Abstract
Background:
Given the superiority of meniscal repair over partial meniscectomy according to biomechanical data, the clinical outcomes of meniscal repair are likely to be better than those of partial meniscectomy for a medial meniscus root tear (MMRT).
Purpose/Hypothesis:
This review was designed to compare the clinical and radiological results between meniscal repair and partial meniscectomy for MMRTs. It was hypothesized that meniscal repair would result in better clinical and radiological results compared with partial meniscectomy.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
Studies were included in the review if they (1) included patients with MMRTs who underwent primary arthroscopic meniscal repair or partial meniscectomy and (2) analyzed validated patient-reported outcomes and/or radiological evaluations. Summary odds ratios (ORs) with 95% CIs were calculated to compare partial meniscectomy with meniscal repair for each outcome.
Results:
A total of 13 studies were included. The mean duration of follow-up was 33.5 and 47.2 months in the meniscal repair group and partial meniscectomy group, respectively. The change in the Lysholm score from preoperatively to postoperatively was statistically significantly in favor of meniscal repair (OR, 2.20 [95% CI, 1.55-3.12]), while no difference was found with respect to the change in the Tegner score between the 2 surgical approaches (OR, 1.21 [95% CI, 0.65-2.24]). The prevalence of postoperative severe knee osteoarthritis (OR, 0.31 [95% CI, 0.17-0.54]) as well as that of reoperations (OR, 0.05 [95% CI, 0.01-0.19]) were significantly in favor of meniscal repair.
Conclusion
Better outcomes were seen after meniscal repair compared with partial meniscectomy for MMRTs, with greater improvements in Lysholm scores, and lower rates of progression to knee osteoarthritis, and lower reoperation rate.
Keywords: medial meniscus, root tear, repair, partial meniscectomy
There are 2 types of medial meniscus root tears (MMRTs).14,25,28,33 One is a trauma-related avulsion injury that occurs just at the attachment site of the insertional ligament of the meniscus root in the posterior aspect of the proximal tibia, which is rare and usually arises in younger patients. The other, more common type is a degenerative MMRT, which is related to knee osteoarthritis in elderly patients and usually occurs farther away from the meniscal insertional ligament site, thus leaving the meniscal stump in the meniscal horn area. Although nonoperative treatment of degenerative MMRTs is effective in the short term, unsatisfactory results and the abrupt progression of knee osteoarthritis in the medial compartment have also been often reported.21,22 Therefore, surgeons have tried to repair MMRTs to restore the hoop strain in the meniscus with various techniques. However, the results of meniscal repair for MMRTs are not always promising because of the technical demands of the repair procedure as well as the decreased healing potential due to degenerative changes in the meniscal stump and tear margin.17
Partial meniscectomy has also been performed in patients with degenerative MMRTs and the symptom of a locking knee long before meniscal repair. Judging by the superiority of meniscal repair over partial meniscectomy as seen from the biomechanical data,11,32,36 the clinical outcomes of meniscal repair are likely to be better than those of partial meniscectomy. Nevertheless, few studies have directly compared the results between meniscal repair and partial meniscectomy in patients with MMRTs. Additionally, most advocates for either meniscal repair or partial meniscectomy for MMRTs have based their suggestions on anecdotal experience; however, there is a lack of systematic reviews and meta-analyses comparing these 2 surgical modalities. Therefore, this systemic review and meta-analysis was designed to compare the clinical and radiological results between meniscal repair and partial meniscectomy for MMRTs. It was hypothesized that meniscal repair would result in better clinical and radiological results than partial meniscectomy.
Methods
Literature Search
The study design was based on Cochrane Review Methods. In accordance with the guidelines of the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement, multiple comprehensive literature databases, including PubMed, Embase, Cochrane Library, Ovid MEDLINE, and Scopus, were searched for studies that evaluated clinical outcomes in patients with MMRTs who underwent arthroscopic surgery either with meniscal repair or partial meniscectomy. There were no restrictions on language or year of publication. Search terms used in the title, abstract, Medical Subject Headings, and keywords fields included the following: (menisci, tibial, OR meniscus) AND (tibial meniscus injuries OR menisc* tear) AND (posterior OR posterior horn OR radial tear OR root tear) AND (meniscectomy OR menisc* repair).
Study Selection
Two reviewers (K.H.-R., J.-H.K.) evaluated the titles and abstracts of the retrieved articles and selected relevant studies for a full review. If the abstract did not provide sufficient data to make a decision, the complete article was reviewed. Studies were included in the systematic review if they (1) included patients with MMRTs who underwent primary arthroscopic meniscal repair or partial meniscectomy and (2) analyzed validated patient-reported outcomes and/or radiological evaluations. Biomechanical and cadaveric studies, technical notes, letters to the editor, expert opinions, review articles, meta-analyses, scientific conference abstracts, and case reports were excluded. Additional exclusion criteria included studies with cohorts that underwent arthroscopic meniscal repair without using the transtibial pullout repair technique, such as repair with suture anchors, so as to minimize heterogeneity, because the pullout repair technique has been widely used and studies of the suture anchor repair technique were lacking.34,37 In assessing and organizing pooled studies, the country and city of the hospital or institution at which arthroscopic surgery was performed, as well as the operating surgeon’s name and the evaluation period, were checked to exclude duplicate cohorts of patients. If the same patient cohort was evaluated in more than 1 study, the latest study with the longest follow-up period was included.
Data Extraction
Again, 2 investigators (K.-H.R., J.-H.K.) independently extracted data from each study using a predefined data extraction form. Any disagreements unresolved by a discussion were settled by a third investigator (D.-H.L.) if needed. The clinical outcomes of interest included Lysholm knee score, International Knee Documentation Committee (IKDC) score, and Tegner activity score. Other outcomes included radiological results such as medial joint-space narrowing, the progression of the Kellgren-Lawrence (K-L) grade postoperatively compared with preoperatively, and the rate of reoperations after arthroscopic surgery.
Assessment of Methodological Quality
The 2 reviewers independently evaluated each study using the MINORS (Methodological Index for Non-Randomized Studies) checklist,40 which is an instrument designed to assess the methodological quality of nonrandomized surgical studies, both comparative and noncomparative. On this checklist, the maximum scores are 24 for comparative studies and 16 for noncomparative studies. Furthermore, the MINORS has external validity to assess the qualities of randomized trials as well as nonrandomized studies. Any unresolved disagreements between the reviewers were resolved by a consensus with a third independent reviewer (D.-H.L.).
Statistical Analysis
For subgroup meta-analyses, continuous variables such as the Lysholm knee score, Tegner activity score, IKDC score, and medial joint-space narrowing were extracted as means and standard deviations. When these variables were not mentioned in the articles, the study authors were contacted by email with a request for the data. Missing standard deviations were calculated from the data according to the following formula: for sample sizes ≤70: range(upper range value – lower range value)/4, and for sample sizes >70: range(upper range value – lower range value)/6.13 Binary outcomes were pooled as percentages, and the total numbers from each study and odds ratios (ORs) were calculated using a 2 × 2 contingency table (George Mason University). Weighted estimates and standard errors were calculated using R statistical software Version 3.4.0 (“metafor” Meta-Analysis Package for R; R Foundation for Statistical Computing)12 and OpenMeta[Analyst] (Brown University).41 The standardized mean difference and standardized variance were calculated from the weighted estimate, standard error, and sample size of each cohort with the use of the logit method.42 Summary ORs and 95% CIs were calculated from the standardized mean difference and standardized variance (George Mason University).
Results
Identification of Studies
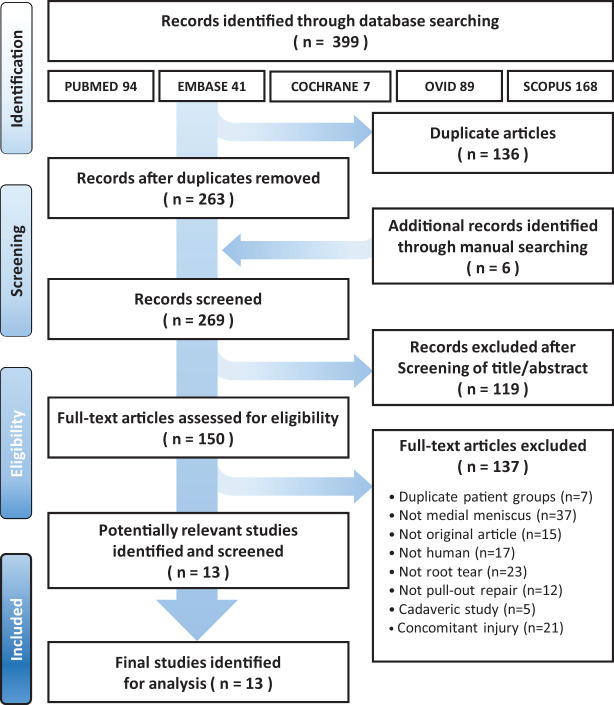
An electronic search of the PubMed, Embase, Cochrane Library, Ovid (Ovid MEDLINE, Ovid MEDLINE Daily, Ovid MEDLINE In-Process & Other Non-Indexed Citations), and Scopus databases yielded 399 studies (Figure 1). After excluding 136 duplicates, 263 studies remained. Of these, 119 were excluded based on the titles and abstracts after 6 additional publications were identified through manual searching. After reading the complete texts of the remaining 150 articles, 137 were excluded through our study selection criteria. Ultimately, 13 studies were included in this systematic review.
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram for the identification and selection of studies included in this meta-analysis.
Study Characteristics, Quality, and Patient Populations
The 14 cohorts of the 13 included studies consisted of 227 knees (8 cohorts) that underwent meniscal repair and 308 knees (6 cohorts) that underwent partial meniscectomy. Overall, 3 studies compared the outcomes of meniscal repair or partial meniscectomy with those of nonoperative treatment, and 3 studies compared the results of meniscal repair with those of a different technique or laterality. Each of the 13 studies reported the results of meniscal repair or partial meniscectomy. Only 1 study7 directly compared the results of meniscal repair with those of partial meniscectomy. The demographic data, study design, follow-up period, and quality score (MINORS) of each included study are presented in Appendix Table A1. The median MINORS score for comparative studies was 18.5 of 24, whereas that of noncomparative studies was 8.5 of 16. In terms of the meniscal repair group, all repair procedures were performed using the pullout suture method with a transtibial tunnel. Details of the surgical technique, such as the suture material, number and location of tibial tunnels, and tibial fixation method, as well as the rehabilitation protocol, are described in Table 1. A total of 6 parameters regarding clinical and radiological outcomes were compared between the 2 surgical approaches: improvements in Lysholm, IKDC, and Tegner scores, plus medial joint-space narrowing, progression of K-L grade, and reoperation rate. Improvement in the IKDC score and change in medial joint-space narrowing were not pooled because only 1 study reported IKDC score improvements from preoperatively and postoperatively as well as changes in medial joint-space narrowing for partial meniscectomy.
Table 1.
Surgical Techniques and Rehabilitation Protocols of Meniscal Repair Studiesa
| Lead Author (Year) | No. of Knees | Suture Technique | Suture Material | No./Location of Tibial Tunnels | Tibial Fixation | Rehabilitation Protocol |
|---|---|---|---|---|---|---|
| Ahn1
(2015) |
25 | Simple stitch | No. 1 PDS | Double/AL | Bony bridge | Not reported |
| Chung7
(2015) |
37 | Simple stitch | No. 1 PDS | Single/AL | Hewson button | Full extension with brace for 3 wk, PWB exercises for 6 wk, FWB and progressive closed kinetic chain strengthening exercises from 6 wk, light running at 3 mo, RTS at 6 mo |
| Kim16
(2011) |
22 | Simple stitch | No. 2 Ethibond | Single/ AL | 3.5-mm cortical screw with washer | Full extension with long cylinder cast for 2 wk; NWB and 30° of flexion in hinged brace for next 2 wk; increased flexion up to 90° until 6 wk; PWB to FWB between 6-8 wk; deep flexion allowed after 8 wk; further flexion, squatting, and RTS allowed after 6 mo |
| LaPrade24
(2017) |
35 | Simple stitch | No. 2 FiberWire | Double/AL | Endobutton | NWB in straight leg brace for first 6 wk, passive ROM from 0°-90° and quadriceps setting exercises initiated from POD 1 to 2 wk, PWB at 7 wk, endurance and strength exercises at 2 mo, normal to full activities at 5-7 mo |
| Lee27
(2014) |
25 | Simple or Mason-Allen stitch | No. 1 PDS | Single/ AL | Hewson button | ROM using continuous passive motion and isometric exercises from POD 1, PWB for 6 wk, FWB and progressive closed kinetic chain strengthening exercises from 6 wk, light running at 3 mo, RTS at 6 mo |
| Lee29
(2009) |
21 | Simple stitch | No. 5 Ethibond | Single/ AL | Endobutton | Full extension with long cylinder cast for 2 wk, passive ROM after first 2 wk, active motion up to 90° after first 4 wk, increased flexion by 10° per week up to 130° until 8 wk, PWB at 6 wk, FWB at 8 wk, full flexion and squatting after 6 mo |
| Moon31
(2012) |
51 | Simple stitch | No. 2 PDS | Double/AM | Bony bridge | Full extension with long cylinder cast for 2 wk, PWB from POD 1 to 2 wk, FWB after 6 wk, full flexion and squatting at 3 mo |
| Seo39
(2011) |
11 | Simple stitch | No. 1 PDS or No. 2 Ethibond | Single/ AM | 3.5-mm cortical screw with washer | Full extension with brace for 2 wk, muscle strengthening exercises at 4 wk, ROM exercises gradually to 90° from 2-6 wk, FWB at 6 wk, squatting and deep flexion after 3 mo, RTS at 6 mo |
aAL, anterolateral; AM, anteromedial; FWB, full weightbearing; NWB, nonweightbearing; POD, postoperative day; PWB, partial weightbearing; ROM, range of motion; RTS, return to sports.
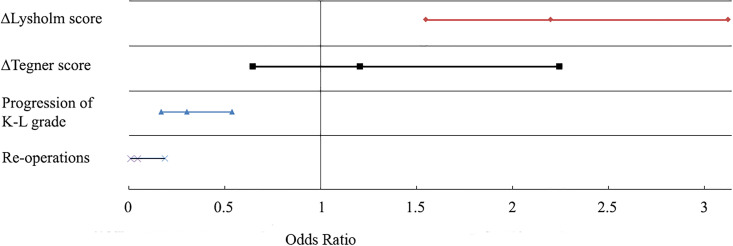
Clinical Outcomes
Overall, 6 studies on meniscal repair1,7,24,27,29,39 and 5 studies on partial meniscectomy4,7,10,35,43 reported pre- and postoperative Lysholm scores. The pooled improvements in the Lysholm score were 33.1 for meniscal repair and 13.1 for partial meniscectomy (Table 2). The summary OR was 2.20 (95% CI, 1.55-3.12) and significantly in favor of meniscal repair (Figure 2). Although the improvement in Tegner score in patients who underwent meniscal repair was 0.39 greater than that in patients who underwent partial meniscectomy, this difference did not reach statistical significance (Table 3).
Table 2.
Outcomes of Included Studiesa
| Outcome | Meniscal Repair | Partial Meniscectomy | ||||||
|---|---|---|---|---|---|---|---|---|
| No. of Knees | No. of Studies | Mean Follow-up, mo | Value | No. of Knees | No. of Studies | Mean Follow-up, mo | Value | |
| Δ Lysholm score | 167 | 6 | 37.9 | 33.1 (SE, 1.90) | 282 | 5 | 41.8 | 13.1 (SE, 3.27) |
| Δ Tegner score | 62 | 2 | 54.9 | 0.74 (SE, 0.196) | 70 | 2 | 36.4 | 0.35 (SE, 0.598) |
| Progression of K-L grade, % | 116 | 5 | 40.1 | 22.2 | 116 | 3 | 55.8 | 48.3 |
| Reoperations, % | 95 | 3 | 44.9 | 2.7 | 92 | 3 | 72.3 | 35.0 |
aΔ, difference between preoperatively and postoperatively; K-L, Kellgren-Lawrence.
Figure 2.
Odds ratios for each outcome compared between meniscal repair and partial meniscectomy. Higher numbers were seen for meniscal repair regarding improvement in Lysholm score (values to the right of the midline), whereas higher numbers were seen for partial meniscectomy regarding worsening of Kellgren-Lawrence (K-L) grade and rate of reoperation (values to the left of the midline). When the 95% CIs (both endpoints of each line) cross the midline (value 1), as with improvement in Tegner score, the difference between the procedures is not significant.
Table 3.
ORs of Outcomes Between Meniscal Repair and Partial Meniscectomya
| Outcome | OR (95% CI) | Better Performance |
|---|---|---|
| Δ Lysholm score | 2.1996 (1.5486-3.1243) | Repair |
| Δ Tegner score | 1.2058 (0.6484-2.2425) | No difference |
| Progression of K-L grade | 0.3054 (0.1728-0.5398) | Repair |
| Reoperations | 0.0515 (0.0139-0.1915) | Repair |
aΔ, difference between preoperatively and postoperatively; K-L, Kellgren-Lawrence; OR, odds ratio.
Radiological Outcomes
A total of 5 studies on meniscal repair1,7,16,27,29 and 3 studies on partial meniscectomy7,20,35 reported data on the proportion of patients who developed worse K-L grades on standing plain radiographs postoperatively. A mean of 22.2% of patients who underwent meniscal repair and 48.3% of those who underwent partial meniscectomy developed worse K-L grades postoperatively (Table 2). The summary OR was 0.31 (95% CI, 0.17-0.54) and significantly in favor of meniscal repair (Table 3 and Figure 2).
Reoperation Rates
There were 3 studies on meniscal repair7,24,29 and 3 studies on partial meniscectomy7,10,20 that reported the number and type of reoperation cases. Out of 95 knees who underwent meniscal repair, 4 underwent revision pullout repair at a mean of 44.9 months postoperatively; while in 92 knees who underwent partial meniscectomy, 30 underwent revision surgery (eg, high tibial osteotomy, unicompartmental knee arthroplasty, or total knee arthroplasty) at a mean of 72.3 months postoperatively. The summary OR was 0.05 (95% CI, 0.01-0.19) and significantly in favor of meniscal repair (Table 3 and Figure 2).
Meta-regression Analyses
Table 4 shows the results of meta-regression analyses. Age and follow-up duration were not significantly associated with improvements in Lysholm score or reoperation rates in patients who underwent meniscal repair or partial meniscectomy. This finding indicates that the results of the current meta-analysis were not biased by differences in age and follow-up duration between the included studies.
Table 4.
Associations of Age and Follow-up Period With Improvements in Lysholm Score and Reoperation Rate
| Variable | Coefficient | 95% CI | SE | P |
|---|---|---|---|---|
| Improvement in Lysholm score | ||||
| Age | –0.436 | –1.863 to 0.991 | 0.728 | .549 |
| Follow-up period | –0.230 | –0.533 to 0.074 | 0.155 | .394 |
| Reoperation rate | ||||
| Age | –0.133 | –0.599 to 0.333 | 0.238 | .576 |
| Follow-up period | 0.062 | –0.073 to 0.198 | 0.068 | .364 |
Discussion
The most important finding of this study was that meniscal repair for MMRTs showed better clinical outcomes and lower reoperation rates than partial meniscectomy. Additionally, the progression of knee osteoarthritis postoperatively was less severe with meniscal repair than it was with partial meniscectomy.
The results of the current study revealed that meniscal repair of MMRTs demonstrated better clinical and radiological results than partial meniscectomy in terms of greater improvements in the Lysholm score, lower proportions of K-L grade progression, and lower reoperation rates. These superior results of meniscal repair are to be expected to a certain degree because of the results of previous promising biomechanical studies. The cadaveric biomechanical study of Allaire et al2 demonstrated that an MMRT causes a 25% increase in peak contact pressure in the medial compartment compared with that found in the intact condition, which is nearly analogous to that of total meniscectomy status, and that repair of MMRTs restored peak contact pressure to that of normal status. Seitz et al38 investigated the effects of partial meniscectomy for MMRTs on contact mechanics in knee joints and reported that 100% partial resection of MMRTs resulted in significant complete discontinuity of the meniscal periphery, increased maximum contact pressure, and decreased contact area in the medial compartment in all tested knee positions. Most orthopaedic surgeons prefer meniscal repair over partial meniscectomy for the surgical treatment of MMRTs because of the biomechanical disadvantage of loss of hoop strain caused by discontinuity in the medial meniscal circumferential fiber as well as the better contact mechanics of meniscal repair shown in biomechanical studies. Our study verified the biomechanical superiority of meniscal repair compared with partial meniscectomy to some extent by showing it to have improved clinical outcomes and less progression of knee arthritis based on the best evidence now available. Furthermore, when considering not only the higher reoperation rates in partial meniscectomy but also the necessity of more invasive revision surgery such as high tibial osteotomy or unicompartmental or total knee arthroplasty, we cautiously recommend meniscal repair over partial meniscectomy for MMRTs if the degenerative changes in the meniscus are not severe and are repairable.
Although the results of our study demonstrated a lower proportion of patients with a progression of knee arthritis for meniscal repair than partial meniscectomy, that proportion was still high at >3-year follow-up (22.2% and 48.3%, respectively). For women in their 60s, approximately 2% per year develop incident radiographic osteoarthritis,9 thus there is a higher rate of osteoarthritis progression in knees with meniscal repair compared with the natural incidence of osteoarthritis in intact knees. An explanation for this can be found in previous biomechanical studies. A recent cadaveric study23 compared the tibiofemoral contact mechanics between anatomic repair at a root tear site and nonanatomic repair 5 mm posteromedially away from the root tear site, which was the reference value of the intact knee. The study reported that the contact pressure of nonanatomically repaired menisci was 33% higher than that of anatomically repaired menisci. This result might be a plausible explanation for the slight progression of arthritis in meniscal repair because of unintended nonanatomic repair. In terms of partial meniscectomy, the contact pressure could not but increase sharply because an MMRT itself reduces hoop stress due to the radial tear component by incising the circumferential fiber in the meniscus. As additional meniscal tissue is removed in partial meniscectomy, there is no way to restore the hoop stress that is important for the shock absorption function of menisci.15 Thus, these results cautiously emphasize the importance of not only meniscal repair but also anatomic meniscal repair in patients with MMRTs to restore the contact area or contact pressure to that corresponding to the intact knee.
The current study showed that pre- to postoperative improvements in the Lysholm score were better with meniscal repair than partial meniscectomy for MMRTs. The mean difference in the improvement in the Lysholm score between the 2 surgical approaches was 20.0 points. We believe that this difference could be clinically important because the minimal clinically important difference for the Lysholm score is 10 to 15 points.18,30 Even considering that the Lysholm score is relatively insensitive in detecting differences in functional outcomes between 2 surgical approaches because of its high ceiling effect,19 the score difference of 20.0 points is sufficiently large to be considered clinically important. The Lysholm and Tegner scores have demonstrated acceptable psychometric performance as outcome measures for patients with a meniscal injury5; however, the current review did not find a significant difference in Tegner score improvement between the 2 surgical approaches, as the responsiveness---that is, the ability of the instrument to reflect a change after treatment---of the Tegner score had a relatively moderate effect size and standardized response mean, whereas the responsiveness of the Lysholm score had a relatively large effect size and standardized response mean.5
Previous systematic reviews have addressed the main indications for meniscal repair: (1) acute or traumatic tears in patients who have yet to progress to osteoarthritis to prevent advanced osteoarthritis in the future, and (2) chronic symptomatic root tears in young or middle-aged patients without dominant preexisting osteoarthritis.3,8,26,33 Recent studies have demonstrated that the age of the patient at the time of meniscal repair does not have a primary effect on the clinical prognosis or on cost-effectiveness.8,24 Although not specifically addressed in our study, factors based on previous studies, such as advanced osteoarthritis, varus alignment, and a large amount of meniscal subluxation, need to be considered when making a treatment plan for patients with MMRTs.6,8,22 The clinical relevance of the present review is that meniscal repair showed favorable outcomes in terms of clinical improvement and radiological progression of arthritis, providing systematic and objective evidence for meniscal repair for MMRTs.
This study has several limitations. One of the most important shortcomings was that we could not take into consideration the differences in the severity of knee osteoarthritis preoperatively, which could have affected the clinical and radiological outcomes after meniscal repair or partial meniscectomy. However, most studies excluded patients with severe knee osteoarthritis with a K-L grade IV or >5° varus deformity. Additionally, the heterogeneity of the demographic data in the included studies, including differences in age distribution and follow-up duration, could be a potential confounding factor. However, our meta-regression analyses found that age and follow-up period were not significantly associated with changes in the Lysholm score or reoperation rate. Another limitation was that we only included meniscal repair using the pullout suture technique through a transtibial tunnel; therefore, the results of this study might not be extrapolated to other techniques of meniscal repair such as suture anchors or meniscal fixation devices. In addition, our meta-analysis was based on studies with level 4 evidence because the research questions have never been explored in the context of randomized or even prospective trials. However, the advancement of meta-analyses has led to the analysis of single-arm studies. Also, a relatively small number of studies was included to draw a definite conclusion; however, the results may still provide useful information to clinicians.
Conclusion
This study found that meniscal repair in patients with degenerative MMRTs was associated with better clinical outcomes and lower reoperation rates compared with partial meniscectomy. Additionally, the progression of knee osteoarthritis was less severe after meniscal repair than it was after partial meniscectomy.
APPENDIX
Table A1.
Study Design, Demographic Data, Quality Scores, and Results of Included Studiesa
| Lead Author (Year) | Study Type | No. of Knees | Mean Age, y | Mean Follow-up, mo | Mean BMI, kg/m2 | MINORS Score |
|---|---|---|---|---|---|---|
| Meniscal repair | ||||||
| Ahn1 (2015) | RCS (vs nonoperative treatment) | 25 | 55.56 | 17.43 | 25.11 | 16 |
| Main findings: The repair group had better IKDC subjective, Tegner, and Lysholm scores. Patients with a mild varus knee achieved better clinical outcomes than did patients with a severe varus knee. The patients with mild cartilage degeneration achieved better outcomes than did those with severe cartilage degeneration. | ||||||
| Chung7 (2015) | RCS (vs meniscectomy) | 37 | 55.5 | 72 | 26.1 | 19 |
| Main findings: The mean Lysholm and IKDC scores improved significantly. However, the width of the medial joint-space and the K-L grade worsened significantly in both groups. The repair group had significantly better Lysholm and IKDC scores, less K-L grade progression, and less medial joint-space narrowing than the meniscectomy group. | ||||||
| Kim16 (2011) | PCS (vs suture anchor) | 22 | 53.2 | 25.9 | 23.9 | 20 |
| Main findings: The repair group showed significant improvements in function and did not show significant differences in the K-L grade compared with preoperatively. On magnetic resonance imaging, the mean meniscal extrusion was significantly decreased postoperatively. Incompletely healed cases showed a progression of cartilage degeneration. | ||||||
| LaPrade24 (2017) | RCS (groups based on age and laterality) | 35 | 41 | 24 | 27.6 | 18 |
| Main findings: For the age groups, the Lysholm and WOMAC scores demonstrated significant postoperative improvements. For the laterality groups, all functional scores significantly improved postoperatively. | ||||||
| Lee27 (2014) | RCS (stitch technique) | 25 | 55.7 | 24.1 | 27.3 | 18 |
| Main findings: The Lysholm, IKDC, and Tegner scores improved significantly in both groups. The Mason-Allen stitch group did not show a significant progression in the K-L grade and cartilage degeneration, whereas both measures increased significantly in the simple stitch group. | ||||||
| Lee29 (2009) | Case series | 21 | 51.2 | 31.8 | NR | 8 |
| Main findings: The mean HSS score improved from 61.1 preoperatively to 93.8 at final follow-up, and the mean Lysholm score improved from 57.0 preoperatively to 93.1 at final follow-up. | ||||||
| Moon31 (2012) | Case series | 51 | 59 | 33 | NR | 9 |
| Main findings: All clinical outcomes significantly improved after surgery. Patients with Outerbridge grade 3 or 4 chondral lesions had poorer results than those with grade 1 or 2 lesions in terms of AKS function and Lysholm scores. Patients with varus alignment of >5° had poorer results than those with varus alignment of <5° in terms of VAS satisfaction, AKS function, and Lysholm scores. Preoperative meniscal extrusion was found to be positively correlated with final extrusion. | ||||||
| Seo39 (2011) | Case series | 11 | 55.4 | 13.4 | NR | 9 |
| Main findings: The mean Lysholm and HSS scores improved significantly. On second-look arthroscopic surgery, there was no case with complete healing. | ||||||
| Partial meniscectomy | ||||||
| Bin4 (2004) | Case series | 96 | 56.3 | 28.3 | NR | 10 |
| Main findings: Most patients were elderly and had degenerated articular cartilage, and subjective symptoms improved significantly after arthroscopic partial meniscectomy. | ||||||
| Chung7 (2015) | RCS (vs pullout technique) | 20 | 55 | 67.5 | 27.4 | 19 |
| Main findings: See this study in the section above. | ||||||
| Han10 (2010) | Case series | 46 | 59 | 78 | NR | 10 |
| Main findings: The modified Lysholm score significantly improved at final follow-up. There was a significant negative correlation between chondral wear during arthroscopic surgery and the preoperative K-L grade with the modified Lysholm score at final follow-up. | ||||||
| Krych20 (2018) | RCS (vs nonoperative treatment) | 26 | 54.7 | 66 | 32.8 | 18 |
| Main findings: There was no significant difference in the final Tegner scores, IKDC scores, K-L grades, progression to arthroplasty, or overall failure rates between the meniscectomy and nonoperative groups. | ||||||
| Ozkoc35 (2008) | Case series | 70 | 55.8 | 56.7 | 33.3 | 7 |
| Main findings: The mean Lysholm score improved from the preoperative value. The mean preoperative K-L grade increased at the latest follow-up, which showed significant worsening. | ||||||
| Yim43 (2013) | RCT (vs nonoperative treatment) | 50 | 54.9 | 24 | 25 | 23 |
| Main findings: In terms of clinical outcomes, meniscectomy did not provide better functional improvements than nonoperative treatment. Although most patients initially had intense knee pain with mechanical symptoms, both groups reported a relief in knee pain, improved knee function, and a high level of satisfaction with their treatment. | ||||||
aThe repair group consisted of 227 knees with a mean age of 53.5 years and mean follow-up of 33.5 months. The meniscectomy group consisted of 308 knees with a mean age of 56.1 years and mean follow-up of 47.2 months. AKS, American Knee Society; BMI, body mass index; HSS, Hospital for Special Surgery; IKDC, International Knee Documentation Committee; K-L, Kellgren-Lawrence; MINORS, Methodological Index for Non-Randomized Studies; NR, not reported; PCS, prospective cohort study; RCS, retrospective cohort study; RCT, randomized controlled trial; VAS, visual analog scale; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index.
Footnotes
Final revision submitted March 4, 2020; accepted April 7, 2020.
The authors have declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Ahn JH, Jeong HJ, Lee YS, et al. Comparison between conservative treatment and arthroscopic pull-out repair of the medial meniscus root tear and analysis of prognostic factors for the determination of repair indication. Arch Orthop Trauma Surg. 2015;135(9):1265–1276. [DOI] [PubMed] [Google Scholar]
- 2. Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus: similar to total meniscectomy. J Bone Joint Surg Am. 2008;90(9):1922–1931. [DOI] [PubMed] [Google Scholar]
- 3. Bhatia S, LaPrade CM, Ellman MB, LaPrade RF. Meniscal root tears: significance, diagnosis, and treatment. Am J Sports Med. 2014;42(12):3016–3030. [DOI] [PubMed] [Google Scholar]
- 4. Bin SI, Kim JM, Shin SJ. Radial tears of the posterior horn of the medial meniscus. Arthroscopy. 2004;20(4):373–378. [DOI] [PubMed] [Google Scholar]
- 5. Briggs KK, Kocher MS, Rodkey WG, Steadman JR. Reliability, validity, and responsiveness of the Lysholm knee score and Tegner activity scale for patients with meniscal injury of the knee. J Bone Joint Surg Am. 2006;88(4):698–705. [DOI] [PubMed] [Google Scholar]
- 6. Chung KS, Ha JK, Ra HJ, Kim JG. Prognostic factors in the midterm results of pullout fixation for posterior root tears of the medial meniscus. Arthroscopy. 2016;32(7):1319–1327. [DOI] [PubMed] [Google Scholar]
- 7. Chung KS, Ha JK, Yeom CH, et al. Comparison of clinical and radiologic results between partial meniscectomy and refixation of medial meniscus posterior root tears: a minimum 5-year follow-up. Arthroscopy. 2015;31(10):1941–1950. [DOI] [PubMed] [Google Scholar]
- 8. Faucett SC, Geisler BP, Chahla J, et al. Meniscus root repair vs meniscectomy or nonoperative management to prevent knee osteoarthritis after medial meniscus root tears: clinical and economic effectiveness. Am J Sports Med. 2019;47(3):762–769. [DOI] [PubMed] [Google Scholar]
- 9. Felson DT, Zhang Y, Hannan MT, et al. The incidence and natural history of knee osteoarthritis in the elderly: the Framingham Osteoarthritis Study. Arthritis Rheum. 1995;38(10):1500–1505. [DOI] [PubMed] [Google Scholar]
- 10. Han SB, Shetty GM, Lee DH, et al. Unfavorable results of partial meniscectomy for complete posterior medial meniscus root tear with early osteoarthritis: a 5- to 8-year follow-up study. Arthroscopy. 2010;26(10):1326–1332. [DOI] [PubMed] [Google Scholar]
- 11. Harner CD, Mauro CS, Lesniak BP, Romanowski JR. Biomechanical consequences of a tear of the posterior root of the medial meniscus: surgical technique. J Bone Joint Surg Am. 2009;91(suppl 2):257–270. [DOI] [PubMed] [Google Scholar]
- 12. Higgins JPT, Deeks JJ, Altman DG. Chapter 16: special topics in statistics In: Higgins J, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration; 2008:481–529. [Google Scholar]
- 13. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kang DG, Park YJ, Yu JH, Oh JB, Lee DY. A systematic review and meta-analysis of arthroscopic meniscus repair in young patients: comparison of all-inside and inside-out suture techniques. Knee Surg Relat Res. 2019;31(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kim JG, Lee SY, Chay S, Lim HC, Bae JH. Arthroscopic meniscectomy for medial meniscus horizontal cleavage tears in patients under age 45. Knee Surg Relat Res. 2016;28(3):225–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kim JH, Chung JH, Lee DH, Lee YS, Kim JR, Ryu KJ. Arthroscopic suture anchor repair versus pullout suture repair in posterior root tear of the medial meniscus: a prospective comparison study. Arthroscopy. 2011;27(12):1644–1653. [DOI] [PubMed] [Google Scholar]
- 17. Kim YM, Joo YB, Noh CK, Park IY. The optimal suture site for the repair of posterior horn root tears: biomechanical evaluation of pullout strength in porcine menisci. Knee Surg Relat Res. 2016;28(2):147–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kocher MS, Steadman JR, Briggs KK, Sterett WI, Hawkins RJ. Reliability, validity, and responsiveness of the Lysholm knee scale for various chondral disorders of the knee. J Bone Joint Surg Am. 2004;86(6):1139–1145. [DOI] [PubMed] [Google Scholar]
- 19. Koutras G, Papadopoulos P, Terzidis IP, Gigis I, Pappas E. Short-term functional and clinical outcomes after ACL reconstruction with hamstrings autograft: transtibial versus anteromedial portal technique. Knee Surg Sports Traumatol Arthrosc. 2013;21(8):1904–1909. [DOI] [PubMed] [Google Scholar]
- 20. Krych AJ, Johnson NR, Mohan R, Dahm DL, Levy BA, Stuart MJ. Partial meniscectomy provides no benefit for symptomatic degenerative medial meniscus posterior root tears. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1117–1122. [DOI] [PubMed] [Google Scholar]
- 21. Krych AJ, Reardon PJ, Johnson NR, et al. Non-operative management of medial meniscus posterior horn root tears is associated with worsening arthritis and poor clinical outcome at 5-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):383–389. [DOI] [PubMed] [Google Scholar]
- 22. Kwak YH, Lee S, Lee MC, Han HS. Large meniscus extrusion ratio is a poor prognostic factor of conservative treatment for medial meniscus posterior root tear. Knee Surg Sports Traumatol Arthrosc. 2018;26(3):781–786. [DOI] [PubMed] [Google Scholar]
- 23. LaPrade CM, Foad A, Smith SD, et al. Biomechanical consequences of a nonanatomic posterior medial meniscal root repair. Am J Sports Med. 2015;43(4):912–920. [DOI] [PubMed] [Google Scholar]
- 24. LaPrade RF, Matheny LM, Moulton SG, James EW, Dean CS. Posterior meniscal root repairs: outcomes of an anatomic transtibial pull-out technique. Am J Sports Med. 2017;45(4):884–891. [DOI] [PubMed] [Google Scholar]
- 25. Lee DH, Lee BS, Kim JM, et al. Predictors of degenerative medial meniscus extrusion: radial component and knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2011;19(2):222–229. [DOI] [PubMed] [Google Scholar]
- 26. Lee DW, Ha JK, Kim JG. Medial meniscus posterior root tear: a comprehensive review. Knee Surg Relat Res. 2014;26(3):125–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lee DW, Kim MK, Jang HS, Ha JK, Kim JG. Clinical and radiologic evaluation of arthroscopic medial meniscus root tear refixation: comparison of the modified Mason-Allen stitch and simple stitches. Arthroscopy. 2014;30(11):1439–1446. [DOI] [PubMed] [Google Scholar]
- 28. Lee DW, Shim JC, Yang SJ, Cho SI, Kim JG. Functional effects of single semitendinosus tendon harvesting in anatomic anterior cruciate ligament reconstruction: comparison of single versus dual hamstring harvesting. Clin Orthop Surg. 2019;11(1):60–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lee JH, Lim YJ, Kim KB, Kim KH, Song JH. Arthroscopic pullout suture repair of posterior root tear of the medial meniscus: radiographic and clinical results with a 2-year follow-up. Arthroscopy. 2009;25(9):951–958. [DOI] [PubMed] [Google Scholar]
- 30. Marx RG. Patient-reported measure of knee function. J Bone Joint Surg Am. 2000;82(8):1199–1202. [DOI] [PubMed] [Google Scholar]
- 31. Moon HK, Koh YG, Kim YC, Park YS, Jo SB, Kwon SK. Prognostic factors of arthroscopic pull-out repair for a posterior root tear of the medial meniscus. Am J Sports Med. 2012;40(5):1138–1143. [DOI] [PubMed] [Google Scholar]
- 32. Nakama GY, Aman ZS, Storaci HW, Kuczmarski AS, Krob JJ, Strauss MJ. Different suture materials for arthroscopic transtibial pull-out repair of medial meniscal posterior root tears: a human biomechanical study. Orthop J Sports Med. 2019;7(9):2325967119873274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Okazaki Y, Furumatsu T, Shimamura Y, et al. Time-dependent increase in medial meniscus extrusion after medial meniscus posterior root tear analyzed by using magnetic resonance imaging. Knee Surg Relat Res. 2019;31(2):120–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Okimura S, Mae T, Tachibana Y, et al. Biomechanical comparison of meniscus-suture constructs for pullout repair of medial meniscus posterior root tears. J Exp Orthop. 2019;6(1):17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ozkoc G, Circi E, Gonc U, Irgit K, Pourbagher A, Tandogan RN. Radial tears in the root of the posterior horn of the medial meniscus. Knee Surg Sports Traumatol Arthrosc. 2008;16(9):849–854. [DOI] [PubMed] [Google Scholar]
- 36. Padalecki JR, Jansson KS, Smith SD, et al. Biomechanical consequences of a complete radial tear adjacent to the medial meniscus posterior root attachment site: in situ pull-out repair restores derangement of joint mechanics. Am J Sports Med. 2014;42(3):699–707. [DOI] [PubMed] [Google Scholar]
- 37. Petersen W, Forkel P, Feucht MJ, Zantop T, Imhoff AB, Brucker PU. Posterior root tear of the medial and lateral meniscus. Arch Orthop Trauma Surg. 2014;134(2):237–255. [DOI] [PubMed] [Google Scholar]
- 38. Seitz AM, Lubomierski A, Friemert B, Ignatius A, Durselen L. Effect of partial meniscectomy at the medial posterior horn on tibiofemoral contact mechanics and meniscal hoop strains in human knees. J Orthop Res. 2012;30(6):934–942. [DOI] [PubMed] [Google Scholar]
- 39. Seo HS, Lee SC, Jung KA. Second-look arthroscopic findings after repairs of posterior root tears of the medial meniscus. Am J Sports Med. 2011;39(1):99–107. [DOI] [PubMed] [Google Scholar]
- 40. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological Index for Non-Randomized Studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. [DOI] [PubMed] [Google Scholar]
- 41. Viechtbauer W. Conducting meta-analyses in R with the metafor package. Journal of Statistical Software. 2010;36(3):1–48. [Google Scholar]
- 42. Wallace BC, Dahabreh IJ, Trikalinos TA, Lau J, Trow P, Schmid CH. Closing the gap between methodologists and end-users: R as a computational back-end. Journal of Statistical Software. 2012;49(5):1–15. [Google Scholar]
- 43. Yim JH, Seon JK, Song EK, et al. A comparative study of meniscectomy and nonoperative treatment for degenerative horizontal tears of the medial meniscus. Am J Sports Med. 2013;41(7):1565–1570. [DOI] [PubMed] [Google Scholar]