Abstract
The study examined two angles of childbirth anxieties of Jewish and Arab pregnant women in Israel during the COVID‐19 pandemic (March‐April, 2020). Specifically, we examined the contribution of personal resources: self‐compassion and perceived social support, as well as a couple of COVID‐19‐related fears of being infected and concern for the foetus, to both the woman's global fear of childbirth (FOC) and her COVID‐19‐related childbirth anxiety. Participants were Jewish and Arab pregnant women (n = 403) aged 20–47, who completed a set of structured self‐report questionnaires from 18 March to 9 April 2020. Findings indicated that Arab women reported higher level of COVID‐19‐related childbirth anxiety and COVID‐19‐related fears of being infected and concern for the foetus. In addition, poorer health, being an Arab woman, being in the third trimester, lower self‐compassion, and higher COVID‐19‐related fears contributed significantly to greater COVID‐19‐related childbirth anxiety. Furthermore, poorer health, being primiparous, at‐risk pregnancy, lower self‐compassion and higher fear of being infected contributed significantly to greater FOC. Importantly, social support was found to moderate the association between self‐compassion and FOC. The results highlight the need to be attentive to pregnant women in times of crisis, and in particular to especially vulnerable subgroups, such as cultural minorities. They also highlight the importance of personal resources that may be applied in targeted interventions to reduce distress in vulnerable populations.
Keywords: anxiety, childbirth, COVID‐19, pregnancy, self‐compassion, social support
What is known about this topic
Fear of childbirth has consequences for women's mental health in the perinatal period.
It is related to women's resources and to cultural nuances.
Self‐compassion and social support are considered as efficient coping tools.
What this paper adds
The impact of COVID‐19 on vulnerable populations such as pregnant women must be considered.
Arab women reported higher levels of both COVID‐19‐related anxieties and a global fear of childbirth then Jewish women.
Self‐compassion and social support were associated with a lower level of both COVID‐19‐related childbirth anxiety and global fear of childbirth. A stronger sense of social support adds to pregnant women's ability to use self‐compassion as a protective shield against fear of the approaching delivery.
1. INTRODUCTION
December, 2019 will go down in history as the start of the COVID‐19 outbreak, which as of today (August 16, 2020) resulted in 21,617,587 infections and 768,995 deaths. In Israel, a country with a population of around 9 million, as of today, there are 92,233 confirmed cases of the virus and 674 people have died. At the time of data collecting and writing of the current study (April 10, 2020), 1,689,000 individuals were infected and 102,000 people have died worldwide as a result of the pandemic. In Israel, which at that time was after a month of lockdown, there were 10,500 confirmed cases of the virus and 95 people have died.
The pandemic has dramatically affected the lives of millions of people around the globe, shutting down businesses, air travel, and public services, and literally quarantining people in their homes for weeks. The crisis is accompanied by overwhelming uncertainty regarding countless aspects of both the near and more distant future. Findings from previous epidemics and pandemics show that an epidemic can have significant psychological consequences for people and lead, among other mental consequences, to depression and general and/or specific anxieties (Taylor, 2019). Accordingly, empirical evidence is being gathered about the implications of COVID‐19 on people's general psychological distress and mental health problems (e.g., Gao et al., 2020; Gómez‐Salgado et al., 2020; Wang et al., 2020), and specifically on depression and anxiety (Ahorsu et al., 2020; Choi et al., 2020; Huang & Zhao, 2020).
One of these is the effect on women who are currently pregnant and due to give birth in the coming months (Taubman – Ben‐Ari et al., 2020). Not only are they plagued by virus specific fears, such as the fear of being infected and concern for the welfare of the foetus, but at a time when hospitals and community clinics are appealing to people to stay away and communicate remotely with their physicians, these women will, sooner or later, have to go to the hospital to deliver their baby. This will require not only leaving home and being in a public place, thereby increasing the chance of infection, but it will also involve a stay in hospital, where people with COVID‐19 are being treated. Moreover, the women will be largely on their own, as they are allowed to bring only one person with them and visitors are prohibited. Thus, the usual fear of childbirth (FOC) is now combined with childbirth anxiety related specifically to the pandemic.
Literature on the FOC reveals that it is observed in all pregnant women, whether nulliparous, primiparous or multiparous, and may have consequences for their health, as well as for the labour, delivery and postpartum period (Nilsson et al., 2018). Several factors have been found to contribute to FOC, including women's internal resources (e.g., poor mental health, anxiety disorders, previous trauma) and external resources (e.g., lack of social support, unemployment, economic problems; Dencker et al., 2019). Studies also indicate cultural differences, such as different beliefs about childbirth, or women's ability to disclose their fears (e.g., Rondung et al., 2016; Soltani et al., 2017).
Dencker et al. (2019) contend that FOC is used as a general label for many types of anxieties relating to women's experience of pregnancy, childbirth and their outcomes, and call on researchers to differentiate between them, and to identify factors that may reduce, and not only increase, women's fears. In this study we sought to examine the global FOC during the current crisis, as well as specific COVID‐19‐related childbirth anxiety, investigating factors that might be associated with these two forms of anxiety, including sociodemographic characteristics, the personal resources of self‐compassion and social support, and the COVID‐19‐related fears of being infected and concern for the welfare of the foetus.
Although several sociodemographic factors have been found to be associated with FOC, some, including age, level of education, ethnicity and migration, have yielded contradictory results (Dencker et al., 2019). For example, certain studies indicate that lower age and education are associated with greater FOC, whereas others report opposite findings (e.g., Laursen et al., 2008; Poikkeus et al., 2006; Räisänen et al., 2014; Ternstrom et al., 2015).
Personal resources have also been investigated in this context. One factor that has gained interest recently is self‐compassion (Neff, 2003, 2011). Self‐compassion consists of three elements: self‐kindness, or being warm and understanding towards ourselves; common humanity, that is, recognising that suffering and personal inadequacy are part of the shared human experience and that as human beings we are vulnerable and imperfect; and mindfulness, being open and receptive to our thoughts and feelings, rather than being judgmental or trying to suppress them, even when they are negative. Findings indicate that self‐compassion helps to cope more adaptively in the face of stress and crisis (Chishima et al., 2018; Zeller et al., 2015), contributes to a low level of psychopathology (MacBeth & Gumley, 2012) in general, and is associated with lower levels of depression and anxiety in women during the perinatal period in particular (Felder et al., 2016; Fourianalistyawati et al., 2018).
Another pertinent personal resource is social support as perceived by the pregnant woman. Perceived social support, which reflects individuals' belief that they are loved, valued, and are a part of a social network of mutual ties and commitment (Stewart et al., 2014), has systematically been found to assist in coping with stressful situations (Gariepy et al., 2016; Zhen et al., 2018). Moreover, it has been shown to shield from distress during pregnancy (Asselmann et al., 2016; Pires et al., 2014), and there is consistent evidence that lack of social support increases the risk of FOC (e.g., Laursen et al., 2008; Lukasse et al., 2014).
While self‐compassion is a person's supportive and sympathetic caring for themselves, perceived social support is the feeling that others around them provide them with the same sort of caring, sympathy and warmth. Indeed, studies report a positive relationship between these variables, so that higher self‐compassion is associated with higher perceived support (Maheux & Price, 2016; Wilson et al., 2020). Although findings indicate a positive association between increased self‐compassion and reduced distress and PTSD symptoms, the precise mechanism or pathway through which self‐compassion increases positive outcomes or creates this protective effect is yet unknown (Winders et al., 2020). In view of the association between social support and self‐compassion, in the present study we sought to examine the possibility that social support may moderate the relationship between self‐compassion and FOC. In other words, we were interested in learning not only whether each of these resources is relevant to FOC in and of itself, but also if there is a dependency between them.
A pregnant woman's fears and anxieties may have detrimental effects on both maternal and foetal well‐being (Ng et al., 2004). Empirical evidence suggests that prenatal stress is related to higher rates of adverse birth outcomes, such as preterm delivery, low birth weight (e.g., Dayan et al., 2002; Mulder et al., 2002; Tomfohr‐Madsen et al., 2019) and a high rate of Cesarean birth (Yedid Sion et al., 2016). Likewise, these outcomes may adversely affect the foetus and may have long‐term negative consequences for its health throughout its life (Barker, 1998). In addition, as noted above, beyond the regular high levels of stress inherent in every pregnancy (Dunkel Schetter & Tanner, 2012; Guardino & Dunkel Schetter, 2014), the uncertainty and threatening information regarding the current COVID‐19 pandemic and its implications put additional burdens on a woman due to give birth in the near future.
In addition, Israel is a multicultural country with a Jewish majority and a relatively large Arab minority (21% of the population). Previous studies show that Arab women in Israel assess their health as poorer (Elnekave & Gross, 2004), and report higher distress during the perinatal period (Glasser et al., 2012; Shwartz et al., 2019). Furthermore, it was found that Arab women reported a higher level of traumatic birth experience, higher of fear and concern for their own safety and health, as well as that of the foetus during childbirth, compared to Jewish women (Halperin et al., 2014).
Moreover, studies comparing the level of psychological distress in the face of the COVID‐19 between the Jewish and Arab populations in Israel have shown a higher level of distress in the Arab population, both among the general population (Kimhi et al., 2020) and among pregnant women (Taubman – Ben‐Ari et al., 2020).
However, as far as we know, studies have thus far not compared the fears and anxieties of childbirth among Jewish and Arab pregnant women, neither in routine times nor in the face of the COVID‐19 pandemic.
1.1. The current study
Given the potentially harmful consequences of prenatal stress and in view of the fact that, as far as we know, no studies have been conducted to date that have examined this topic, this study sought to understand the factors that contribute to pregnant women's global FOC in this particularly difficult period, as well as to their specific anxiety over giving birth in the shadow of COVID‐19. Moreover, given the need to deepen our understanding on the implications of the COVID‐19 pandemic on multicultural societies and specifically on minority populations, this study compared Jewish and Arab women in an effort to identify differences between them.
In view of the literature, the following hypotheses were formulated.
Negative associations will be found between pregnant women's personal resources and their childbirth anxieties: the higher their self‐compassion and perceived social support, the lower the FOC and COVID‐19‐related childbirth anxiety they will report.
Positive associations will be found between pregnant women's COVID‐19‐related fears of being infected and concern for the welfare of the foetus and their anxieties over childbirth, so that the higher the COVID‐19‐related fears, the higher the FOC and COVID‐19‐related childbirth anxiety they will report.
In addition, given the lack of previous research on which to rely, the following questions were examined exploratively: (a) Are there differences between Jewish and Arab women in FOC and COVID‐19‐related childbirth anxiety, as well as in personal resources? (b) What is the unique and combined contribution of the background variables, personal resources and COVID‐19‐related fears to the pregnant woman's FOC and COVID‐19‐related childbirth anxiety? More specifically, the possibility that social support may moderate the association between self‐compassion, on one hand, and FOC and COVID‐19‐related childbirth anxiety will be examined.
2. METHODS
2.1. Study design
The current study is part of a larger research project pertaining to several psychological aspects of pregnant women in Israel in the shadow of COVID‐19. However, this study presents new information, not presented before (Chasson et al., 2020; Taubman – Ben‐Ari et al., 2020).
Following approval from the university's Institutional Review Board for this cross‐sectional study. A request to participate in the study was posted on social media groups for women in general and specifically for pregnant women, and a link to an online survey of the questionnaire was provided. The opening page ensured, in Hebrew and Arabic, the anonymity and confidentiality of the information, and explained that the woman could cease to participate at any stage should she wish to do so. In addition, the women were informed that if they felt any distress during or after completing the questionnaire, they could call or email the researchers, whose contact details were supplied.
2.2. Sampling frame
A convenience sample of Jewish and Arab Israeli women was recruited from 18 March to 9 April 2020. Participants were considered eligible for the study if they were pregnant and indicated that they could complete questionnaires in Hebrew. Of the 799 women who started to respond to the questionnaire, 403 completed it in full (50.4% response rate).
2.3. Instruments
The Pregnancy‐Related Anxiety Scale (Rini et al., 1999) was used to assess global FOC. Of the 10 items in the scale, the 4 which relate specifically to childbirth were employed: 1. “I am confident of having a normal childbirth” (reversed). 2. “I think my labour and delivery will go normally” (reversed). 3. “I am afraid that I will be harmed during delivery.” 4. “I am concerned (worried) about having a hard or difficult labour and delivery.” Participants were asked to respond to each item on a 4‐point scale ranging from 1 (never or not at all) to 4 (almost all the time or very much). Cronbach's alpha for the 4 items in the current study was α = 0.75. After reversing items, responses to all items were averaged to produce an FOC score, with higher scores indicating a higher level of global FOC.
The Self‐Compassion Scale‐Short Form (SCS‐SF; Raes et al., 2011) was used to measure self‐compassion. The questionnaire consists of 12 items divided into six subscales, a positive and a negative indication of each of the three elements of self‐compassion (negative indications are reverse coded): Self‐Kindness (e.g., “When I'm going through a very hard time, I give myself the caring and tenderness I need"); Self‐Judgment (e.g., “I'm disapproving and judgmental about my own flaws and inadequacies”); Common Humanity (e.g., “I try to see my failings as part of the human condition”); Isolation (e.g., “When I fail at something that's important to me, I tend to feel alone in my failure”); Mindfulness (e.g., “When something upsets me I try to keep my emotions in balance”); and Over‐Identification (e.g., “When I'm feeling down I tend to obsess and fixate on everything that's wrong”). Responses are marked on a 7‐point scale ranging from 1 (almost never) to 5 (almost always). Cronbach's alpha for the whole scale in the current study was 0.84. After reversing items, each participant's responses to all items were averaged to produce a single score, with higher scores indicating a higher level of self‐compassion.
The Multidimensional Scale of Perceived Social Support (MPSS; Zimet et al., 1988), a 12‐item questionnaire, which has been translated and validated in 22 different languages (Dambi et al., 2018), was used to assess social support. The scale relates to the respondent's perception of support from the family (e.g., “I get the emotional help and support I need from my family”), friends (e.g., “My friends really try to help me”) and a significant other (e.g., “I have a special person who is a real source of comfort to me”). Responses are marked on a scale ranging from 1 (very strongly disagree) to 7 (very strongly agree). In the current study, Cronbach's alpha for the whole scale was 0.91. Each participant's responses to all items were averaged to produce a social support score, with higher scores indicating a higher perception of available support.
Two items were used to tap the respondents' COVID‐19‐related fears (Taubman – Ben‐Ari et al., 2020). The women were asked how anxious they were about: (a) being infected by COVID‐19; and (b) the welfare of their foetus. Responses were marked on a scale from 1 (very little) to 5 (very much). Each item was scored separately, with higher scores indicating a higher level of the particular anxiety.
COVID‐19‐related childbirth anxiety was assessed by one item asking them how anxious they were about delivery during the pandemic. Responses were marked on a scale from 1 (very little) to 5 (very much), with higher scores indicating a higher level of COVID‐19‐related childbirth anxiety.
A sociodemographic questionnaire was used to tap the woman' background characteristics: age (continuous), education (1 = elementary; 2 = high school; 3 = post high school; 4 = academic), economic status (1 = below average; 2 = average; 3 = above average), physical health (1 = poor; 2 = average; 3 = good; 4 = very good), marital status (1 = single; 2 = married; 3 = in a couple relationship without marriage), ethnicity (0 = Jewish; 1 = Arab), gestation week (continuous), parity (0 = primiparous; 1 = multiparous), at‐risk pregnancy (0 = having medical diagnosis for a particular risk factor for pregnancy; 1 = regular/not at risk), and whether or not the women had undergone fertility treatments to conceive (0 = spontaneous pregnancy; 1 = pregnancy following fertility treatments). Women up to gestation week 27 were defined as being in trimesters 1 and 2, and women in week 28 and over as being in trimester 3.
2.4. Data analysis
Analyses were conducted using SPSS (ver. 24). First, imputation techniques were employed to recover missing values in the data. The actual rate of missing values fell below five percent, except for age, which reached ten percent. Thus, based on Enders's (2010) recommendation and a preliminary test of randomness (Little's MCAR test: χ2 = 208.184, df = 215, p = 0.618), we performed one imputation repeat to recover missing values, making it possible to use the full data set. Note that in further modelling, age did not have an effect on the dependent variables.
Next, a series of t tests were computed to examine ethnic differences in the study variables between Jewish and Arab women. We then calculated the correlations between the study and background variables and the level of FOC and COVID‐19‐related childbirth anxiety. Finally, two 5‐step hierarchical regressions were performed to determine the contribution of the independent variables to the outcome variables. The variables were entered as follows: In step 1, background variables; in Step 2, self‐compassion; in Step 3, perceived social support; in Step 4, COVID‐19‐related fears (being infected and concern for the foetus); and in Step 5, the interaction between self‐compassion and social support. Analysis of the source of the interaction was performed using the PROCESS procedure (Hayes, 2017).
3. RESULTS
3.1. Characteristic of study participants
As can be seen from Table 1, the final sample consisted of 403 women (233 Jewish and 170 Arab) aged 20–47 (M = 30.18, SD = 4.74) who were in gestational weeks 4–41 (M = 25.48, SD = 9.44). Of these, 44.4% were expecting their first child, while 55.6% already had at least one child. Most of the participants were married or in a spousal relationship (98.1%); 87.5% had an academic degree, and the rest had a high school or post‐high school diploma; 70.5% defined their income as average, 22.2% as above average, and 7.3% as below average; and 56.7% defined their health status as very good, 39.1% as good, and the rest as poor. No significant differences were found in the background variables between the two ethnic groups, save for the age of the women: the Arab women in the sample were somewhat younger than the Jewish women (M = 28.57, SD = 3.77; M = 31.20, SD = 5.11 respectively).
Table 1.
Sociodemographic characteristics of the participants (n = 403)
| Variable | |
| Age, M (SD) | 30.18 (4.74) |
| Gestation week, M (SD) | 25.48 (9.44) |
| Ethnicity, n (%) | |
| Jewish | 233 (57.8) |
| Arab | 170 (42.2) |
| Family status, n (%) | |
| Single | 7 (1.8) |
| Married | 383 (95) |
| In a marital relationship without marriage | 9 (2.3) |
| Education, n (%) | |
| Elementary | 4 (1) |
| High school | 19 (4.8) |
| Post‐high school | 27 (6.8) |
| Academic | 350 (87.5) |
| Socioeconomic status, n (%) | |
| Below average | 88 (22.2) |
| Average | 279 (70.5) |
| Above average | 29 (7.3) |
| Physical health, n (%) | |
| Poor | 1 (2) |
| Average | 16 (4) |
| Good | 157 (39.1) |
| Very good | 228 (56.7) |
| Parity, n (%) | |
| Primiparous | 178 (44.4) |
| Multiparous | 223 (55.6) |
| At‐risk pregnancy, n (%) | |
| Regular | 297 (74.6) |
| At risk | 101 (25.1) |
3.2. Differences between ethnic groups
The means and standard deviations of the study variables for each ethnic group, along with the results of the t tests, appear in Table 2. As can be seen from the table, Arab women reported significantly higher COVID‐19‐related fears both regarding their own infection and concern for the foetus. In addition, they displayed significantly more COVID‐19‐related childbirth anxiety, and marginally more FOC than Jewish women. No differences were found in personal resources between the two ethnic groups.
Table 2.
Means, standard deviations and t tests for the study variables by ethnic group
| Jewish women (n = 233) | Arab women (n = 170) | Cohen's d | t | |||
|---|---|---|---|---|---|---|
| M | SD | M | SD | |||
| Self‐compassion | 3.25 | 0.70 | 3.32 | 0.51 | 0.05 | 0.98 |
| Social support | 5.87 | 0.89 | 5.78 | 0.97 | 0.08 | 0.92 |
| Fear of infection | 3.58 | 1.12 | 3.79 | 0.99 | 0.20 | 1.96* |
| Concern for foetus | 3.88 | 1.15 | 4.18 | 1.05 | 0.26 | 2.67** |
| COVID‐related childbirth anxiety | 3.38 | 1.20 | 3.80 | 1.11 | 0.38 | 3.60*** |
| Fear of childbirth | 2.35 | 0.73 | 2.47 | 0.73 | 0.16 | 1.66† |
p < 0.05,
p < 0.01,
p < 0.001,
p = 0.10.
3.3. Associations between background and personal variables and COVID‐19‐related childbirth anxiety and FOC
The results of the Pearson correlations between the background variables and the personal resources (self‐compassion and perceived social support) on the one hand, and the outcome variables on the other, for the sample as a whole are presented in Table 3. As Table 3 shows, younger age, having poorer physical health, at‐risk pregnancy, lower self‐compassion and higher COVID‐19‐related fears were related to higher COVID‐19‐related childbirth anxiety. Poorer health, at‐risk pregnancy, lower self‐compassion, lower perceived social support and higher COVID‐19‐related fears were related to higher FOC. No significant correlations were found between the other background variables and either of the outcomes.
Table 3.
Hierarchical regression coefficients (beta weights) for fear of childbirth COVID‐19‐related childbirth anxiety
| COVID−19 related childbirth anxiety | Fear of childbirth | |||||||
|---|---|---|---|---|---|---|---|---|
| r | β | t | ∆R 2 | r | β | t | ∆R 2 | |
| Step 1 | ||||||||
| Age | −0.12* | −0.07 | 1.22 | 0.088*** | −0.05 | −0.03 | 0.47 | 0.088*** |
| Education | −0.07 | −0.05 | 1.08 | 0.04 | 0.06 | 1.14 | ||
| Economic status | −0.07 | −0.05 | 0.88 | −0.03 | 0.002 | 0.04 | ||
| Physical health | −0.12** | −0.16 | 3.21*** | −0.21*** | −0.21 | 4.29*** | ||
| Trimester a | 0.1 | 0.14 | 2.77** | −0.04 | 0 | 0.01 | ||
| Parity b | −0.08 | −0.07 | 1.32 | −0.09 | −0.11 | 1.96* | ||
| Fertility treatments c | 0.02 | −0.01 | 0.24 | 0.02 | −0.06 | 1.09 | ||
| At‐risk pregnancy d | 0.11* | 0.09 | 1.87 † | 0.16*** | 0.15 | 3.02** | ||
| Ethnic group e | 0.19*** | 0.19 | 3.36*** | 0.08 | 0.09 | 1.78 † | ||
| Step 2 | ||||||||
| Self‐compassion | −0.15** | −0.16 | 3.36*** | 0.043*** | −0.24*** | −0.24 | 4.91*** | 0.053*** |
| Step 3 | ||||||||
| Social support | −0.09 | 0.060‐ | 1.13 | 0.007 | −0.14** | −0.1 | 1.94 † | 0.008 |
| Step 4 | ||||||||
| Fear of infection | 0.58*** | 0.38 | 7.46*** | 0.325*** | 0.41*** | 0.28 | 4.70*** | 0.114*** |
| Concern for fetus | 0.54*** | 0.29 | 5.83*** | 0.29*** | 0.09 | 1.58 | ||
| Step 5 | ||||||||
| Self‐compassion X Social support | −0.02 | 0.56 | 0 | −0.14 | 2.96** | 0.016** | ||
| R 2 | 47.2 | 27.9 | ||||||
| F (14, 388) | 24.80*** | 10.71*** | ||||||
0 = trimesters 1 and 2, 1 = trimester 3.
0 = primiparous, 1 = multiparous.
0 = spontaneous pregnancy, 1 = pregnancy following fertility treatments.
0 = regular, 1 = at‐risk.
0 = Jewish women, 1 = Arab women.
p < 0.05,
p < 0.01,
p < 0.001,
p = 0.08.
3.4. Contribution of the independent variables to COVID‐19‐related childbirth anxiety and FOC
The regression analysis for COVID‐19‐related childbirth anxiety revealed that the independent variables explained 47.2% of the variance in this outcome. The results are presented in Table 3.
As can be seen from Table 3, the women's background characteristics in Step 1 contributed a significant 9.6% to the explained variance, with poorer health, being an Arab woman, and being in the third trimester of pregnancy contributing significantly to higher COVID‐19 related childbirth anxiety. At‐risk pregnancy contributed marginally to the variance in this step. Self‐compassion in Step 2 made a significant contribution of 2.5% to the explained variance, so that the lower the self‐compassion, the higher the anxiety. The contribution of perceived social support in Step 3 was nonsignificant (less than 1 percent). The COVID‐19‐related fears in Step 4 added a further 34.7% to the explanation of the variance, so that the more anxious the woman was about being infected and the more she was concerned for the welfare of the foetus, the higher her anxiety about giving birth during the pandemic. Finally, the interaction between self‐compassion and perceived social support, entered in Step 5 was not significant.
The regression analysis for FOC (Table 3) revealed that the independent variables explained 27.9% of its variance. The women's background characteristics in Step 1 contributed 8.8% to the explained variance, with poorer health, being primiparous, at‐risk pregnancy contributing significantly, and being an Arab woman making a marginally significant contribution to higher FOC. Self‐compassion in Step 2 contributed a further 5.3% to the explained variance, so that lower self‐compassion was associated with higher FOC. Although the contribution of Step 3 was nonsignificant, lower perceived support was marginally associated with higher FOC. The COVID‐19‐related fears in Step 4 added a further 11.4% to the explanation of the variance, with only the fear of being infected significantly associated with higher FOC. Finally, the interaction between self‐compassion and perceived social support was significant, adding 1.6% to the explained variance in FOC. Analysis of the source of the interaction (Hayes, 2017), presented in Figure 1, revealed a negative association between self‐compassion and FOC among women perceiving a high level of social support (b = −0.34, p < 0.001). Among women perceiving a low level of social support, the association between self‐compassion and FOC was not significant (b = −0.09, p = 0.19). In other words, only among women who reported a high level of social support, was higher self‐compassion associated with lower FOC.
Figure 1.
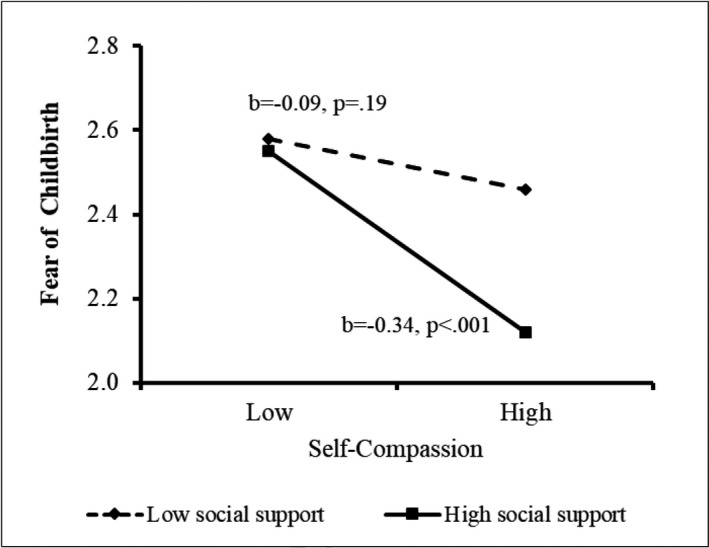
Effect of the interaction between self‐compassion and social support on fear of childbirth
4. DISCUSSION
The spread of COVID‐19 has impacted the lives of people around the world. In addition to health and economic consequences, the crisis undoubtedly has psychological implications, especially for vulnerable populations that are at increased risk, such as pregnant women. This study therefore sought to gain greater understanding of the implications of the pandemic for the childbirth anxieties of Jewish and Arab pregnant women in Israel.
4.1. Ethnicity differences and the contribution of background variables to pregnant women's anxieties
The findings show that Arab women reported higher levels of both COVID‐19‐related childbirth anxiety, global FOC and higher fears over of being infected and the welfare of the foetus. This is consistent with previous findings of an association between ethnicity and FOC (Dencker et al., 2019) and with studies that show a higher level of distress and psychological symptoms in the Arab population in Israel compared to the Jewish population, both among the general population and specifically among women in the perinatal period (Glasser et al., 2012; Halperin et al., 2014; Kimhi et al., 2020; Taubman – Ben‐Ari et al., 2020). It can be assumed that these differences may be due to the fact that Arab society in Israel lives in more crowded physical conditions, the level of income per family is lower, as well as the infrastructure and accessibility to health services are poorer compared to Jewish society (Chernichovsky et al., 2017). Thus, as essential gaps between the ethnic groups already exist due to difficulties that may be associated with belonging to a minority group, Arab women may be more vulnerable to higher levels of childbirth anxieties during the current crisis, as well as other related fears.
Moreover, although no difference in the level of social support between Jewish and Arab women was found in the present study, Arab society in Israel is characterised by family and community cohesion, which is usually expressed in residences close to the extended family (Feldman et al., 2001). Accordingly, it is possible that the requirement for social distance following the COVID‐19 crisis constituted a more threatening and undesirable factor for pregnant women from Arab society who are accustomed to living in close proximity to a wide social network and receiving support and assistance from their family and community. Thus, it is possible that a different measure of support from the community will be able to provide better explanation to the cultural and social implications of the social restrictions on Arab women and would also shed light on the differences found in the study between them and Jewish women.
In addition, our study indicates that poorer health, being in the third trimester of pregnancy, and to a lesser extent, at‐risk pregnancy, contribute significantly to higher COVID‐19‐related childbirth anxiety. It is reasonable to assume that those who are closest to the time of delivery are most conscious of the threat of the pandemic, particularly if their health or pregnancy is compromised. Similarly, poorer health, at‐risk pregnancy, and being primiparous significantly contributed to higher FOC. The associations between higher FOC and both poorer health and at‐risk pregnancy most likely reflect the understanding of the higher risk of giving birth in these conditions, particularly at this time. In regard to being primiparous, previous studies also indicate that these women report greater FOC than multiparous women (Rouhe et al., 2009; Zar et al., 2001). Having not yet experienced delivery, primiparous women are likely to have less of a sense of self‐efficacy and greater concerns about childbirth, which may be intensified by the ambiguity of the current situation and the restrictions placed on visitors to hospitals in general and maternity wards in particular. Women now have to choose whether to be accompanied by their spouse or mother, for example, and can no longer use the professional assistance of a doula. This may be especially stressful for a woman giving birth for the first time.
4.2. The contribution of personal resources to pregnant women's anxieties
The present study also highlights the contribution of personal resources to reducing childbirth anxieties in times of ambiguity and uncertainty. As predicted, the internal resource of self‐compassion was found to be associated with a lower level of both COVID‐19‐related childbirth anxiety and global FOC. The role played by self‐compassion as a shield against anxiety during stressful situations has been shown in previous studies (Chishima et al., 2018; Neff et al., 2007; Van Dam et al., 2011). However, to the best of our knowledge, this is the first study to report an association between self‐compassion and childbirth anxieties, a finding that has particular significance in view of the unique context of the pandemic. The results underline the importance of this personal resource in times of unusual stress, indicating that a woman's ability to be kind to herself—to be generous and uncritical of herself, to see her concerns as human and shared by women around the world, and to maintain a balanced view of her feelings and situation—enables her to feel less anxious even in uniquely threatening conditions.
In contrast, and contrary with our hypothesis, the external resource of perceived social support was found to contribute only marginally to a lower level of FOC, and not at all to COVID‐19‐related childbirth anxiety. We expected social support to serve as a major protective factor against stress and anxiety, as previous studies have consistently indicated (Laursen et al., 2008; Lukasse et al., 2014). However, it would seem that the special circumstances of the pandemic detract from its effectiveness, perhaps due to the enforcement of social distancing and the woman's knowledge that she will not be able to rely on the presence of her support system when the time comes for her to give birth.
Having said that, the finding of the moderating role of social support in the association between self‐compassion and FOC is worthy of note, as it suggests that perceived support may still play a role in reducing anxiety, and indicates the importance of the combination of the two personal resources, which have been found to be positively correlated in earlier studies (Maheux & Price, 2016; Wilson et al., 2020). Thus, whereas no connection was found between the level of self‐compassion and FOC among women with a low perception of social support, among those who perceived a high degree of available support, greater self‐compassion was associated with lower FOC. In other words, a stronger sense of social support may enhance the ability of a pregnant woman's self‐compassion to serve as a protective shield against fear of the approaching delivery.
4.3. The contribution of COVID‐19‐related anxieties to pregnant women's childbirth anxieties
Finally, as predicted, positive associations were found between pregnant women's COVID‐19‐related fears of being infected and concern for the welfare of the foetus and their anxieties over childbirth, suggesting that pregnancy during the pandemic is perceived as a risk in and of itself, a perception that may be shared by all women, regardless of their sociodemographic background and personal resources. The fact that concerns for the foetus contributed only to COVID‐19‐related childbirth anxiety and not to FOC should be further explored in future studies. It is possible that asking women to relate to giving birth during the pandemic directed their attention to the health risks involved, while asking specifically about delivery and labour shifted their attention to their feelings about the experience of childbirth itself. However, these findings are consistent with the theoretical framework that deals with the psychological consequences of a pandemic (Taylor, 2019) and in line with studies conducted during the SARS pandemic, which showed that pregnant women had high levels of anxieties and concerns related to the pandemic (Lee et al., 2006; Ng et al., 2004). The current study expands further and shows the negative consequences of COVID‐19 on the anxiety of pregnant women ahead of their expected birth.
4.4. Limitations
Certain limitations of the study should be noted. First, it is not based on a representative sample, which may limit its generalisability. More specifically, for purposes of comparing Jewish and Arab women, the proportion of Arabs in the current study is higher than in the Israeli population. However, as we are not aiming at presenting at describing proportions, but at understanding anxieties related to childbirth, this should not be considered a shortcoming of the study. In addition, a high proportion of women with academic education participated in the current study. This is frequent in non‐representative samples, as more educated women tend to participate more in studies (Radler & Ryff, 2010). Furthermore, it was conducted at single point in time during the crisis, when there is not yet any indication of when or how it will end and what the consequences in general, and the health implications for pregnant women in particular, will be. Therefore, further studies are needed, that will examine these and other aspects at additional points in time among pregnant women in the shadow of the COVID‐19 pandemic, with the aim of providing more information on the implications of women's anxieties during pregnancy on both the mother and the baby after birth.
4.5. Implications
Despite these limitations, we believe that the study makes an important contribution to the literature. Not only does it relate to a particularly vulnerable population, but it also examined two subpopulations of different religions and cultures. The findings suggest that pregnant women may be at increased risk for childbirth anxieties during a crisis. In addition, they indicate that minority populations, as well as primiparous women and those with poorer physical health and/or at‐risk pregnancies, are at greater risk of adverse psychological effects than others. This information should be available to clinicians, highlighting the potential negative consequences that women's anxieties may have during pregnancy both on childbirth and on the mental and physical health of the mother and the baby.
At the same time, the results highlight the contribution of a woman's personal and environmental resources, and particularly a combination of the two, in reducing childbirth anxieties, suggesting that professionals should attempt to strengthen and encourage these resources, especially in challenging times. The unique characteristics of the current crisis, unprecedented in the last hundred years, require individuals to maintain social distance and isolate themselves from their wider social and family systems. This isolation may compromise their ability to lean on their usual support network. As a society, we are called upon to do whatever possible under these circumstances to ensure the health, both physical and psychological, of pregnant women, who are at risk for perinatal and postpartum depression and other psychopathological disorders in the best of times, and especially in ambiguous, threatening and dangerous times. Awareness of the two resources found here to aid in reducing distress may help national leaders, clinicians and public health professionals, whether through public messages or focused culturally sensitive interventions, to enhance the well‐being of this vulnerable population.
CONFLICTS OF INTEREST
The authors have no conflict of interest.
Taubman – Ben‐Ari O, Chasson M, Abu‐Sharkia S. Childbirth anxieties in the shadow of COVID‐19: Self‐compassion and social support among Jewish and Arab pregnant women in Israel. Health Soc Care Community.2021;29:1409–1419. 10.1111/hsc.13196
Funding information
No funding was provided for this study.
REFERENCES
- Ahorsu, D. K. , Lin, C. Y. , Imani, V. , Saffari, M. , Griffiths, M. D. , & Pakpour, A. H. (2020). The fear of COVID‐19 scale: Development and initial validation. International Journal of Mental Health and Addiction. Advance Online Publication, 10.1007/s11469-020-00270-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asselmann, E. , Wittchen, H. U. , Erler, L. , & Martini, J. (2016). Peripartum changes in social support among women with and without anxiety and depressive disorders prior to pregnancy: A prospective‐longitudinal study. Archives of Women's Mental Health, 19(6), 943–952. 10.1007/s00737-016-0608-6 [DOI] [PubMed] [Google Scholar]
- Barker, D. J. (1998). In utero programming of chronic disease. Clinical Science, 95(2), 115–128. 10.1042/cs0950115 [DOI] [PubMed] [Google Scholar]
- Chasson, M. , Taubman‐Ben‐Ari, O. , & Abu‐Sharkia, S. (2020). Jewish and Arab pregnant women’s psychological distress during the COVID‐19 pandemic: The contribution of personal resources. Ethnicity & Health. Advance online publication. 10.1080/13557858.2020.1815000 [DOI] [PubMed] [Google Scholar]
- Chernichovsky, D. , Bisharat, B. , Bowers, L. , Brill, A. , & Sharony, C. (2017). The health of the Arab Israeli population: Taub Center for Social Policy Studies in Israel. [Google Scholar]
- Chishima, Y. , Mizuno, M. , Sugawara, D. , & Miyagawa, Y. (2018). The influence of self‐compassion on cognitive appraisals and coping with stressful events. Mindfulness, 9(6), 1907–1915. 10.1007/s12671-018-0933-0 [DOI] [Google Scholar]
- Choi, E. P. H. , Hui, B. P. H. , & Wan, E. Y. F. (2020). Depression and anxiety in Hong Kong during COVID‐19. International Journal of Environmental Research and Public Health, 17(10), 3740. 10.3390/ijerph17103740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dambi, J. M. , Corten, L. , Chiwaridzo, M. , Jack, H. , Mlambo, T. , & Jelsma, J. (2018). A systematic review of the psychometric properties of the cross‐cultural translations and adaptations of the Multidimensional Perceived Social Support Scale (MSPSS). Health and Quality of Life Outcomes, 16, 80. 10.1186/s12955-018-0912-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dayan, J. , Creveuil, C. , Herllicoviez, M. , Herbel, C. , Baeanger, E. , Savoye, C. , & Thouin, A. (2002). Role of anxiety and depression in the onset of spontaneous preterm labour. American Journal of Epidemiology, 155(4), 295–301. [DOI] [PubMed] [Google Scholar]
- Dencker, A. , Nilsson, C. , Begley, C. , Jangsten, E. , Mollberg, M. , Patel, H. , Wigert, H. , Hessman, E. , Sjöblom, H. , & Sparud‐Lundin, C. (2019). Causes and outcomes in studies of fear of childbirth: A systematic review. Women and Birth, 32(2), 99–111. 10.1016/j.wombi.2018.07.004 [DOI] [PubMed] [Google Scholar]
- Dunkel Schetter, C. , & Tanner, L. (2012). Anxiety, depression and stress in pregnancy: Implications for mothers, children, research, and practice. Current Opinion in Psychiatry, 25(2), 141–148. 10.1097/YCO.0b013e3283503680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elnekave, E. , & Gross, R. (2004). The healthcare experiences of Arab Israeli women in a reformed healthcare system. Health Policy, 69(1), 101–116. 10.1016/j.healthpol.2003.12.005 [DOI] [PubMed] [Google Scholar]
- Enders, C. K. (2010). Applied missing data analysis: Guilford Press. [Google Scholar]
- Felder, J. N. , Lemon, E. , Shea, K. , Kripke, K. , & Dimidjian, S. (2016). Role of self‐compassion in psychological well‐being among perinatal women. Archives of Women's Mental Health, 19(4), 687–690. 10.1007/s00737-016-0628-2 [DOI] [PubMed] [Google Scholar]
- Feldman, R. , Masalha, S. , & Nadam, R. (2001). Cultural perspective on work and family: Dual‐earner Israeli Jewish and Arab families at the transition to parenthood. Journal of Family Psychology, 15(3), 492–509. 10.1037/0893-3200.15.3.492 [DOI] [PubMed] [Google Scholar]
- Fourianalistyawati, E. , Uswatunnisa, A. , & Chairunnisa, A. (2018). The role of mindfulness and self‐compassion toward depression among pregnant women. International Journal of Public Health Science, 7(3), 162–167. 10.11591/ijphs.v7i3.11662 [DOI] [Google Scholar]
- Gao, J. , Zheng, P. , Jia, Y. , Chen, H. , Mao, Y. , Chen, S. , Wang, Y. I. , Fu, H. , & Dai, J. (2020). Mental health problems and social media exposure during COVID‐19 outbreak. PLoS One, 15(4), e0231924. 10.1371/journal.pone.0231924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gariepy, G. , Honkaniemi, H. , & Quesnel‐Vallee, A. (2016). Social support and protection from depression: Systematic review of current findings in Western countries. The British Journal of Psychiatry, 209(4), 284–293. 10.1192/bjp.bp.115.169094 [DOI] [PubMed] [Google Scholar]
- Glasser, S. , Tanous, M. , Shihab, S. , Goldman, N. , Ziv, A. , & Kaplan, G. (2012). Perinatal depressive symptoms among Arab women in Northern Israel. Maternal and Child Health Journal, 16(6), 1197–1205. 10.1007/s10995-011-0845-2 [DOI] [PubMed] [Google Scholar]
- Gómez‐Salgado, J. , Andrés‐Villas, M. , Domínguez‐Salas, S. , Díaz‐Milanés, D. , & Ruiz‐Frutos, C. (2020). Related health factors of psychological distress during the COVID‐19 pandemic in Spain. International Journal of Environmental Research and Public Health, 17(11), 3947. 10.3390/ijerph17113947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guardino, C. M. , & Dunkel Schetter, C. (2014). Coping during pregnancy: A systematic review and recommendations. Health Psychology Review, 8(1), 70–94. 10.1080/17437199.2012.752659 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halperin, O. , Sarid, O. , & Cwikel, J. (2014). A comparison of Israeli Jewish and Arab women's birth perceptions. Midwifery, 30(7), 853–861. 10.1016/j.midw.2013.11.003 [DOI] [PubMed] [Google Scholar]
- Hayes, A. F. (2017). Introduction to mediation, moderation, and conditional process analysis: A regression‐based approach: Guilford Press. [Google Scholar]
- Huang, Y. , & Zhao, N. (2020). Generalized anxiety disorder, depressive symptoms and sleep quality during COVID‐19 outbreak in China: A web‐based cross‐sectional survey. Psychiatry Research, 288, 112954. 10.1016/j.psychres.2020.112954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimhi, S. , Eshel, Y. , Marciano, H. , & Adini, B. (2020). Distress and resilience in the days of COVID‐19: Comparing two ethnicities. International Journal of Environmental Research and Public Health, 17(11), 3956. https://10.3390/ijerph17113956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laursen, M. , Hedegaard, M. , & Johansen, C. (2008). Fear of childbirth: Predictors and temporal changes among nulliparous women in the Danish National Birth Cohort. BJOG: an International Journal of Obstetrics and Gynaecology, 115(3), 354–360. 10.1111/j.1471-0528.2007.01583.x [DOI] [PubMed] [Google Scholar]
- Lee, D. T. , Sahota, D. , Leung, T. N. , Yip, A. S. , Lee, F. F. , & Chung, T. K. (2006). Psychological responses of pregnant women to an infectious outbreak: A case‐control study of the 2003 SARS outbreak in Hong Kong. Journal of Psychosomatic Research, 61(5), 707–713. 10.1016/j.jpsychores.2006.08.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lukasse, M. , Schrei, B. , & Ryding, E. (2014). Prevalence and associated factors of fear of childbirth in six European countries. Sex and Reproductive Health, 5(3), 99–106. 10.1016/j.srhc.2014.06.007 [DOI] [PubMed] [Google Scholar]
- MacBeth, A. , & Gumley, A. (2012). Exploring compassion: A meta‐analysis of the association between self‐compassion and psychopathology. Clinical Psychology Review, 32(6), 545–552. 10.1016/j.cpr.2012.06.003 [DOI] [PubMed] [Google Scholar]
- Maheux, A. , & Price, M. (2016). The indirect effect of social support on post‐trauma psychopathology via self‐compassion. Personality and Individual Differences, 88, 102–107. 10.1016/j.paid.2015.08.051 [DOI] [Google Scholar]
- Mulder, E. J. , De Medina, P. R. , Huizink, A. C. , Van den Bergh, B. R. , Buitelaar, J. K. , & Visser, G. H. (2002). Prenatal maternal stress: Effects on pregnancy and the (unborn) child. Early Human Development, 70(1–2), 3–14. 10.1016/S0378-3782(02)00075-0 [DOI] [PubMed] [Google Scholar]
- Neff, K. D. (2003). The development and validation of a scale to measure self‐compassion. Self and Identity, 2(3), 223–250. 10.1080/15298860309027 [DOI] [Google Scholar]
- Neff, K. D. (2011). Self‐compassion: Hodder and Stoughton. [Google Scholar]
- Neff, K. D. , Kirkpatrick, K. L. , & Rude, S. S. (2007). Self‐compassion and adaptive psychological functioning. Journal of Research in Personality, 41(1), 139–154. 10.1016/j.jrp.2006.03.004 [DOI] [Google Scholar]
- Ng, J. , Sham, A. , Leng Tang, P. , & Fung, S. (2004). SARS: Pregnant women's fears and perceptions. British Journal of Midwifery, 12(11), 698–703. 10.12968/bjom.2004.12.11.16710 [DOI] [Google Scholar]
- Nilsson, C. , Hessman, E. , Sjöblom, H. , Dencker, A. , Jangsten, E. , Mollberg, M. , Patel, H. , Sparud‐Lundin, C. , Wigert, H. , & Begley, C. (2018). Definitions, measurements and prevalence of fear of childbirth: A systematic review. BMC Pregnancy Childbirth, 18(1), 28. 10.1186/s12884-018-1659-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pires, R. , Araújo‐Pedrosa, A. , & Canavarro, M. C. (2014). Examining the links between perceived impact of pregnancy, depressive symptoms, and quality of life during adolescent pregnancy: The buffering role of social support. Maternal and Child Health Journal, 18(4), 789–800. 10.1007/s10995-013-1303-0 [DOI] [PubMed] [Google Scholar]
- Poikkeus, P. , Saisto, T. , Unkila‐Kallio, L. , Punamaki, R. L. , Repokari, L. , Vilska, S. , Tiitnen, A. , & Tulppala, M. (2006). Fear of childbirth and pregnancy‐related anxiety in women conceiving with assisted reproduction. Obstetrics and Gynecology, 108(1), 70–76. 10.1097/01.AOG.0000222902.37120.2f [DOI] [PubMed] [Google Scholar]
- Radler, B. T. , & Ryff, C. D. (2010). Who participates? Accounting for longitudinal retention in the MIDUS national study of health and well‐being. Journal of Aging and Health, 22(3), 307–331. 10.1177/0898264309358617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raes, F. , Pommier, E. , Neff, K. D. , & Van Gucht, D. (2011). Construction and factorial validation of a short form of the self‐compassion scale. Clinical Psychology & Psychotherapy, 18(3), 250–255. 10.1002/cpp.702 [DOI] [PubMed] [Google Scholar]
- Räisänen, S. , Lehto, S. M. , Nielsen, H. S. , Gissler, M. , Kramer, M. R. , & Heinonen, S. (2014). Fear of childbirth in nulliparous and multiparous women: A population‐based analysis of all singleton births in Finland in 1997–2010. BJOG: an International Journal of Obstetrics and Gynaecology, 121(8), 965–970. 10.1111/1471-0528.12599 [DOI] [PubMed] [Google Scholar]
- Rini, C. K. , Dunkel‐Schetter, C. , Wadhwa, P. D. , & Sandman, C. A. (1999). Psychological adaptation and birth outcomes: The role of personal resources, stress, and sociocultural context in pregnancy. Health Psychology, 18(4), 333–345. 10.1037/0278-6133.18.4.333 [DOI] [PubMed] [Google Scholar]
- Rondung, E. , Thomten, J. , & Sundin, O. (2016). Psychological perspectives on fear of childbirth. Journal of Anxiety Disorders, 44, 80–91. 10.1016/j.janxdis.2016.10.007 [DOI] [PubMed] [Google Scholar]
- Rouhe, H. , Salmela‐Aro, K. , Halmesmäki, E. , & Saisto, T. (2009). Fear of childbirth according to parity, gestational age, and obstetric history. BJOG: an International Journal of Obstetrics and Gynaecology, 116(1), 67–73. 10.1111/j.1471-0528.2008.02002.x [DOI] [PubMed] [Google Scholar]
- Shwartz, N. , Shoahm‐Vardi, I. , & Daoud, N. (2019). Postpartum depression among Arab and Jewish women in Israel: Ethnic inequalities and risk factors. Midwifery, 70, 54–63. 10.1016/j.midw.2018.12.011 [DOI] [PubMed] [Google Scholar]
- Soltani, F. , Eskandari, Z. , Khodakarami, B. , Parsa, P. , & Roshanaei, G. (2017). Factors contributing to fear of childbirth among pregnant women in Hamadan (Iran) in 2016. Electron Physician, 9(7), 4725–4731. 10.19082/4725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart, R. C. , Umar, E. , Tomenson, B. , & Creed, F. (2014). Validation of the multi‐dimensional scale of perceived social support (MSPSS) and the relationship between social support, intimate partner violence and antenatal depression in Malawi. BMC Psychiatry, 14(1), 180. 10.1186/1471-244X-14-180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taubman – Ben‐Ari, O. , Chasson, M. , Abu Sharkia, S. , & Weiss, E. (2020). Distress and anxiety associated with COVID‐19 among Jewish and Arab pregnant women in Israel. Journal of Reproductive and Infant Psychology, 38(3), 340–348. 10.1080/02646838.2020.1786037 [DOI] [PubMed] [Google Scholar]
- Taylor, S. (2019). The psychology of pandemics: Preparing for the next global outbreak of infectious disease: Cambridge Scholars Publishing. [Google Scholar]
- Ternstrom, E. , Hildingsson, I. , Haines, H. , & Rubertsson, C. (2015). Higher prevalence of childbirth related fear in foreign born pregnant women—Findings from a community sample in Sweden. Midwifery, 31(4), 445–450. 10.1016/j.midw.2014.11.011 [DOI] [PubMed] [Google Scholar]
- Tomfohr‐Madsen, L. , Cameron, E. E. , Dunkel Schetter, C. , Campbell, T. , O'Beirne, M. , Letourneau, N. , & Giesbrecht, G. F. (2019). Pregnancy anxiety and preterm birth: The moderating role of sleep. Health Psychology, 38(11), 1025–1035. 10.1037/hea0000792 [DOI] [PubMed] [Google Scholar]
- Van Dam, N. T. , Sheppard, S. C. , Forsyth, J. P. , & Earleywine, M. (2011). Self‐compassion is a better predictor than mindfulness of symptom severity and quality of life in mixed anxiety and depression. Journal of Anxiety Disorders, 25(1), 123–130. 10.1016/j.janxdis.2010.08.011 [DOI] [PubMed] [Google Scholar]
- Wang, C. , Pan, R. , Wan, X. , Tan, Y. , Xu, L. , Ho, C. S. , & Ho, R. C. (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID‐19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17(5), 1729. 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson, J. M. , Weiss, A. , & Shook, N. J. (2020). Mindfulness, self‐compassion, and savoring: Factors that explain the relation between perceived social support and well‐being. Personality and Individual Differences, 152, 109568. 10.1016/j.paid.2019.109568 [DOI] [Google Scholar]
- Winders, S. J. , Murphy, O. , Looney, K. , & O'Reilly, G. (2020). Self‐compassion, trauma, and posttraumatic stress disorder: A systematic review. Clinical Psychology & Psychotherapy, 27, 300–329. 10.1002/cpp.2429 [DOI] [PubMed] [Google Scholar]
- Yedid Sion, M. , Harlev, A. , Weintraub, A. Y. , Sergienko, R. , & Sheiner, E. (2016). Is antenatal depression associated with adverse obstetric and perinatal outcomes? The Journal of Maternal‐Fetal & Neonatal Medicine, 29(6), 863–867. 10.3109/14767058.2015.1023708 [DOI] [PubMed] [Google Scholar]
- Zar, M. , Wijma, K. , & Wijma, B. (2001). Pre‐ and postpartum fear of childbirth in nulliparous and parous women. Scandinavian Journal of Behaviour Therapy, 30, 75–84. 10.1080/02845710121310 [DOI] [Google Scholar]
- Zeller, M. , Yuval, K. , Nitzan‐Assayag, Y. , & Bernstein, A. (2015). Self‐compassion in recovery following potentially traumatic stress: Longitudinal study of at‐risk youth. Journal of Abnormal Child Psychology, 43(4), 645–653. 10.1007/s10802-014-9937-y [DOI] [PubMed] [Google Scholar]
- Zhen, R. , Quan, L. , & Zhou, X. (2018). How does social support relieve depression among flood victims? The contribution of feelings of safety, self‐disclosure, and negative cognition. Journal of Affective Disorders, 229, 186–192. 10.1016/j.jad.2017.12.087 [DOI] [PubMed] [Google Scholar]
- Zimet, G. D. , Dahlem, N. W. , Zimet, S. G. , & Farley, G. K. (1988). The multidimensional scale of perceived social support. Journal of Personality Assessment, 52(1), 30–41. 10.1207/s15327752jpa5201_2 [DOI] [PubMed] [Google Scholar]


