Abstract
The coronavirus disease 2019 crisis in South Africa has been managed through an effective evidence-based approach. The aim of this case report was to determine the value of staying physically active during the coronavirus disease 2019 pandemic, using online resources to prevent the harmful effects of sedentary behaviour under confined living conditions. A repatriated South African citizen was placed into monitored 14-day quarantine confined to a room, self-monitoring dietary intake and physical and health measures, while engaged in online exercise videos and indoor walking. This study demonstrates that structured indoor activity improves physical and mental health outcomes, despite prolonged sitting time during the day. During the current pandemic and in the presence of limited freedom of movement, sustained physical activity is made feasible by accessing online tools and resources, essentially reducing vulnerability to existing cardiovascular health concerns. However, these findings are based on a single participant and therefore further study is required.
Keywords: COVID-19, quarantine, exercise, physical activity, quality of life
Introduction
It is now established that the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causes the coronavirus disease 2019 (COVID-19).1 A review of early publications revealed that the first recorded cases were linked to possible contact with animals at a seafood market in Wuhan, China, followed by human-to-human transmission through close contact, which increased risk among medical professionals. Adults in the age group 25–89 years were more affected than children, and the level of transmissibility and pandemic risk was higher than for the SARS-CoV-1. Therefore, the spread to other countries was quick. Symptoms ranged from mild fever, myalgia and fatigue to severe complicated dyspnoea, with progressive respiratory failure, which caused death, particularly in patients with comorbidities. Countries introduced public health prevention measures, such as case isolation, contacts identification and quarantine.2 The South African government responded rapidly to the pandemic by introducing nationwide risk adjusted strategy on the 26 March 2020,3 essentially limiting economic and social activities to essential services associated with addressing and managing COVID-19. The current consensus is for people to remain physically and socially distanced from society, predominantly at home and following a standard universal hygiene protocol.2 The call to stay at home has not been heeded by all South Africans, but there are obvious health implications during the lockdown period in the form of mental illness, boredom, stress, sleep disturbances, sedentariness and physical inactivity.4 Stress conditions trigger carbohydrate craving, which may contribute to excessive weight gain and obesity, which in turn increase the risk for complications of COVID-19.5 Observations from several critical care centres in the United Kingdom, Italy and France confirmed that COVID-19 further exacerbated inflammation in obese patients with chronic low-grade inflammation. Obesity-driven type 2 diabetes, hypertension, fatty liver disease and impaired fibrinolysis contribute to the increased risk for COVID-19 severity.6 The benefits of physical activity are well known and include better cardiovascular and immune health;7 however, recommendations for at home or indoors physical activity are limited, and even more so under these exceptional circumstances and social distancing. A study from Italy reported decreased physical activity and significant increases in BMI among normal weight, as well as overweight and obese adults during quarantine.8
The South African government has been actively repatriating citizens from several countries and regions, with the first cohort returned from the initial epicentres of the diseases’ outbreak.3 Repatriated citizens were placed under quarantine in temporary repurposed accommodation where monitoring and surveillance was routinely conducted by government employees for a 14-day period. The state provided services, including all meals and amenities during the quarantine, but movement out of the allocated quarantine room was strictly prohibited. The purpose of this case report is to describe the lifestyle factors and quality of life experiences of a repatriated South African citizen undergoing quarantine in a confined space.
Case report
The participant, Ms X, was a 49-year-old South African citizen, with no known medical history, who had been living and working in a Middle East country. In the latter part of March 2020, most countries introduced COVID-19 lockdown measures, resulting in the revoking of travel and working visas. The embassy arranged and funded an evacuation flight for Ms X and other stranded South Africans in the region. After return to South Africa, citizens were transported to a government site in Johannesburg and underwent mandatory 14-day quarantine. Ms X was allocated a 4 × 4 m2 room with bed and amenities with meals and drinks provided. Military and police personnel monitored the accommodation to ensure persons remained confined to their rooms. Medical staff were on duty to monitor the general health status of people. Extracted nasal and oropharyngeal samples for the detection of COVID-19 were collected by on-call government laboratory staff. Individuals received their test results from the in-house medical personnel. Given the rapid spread of the virus and the urgent need and priority for screening in communities at the time, the repatriated citizens could only be tested in the latter part of the quarantine and, Ms X could only be tested on Day 14.
Ms X provided self-reported height (1.65 m) and weight (68 kg) on Day 1. A cloth measuring tape was made available to measure waist and hip circumferences daily using standard procedures. Circumferences were recorded by Ms X, and body mass index (BMI) was calculated as kg/m2 and waist-to-height ratio (WHtR) was calculated as waist (cm)/height (cm). Daily dietary intake and beverage consumption was diarised and converted to macronutrients (calories, fats, carbohydrates, protein and dietary fibre) using an online conversion application (https://caloriecontrol.org/healthy-weight-tool-kit/food-calorie-calculator/). The short-form health survey (SF-36) was completed online (https://www.orthotoolkit.com/sf-36/) to determine physical health (physical function, role-physical, bodily pain and general health) and mental health (vitality, role-emotional, social function and vitality). Scores ranged from 0 to 100 with higher scores indicating enhanced overall physical and mental health (https://www.orthotoolkit.com/sf-36/). Night-time sleep (hours/night) and estimated sitting time per day were recorded by the study participant.
Ms X followed online curated moderate-to-vigorous home-based/indoor exercise videos requiring no equipment with intermittent stepping during the 14-day quarantine period. The type of exercises performed included continuous aerobic activity, high-intensity interval training and resistance training using body weight. A wireless heart rate (HR) monitor (MZ-3; Myzone Ltd, Isle of Man) was worn during physical exercise and activity. Physiological measures, including peak and average HR, calories expended and exercise intensity (%max) were monitored in real time on a smartphone application and saved on a cloud-based facility (Myzone Ltd., Isle of Man). The number of steps per day and duration spent stepping were recorded using the iPhone Health application on the participant’s personal iPhone.
Ms X remained asymptomatic and tested negative for COVID-19 on Day 14. The self-reported height (1.65 m) and weight (68 kg) did not change since Day 1. The BMI was 25.0 kg/m2, classified as ‘overweight’ or BMI ⩾ 25 kg/m2,9 while waist circumference (82 cm) and hip circumference (102 cm) were constant throughout the 14 days. The WHtR was 0.497, which is just below 0.5, the cut-point for abdominal obesity.10
The average resting HR was 63.8 b/min, ranging from 58 to 73 b/min, while average night-time sleep was 8.4 h/night. Caloric intake fluctuated, with peaks in caloric consumption on the second and fourth quarantine days that ranged from 1617 to 2854 kcal/day (Table 1). Energy contribution from macronutrient intake during the 14-day period was provided mostly by carbohydrates, contributing around 40%–54% to total dietary energy intake on most days, followed by fats (25%–45% of energy) and proteins (15%–25% of energy). Added sugars contributed 4.4%–12.5% of energy per day. The overall quality of life outcomes were initially low and improved towards the end of the quarantine (Table 2).
Table 1.
Dietary intake during quarantine.
| Food consumption | Energy (kcal/day) |
Fat (g/day) | Protein (g/day) | Carbohydrate (g/day) | Added sugar (g/day) |
Sugar (% of energy) |
|---|---|---|---|---|---|---|
| Day 1 | 1997 | 96 | 101 | 182 | 37 | 7.4 |
| Day 2 | 2854 | 139 | 126 | 275 | 65 | 9.1 |
| Day 3 | 2332 | 77 | 112 | 298 | 60 | 10.3 |
| Day 4 | 2668 | 80 | 100 | 387 | 50 | 7.5 |
| Day 5 | 2392 | 82 | 91 | 322 | 65 | 10.9 |
| Day 6 | 2040 | 85 | 77 | 242 | 50 | 9.8 |
| Day 7 | 1617 | 70 | 78 | 169 | 30 | 7.4 |
| Day 8 | 2271 | 92 | 102 | 259 | 25 | 4.4 |
| Day 9 | 2178 | 87 | 100 | 249 | 60 | 11.0 |
| Day 10 | 1963 | 96 | 82 | 193 | 25 | 5.1 |
| Day 11 | 2183 | 100 | 92 | 229 | 30 | 5.5 |
| Day 12 | 1930 | 95 | 90 | 179 | 25 | 5.2 |
| Day 13 | 1793 | 60 | 88 | 225 | 56 | 12.5 |
| Day 14 | 2260 | 92 | 95 | 263 | 35 | 6.2 |
Table 2.
Quality of life measures during quarantine.
| Quality of life | Day 1 | Day 7 | Day 14 |
|---|---|---|---|
| Physical functioning | 40 | 80 | 90 |
| Role limitations due to physical health | 0 | 50 | 100 |
| General health | 65 | 85 | 85 |
| Bodily pain | 80 | 100 | 100 |
| Role limitations due to emotional health | 0 | 33.3 | 33.3 |
| Vitality | 40 | 75 | 75 |
| Social functioning | 12.5 | 50 | 50 |
| Emotional functioning | 28 | 60 | 60 |
Ms X did not participate in physical exercise or walking everyday (Figure 1). Total sitting time was an average of 516 min/day, ranging from 7 to 10 h/day. Time spent stepping ranged from 20 to 49 min/day, spread over the course of each day. However, 10 exercise sessions were completed, with an average effort of 71.8 %Effort/session (62–81 %Effort), average duration of 46.9 min/session (15–75 min/session) and average caloric expenditure of 366 calories expended/session (79–591 calories expended/session).
Figure 1.
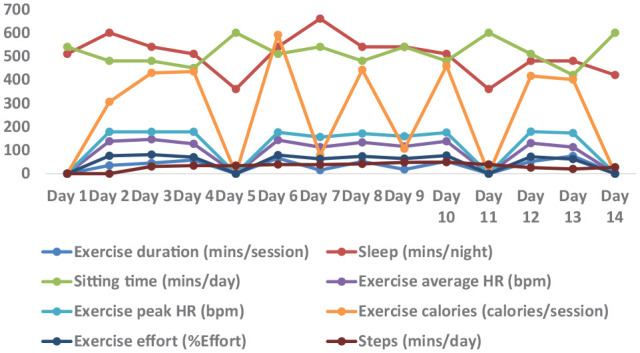
Movement and sedentary behaviour of the participant during mandatory quarantine.
The total time spent in physical activity was 7.82 h over the 14-day period. Physical exercise was completed at a moderate intensity using a mobile application which provided real-time feedback.
Discussion
This study demonstrates positive health outcomes using online exercise videos during a mandatory COVID-19 quarantine; however, these findings require further investigation. Ms X was asymptomatic and did not develop symptoms during the quarantine. On Day 14 of the quarantine, she tested negative for the virus. The health-related quality of life measures were noticeably low at the start of the quarantine and improved towards the end of the quarantine, indicating improved physical and mental health. Improved quality of life measures may in part be related to the structured physical activity and exercise; however, several other undocumented factors could have influenced the outcome.8
Ms X was sufficiently active, accumulating more than the recommended 150 moderate physical activity minutes per week to prevent disease while confined to a small room. Body weight status did not seem to change during the quarantine period, despite relatively high energy intakes, above 2000 kcal/day on 9 out of 14 days.11 On 4 of the 14 days, added sugar intakes were higher than the recommended 10% of the total energy intake.12 Fruit juice, snack bars, yogurt, jam, sugar in hot drinks and cookies were the sources of added sugar. These foods may have been eaten as ‘comfort foods’ in the quarantine situation.13 However, more robust measures of dietary intake, with accurate quantification of serving sizes, are required to confirm the exact levels of intake. All foods were provided in the quarantine setting and the study participant could not go out to buy food at shops. Foods provided included good sources of immuno-supportive nutrients, such as antioxidants, zinc and proteins, from fruit, vegetables, milk, yogurt, meat, poultry and fish.4 A recent study on the immediate impact of the COVID-19 pandemic on eating habits and lifestyle changes of Italian adolescents and adults showed that younger people tended to have an increased appetite when confined to their homes during the pandemic, compared to older adults. Those who took savoury snacks and foods and drink high in sugar after dinner had a higher BMI than their counterparts who did not take snacks.13 Another study among adults in quarantine showed a significant decrease in physical activity and increase in BMI during quarantine.8
Using online resources demonstrates the value of staying physically active during the COVID-19 pandemic. The total time spent in physical activity was 7.82 h over the 14-day period at a moderate intensity. Using a mobile application to provide real-time feedback possibly helped to reach a level of physical activity to prevent the harmful effects of sedentary behaviour under confined living conditions.7 Further health gains were supplemented by disrupting the relatively high sitting time with intermittent indoor walking (stepping) during daylight hours.
The regulations for social isolation and physical distancing are clear and have not generally been followed in South Africa,3 and the abrupt cessation of economic activity and limited movement has not considered the existing obesity and chronic non-communicable diseases (NCDs) crises in the country.14 Older individuals (aged above 60 years) and persons with ⩾ 1 pre-existing conditions and NCDs are at greater risk of more severe outcomes with COVID-19 infection.1 It is therefore important to prevent and address NCDs during this extraordinary period by creating opportunities for physical activity and ensuring healthy eating behaviour with the recommended hygiene practices.15 Recent evidence indicates that opportunities for physical activity during the lockdown are varied and accessible for individuals across the socioeconomic spectrum.16 Online exercise videos and gamified mobile applications are available for free and through recurrent subscription services providing additional features.17 As governments scale up the operation to manage the pandemic, these online tools can provide meaningful support for maintaining health.
The strengths of this study include the robust record of dietary intake and physical activity kept during the 14 days of quarantine. Limitations of this study include that the study participant did not have access to tools to estimate portion sizes of foods accurately and the available database used to calculate the energy and macronutrient intakes may not be complete and nutrient values may not be accurate.
Conclusion
This case report demonstrates that structured indoor activity during confined quarantine contributed to mental health outcomes and prevented weight gain over 14 days, despite prolonged sitting time and high sugar intakes. During the current pandemic and in the presence of limited freedom of movement, sustained physical activity was feasible by accessing online resources, essentially reducing vulnerability to existing cardiovascular health concerns. However, these findings are based on a single participant and, therefore, further study is required.
Acknowledgments
The author (P.J-L.G.) thanks the National Research Foundation of South Africa for their support.
Footnotes
Author contributions: P.J-L.G. conceived the study design. P.J-L.G. and H.S.K. performed the analysis, wrote the article and approved the final version of the article.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethical approval: Ethical approval to report this case was obtained from the Human Research Ethics Committee, University of the Witwatersrand (No. M200679).
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: This research was supported by a grant provided by the National Research Foundation of South Africa (NRF; Grant No. 113366). Any opinion, finding and conclusion or recommendation expressed in this material are those of the author(s) and the NRF does not accept any liability in this regard.
Informed consent: Written informed consent was obtained from the patient(s) for their anonymized information to be published in this article.
ORCID iD: Philippe Jean-Luc Gradidge  https://orcid.org/0000-0001-5225-1184
https://orcid.org/0000-0001-5225-1184
References
- 1. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395: 497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Adhikari SP, Meng S, Wu Y-J, et al. Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of coronavirus disease (COVID-19) during the early outbreak period: a scoping review. Infect Dis Poverty 2020; 9: 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. South African Government. Disaster Management Act: amendment of regulations: coronavirus COVID-19 lockdown, 2020, https://www.gov.za/sites/default/files/gcis_document/202007/43521gon763.pdf
- 4. Muscogiuri G, Barrea L, Savastano S, et al. Nutritional recommendations for CoVID-19 quarantine. Euro J Clin Nutr 2020; 74: 850–851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Int Med 2020; 180: 934–943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Muscogiuri G, Pugliese G, Barrea L, et al. Commentary: obesity: the ‘Achilles heel’ for COVID-19. Metabolism 2020; 108: 154251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hamer M, O’Donovan G, Stamatakis E. Lifestyle risk factors, obesity and infectious disease mortality in the general population: linkage study of 97,844 adults from England and Scotland. Prev Med 2019; 123: 65–70. [DOI] [PubMed] [Google Scholar]
- 8. Barrea L, Pugliese G, Framondi L, et al. Does Sars-Cov-2 threaten our dreams? Effect of quarantine on sleep quality and body mass index. J Trans Med 2020; 18: 318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. World Health Organization. Obesity. Preventing and managing the global epidemic. Geneva: World Health Organization, 1998. [PubMed] [Google Scholar]
- 10. Ware LJ, Rennie KL, Kruger HS, et al. Evaluation of waist-to-height ratio to predict 5 year cardiometabolic risk in sub-Saharan African adults. Nutr Metab Cardiovasc Dis 2014; 24(8): 900–907. [DOI] [PubMed] [Google Scholar]
- 11. U.S. Department of Health and Human Services and U.S. Department of Agriculture. 2015–2020 dietary guidelines for Americans. 8th ed., 2015, https://health.gov/our-work/food-nutrition/2015-2020-dietary-guidelines/guidelines/
- 12. World Health Organization. Guideline: sugars intake for adults and children. Geneva: World Health Organization, 2015. [PubMed] [Google Scholar]
- 13. Di Renzo L, Gualtieri P, Pivari F, et al. Eating habits and lifestyle changes during COVID-19 lockdown: an Italian survey. J Trans Med 2020; 18: 229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. NCD| Risk Factor Collaboration (NCD-RisC) – Africa Working Group. Trends in obesity and diabetes across Africa from1980 to 2014: an analysis of pooled population-based studies. Int J Epidemiol 2017; 46: 1421–1432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kluge HHP, Wickramasinghe K, Rippin HL, et al. Prevention and control of non-communicable diseases in the COVID-19 response. Lancet 2020; 395: 10238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lippi G, Henry BM, Sanchis-Gomar F. Physical inactivity and cardiovascular disease at the time of coronavirus disease 2019 (COVID-19). Euro J Prevent Cardiol 2020; 27(9): 906–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hammami A, Harrabi B, Mohr M, et al. Physical activity and coronavirus disease 2019 (COVID-19): specific recommendations for home-based physical training. Managing Sport and Leisure. Epub ahead of print 1 April 2020. DOI: 10.1080/23750472.2020.1757494. [DOI] [Google Scholar]


