Abstract
SARS-CoV2, first described in December 2019, was declared a pandemic by the World Health Organization in March 2020. Various surgical and medical societies promptly published guidelines, based on expert opinion, on managing patients with COVID-19, with a consensus to postpone elective surgeries and procedures. We describe the case of an orthotopic liver transplantation (OLT) in a young female who presented with acute liver failure secondary to acetaminophen toxicity to manage abdominal pain and in the setting of a positive SARS-CoV2 test. Despite a positive test, she had no respiratory symptoms at time of presentation. The positive test was thought to be residual viral load. The patient had a very favorable outcome, likely related to multiple factors including her young age, lack of respiratory COVID-19 manifestations and plasma exchange peri-operatively. We recommend a full work-up for OLT in COVID-19 patients with uncomplicated disease according to standard of care, with careful interpretation of COVID-19 testing in patients presenting with conditions requiring urgent or emergent surgery as well as repeat testing even a few days after initial testing, as this could alter management.
KEYWORDS: clinical research/practice, drug toxicity, fulminant hepatic failure, infection and infectious agents – viral, infectious disease, liver transplantation/hepatology, plasmapheresis/plasma exchange
Abbreviations: ALT, alanine transaminase; AST, aspartate transaminase; COVID-19, coronavirus disease 2019; CT, computerized tomography; ECG, electrocardiogram; ER, emergency room; HV-PE, high-volume plasma exchange; OLT, orthotopic liver transplantation; SARS-CoV2, severe acute respiratory syndrome coronavirus 2
1. INTRODUCTION
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV2) was first identified in December 2019 after a series of unexplained pneumonia cases began to spread in Wuhan, China. Since then, it rapidly became an international public health emergency and was declared a pandemic on March 11, 2020 with more than eight million confirmed cases to date according to the World Health Organization.1 , 2 While Coronavirus disease COVID-19 mainly involves the respiratory system, it has also been shown to affect other organs including the kidneys, heart, and digestive tract3 , 4 with a recent study showing abdominal pain in 4% of cases with mild disease severity, diarrhea in 32% and vomiting in 12% of cases.3 Various surgical and medical societies promptly published guidelines, based on expert opinion, on managing patients with COVID-19, with a consensus to postpone elective surgeries and procedures.5 , 6 With the urgent need for evidence on outcomes of surgeries performed on patients with COVID-19, a recently published study found an increased risk of postoperative pulmonary complications in patients with preoperative SARS-CoV2 infection and increased mortality in men older than 70, a finding supporting postponing elective surgeries.7 However, with the ongoing spread of the infection and increased testing, we expect a higher number of patients presenting with an emergent surgical indication who could have SARS-CoV2 and outcomes remain largely unknown. In this article, we describe the case of an orthotopic liver transplant (OLT) in a patient with a positive SARS-CoV2 test, presenting with acute liver failure secondary to acetaminophen overdose to manage abdominal pain.
2. CASE
2.1. Presentation and pretransplant hospital course
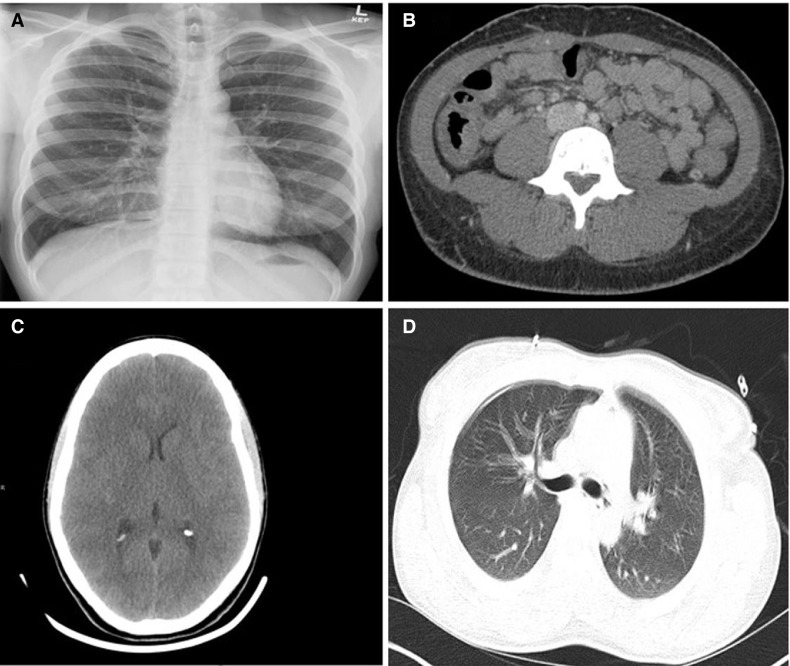
A 27-year-old healthy African American female with a remote history of focal segmental glomerular sclerosis and body mass index of 22.6 presented to the emergency room (ER) with nausea, vomiting, and abdominal pain radiating to the chest for 2 weeks. To manage her pain, she ingested >50 tablets of acetaminophen over the 3–4 days preceding presentation. In the ER, she was hemodynamically stable except for mild tachycardia. Blood pressure was 133/85 mm Hg, heart rate was 104 beats-per-minute and she had normal temperature. She had no tachypnea and oxygen saturation was 100% on room air. She had generalized abdominal tenderness, normal cardiac and pulmonary examination otherwise. Her mental status and neurological exam were intact upon presentation. Initial blood work revealed a leukocytosis of 19.36 k/µl, and elevated aminotransferases with alanine transaminase (ALT) of 2791 U/L and aspartate transaminase (AST) of 3202 U/L. Her total bilirubin was 2.9 mg/dl, alkaline phosphatase was 97 U/L and INR 1.7. She had a mild acute kidney injury with a creatinine of 1.04 mg/dl (baseline of 0.8 mg/dl). Lactate was 12.9 mEq/l and D-dimer was 21 830 ng/ml. Acetaminophen level was 42 µg/ml (upper limit of normal 30 µg/ml). A chest X-ray was obtained and was normal ( Figure 1A). Computerized tomography (CT) of her abdomen and pelvis demonstrated diffuse colonic wall thickening most pronounced in the cecum, ascending, and sigmoid colon (Figure 1B). There was no evidence of hepatic steatosis on imaging. A COVID-19 nasopharyngeal swab was obtained given diarrhea and abdominal pain and was positive for SARS-CoV2 by reverse transcriptase polymerase chain reaction. On further history, she had taken care of her significant other with COVID-19 around 6–10 weeks prior to presentation. She had developed cough but was not tested. By the time she presented to the ER, her respiratory symptoms had resolved. She was started on N-acetylcysteine infusion and the decision was to admit her to the medical intensive liver care unit for further management and close monitoring of acute liver injury in the setting of acetaminophen overdose and a positive SARS-CoV2 test. Liver injury work-up included negative testing for acute viral hepatitis, negative serological testing for autoimmune and genetic etiologies of liver disease. Two days after admission, her hepatic synthetic function worsened significantly. Her total bilirubin peaked to 4.3 mg/dl and INR to 6.3. Aminotransferases peaked to an AST 9741 U/L and ALT 11 322 U/L. Her kidney function worsened, and she became oliguric. Later that day, frequent neurological examinations showed progressive changes in her mental status and the patient met criteria for acute liver failure attributed to acetaminophen overdose. Hepatic encephalopathy eventually progressed to grade 3 of West Haven Grading system. An urgent CT brain showed diffusely small cerebral sulci and basal cisterns concerning for brain swelling (Figure 1C). Arterial ammonia was 196 µmol/L and the patient was started on continuous renal replacement therapy and eventually required intubation for airway protection. Neurology and neurosurgery were consulted, and it was decided to proceed with placement of a right frontal intracranial pressure monitor. Increased intracranial pressure was treated with 3% hypertonic saline for a sodium goal between 145 and 155 mmol/L, and supportive measures. She retained all brainstem reflexes. She required high-dose vasopressors for undifferentiated shock, as she had normal cardiac function (ejection fraction 64%) and negative infectious work-up.
FIGURE 1.
(A) Chest X-ray upon admission; (B) computerized tomography of the abdomen and pelvis upon admission with evidence of colitis; (C) computerized tomography of the brain with evidence of brain edema; (D) computerized tomography of the chest with no gross interstitial lung disease and evidence of mild pneumomediastinum
2.2. Emergent liver transplant evaluation and preoperative management
An emergent liver transplant evaluation was initiated. Interleukin-6 was 131.3 pg/L. Work-up was notable for absolute lymphocytopenia, thrombocytopenia, and hypoalbuminemia. CT chest was obtained to evaluate the lung parenchyma in the setting of possible COVID-19. While imaging did not demonstrate interstitial lung disease, mild pneumomediastinum predominantly involving the posterior mediastinum was found and was most prominent around the esophagus and left mainstem bronchus (Figure 1D). Of note, imaging was obtained shortly prior to intubation and pneumomediastinum was attributed possibly to an esophageal microperforation secondary to vomiting. She was started on broad-spectrum antimicrobials and further investigations of pneumomediastinum were held as she was eventually intubated and developed brain edema. Repeat COVID-19 testing 2 days after the initial test came back negative. She was evaluated by anesthesia, psychiatry, pharmacy, nutrition, and the transplant social worker in addition to transplant hepatology and surgery. Given her initial high vasopressor requirements making her unsuitable for OLT, she underwent high-volume plasma exchange (HV-PE) (8.0 L per session) using 100% plasma replacement and completed two HV-PE treatments as a bridge to liver transplantation. Following the first HV-PE, her vasopressor requirements improved to minimal doses, and her prothrombin time/INR corrected to 1.2, enabling further evaluation for liver transplant candidacy. After multi-disciplinary discussions including transplant hepatology, transplant surgery, infectious diseases, psychiatry, transplant social worker, pharmacy, nutrition, and anesthesia, her initial positive COVID-19 test was thought to represent residual virus from a previous infection that has cleared. A viral load was estimated by the cycle threshold of the SARS-CoV-2 RNA detection assay used. Based on this result that corroborated the patient’s history it was concluded she had cleared her prior SARS-CoV-2 infection. The case was hence approached like any other ALF case. She was deemed an acceptable candidate and was listed in the United Network for Organ Sharing as status 1A.
2.3. Orthotopic liver transplantation
She underwent successful OLT with skin closure only from a donor after brain death the day after she was listed. Surgery was complicated by hypotension, bradycardia with junctional rhythm and rise in intracranial pressure prior to native liver explantation, leading to significant ST elevation on electrocardiogram (ECG) concerning for an ST elevation myocardial infarction. ECG changes largely resolved after reperfusion. Cold ischemic time was 7 hours 19 minutes, warm ischemic time was 29 minutes. Intraoperative estimated blood loss was 5 L and the patient received 5 units of packed red blood cells, 1 unit of platelets, 10 units of cryoprecipitates and 750 ml of autotransfusion via CellSaver. Thromboelastography was used to trend coagulopathy during surgery. Pathology revealed hepatic parenchyma with extensive (>95%) centrilobular necrosis suggestive of acetaminophen toxicity. There was no significant steatosis.
2.4. Recovery following orthotopic liver transplantation
She was transferred to the surgical intensive care unit following OLT and was started on tacrolimus with a trough level goal of 10–12 ng/ml and a steroid taper for immunosuppression, per standard of care as she was deemed not to have an active COVID-19 infection. She initially continued to have intermittent spikes in intracranial pressure on postoperative days 1 and 2. The intracranial pressure monitor was removed on day 3 after surgery and the patient came off vasopressors. Her neurological status returned to baseline. She received COVID-19 convalescent plasma on postoperative day 1, per expert opinion, in the event where she had an active infection, given the severity of her illness and lack of available literature. Her hepatic function tests continued to improve following OLT. Her total bilirubin and INR normalized to 0.5 mg/dl and 1.1, respectively. An ECG was obtained postoperatively and was normal. A repeat echocardiogram revealed normal cardiac function. She was extubated 5 days postoperatively and transferred to a regular nursing floor. Repeat CT chest demonstrated resolution of previously seen pneumomediastinum. A third COVID-19 test was obtained 6 days following surgery and came back negative. She underwent closure of fascia 10 days postoperatively. A CT abdomen days later revealed abdominal wall hematomas requiring hematoma evacuation in the OR. She continued to improve and was discharged 27 days post-OLT in good condition.
3. DISCUSSION
We report the case of OLT in a patient with positive SARS-CoV2 and acute liver failure secondary to acetaminophen toxicity. The patient had excellent outcomes post OLT. While COVID-19 has been shown to cause acute liver injury,8, 9, 10, 11 there have been no reports of acute liver failure related to the viral illness itself. In one study looking at abnormal liver function tests in COVID-19 patients, 85 of 318 patients with COVID-19 had severe disease. Of those, 10 had multiorgan failure with 2 developing liver failure thought to be secondary to critical illness or possibly medications used to treat COVID-19.8 Xu et al4 examined pathological findings from a patient with COVID-19 and liver biopsy specimens showed moderate microvesicular steatosis with mild lobular and portal activity, suggesting drug-induced liver injury or injury caused directly by the virus. Two other studies found a higher AST elevation with more severe disease.10 , 11 Huang et al10 noted an AST elevation in 62% (N = 8/13) of patients requiring intensive care unit care as opposed to 25% (N = 7/28) of patients with COVID-19 who did not. It has been hypothesized that SARS-CoV2 might directly bind to the angiotensin-converting enzyme 2 present in cholangiocytes and hence causing liver injury. Another theory is direct liver injury caused by the hepatotoxic drugs used to suppress the immune-mediated response to COVID-19 and finally the cytokine storm and critical illness could also play a role.9 Our patient did not receive any hepatotoxic drugs to suppress the COVID-19-related cytokine storm. While there could have been a component of liver injury related to recent COVID-19, the patient’s pathology was supportive of acetaminophen toxicity.
Our patient had favorable clinical and surgical outcomes following a major emergent liver transplantation surgery. This is an important addition to the literature given the emerging evidence and concerns for increased mortality and pulmonary complications in patients with SARS-CoV2 undergoing surgery. Studies so far have demonstrated increased postoperative mortality and pulmonary complications in patients with SARS-CoV2 undergoing surgery with 30-day mortality ranging between 20% and 30%.7 , 12 , 13 Our patient could have had favorable outcomes for various reasons: (1) she had no respiratory symptoms or interstitial lung disease related to SARS-CoV2; (2) she was young and healthy; (3) she received COVID-19 convalescent plasma the day following surgery and (4) received HV-PE per the acute liver failure protocol, which might have also helped eliminate inflammatory cytokines and resetting the hypercoagulable state induced by COVID-1914; (5) given her history, it is likely she had remote COVID-19 infection and the initial positive test represented residual measurable virus.
In conclusion, we present the case of an OLT in a patient with recent COVID-19 and acute liver failure secondary to acetaminophen overdose. Our patient showed favorable clinical and surgical outcomes likely in the setting of her young age, lack of respiratory COVID-19 manifestations and HV-PE peri-operatively which might have helped clear cytokines produced in response to recent COVID-19, although the infection was then thought to have cleared by the time of transplant. We recommend careful interpretation of COVID-19 testing in patients presenting with conditions requiring urgent or emergent surgery as well as repeat testing, even if a couple days after initial testing, as this could alter management.
Acknowledgments
DISCLOSURE
The authors of this manuscript have no conflicts of interest to disclose as described by the American Journal of Transplantation.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1.WHO. WHO Coronavirus Disease (COVID-19) Dashboard. https://www.who.int/news-room/detail/27-04-2020-who-timeline–-covid-19. Accessed June 20, 2020.
- 2.WHO. WHO Coronavirus Disease (COVID-19) Dashboard. https://covid19.who.int/?gclid=Cj0KCQjwirz3BRD_ARIsAImf7LN-y9U4MxwDjv3qHdlEsUxn6LsJOR4qCcHSnxYI1Fn5zZSA0YtoICsaAr4GEALw_wcB. Accessed June 20, 2020.
- 3.Han C, Duan C, Zhang S, et al. Digestive symptoms in COVID-19 patients with mild disease severity: clinical presentation, stool viral RNA testing, and outcomes. Am J Gastroenterol. 2020;115(6):916–923. doi: 10.14309/ajg.0000000000000664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8(4):420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American College of Surgeons. COVID-19: Recommendations for Management of Elective Surgical Procedure. https://www.facs.org/-/media/files/covid19/recommendations_for_management_of_elective_surgical_procedures.ashx. Released March 13, 2020.
- 6.American Society of Transplant Surgeons. Re-engaging Organ Transplantation in the COVID-19 Era. https://asts.org/advocacy/covid-19-resources/asts-covid-19-strike-force/re-engaging-organ-transplantation-in-the-covid-19-era#.Xu99sW5Fxgs. Released June 5, 2020.
- 7.Archer JE, Odeh A, Ereidge S, et al. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV2-infection: an international cohort study. Lancet. 2020;396:27–38. doi: 10.1016/S0140-6736(20)31182-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cai Q, Huang D, Yu H, et al. COVID-19: abnormal liver function tests. J Hepatol. 2020;73(3):566–574. doi: 10.1016/j.jhep.2020.04.006. S0168-8278(20)30218-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang C, Shi L, Wang FS. Liver injury in COVID-19: management and challenges. Lancet Gastroenterol Hepatol. 2020;5(5):428–430. doi: 10.1016/S2468-1253(20)30057-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang C, Wang Y, Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guan W-J, Ni Z-Y, Hu Y. Clinical characteristics of 2019 novel coronavirus infection in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lei S, Jiang F, Su W, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine. 2020;21:100331. doi: 10.1016/j.eclinm.2020.100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nahshon C, Bitterman A, Haddad R, et al. Hazardous postoperative outcomes of unexpected COVID-19 infected patients: a call for global consideration of sampling all asymptomatic patients before surgical treatment. World J Surg. 2020;44(8):2477–2481. doi: 10.1007/s00268-020-05575-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Keith P, Day M, Perkins L, et al. A novel treatment approach to the novel coronavirus: an argument for the use of therapeutic plasma exchange for fulminant COVID-19. Crit Care. 2020;24(1):128. doi: 10.1186/s13054-020-2836-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.