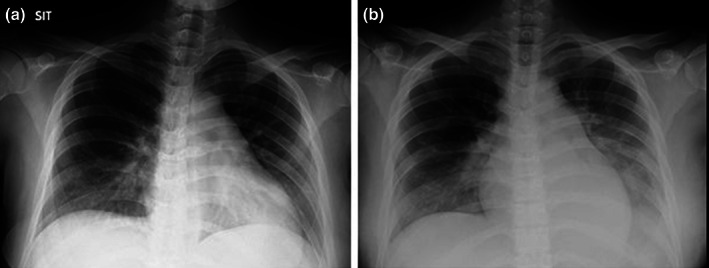
Chest X‐rays. (a) Preoperation. (b) The first day after surgery: Ground‐glass opacity was observed in the lower lungs.
The neonate was quarantined and isolated away from the mother. The baby boy was in and remained in stable condition. All the SARS‐CoV‐2 PCR tests of nasopharyngeal, oral and anal swabs and blood sampled at 9 h, 30 h and 4 days after birth were negative. The mother had complained of breathing difficulty upon physical movement, and chest computed tomographic scans 36 h after the surgery demonstrated ground‐glass opacity and a crazy‐paving appearance with consolidation in the bilateral lungs (Fig. 2). Therefore, we diagnosed her as having COVID‐19 pneumonia. Although our original plan was to give the baby the mother's expressed breast milk, because of the maternal intermittent fever beginning 3 days after the surgery, most likely due to COVID‐19, the neonate was given formula milk for nutrition. The mother was treated with a combination of the human immunodeficiency virus protease inhibitors lopinavir/ritonavir from 5 days after the surgery. The PCR test results of the mother's breast milk samples 4 and 8 days after the C‐section and those of her nasopharyngeal mucous samples at 20 and 21 days were all negative. The mother hugged her baby for the first time on the 22nd day after birth, and they were discharged on the following day. No nosocomial infection of COVID‐19 was detected among our hospital staff up to the present time.
Figure 2.
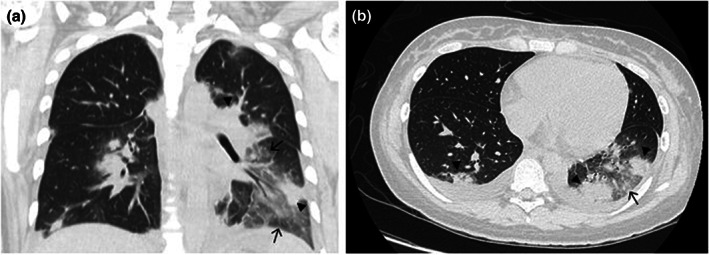
Chest computed tomographic scans 36 h after surgery. Ground‐glass opacity and a crazy‐paving appearance (arrows) with consolidation (arrow heads) in the bilateral lungs. (a) Frontal plane. (b) Transverse plane.
According to the report from the local public health center, most of the patient's household members, including her husband and her daughter, were found to be positive for COVID‐19. Her adult sister, one of the positive household members, had been living in France and just returned to Japan, the first week of March 2020, and was currently living with the family.
Discussion
To the best of our knowledge, this is the first report in Japan of a delivery of a baby from a woman infected with COVID‐19. This year, the spread of COVID‐19 infection here in Japan accelerated exponentially from the beginning of April. There were 2103 and 7509 real‐time PCR test‐confirmed positive cases, with 57 (3%) and 109 (1%) deaths on April 1 and 14, respectively. However, to date, the experience with COVID‐19 patients in pregnancy remains limited.
In the present case, to avoid the potential risk of vertical transmission, the newborn was resuscitated on a radiant warmer 2 m proximal to the operation table of the mother, was not breastfed, and not allowed contact with mother. Considering that all six samples of the mothers' breastmilk tested for SARS‐CoV‐2 were negative, according to Chen et al. 3 hygienically pumped breastmilk may safely be fed to neonates born from mothers with confirmed COVID‐19 infection. Chen et al. 3 also tested the amniotic fluid, cord blood and neonatal throat swab samples at the time of their C‐sections to determine the possibility of intrauterine fetal infection. That the results of all of those samples were negative suggests that no intrauterine fetal infections occurred as a result of COVID‐19 infection during the late stage of pregnancy. Studies on the delivery modality, of whether COVID‐19 could be transmitted during vaginal delivery, are currently not available.
To prevent nosocomial infection, pregnant women with suspected or confirmed COVID‐19 infection and their babies should be isolated in a designated area. Healthcare workers need to wear PPE (masks, gowns, gloves and goggles) at all times when performing medical procedures. Because personal cell phones cannot be taken into the units or operation rooms, the medical staff members should know the plans and how to communicate before entering the units. It is also important to put buck‐up members outside the units. Critical conditions, requiring emergency responses, must be avoided.
In Japan, there are approximately 1000 private clinics providing delivery service for 45% of the approximately 864,000 births per year. In these clinics, teams, usually consisting of an average of 1.5 obstetricians and 4.8 midwives, perform deliveries on a 24‐h basis. Furthermore, there are only 1 to 2 OB/GYNs working in 17% of the approximately 1200 hospitals that provide delivery services in Japan. 6 Those facilities mainly manage low‐risk pregnancies with basic infection control capabilities. Parturient women are then to be transported from those facilities to regional secondary or tertiary perinatal centers for perinatal care when the need arises. 7 Therefore, at private clinics, it is now important to develop an improved transport system for women with perinatal complications, simultaneously with suspected or confirmed COVID‐19 infection to select a proper medical facility.
The successful clinical course of this case may be used as an example pattern of a COVID‐19 complicated pregnancy as we are currently handling them in the Japanese obstetric healthcare system. The procedures in this case report are meant to be informative to medical professionals in not only the Japanese obstetric healthcare system but also in such systems worldwide.
Disclosure
None declared.
References
- 1. WHO . Novel Coronavirus – China. Geneva, Switzerland: WHO, 2020. Available from URL: (https://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/). [Google Scholar]
- 2. Zaigham M, Andersson O. Maternal and perinatal outcomes with COVID‐19: a systematic review of 108 pregnancies. Acta. Obstet. Gynecol. Scand 2020; 99 (7): 823–829. 10.1111/aogs.13867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chen H, Guo J, Wang C et al. Clinical characteristics and intrauterine vertical transmission potential of COVID‐19 infection in nine pregnant women: a retrospective review of medical records. Lancet 2020; 395: 809–815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zhu H, Wang L, Fang C et al. Clinical analysis of 10 neonates born to mothers with 2019‐nCoV pneumonia. Transl Pediatr 2020; 9 (1): 51–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zeng L, Xia S, Yuan W et al. Neonatal Early‐Onset Infection With SARS‐CoV‐2 in 33 Neonates Born to Mothers With COVID‐19 in Wuhan, China. JAMA Pediatrics 2020; 174 (7): 722–725. 10.1001/jamapediatrics.2020.0878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Japanese Association of Obstetricians and Gynecologists . The survey report for the workload of obstetricians in Japan. December 2019. (in Japanese).
- 7. Unno N. The Perinatal Care System in Japan. JMAJ 2011; 54: 234–240. [Google Scholar]


