Abstract
Hydroxychloroquine (HCQ) is a widely used drug to treat patients with coronavirus disease 19 (COVID-19). Although evidence of its efficacy and safety remains limited and controversial, both cardiac and non-cardiac adverse events are known to be associated with its use. To our knowledge, electrical storm in patients with COVID-19, or in any case treated with HCQ, has not been reported. We report the case of a 78-year-old male with an implantable cardiac resynchronization defibrillator (CRT-D) and a non-severe form of COVID-19. After a few days of home therapy with HCQ, an electrical storm was revealed that was associated with an increase in QTc. Following admission to the intensive care unit, HCQ was discontinued and progressive reduction of the QTc with electrical stabilization was observed. This clinical case highlights the potential risk of arrythmia associated with the use of HCQ and stresses the need for close electrocardiographic monitoring, especially in patients with established heart disease.
Keywords: Electrical storm, case report, ventricular tachycardia, hydroxychloroquine, QTc prolongation, COVID-19
Introduction
While SARS-CoV-2 infection is related to subclinical or mild forms of coronavirus disease 19 (COVID-19) in roughly 85% of cases, respiratory complications such as severe interstitial pneumonitis and severe acute respiratory distress syndrome occur in 10%–15% of cases.1,2 Furthermore, COVID-19 affects multiple organs, including the cardiovascular system; various forms of cardiac arrhythmia occur in roughly 15% of patients, with a higher prevalence in more severe cases.3 However, the risk of arrhythmia is also increased by some drugs, especially in the presence of polypharmacotherapy.
Hydroxychloroquine (HCQ) is widely used in patients with COVID-19.4 While its effectiveness in patients with COVID-19 has not been unequivocally confirmed, its use is associated with adverse effects mainly affecting the eye, liver, and heart.3,5 It is known, in fact, that HCQ can increase the risk of arrhythmia by increasing the QTc.5,6 Moreover, polypharmacotherapy, which is especially common in elderly patients with heart disease, poses an additional risk for possible drug interactions.
Case presentation
A 78-year-old Caucasian male with non-ischemic dilated cardiomyopathy, who had received a cardiac resynchronization therapy device (a CRT-D) 2 years earlier at our center, was brought to our clinic in an emergency situation for an electric storm (ES) with repeated shock delivery. ES is the sequela of a state of cardiac electrical instability leading to multiple episodes of ventricular arrhythmia in a short period of time and is commonly defined as the occurrence of at least three sustained episodes of appropriate ventricular tachycardia, ventricular fibrillation or ICD shock during a 24-h period.7
During the 2 years after biventricular implantation of an implantable cardioverter-defibrillator (ICD), the patient referred moderate improvement in general conditions, corresponding to an increase in the ejection fraction from 28% to 34% with functional improvement from III to II New York Heart Association (NYHA) class.7 Medical therapy included bisoprolol 5 mg, ramipril 10 mg, furosemide 75 mg, and aldactone 25 mg. During periodic checks of the device, no significant ventricular arrhythmias had emerged that required anti-tachycardia therapy with shock delivery or anti-tachycardia pacing (ATP), or that fell within the window of monitoring, except for rare ventricular triplets. About 10 days before the current hospitalization, the patient experienced fever, which after 2 days was associated with anosmia and ageusia, in the absence of cough, dyspnea, or other symptoms. SpO2 by percutaneous pulse oximetry was constantly around 95%, which was similar to levels prior to the febrile episode. On the advice of his general practitioner, home therapy with HCQ was initiated (400 mg BID on day 1, followed by 200 mg BID for a total period of 6 days), 5 days before admission.
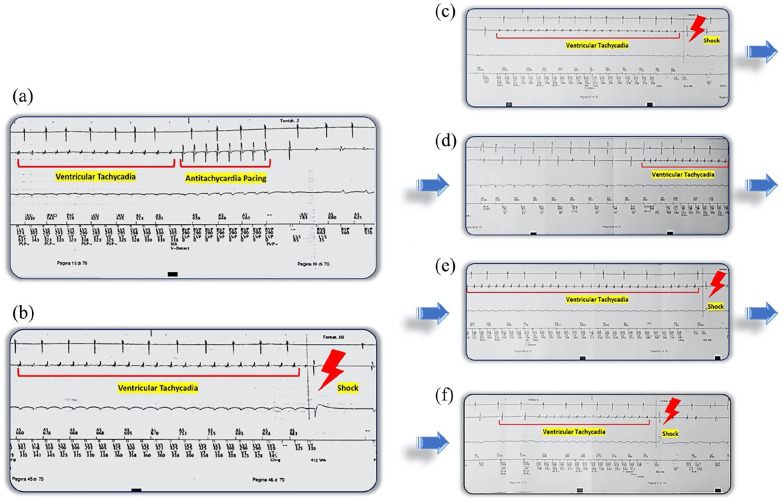
Upon arrival at the emergency department, blood pressure was 130/70 mmHg, heart rate 80 bpm, temperature was 36.8 °C, and oxygen saturation was 96% while breathing ambient air. The patient had cold sweats and was clearly agitated. Blood glucose was within normal limits. Arterial gases, lactate and electrolytes were within normal ranges. Blood tests revealed high levels of hs-troponin T, creatine kinase-MB, and NT-proBNP (Table 1), and a slight increase in creatinine (1.3 mg/dL, corresponding to creatinine clearance of 46.37 mL/ min by Cockcroft-Gault formula). Tisdale score, which at the last visit 2 months earlier was 5 (low risk) was 11 (high risk). Chest X-ray did not detect any notable pulmonary changes and confirmed regular placement of the leads. A 12-lead electrocardiogram (ECG) revealed a sequential biventricular pacemaker rhythm (Figure 1). Interrogation of the device revealed, during the last 6 hours, the presence of numerous episodes of sustained and non-sustained ventricular tachycardia (VT), which in three occasions reverted with ATP and on eight occasions with shock delivery of 41 Joules (Figure 2). In addition, the device showed functionality parameters within normal limits and superimposable on previous control visits with 98% of correct biventricular stimulation.
Table 1.
Main laboratory findings at admission and on the fourth day of hospitalization.
| Parameter | Admission | Day 4 |
|---|---|---|
| QTc length | 483 ms | 446 m |
| SPO2 | 95% | 95% |
| PO2 | 84 mmHg | 85 mmHg |
| PCO2 | 30 mmHg | 32 mmHg |
| pH | 7.45 | 7.44 |
| Sodium | 145 mmol/L | 145 mmol/L |
| Potassium | 4.1 mmol/L | 4 mmol/L |
| Hs-troponin T | 1.8 ng/mL | 1.4 ng/mL |
| CPK-MB | 48 ng/mL | 25 ng/mL |
| NT-proBNP | 2613 pg/mL | 1508 pg/mL |
| Creatinine | 1.3 mg/dL | 1.2 mg/dL |
| eGFR | 46.37 mL/min | 50.2 mL/min |
| Leukocytes | 6.92 × 109/L | 7.2 × 109/L |
| Platelets | 151 × 109/L | 182 × 109/L |
| Hb | 13.7 g/dL | 13.2 g/dL |
CPK-MB: creatine kinase myocardial band; eGFR: estimated glomerular filtration rate; Hb: hemoglobin; Hs: high sensitivity.
Figure 1.
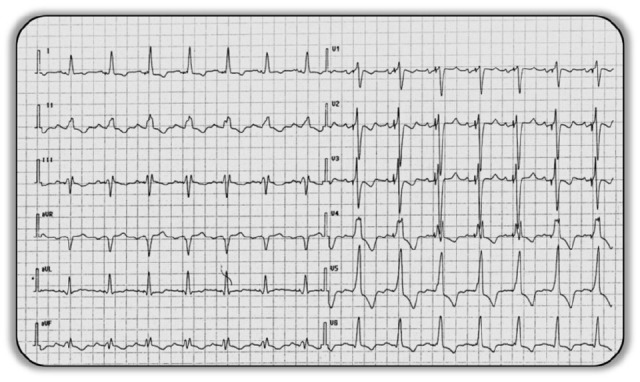
12-Lead ECG at admission showing biventricular pacing.
Figure 2.
(a) Ventricular tachycardia interrupted by anti-tachycardia pacing. (b) Ventricular tachycardia interrupted by shock delivery. (c–f) Sequence of multiple episodes of ventricular tachycardia treated with shock delivery.
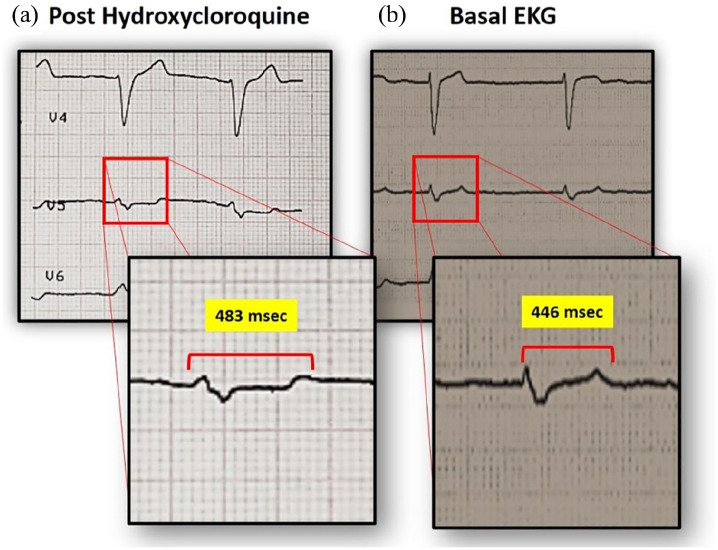
The patient was admitted to the intensive care unit, sedated with propofol, intubated, and administered intravenous metoprolol and magnesium sulfate. Nasopharyngeal swab was positive for SARS-CoV-2 by reverse transcription polymerase chain reaction (RT-PCR), and did not have a very high viral load of 27 cycle-threshold, while the search for common cardiotropic infectious agents was negative. Echocardiographic examination revealed deterioration of cardiac contractility, in the absence of specific contractile deficits, with an ejection fraction that had decreased to levels seen prior to implantation of the biventricular ICD. Urgent coronary angiography showed no evidence of obstructive coronary artery disease. Upon arrival at the emergency department, while checking the biventricular ICD, an ECG was also done in the absence of pacing, with the observation of spontaneous electrical activity, highlighting a QTc of 483 ms; at electrocardiogram (ECG) performed 2 months earlier, the QTc was 446 ms (Figure 3). The only change in therapy was the introduction of HCQ, and after consultation with an infectious disease specialist the drug was discontinued (it had been administered for a total of 6 days). This was followed by progressive improvement in the QTc and parallel regression of ventricular arrhythmias. On the second day, therapy with propofol was stopped, and on the fourth day therapy with oral beta-blockers was restarted.
Figure 3.
QTc interval during administration of HCQ (a) and at baseline 2 months prior (b).
Discussion
The incidence of ES in patients with ICD is 10%–20%, decreasing to about 7% in patients with CRT-D devices.8 The most common causes of ES are myocardial ischemia, thyrotoxicosis, electrolyte alterations, and use of drugs that promote QTc prolongation.8,9 QTc prolongation is most commonly associated with polymorphic VT, although cases of monomorphic VT, such as the one presented in this case report, have been described in the literature.9,10 Monomorphic VT in acquired LQT syndrome has been described as a focal discharge that could be attributed to early afterdepolarization as a triggered activity.11 HCQ is known to promote delayed ventricular repolarization which, by enabling early afterdepolarizations, can trigger ventricular arrhythmias.12 In the present case, after discontinuing HCQ, a progressive reduction in both QTc and cardiac electrical instability was seen.
In COVID-19, HCQ is widely used experimentally on a compassionate basis (off-label) in both home and hospital settings, and has become part of numerous therapeutic algorithms for COVID-19, both alone and in combination with azithromycin.4,10 The partial results of ongoing trials have yielded conflicting results in terms of efficacy and safety, leading the World Health Organization to stop ongoing investigations.11 It is known that HCQ can promote adverse cardiac effects. In addition to rare cases of direct myocardiotoxicity, HCQ can promote electrical conduction disturbances with atrioventricular block and bundle branch block, as well as prolong the QTc.12 HCQ is structurally similar to the class IA antiarrhythmic quinidine, which inhibits voltage-gated sodium and potassium channels, thereby prolonging the QT interval and increasing the risk of ventricular arrhythmias, torsades de pointes, and sudden cardiac death.3,5
In patients with COVID-19, the use of HCQ is associated with an increase in QTc in approximately 25% of cases.13,14 In particular, it has been shown that in 19% of patients the use of HCQ favors elongation of the QTc > 500 ms, and that in 3% of cases this elongation was > 60 ms compared with baseline values.15 In the present case, QTc elongation of 37 ms over baseline was observed. To our knowledge, there are no reports of ES in patients with COVID-19, or in any case treated with HCQ. Although cardiac damage caused by COVID-19 cannot be excluded, the chronology of events, with progressive shortening of the QTc and subsequent cardiac electrical stabilization seen after discontinuation of HCQ, leads us believe that the ES in the present case was an iatrogenic effect of HCQ.
Conclusion
While the efficacy and safety of HCQ in patients with COVID-19 is beyond the scope of the current case report, it is important to draw attention to the principles of prudence in the use of this drug, especially in elderly patients with established heart disease and polypharmacotherapy. In particular, home therapy with HCQ should require strict electrocardiographic monitoring and laboratory tests, and when difficult to perform in a home setting, the patient should be hospitalized.
Acknowledgments
We thank Patrick Moore, an independent medical writer, who provided English-language editing and journal styling prior to submission on behalf of Health Publishing & Services Srl.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Our institution does not require ethical approval for reporting individual cases or case series.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Medical writing support was funded by Novartis Farma SpA.
Informed consent: Written informed consent was obtained from the patient for his anonymized information to be published in this article.
ORCID iDs: Francesco Vetta  https://orcid.org/0000-0003-0778-7160
https://orcid.org/0000-0003-0778-7160
Leonardo Marinaccio  https://orcid.org/0000-0002-7480-2861
https://orcid.org/0000-0002-7480-2861
References
- 1. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395: 497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Young BE, Ong SWX, Kalimuddin S, et al. Epidemiologic features and clinical course of patients infected with SARS-CoV-2 in Singapore. JAMA 2020; 323: 1488–1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Vetta F, Vetta G, Marinaccio L. Coronavirus disease 2019 (COVID-19) and cardiovascular disease: a vicious circle. J Cardiol Cardiovasc Res 2020; 1: 1–12. [Google Scholar]
- 4. Cortegiani A, Ingoglia G, Ippolito M, et al. A systematic review on the efficacy and safety of chloroquine for the treatment of COVID-19. J Crit Care 2020; 57: 279–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. World Health Organization. The cardiotoxicity of antimalarials: Malaria Policy Advisory Committee Meeting, https://www.who.int/malaria/mpac/mpac-mar2017-erg-cardiotoxicity-report-session2.pdf (accessed 28 May 2020).
- 6. Bonow RO, Hernandez AF, Turakhia M. Hydroxychloroquine, coronavirus disease 2019, and QT prolongation. JAMA Cardiol 2020; 5: 986–987. [DOI] [PubMed] [Google Scholar]
- 7. American Heart Association. Classes of heart failure, https://www.heart.org/en/health-topics/heart-failure/what-is-heart-failure/classes-of-heart-failure (accessed 20 October 2020).
- 8. Gao D, Sapp JL. Electrical storm: definitions, clinical importance, and treatment. Curr Opin Cardiol 2013; 28: 72–79. [DOI] [PubMed] [Google Scholar]
- 9. Al-Khatib SM, Stevenson WG, Ackerman MJ, et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice guidelines and the Heart Rhythm Society. Circulation 2018; 138: e210–e271. [DOI] [PubMed] [Google Scholar]
- 10. Gautret P, Lagier JC, Parola P, et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents 2020; 56: 105949. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 11. World Health Organization. Coronavirus disease (COVID-19): hydroxychloroquine, https://www.who.int/news-room/q-a-detail/q-a-hydroxychloroquine-and-covid-19 (accessed 28 May 2020).
- 12. Guzik TJ, Mohiddin SA, Dimarco A, et al. COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. Cardiovasc Res 2020; 116: 1666–1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Borba MGS, Val FFA, Sampaio VS, et al. Effect of high vs low doses of chloroquine diphosphate as adjunctive therapy for patients hospitalized with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection: a randomized clinical trial. JAMA Netw Open 2020; 3: e208857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Roden DM, Harrington RA, Poppas A, et al. Considerations for drug interactions on QTc in exploratory COVID-19 treatment. Circulation 2020; 141: e906–e907. [DOI] [PubMed] [Google Scholar]
- 15. Mercuro NJ, Yen CF, Shim DJ, et al. Risk of QT interval prolongation associated with use of hydroxychloroquine with or without concomitant azithromycin among hospitalized patients testing positive for coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020; 5: 1036–1041. [DOI] [PMC free article] [PubMed] [Google Scholar]