Abstract
Due to the COVID‐19 pandemic, in‐person educational activities for emergency medicine (EM) residents were suspended. As a result, we developed a virtual point‐of‐care ultrasound (POCUS) course for incoming EM interns consisting of online didactics and faculty‐proctored hands‐on scan sessions utilizing a video conferencing platform and a handheld smartphone‐compatible ultrasound transducer. Learners found the course to be effective in improving their POCUS knowledge and scanning skills. Feedback obtained from this course will allow us to improve future virtual courses.
A mainstay of point‐of‐care ultrasound (POCUS) education for emergency medicine (EM) residents is an introductory course consisting of didactics and faculty‐guided hands‐on scan sessions. 1 , 2 , 3 Precepted hands‐on practice is critical for clinicians in developing competence in emergency ultrasound (EUS). Limitations placed on in‐person educational activities due to the COVID‐19 pandemic have had a particularly profound effect on this aspect of ultrasound education. In a recently published consensus document describing pandemic‐related modifications in ultrasound education, national ultrasound education leaders recommended the use of handheld portable ultrasound devices to provide EM residents with increased scanning experience outside of the clinical setting. 4 Aligning with this recommendation, we developed a virtual emergency ultrasound course for EM interns using a teleconferencing platform and smartphone‐compatible ultrasound devices.
EXPLANATION
We hosted the course utilizing a video conferencing platform (Zoom Video Communications, Inc., San Francisco, CA) for 12 EM interns. Eight EM advanced practice provider residents and two pediatric EM fellows also enrolled in the course. Before the course, learners were divided into pairs. EM interns were paired with each other. As social distancing guidelines prohibited large‐group gatherings at the hospital, each pair participated in the course from one pair member’s residence. During the course, learners viewed live online lectures and scanned each other using a smartphone‐compatible ultrasound transducer (Butterfly Network, Inc., Guilford, CT).
All course faculty members were emergency ultrasound fellowship trained or credentialed as registered diagnostic medical sonographers. During the course, faculty delivered lectures reviewing core POCUS applications. Small‐group breakout sessions followed lectures throughout the course. During these sessions, faculty members were each assigned to two pairs of learners. Over Zoom, faculty viewed each learner scanning his/her course partner. Learners were instructed to position their cameras so that faculty could view simultaneously transducer placement and the smartphone screen showing ultrasound images (Figure 1). Faculty provided feedback on scanning technique and adequacy of obtained views.
Figure 1.

In this screenshot from the course, one learner scans his partner with a handheld ultrasound device while showing both probe position and the resulting ultrasound image on his smartphone screen to the camera.
DESCRIPTION
Ten interns responded to a postcourse survey. On a 5‐point Likert scale (ranging from “not at all effective” to “extremely effective”), eight learners rated the hands‐on portion of the course “very effective” or “extremely effective.” On a 4‐point Likert scale (ranging from “strongly disagree” to “strongly agree”), 90 and 80% of respondents strongly agreed that the course improved their POCUS fund of knowledge and POCUS scanning skills, respectively. When asked to choose a substitute for in‐person scan sessions should COVID‐19 restrictions continue, all respondents chose hands‐on scanning with Zoom faculty guidance over ultrasound simulators and instructional videos.
During the course, we found that using the Zoom “share screen” option on the phone connected to the transducer while maintaining a laptop camera directed at the learner being scanned allowed for better visualization of both probe position and resulting images (Figure 2). For future courses, utilizing Butterfly’s telemedicine option may also improve virtual scan sessions.
Figure 2.
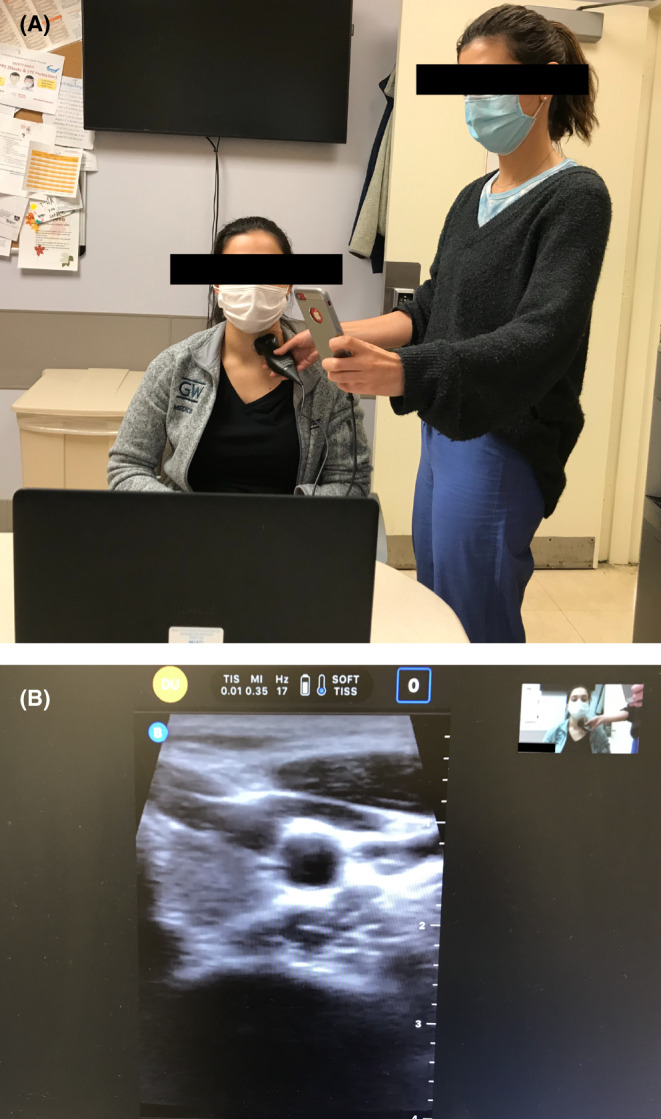
Utilizing the Zoom share screen option on the learner’s smartphone may aid faculty in better visualizing the learner’s ultrasound images. (A) The learner’s computer camera is directed at the ultrasound probe to show probe position. (B) The ultrasound instructor’s Zoom meeting display shows both probe position and the learner's smartphone screen with the resulting ultrasound image.
Faculty found that because teaching POCUS skills virtually preclude physically guiding a learner’s hand in probe placement and movement, a higher level of expertise is required to teach these skills over Zoom. Reviewing standard terms used to describe transducer manipulation before the course would have been useful in guiding learners as they scanned their partners. Preventing faculty from steering a learner’s hand was an unexpected benefit of the virtual course as this forced learners to incorporate verbal and somatosensory feedback in adjusting their probes, which may be more effective in psychomotor skill development. 5 , 6 , 7 For future courses, having faculty employ hands‐off modeling during scan sessions may further enhance EUS skill acquisition. In this teaching technique described by Gottlieb, 8 the instructor models probe placement and adjustment in real time as the learner scans his/her model.
This virtual POCUS course was well received by learners. We believe that this is an effective method of providing EUS education if COVID‐19 restrictions on medical education continue. Insight gained from the first iteration of this course will aid us in optimizing future courses.
AEM Education and Training. 2021;5:102–104
The author has no relevant financial information or potential conflicts to disclose.
Author contributions: SDL—study concept and design, data acquisition, data analysis and interpretation, drafting of manuscript.
References
- 1. Akhtar S, Theodoro D, Gaspari R, et al. Resident training in emergency ultrasound: consensus recommendations from the 2008 Council of Emergency Medicine Residency Directors Conference. Acad Emerg Med 2009;16:S32–6. [DOI] [PubMed] [Google Scholar]
- 2. Ultrasound guidelines: emergency, point‐of‐care and clinical ultrasound guidelines in medicine. Ann Emerg Med 2017;69:e27–54. [DOI] [PubMed] [Google Scholar]
- 3. McGrath J, Barrie M, Way DP. Emergency medicine resident orientation: how training programs get their residents started. West J Emerg Med 2017;18:97–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Panebianco NA, Liu RB, Alerhand S, et al. Joint recommendations and resources for clinical ultrasound education amidst the COVID‐19 era. AEM Educ Train 2020. doi: 10.1002/aet2.10506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Elliott D, Grierson LE, Hayes SJ, Lyons J. Action representations in perception, motor control and learning: implications for medical education. Med Educ 2011;45:119–31. [DOI] [PubMed] [Google Scholar]
- 6. Nicholls D, Sweet L, Hyett J. Psychomotor skills in medical ultrasound imaging: an analysis of the core skill set. J Ultrasound Med 2014;33:1349–52. [DOI] [PubMed] [Google Scholar]
- 7. Wulf G, Shea C, Lewthwaite R. Motor skill learning and performance: a review of influential factors. Med Educ 2010;44:75–84. [DOI] [PubMed] [Google Scholar]
- 8. Gottlieb M. Hands‐off ultrasound technique: utilizing simultaneous modeling to enhance ultrasound training. AEM Educ Train 2018;2:55–6. [DOI] [PMC free article] [PubMed] [Google Scholar]


