Abstract
Purpose:
To identify and synthesize the literature on healthcare system distrust across the breast cancer continuum of care
Methods:
We searched CINAHL, Cochrane, EMBASE, PubMed, PsycINFO, and Web of Science from January 1st, 1990 to December 31st 2018 for all peer-reviewed publications addressing the role of healthcare system trust, distrust or mistrust in the breast cancer continuum of care.
Results:
We identified a total of 20 studies, seven qualitative studies and thirteen quantitative studies. Two studies assessed genetic testing, eleven assessed screening and seven assessed treatment and follow-up. Twelve studies evaluated mistrust, five evaluated distrust, and three evaluated trust. Study populations included African American, American Indian, Latina, Hispanic, and Asian-American participants.
Conclusions:
Healthcare system distrust is prevalent across many different racial and ethnic groups and operates across the entire breast cancer continuum of care. It is an important yet understudied barrier to cancer. We hope that the knowledge garnered by this study will enable researchers to form effective and targeted interventions to reduce healthcare system distrust mediated disparities in breast cancer outcomes.
Keywords: Trust in healthcare system, breast cancer prevention, breast cancer treatment, racial/ethnic disparities
Introduction
Healthcare system distrust (HCSD) has been increasingly shown to be important to outcomes across the breast cancer continuum [1–6]. HCSD affects utilization of breast cancer preventive and screening services, treatment and post-treatment behaviors, and quality of life [1–3]. Breast cancer is one of the most common cancers in the United States [7], with a high survival rate (89.9% five-year survival in the United States) [8] and treatment trajectory that can span up to ten years [9,10]. Taken together, each patient will likely interact many times with the healthcare system across the breast cancer continuum of care, leaving many opportunities for HCSD to affect breast cancer outcomes. Given emerging information about the critical link between institutional trust and breast cancer outcomes, the present study aims to address the state-of-the science.
Trust, as it pertains to healthcare, has been conceptualized in a variety of ways across the literature. To enhance clarity, we provide definitions for terms related to trust. Institutional trust is defined as an individual’s belief in the competence and values of an institution [11, 12]. Healthcare system trust is considered a subset of institutional trust that specifically pertains to healthcare systems, including hospitals, community clinics, labs, insurance companies, and pharmaceutical companies [13]. By contrast, distrust is more than an absence of trust; it is a belief - informed by reliable knowledge or previous experiences - that the trusted party will not act in the trustee’s best interest [11,14]. Distrust occurs in relationships in which perceptions and expectations for action are directed toward an individual or organization that is being trusted [11, 15–17]. Mistrust is a distinct concept, although it is often used synonymously with distrust in the literature. It is a perception that does not find its basis in specific knowledge, but rather is rooted in a general sense of suspicion [14]. Acknowledging inconsistencies in usage of terms, we use healthcare system distrust to refer to both mistrust and distrust in the healthcare system. To completely assess the role of HCSD in the breast cancer continuum of care, we evaluated studies reporting on mistrust and distrust.
A brief review of the literature shows that most studies of distrust in the context of cancer have focused on interpersonal relationships; and more specifically on patient-physician relationships [11, 13, 18]. This narrowed focus yields an incomplete understanding of distrust and mistrust’s role in cancer care. Research has shown that institutional trust, such as healthcare system trust, has the strongest impact on people’s trust attitudes and behaviors. Additionally, although physician trust and healthcare system trust are correlated, an individual can display trust in one level and not the other [19,20]. Studies that focus solely on individual-level trust may miss the contribution of healthcare system distrust entirely, despite that it may be a contributor to gaps in breast cancer treatment and survivorship outcomes [21].
Many studies have shown that African -Americans/Blacks experience high levels of HCSD [22–27]. This likely stems in part from a legacy of oppression, historical experiences of slavery, and Jim Crow specific incidents of unethical treatment by the medical system (such as the Tuskegee Syphilis Study [28], and the forced sterilization of Black women in the 1970s [29]). Interestingly, recent studies suggest that distrust also operates among populations in the United States that do not share African Americans’ unique history of oppression, such as American Indians, Asian Americans and Hispanic/Latino men and women [30,31]. Considering that racial and ethnic differences in breast cancer prevention and outcomes are well documented [32–34], and that HCSD seems to affect breast cancer screening attitudes and treatment outcomes for racial and ethnic minorities [1–3], HCSD may be a significant yet understudied contributor to racial and ethnic disparities across the entire breast cancer continuum of care.
Considering the potential significance and prevalence of HCSD across the breast cancer continuum, this scoping review aims to (1) delineate the current understanding of HCSD across the breast cancer continuum, (2) to identify areas of the breast cancer continuum of care where distrust is most closely associated with poor patient outcomes, and (3) to identify which populations are most at risk. We will also address what is known and unknown about HCSD across population subgroups in the United States. As such, this review will serve as a platform from which to expand our understanding of distrust and mistrust’s role in the context of breast cancer care. Additionally, the findings of this study will enable researchers to develop effective and targeted interventions to reduce HCSD mediated disparities in breast cancer outcomes.
Methods
Consistent with the definition of a scoping study [35], we will examine the extent, range, and nature of research activity, summarize and disseminate research findings, and identify gaps in the existing literature on the topic of HCSD in the context of the breast cancer continuum. Review implementation was guided by a 5-step methodology for scoping reviews, as outlined by Kahlil et al., which consists of (1) identifying the research question, (2) identifying the relevant studies, (3) selecting the studies, (4) presenting the data, and (5) collating the results. As this is not a systematic review, we will not assess the methodological quality and rigor of the included studies. This work is intended to assess the breadth and depth of the spectrum of knowledge in these topical areas [35,36].
Study Selection
Articles were included if they met the following criteria: (1) published in a peer-reviewed journal or presented as an abstract at a scientific conference; (2) published or presented between January 1, 1990 and December 31, 2018; (3) measured mistrust, distrust, or trust qualitatively or quantitatively, either as a primary exposure or outcome of interest; (4) conducted in the United States; and (5) involved any part of the breast cancer continuum of care as the primary or a substantive focus of the article. Studies were restricted to the U.S. because trust attitudes vis-à-vis institutions are shaped by the history and framework of healthcare organizations, which are highly-specific to countries. The breast cancer continuum of care has historically encompassed education, screening, diagnosis, treatment, follow-up, and survivorship. However, in light of its emerging and growing relevance, we also included genetic testing and counseling. Mistrust, distrust and trust, as conceptualized in our introduction, are three related but distinct concepts and were treated as such.
Study Search
The following six databases were searched: CINAHL, Cochrane, EMBASE, PubMed, PsycINFO, and Web of Science. We used the search term “trust* OR distrust OR mistrust*” and “health facilities* OR delivery of healthcare* OR healthcare” to capture articles related to healthcare system trust, mistrust or distrust. The breast cancer continuum of care was captured using the following terms: “breast neoplasms*”, “mammography*”, “breast self-examination*”, “breast cancer screening”, “genes, brca1*”, “genes, brca2*”, “breast cancer genetic testing”, “breast cancer prevention”, “breast cancer AND survivorship* OR treatment”. Boolean logic and MeSH terms (as indicated by asterisks) were used as appropriate to maximize search results.
Study Screening
Once candidate articles were identified, titles and abstracts were screened by a single investigator (M.M.) using prespecified inclusion/exclusion criteria. The included full texts were then further reviewed by three independent investigators (M.M., L.D. and R.M.J.), and any conflict was resolved through general consensus.
Results
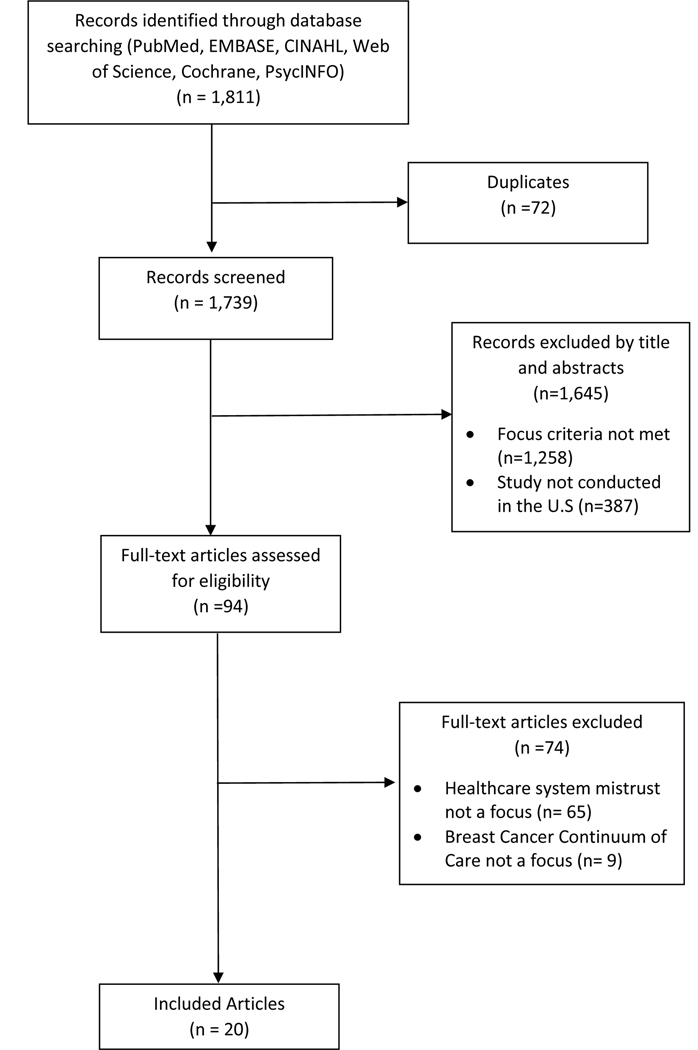
A total of 20 studies met all the prespecified inclusion criteria (Figure 1). The combined database searches yielded 1,811 results. Once duplicates were removed, 1,739 unique articles remained for title and abstract screening. Of those, 1,258 were excluded because they did not meet the prespecified focus criteria, 387 were excluded because the studies were not conducted in the United States, and the remaining 94 articles were retrieved for full text review. Subsequently, 65 articles were excluded because trust, distrust or mistrust were not a primary outcome or exposure of interest, and 9 were excluded because the breast cancer continuum of care did not represent a primary or substantive focus of the study (final n=20).
Figure 1.
PRISMA Flow Diagram for Inclusion of Studies
Qualitative Studies (Table 1)
Table 1.
Characteristics of Qualitative Studies of Healthcare System Distrust and Breast Cancer Care (n=7)
| Reference | Study Setting | Sample Characteristics | Type of Trust Measured | Data Collection Type | Main Findings |
|---|---|---|---|---|---|
| Screening (n=6) | |||||
| Ahmed et al. 2004 | Tennessee | 24 African-American and 1 White woman, 40+ | Trust | Focus group interviews | Trust is a key empowering factor in mammography adherence |
| Brandzel et al. 2016 | Seattle, WA | 39 Black and Latina women, 30 – 60 | Trust | Focus group interviews | Mistrust of the healthcare system is prevalent in Back and Latina women, stemming from historical trauma and cultural insensitivity |
| Canales et al. 2004 | Native communities in Vermont | 20 American Indian Women, 39 – 75 | Trust | Individual interviews | Healthcare system trust is a key factor in mammography adherence |
| Daley et al. 2012 | Rural communities in Kansas and Missouri | 84 American Indian women, 40+ | Mistrust | Focus group interviews | Mistrust of Western medicine primary barrier to mammography |
| Shelton et al. 2011 | Communities with high volume of low-income, multi-ethnic patients | 64 Black and Latina women, 40 + | Mistrust | Individual interviews | Black women expressed high levels of mistrust due to a history of oppression and abuse by the medical system |
| Thorburn et al. 2012 | Communities in Oregon | 83 Hmong men and women representing 12 out of 17 Oregon Hmong clans, 18+ | Mistrust | Focus group interviews | Participants did not identify medical mistrust as a major barrier to breast and cervical cancer screening |
| Treatment (n=1) | |||||
| Ferrera et al. 2015 | Communities in Chicago | 503, 96% African-American, men and women, 18–87 | Mistrust | Focus group interviews | Healthcare system mistrust towards breast cancer treatment was highly prevalent and identified as a significant barrier to care |
Seven qualitative studies were identified; six focused on breast cancer screening and one on breast cancer treatment. Researchers predominantly used focus group interviews (n=5), and all studies explored institutional trust as part of a broader conversation about “attitudes,”\ “beliefs,” or “perceptions” towards breast cancer care. Two research groups additionally opted to use conceptual framework guided interviews to enhance conversation; Ferrera et al. (2015) used Camara Jones’s theoretical framework on levels of racism, and Shelton et al. (2011) used the social contextual framework [37,38]. Apart from one study with 503 participants, study sample sizes ranged from 20 to 100 participants. All four U.S. Census Bureau regions were represented (Northeast=1, Midwest =2, South = 1, and West =2) and study settings evenly spanned urban (n=3) and rural (n=4) communities. Study populations were varied and included Black and Latina women (n=2), American Indian women in Vermont and South Dakota (n=2), exclusively Black women (n=1), Black men and women (n=1) and Hmong men and women (n=1). Historical trauma, lack of trust in Western Medicine, and cultural insensitivity were identified as common components of medical distrust. Complete results are presented in Table 1.
Quantitative Studies
Genetic Testing (Table 2.)
Table 2.
Characteristics of Quantitative Studies of Healthcare System Distrust and Breast Cancer Genetic Testing and Screening (n=7)
| Reference | Study Setting | Sample Characteristics | Type of Trust | Measure of Trust | Main Findings (in relation to higher mis/distrust) |
|---|---|---|---|---|---|
| Genetic Testing (n=2) | |||||
| Sheppard et al, 2013. | Cancer center and community in mid-Atlantic region | 100 African-American women, 21 + | Mistrust | Medical Mistrust Index (ɑ=0.69) | ↓ genetic counseling and testing engagement (B = −0.26, p<0.01) |
| Thompson et al, 2003 | Hospitals +community health centers in north Manhattan, New York | 273 Black, Latina and White women, 18 + | Mistrust | Group Based Medical Mistrust Scale | ↑ perceived disadvantages of genetic testing (p<0.0001) ↑ concerns about genetic testing abuses (p<0.0001) |
| Screening (n=5) | |||||
| Arnold et al. 2017 | Urban federally qualified health centers in Saint Louis, Missouri | subsample of 45 women, 40+ | Mistrust | Group Based Medical Mistrust Scale; (ɑ=0.88) | No significant difference in mistrust between women who adhered to mammography guidelines and those who did not (p=0.81). |
| Hong et al. 2018 | Korean churches in metropolitan Chicago | 196 Korean American women, 50 – 74 | Distrust | Revised Healthcare System Distrust Scale; (ɑ=0.83) | ↓ screening within the past 2 years (OR 0.84, 95% CI 0.72–0.99) |
| Katapodi et al. 2010 | Urban communities in a large west coast metropolitan area | 184 women 30 – 85 | Distrust | Study developed distrust in the healthcare system scale; (ɑ=0.71) | ↓ health services use (r = −0.26, p<0.001) and ↑ time since last clinical breast exam (p<0.05) |
| Molina et al. 2015 | 3 community hospitals Chicago, Illinois | 671 African- American women | Mistrust | Health Care System Distrust Scale (ɑ=0.71) | ↓ patient satisfaction of mammography services (B = −0.52, p< 0.0001) Mistrust-satisfaction relationship significantly mediated by healthcare self-efficacy (p=0.002) |
| Yang et al. 2011 | Philadelphia, Pennsylvania | 5268 women, 18 + | Distrust | Revised Healthcare System Distrust Scale | ↓ odds of having had a clinical breast examination in the past year (OR = 0.923, 95% CI = 0.864 – 0.986) |
This review identified two quantitative studies regarding trust and genetic counseling and testing (GC/T), the first published in 2002, and the second published in 2013. Both studies were cross-sectional, conducted in communities and medical centers in the Mid-Atlantic region of the United States, and both research teams measured medical mistrust. Thompson et al. used the Group Based Medical Mistrust Scale (GBMMS) [22] to estimate the association between mistrust and perceived disadvantage and concerns about abuse of GC/T in a study population of 273 Black, Latina and White women; no measure of scale reliability in the study population was reported. Other predictors of interest in this study included awareness of genetic testing and race/ethnicity. Alternatively, Sheppard et al. used the Medical Mistrust Index Scale [26] to measure the association between mistrust and GC/T engagement in a study population of 100 Black women only and reported a Cronbach’s alpha of 0.69. Other predictors of interest in this study included self-efficacy, and confidence in the Genetic Information Non-Discrimination Act of 2008, which prohibits employer and insurance discrimination based on genetic testing results [39,40]. Both studies reported a significant negative relationship between mistrust and GC/T.
Screening (Table 2.)
We identified five studies regarding breast cancer screening. Study outcomes included mammography adherence (n=2), clinical breast examination (CBE) adherence (n=1), both CBE and mammography adherence (n=1), as well as patient satisfaction with mammography services (n=1). All studies were conducted in large urban centers which included Chicago (n=2), Saint Louis (n=1), Philadelphia (n=1) and one unspecified large west coast metropolitan area. Study populations were varied with three studies enrolling women of any race/ethnicity, one including exclusively medically underserved Black women, and one consisting exclusively of Korean American women. Three studies measured distrust, two measured mistrust and none measured trust. Scales used include the Group Based Medical Mistrust Scale [22] (ɑ=0.88), the Healthcare System Distrust Scale [27] (ɑ=0.71), the revised Healthcare System Distrust Scale [9] (ɑ=0.83), as well as a study developed distrust in the healthcare system scale (ɑ=0.71) [3]. Two studies [41,42], one which used the Group Based Medical Mistrust Scale, and the other which used the revised Healthcare System Distrust Scale, did not report a measure of reliability. Four of the five studies identified found a significant negative relationship between either mistrust (n=2) or distrust (n=3) and screening. Arnold et al. was the only study that did not report a significant association between trust and screening, as they found no difference in mammography adherence between women with high and low levels of medical mistrust.
Treatment and follow-up (Table 3.)
Table 3.
Characteristics of Quantitative Studies of Healthcare System Distrust and Breast Cancer Treatment and Follow-up (n=6)
| Reference | Study Setting | Sample Characteristics | Type of Trust Measured | Measure of Trust | Main Findings (in relation to higher mis/distrust) |
|---|---|---|---|---|---|
| Barsevick et al; 2016 | Pennsylvania cancer registries | 297 African American women treated for primary breast cancer, 18+ | Mistrust | Group Based Medical Mistrust Scale | ↑ emotional problems (p<0.0001), ↑ physical problems (p=0.007), ↑ resource problems (p<0.0001) and ↑ sexual problems (p=0.002) |
| Bickell et al; 2009 | Six New York City hospitals | 258 White, Black, Hispanic and Asian women with stage I or II breast cancer | Mistrust | Study adaptation of Medical Mistrust Index (ɑ=0.66) | Untreated women had ↑ medical mistrust (aRR = 1.003, 95% CI: 1.00 to 1.007) |
| Dean et al; 2017 | Pennsylvania and Florida cancer registries | 2,754 women with localized breast cancer, <65 | Distrust | Revised Health Care System Distrust Scale (ɑ=0.84) | ↑ treatment discordance (OR = 1.22, p=0.03). Physician distrust not a mediator between HCSD and treatment discordance (p=0.49) |
| Jiang et al; 2016 | Urban cancer centers in Ohio + Pennsylvania | 101 African-American women recommended for chemotherapy | Distrust | Health Care System Distrust Scale | ↓belief in the necessity of chemotherapy. No association with knowledge of tumor/chemotherapy |
| Maly et al; 2008 | Los Angeles | 257 Black, Latina and White women, diagnosed + treated for breast cancer, 55+ | Mistrust | Study created racism/medical mistrust measure (ɑ=0.67) | ↓ quality of life (p < 0.001), ↓ breast cancer knowledge (p<0.01), ↑ breast cancer stage (p<0.05) |
| Sutton et al; 2018. | Medical centers in D.C. and Detroit | 210 Black women | Mistrust | Group Based Medical Mistrust Scale; (ɑ=0.55) | ↓ radiation communication ratings (p <0.01) |
Six of the included studies assessed breast cancer treatment and follow-up. Reported outcomes were varied and included adjuvant treatment utilization (n=2), treatment discordance (n=1), beliefs in chemotherapy and knowledge of cancer treatment (n=1), quality of life and surgery type (n=1), as well as patient satisfaction (n=1). Five different scales were used: the Group Based Medical Mistrust Scale (GBMMS) [22] (ɑ=0.55), the Healthcare System Distrust Scale[27], the revised Healthcare System Distrust Scale [9] (ɑ=0.84), an adaptation of the Medical Mistrust Index [26] (ɑ=0.66), and a study-designed racism/medical mistrust measure (ɑ=0.67) [43]. Two studies failed to report a measure of internal consistency reliability [1,44]. Independent variables commonly measured alongside distrust/mistrust included physician communication (n=3), trust in physician (n=2), and self-efficacy (n=2). All of the included studies identified a negative relationship between mistrust/distrust and treatment/follow-up.
Discussion
In this scoping review, we summarized the literature on HCSD within the context of the breast cancer continuum of care. We identified 20 qualitative and quantitative studies that met inclusion criteria. This review provides evidence that: (1) trust facilitates access to breast cancer screening, and (2) mistrust and distrust negatively impact care across the breast cancer continuum. None of the studies showed a positive association between distrust/mistrust and care and only two studies reported no association between mistrust and care. Based on our synthesis and analysis of the studies, we report findings and gaps in what is known about healthcare system distrust across the breast cancer care continuum.
The Continuum of Care
Our results confirmed a research emphasis on distrust at the time of breast cancer screening, most evident in qualitative studies, where all but one of the included articles centered around screening practices. The majority of quantitative studies also focused on screening. However, recent studies have shown that distrust operates in areas other than screening, including genetic testing and counseling [42,45], treatment [2,46], and survivorship [2,47]. As such, a lack of qualitative and quantitative studies outside of screening practices suggests that we may have an incomplete understanding of HCSD’s components and role across the breast cancer continuum. Future distrust research should include qualitative studies, mixed-method and quantitative studies that span the entire breast cancer continuum of care.
Defining Trust
This review highlighted definitional inconsistency regarding terms related to the concept of trust, particularly mistrust and distrust. These two terms, while correlated, represent distinct concepts in that distrust is the belief that a trustee will act against one’s interests based on reliable knowledge or experience, whereas mistrust is a belief based on a general sense of suspicion, not rooted in previous experiences or on specific knowledge [14,27]. Mistrust and distrust are often used interchangeably, limited the conceptual clarity of these terms. A notable example of this definitional ambiguity is the GBMMS, a scale used by nearly one-third of the quantitative papers in this review. GBMMS is called an assessment of “the tendency to distrust” individuals or institutions outside one’s racial/ethnic group based on “a legacy of racism or unfair treatment” [22], but would more precisely be characterized as a scale assessing distrust.
The lack of precision in defining and conceptualizing trust and related terms is widespread. Within health sciences alone trust has been conceptualized in a variety of ways including: competence, control and agency [48], cooperation and compliance [49], vulnerability [50], and competence and value [13]. As this field grows, it may benefit researchers to simply acknowledge the complexity of defining trust and to clearly identify which conceptualization of the term they are using, allowing their study definition to guide measurement tool selection.
Measuring Mistrust and Distrust
All of the included quantitative studies measured either mistrust or distrust using multi-item Likert-type scales. While we identified six different validated scales, the following four were most commonly used: the Group Based Medical Mistrust Scale (GBMMS) [22], the Healthcare System Distrust Scale (HSDS) [27], the revised Healthcare System Distrust Scale [9], and the Medical Mistrust Index (MMI) [28] aligning with findings of a recent systematic review of “medical mistrust measures” [51].
We did not observe preferential use of a particular scale by study population or breast cancer continuum area. However, each instrument assesses different dimensions of trust, mistrust, or distrust. While the GBMMS, HSDS, revised HSDS and MMI can all be broadly referred to as medical mistrust/distrust scales, they assess different dimensions of trust. The GBMMS consists of three subscales that measure “suspicion, perceived discrimination and group-based disparities in healthcare settings, and lack of support” [22]. The revised HSDS is broken down into a “value” and a “competence” subscale [13]. The HSDS consists of one scale which assesses “competence, confidentiality, honesty, and fidelity” [27]. The MMI also consists of a single scale, and broadly measures mistrust in the “medical care system” [5,26].
The majority of included studies reported Cronbach’s alpha as a measure of scale reliability. Due to the small number of included studies, our sample size for any given scale is small, however, our results suggest that there is no meaningful difference in scale reliability across racial/ethnic groups. We do note that out of the 13 quantitative studies identified in our review, four did not report any measure of distrust/mistrust scale reliability.
In future research, we recommend that researchers consider these important scale differences and provide a rationale for tool selection. Additionally, scale reliability should consistently be reported.
Study Populations
We observed a strong research emphasis on HCSD and breast cancer care in Black women. This is an understandable focus as Black women have a well-documented history of oppression at the hands of U.S. institutions [29]. Interestingly, though rates of breast cancer in men are comparatively smaller than among women (70–100 times lower) [52], none of the studies identified in this review assessed HCSD and breast cancer in men. Although two studies did include men in their study population [53,54], their inclusion was meant to provide further insight into perspectives and attitudes of a particular racial/ethnic group on breast cancer care in women of that particular group. No studies looked at HCSD alongside breast cancer care in male patients. We also note the exclusion of Pacific Islander and Arab-American women as well as sexual and gender minority groups; these populations experience high levels of discrimination and/or medical mistrust [55–60] and may have high levels of HCSD. Additionally, few studies included White women. Although White women have high rates of breast cancer screening and experience better breast cancer outcomes than racial/ethnic minorities, socio-economic disparities in breast cancer health exist within this group[61]. Thus, HCSD among under- or uninsured and low-income White women should be investigated.
Our results suggest that distrust and mistrust operate differently across different racial and ethnic groups. While the majority of included populations reported experiencing high levels of perceived discrimination and cultural insensitivity, American Indian and Hmong women were the only groups to identify “lack of trust in Western Medicine” as a significant barrier to care [52,62,63]. This suggests that some distrust mechanisms may be specific to particular racial and ethnic groups, and may relate to immigrant status. However, medical distrust/mistrust scales have been predominantly developed and validated in Black and Hispanic/Latinx populations [51]. Considering this, it may be important for researchers to validate commonly used trust scales in a variety of racial and ethnic groups.
Limitations
Inherent to the nature of a scoping review, our study did not assess the quality of the included studies. However, we were able to assess the breadth and depth of knowledge regarding trust, mistrust and distrust’s role in the breast cancer continuum of care and identified important gaps in the literature [35,36]. Additionally, it is possible that this review may not have identified all studies related to healthcare system distrust and the breast cancer continuum of care. For example, we did not review reports not published in the peer-reviewed literature given that there was no sampling frame for identifying them. Google Scholar, due to the proprietary nature of its search algorithm, the lack of reproducibility and vetting of its search results, and its inclusion of predatory journals [64], was also omitted. Despite these exclusions, our search protocol included six different major databases of indexed and peer-review articles, and reference lists of included studies will also be examined for additional study selection. As such we believe that our scoping review yielded comprehensive results. Finally, studies conducted outside of the United States were excluded, which may limit the generalizability of our results to other countries. This geographic exclusion was motivated by the unique structure of the United States healthcare system as well as the fact that trust attitudes vis-à-vis institutions are shaped by the history and framework of these organizations. This suggests that distrust relationships, inherent to their development, may be unique to a country.
Conclusions
In this scoping review to examine the role of healthcare system distrust in the breast cancer continuum of care, our findings suggest that distrust and mistrust significantly negatively impact all aspects of the breast continuum and operate in many different racial and ethnic groups. Given that the literature focuses on screening, we encourage further research to span the entire breast cancer continuum, and to include men, a variety of racial/ethnic and socio-economic groups, and sexual and gender minority populations. We noted a lack of definitional consistency in the literature regarding trust terms, and recommend that future research clearly define what level and form of trust they are investigating. We further advise researchers to let their specification of trust guide study tool selection. Adopting these recommendations will allow for a more complete understanding of healthcare system distrust’s role in the breast cancer continuum of care and better enable us to address its effects on breast cancer care.
Supplementary Material
Acknowledgments
Funding: This work was supported by the National Cancer Institute grant K01CA184288; the National Institute of Mental Health grant R25MH083620; the Sidney Kimmel Cancer Center grant P30CA006973, and the National Heart, Lung and Blood Institute Pharmacoepidemiology training grant 1T32HL139426-1.
Footnotes
Compliance with Ethical Standards:
Ethics: This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent: As this article did not contain any studies with human participants or animals performed by any of the authors informed consent was not required.
Conflict of Interest: The authors declare that they have no conflict of interest
References
- 1.Barsevick AM, Leader A, Bradley PK, et al. (2016) Post-treatment problems of African American breast cancer survivors. Support Care Cancer. 24(12):4979–4986. doi: 10.1007/s00520-016-3359-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dean LT, Moss SL, McCarthy AM, Armstrong K (2017) Healthcare system distrust, physician trust, and patient discordance with adjuvant breast cancer treatment recommendations. Cancer Epidemiol Biomark Prev 26(12):1745–1752. doi: 10.1158/1055-9965.EPI-17-0479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Katapodi MC, Pierce PF, Facione NC (2010) Distrust, predisposition to use health services and breast cancer screening: results from a multicultural community-based survey. Int J Nurs Stud 47(8):975–983. doi: 10.1016/j.ijnurstu.2009.12.014 [DOI] [PubMed] [Google Scholar]
- 4.King WD. (2003) Examining African Americans’ mistrust of the health care system: expanding the research question. Public Health Rep 118(4):366–367. doi: 10.1016/S0033-3549(04)50263-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.LaVeist TA, Isaac LA, Williams KP (2009) Mistrust of health care organizations is associated with underutilization of health services. Health Serv Res 44(6):2093–2105. doi: 10.1111/j.1475-6773.2009.01017.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Scheppers E (2006) Potential barriers to the use of health services among ethnic minorities: a review. Fam Pract 23(3):325–348. doi: 10.1093/fampra/cmi113 [DOI] [PubMed] [Google Scholar]
- 7.Tao Z, Shi A, Lu C, Song T, Zhang Z, Zhao J (2015) Breast cancer : epidemiology and etiology. Cell Biochem Biophys 72(2):333–338. doi: 10.1007/s12013-014-0459-6 [DOI] [PubMed] [Google Scholar]
- 8.Howlader N, Noone AM, Krapcho M, Miller D, Brest A, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds) (2019) SEER Cancer Statistics Review, 1975–2016. National Cancer Institute, Bethesda, MD: https://seer.cancer.gov/csr/1975_2016/. Accessed 8 January 2020 [Google Scholar]
- 9.Goss PE, Ingle JN, Pritchard KI et al. (2016) Extending aromatase-inhibitor adjuvant therapy to 10 years. N Engl J Med 375:209–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burstein HJ, Temin S, Anderson H et al. (2014) Adjuvant endocrine therapy for women with hormone receptor-positive breast cancer: American Society of Clinical Oncology practice guideline focused updated. J Clin Oncol 32(21):2255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Armstrong K, Rose A, Peters N, Long JA, McMurphy S, Shea JA (2006) Distrust of the health care system and self-reported health in the United States. J Gen Intern Med 21(4):292–297. doi: 10.1111/j.1525-1497.2006.00396.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hovland CI, Janis IL, Kelley HH. (1953) Communication and persuasion. New Haven, CT, US: Yale University Press. [Google Scholar]
- 13.Shea JA, Micco E, Dean LT, McMurphy S, Schwartz JS, Armstrong K (2008) Development of a revised Health Care System Distrust Scale. J Gen Intern Med 23(6):727–732. doi: 10.1007/s11606-008-0575-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smirnoff M, Wilets I, Ragin DF, et al. (2018) A paradigm for understanding trust and mistrust in medical research: The Community VOICES study. AJOB Empir Bioeth 9(1):39–47. doi: 10.1080/23294515.2018.1432718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goold SD (2002) Trust, distrust and trustworthiness. J Gen Intern Med 17(1):79–81. doi: 10.1046/j.1525-1497.2002.11132.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hardin R (2001) Conceptions and explanations of trust In: Trust in Society. Russell Sage foundation series on trust, vol. 2 New York, NY, US: Russell Sage Foundation, pp 3–39. [Google Scholar]
- 17.Heimer CA (2001) Solving the problem of trust. Trust Soc 40–88. [Google Scholar]
- 18.Hall MA (2006) Researching medical trust in the United States. Calnan M, ed. J Health Organ Manag 20(5):456–467. doi: 10.1108/14777260610701812 [DOI] [PubMed] [Google Scholar]
- 19.Calnan M, Rowe R, Entwistle V (2006) Trust relations in health care: an agenda for future research. J Health Organ Manag 20(5):477–484. doi: 10.1108/14777260610701830 [DOI] [PubMed] [Google Scholar]
- 20.Blendon RJ, Benson JM (2001) Americans’ views on health policy: A Fifty-Year Historical Perspective. Health Affb 20(2):33–46. doi: 10.1377/hlthaff.20.2.33 [DOI] [PubMed] [Google Scholar]
- 21.Kawachi I, Kennedy BP, Glass R (1999) Social capital and self-rated health: a contextual analysis. Am J Public Health 89(8):1187–1193. doi: 10.2105/AJPH.89.8.1187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thompson HS, Valdimarsdottir HB, Winkel G, Jandorf L, Redd W (2004) The Group-Based Medical Mistrust Scale: psychometric properties and association with breast cancer screening. Prev Med 38(2):209–218. doi: 10.1016/j.ypmed.2003.09.041 [DOI] [PubMed] [Google Scholar]
- 23.Boulware LE, Cooper LA, Ratner LE, LaVeist TA, Powe NR (2003) Race and trust in the health care system. Public Health Rep 118(4):358–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Corbie-Smith G, Thomas SB, St George DMM (2002) Distrust, race, and research. Arch Intern Med 162(21):2458–2463. doi: 10.1001/archinte.162.21.2458 [DOI] [PubMed] [Google Scholar]
- 25.Gamble VN (1997) Under the shadow of Tuskegee: African Americans and health care. Am J Public Health 87(11):1773–1778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.LaVeist TA, Nickerson KJ, Bowie JV (2000) Attitudes about racism, medical mistrust, and satisfaction with care among African American and white cardiac patients. Med Care Res Rev 257(1):146–161. doi: 10.1177/1077558700057001S07 [DOI] [PubMed] [Google Scholar]
- 27.Rose A, Peters N, Shea JA, Armstrong K (2004) Development and testing of the Health Care System Distrust Scale. J Gen Intern Med 19(1):57–63. doi: 10.1111/j.1525-1497.2004.21146.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thomas SB, Quinn SC (1991) The Tuskegee Syphilis Study, 1932 to 1972: implications for HIV education and AIDS risk education programs in the black community. Am J Public Health 81(11):1498–1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Williams K, Johnson VW (2002) Eliminating African-American health disparity via history-based policy. Harvard Health Policy Review. 3(2). [Google Scholar]
- 30.Guadagnolo BA, Cina K, Helbig P, et al. (2009) Medical mistrust and less satisfaction with health care among Native Americans presenting for cancer treatment. J Health Care Poor Underserved 20(1):210–226. doi: 10.1353/hpu.0.0108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hong Y-R, Tauscher J, Cardel M (2018) Distrust in health care and cultural factors are associated with uptake of colorectal cancer screening in Hispanic and Asian Americans. Cancer 124(2):335–345. doi: 10.1002/cncr.31052 [DOI] [PubMed] [Google Scholar]
- 32.Bigby J, Holmes MD (2005) Disparities across the breast cancer continuum. Cancer Causes Control 16(1):35–44. doi: 10.1007/s10552-004-1263-1 [DOI] [PubMed] [Google Scholar]
- 33.Lannin DR, Mathews HF, Mitchell J, Swanson MS (2002) Impacting cultural attitudes in African-American women to decrease breast cancer mortality. Am J Surg 184(5):418–423. doi: 10.1016/S0002-9610(02)01009-7 [DOI] [PubMed] [Google Scholar]
- 34.McCarthy EP (1998) Mammography use helps to explain differences in breast cancer stage at diagnosis between older Black and White women. Ann Intern Med 128(9):729. doi: 10.7326/0003-4819-128-9-199805010-00005 [DOI] [PubMed] [Google Scholar]
- 35.Levac D, Colquhoun H, O’Brien KK (2010) Scoping studies: advancing the methodology. Implement Sci 5:69. doi: 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Khalil H, Peters M, Godfrey CM, McInerney P, Soares CB, Parker D (2016) An Evidence-based approach to scoping reviews. Worldviews Evid Based Nurs 13(2):118–123. doi: 10.1111/wvn.12144 [DOI] [PubMed] [Google Scholar]
- 37.Jones CP (2000) Levels of racism: a theoretic framework and a gardener’s tale. Am J Public Health 90(8):1212–1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sørensen K, Van den Broucke S, Fullam J, et al. (2012) Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 12(1):80. doi: 10.1186/1471-2458-12-80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Honey K (2008) GINA: making it safe to know what’s in your genes. J Clin Invest. 118(7):2369. doi: 10.1172/JCI36366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Genetic Discrimination. Genome.gov. https://www.genome.gov/about-genomics/policy-issues/Genetic-Discrimination. Accessed September 30, 2019.
- 41.Yang T-C, Matthews SA, Hillemeier MM (2011) Effect of health care system distrust on breast and cervical cancer screening in Philadelphia, Pennsylvania. Am J Public Health 101(7):1297–1305. doi: 10.2105/AJPH.2010.300061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Thompson HS, Valdimarsdottir HB, Jandorf L, Redd W (2003) Perceived disadvantages and concerns about abuses of genetic testing for cancer risk: differences across African American, Latina and Caucasian women. Patient Educ Couns 51(3):217–227. doi: 10.1016/s0738-3991(02)00219-7 [DOI] [PubMed] [Google Scholar]
- 43.Maly RC, Stein JA, Umezawa Y, Leake B, Anglin MD (2008) Racial/ethnic differences in breast cancer outcomes among older patients: effects of physician communication and patient empowerment. Health Psychol 27(6):728–736. doi: 10.1037/0278-6133.27.6.728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jiang Y, Sereika SM, Bender CM, Brufsky AM, Rosenzweig MQ (2016) Beliefs in chemotherapy and knowledge of cancer and treatment among African American women with newly diagnosed breast cancer. Oncol Nurs Forum. 2016;43(2):180–189. doi: 10.1188/16.ONF.180-189 [DOI] [PubMed] [Google Scholar]
- 45.Hann KEJ, Freeman M, Fraser L, et al. (2017) Awareness, knowledge, perceptions, and attitudes towards genetic testing for cancer risk among ethnic minority groups: a systematic review. BMC Public Health 17(1):503. doi: 10.1186/s12889-017-4375-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bickell NA, Weidmann J, Fei K, Lin JJ, Leventhal H (2009) Underuse of breast cancer adjuvant treatment: patient knowledge, beliefs, and medical mistrust. J Clin Oncol Off J Am Soc Clin Oncol 27(31):5160–5167. doi: 10.1200/JCO.2009.22.9773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cavanagh BM, Wakefield CE, McLoone JK, Garvey G, Cohn RJ (2016) Cancer survivorship services for indigenous peoples: where we stand, where to improve? A systematic review. J Cancer Surviv 10(2):330–341. doi: 10.1007/s11764-015-0479-2 [DOI] [PubMed] [Google Scholar]
- 48.Mechanic D, Schlesinger M (1996) The impact of managed care on patients’ trust in medical care and their physicians. JAMA 275(21):1693–1697. [PubMed] [Google Scholar]
- 49.Dibben MR, Morris SE, Lean ME (2000) Situational trust and co-operative partnerships between physicians and their patients: a theoretical explanation transferable from business practice. QJM 93(1):55–61. doi: 10.1093/qjmed/93.1.55 [DOI] [PubMed] [Google Scholar]
- 50.Hall MA, Dugan E, Zheng B, Mishra AK (2001) Trust in physicians and medical institutions: what is it, can it be measured, and does it matter? Milbank Q 79(4):613–639. doi: 10.1111/1468-0009.00223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Williamson LD, Bigman CA (2018) A systematic review of medical mistrust measures. Patient Educ Couns 101(10):1786–1794. doi: 10.1016/j.pec.2018.05.007 [DOI] [PubMed] [Google Scholar]
- 52.Key Statistics for Breast Cancer in Men. https://www.cancer.org/cancer/breast-cancer-in-men/about/key-statistics.html. Accessed October 21, 2019.
- 53.Thorburn S, Kue J, Keon KL, Lo P (2012) Medical mistrust and discrimination in health care: a qualitative study of Hmong women and men. J Community Health 37(4):822–829. doi: 10.1007/s10900-011-9516-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ferrera MJ, Feinstein RT, Walker WJ, Gehlert SJ (2016) Embedded mistrust then and now: findings of a focus group study on African American perspectives on breast cancer and its treatment. Crit Public Health 26(4):455–465. doi: 10.1080/09581596.2015.1117576 [DOI] [Google Scholar]
- 55.Sorkin DH, Ngo-Metzger Q, De Alba I (2010) Racial/ethnic discrimination in health care: impact on perceived quality of care. J Gen Intern Med 25(5):390–396. doi: 10.1007/s11606-010-1257-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Brenick A, Romano K, Kegler C, Eaton LA (2017) Understanding the influence of stigma and medical mistrust on engagement in routine healthcare among Black women who have sex with women. LGBT Health 4(1):4–10. doi: 10.1089/lgbt.2016.0083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Eaton LA, Driffin DD, Kegler C, et al. (2015) The Role of stigma and medical mistrust in routine health care engagement of Black men who have sex with men. Am J Public Health 105(2):e75–e82. doi: 10.2105/AJPH.2014.302322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Samari G (2016) Islamophobia and public health in the United States. Am J Public Health 106(11):1920–1925. doi: 10.2105/AJPH.2016.303374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Shah SM, Ayash C, Pharaon NA, Gany FM (2008) Arab American immigrants in New York: health care and cancer knowledge, attitudes, and beliefs. J Immigr Minor Health 10(5):429–436. doi: 10.1007/s10903-007-9106-2 [DOI] [PubMed] [Google Scholar]
- 60.Dean L, Meyer IH, Robinson K, et al. (2000) Lesbian, gay, bisexual, and transgender health: findings and concerns. J Gay Lesbian Med Assoc 4(3):102–151. doi: 10.1023/A:1009573800168 [DOI] [Google Scholar]
- 61.Sabatino SA, Coates RJ, Uhler RJ, Breen N, Tangka F, Shaw KM (2008) Disparities in mammography use among US women aged 40–64 Years, by race, ethnicity, income, and health insurance status, 1993 and 2005. Med Care 46(7):692. doi: 10.1097/MLR.0b013e31817893b1 [DOI] [PubMed] [Google Scholar]
- 62.Daley CM, Kraemer-Diaz A, James AS, et al. (2012) Breast cancer screening beliefs and behaviors among American Indian women in Kansas and Missouri: a qualitative inquiry. J Cancer Educ 27(1 Suppl):S32–40. doi: 10.1007/s13187-012-0334-3 [DOI] [PubMed] [Google Scholar]
- 63.Canales MK, Geller BM (2004) Moving in between mammography: screening decisions of American Indian women in Vermont. Qual Health Res 14(6):836–857. doi: 10.1177/1049732304265845 [DOI] [PubMed] [Google Scholar]
- 64.Coiffait L. Criticisms of the Citation System, and Google Scholar in Particular – Social Science Space. https://www.socialsciencespace.com/2019/03/criticisms-of-the-citation-system-and-google-scholar-in-particular/. Accessed October 16, 2019.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.