Abstract
The pandemic of the new coronavirus (COVID-19) may be affecting the physical activity (PA) level in much of the population. This study aimed to investigate the prevalence of physical inactivity and sedentary behavior (SB) among adults with chronic diseases and their associations with sociodemographic factors during the COVID-19 pandemic. This cross-sectional study included 249 participants (age: 18–91 years; 61.4% female) with chronic conditions and attended the Family Health Strategy program in a small town in Brazil. Data were collected between 2020-07–13 and 2020-07-24 by face-to-face interviews. Self-reported PA, sitting time, chronic diseases, medication use, sociodemographic data, and self-isolation adherence were obtained by questionnaire. During this specific time point of the COVID-19 pandemic, 71.5% of participants did not meet the PA recommendations (≥500 METs-min/week), and the prevalence of SB risk (≥4 h sitting) was 62.7%. Adjusted logistic regression indicated that male participants (odds ratio [OR]: 1.89 [95% CI 1.02–3.53]), living alone (OR: 2.92 [95% CI 1.03–8.30]) or in a two-person household (OR: 2.32 [95% CI 1.16–4.63]), and those who reported sometimes performing self-isolation (OR: 3.07 [95% CI 1.47–6.40]) were more likely to meet the minimum PA recommendations. Current smokers had a lower odds (OR: 0.36 [95% CI 0.14–0.95]) of meeting the PA recommendations. Older participants (OR: 2.18 [95% CI 1.06–4.50]) and those who had multimorbidity (OR: 1.92 [95% CI 1.07–3.44]) were more likely to have a higher degree of SB. There is an urgent need to mitigate physical inactivity and SB, and public health interventions must take into account sociodemographic status.
Keywords: Moderate-to-vigorous physical activity, Sitting time, Morbidity, Coronavirus, Quarantine
Introduction
Its rapid spread, coupled with government authorities' inaction, led the World Health Organization to declare the outbreak by COVID-19 a pandemic.1 In this context, social distancing measures (such as restricting events requiring a physical presence, closing schools and non-essential businesses, and recommendations to stay at home) have been implemented to reduce the virus contagion and avoid the collapse of health care systems.2 On the other hand, these social distance measures have decreased the practice of moderate-to-vigorous intensity physical activities (PA) and have increased sedentary behavior (SB).3,4
As physical inactivity and SB have serious health implications in the short term,5, 6, 7 the incentive to maintain a good PA level becomes a vital ally to health in times of a pandemic.8,9 A physically active lifestyle is even more relevant for subjects with chronic diseases since PA is indicated for their control and treatment.10 Related to this, as more severe cases of COVID-19 are associated with chronic diseases,11 the regular practice of PA can play an essential role in improving the functioning of the immune system and reducing systemic inflammation, which are essential factors to decrease the severity of viral respiratory infections.10
Although online survey studies have been conducted to verify the impact of the COVID-19 pandemic on PA and SB aspects,12, 13, 14, 15 to the best of our knowledge, no study has collected data through face-to-face interviews. Face-to-face interviews allow the researcher to clarify specific questions (such as duration and intensity of daily physical activities), engage responders, and provide higher quality data. In contrast, an internet-based survey is restricted participants with internet access, tending to lead to a bias selection and making it challenging to achieve representativeness of the investigated sample (external validity).16
The COVID-19 pandemic does not affect everyone equally, especially in countries with high levels of social inequality.17 Understanding how the sociodemographic profile has impact behaviors is relevant to public health authorities, which can propose strategic actions to mitigate other pandemic adverse effects. Therefore, this study aimed to investigate, through face-to-face interviews, the prevalence of physical inactivity and SB among adults with chronic diseases and their associations with sociodemographic factors during the COVID-19 pandemic.
Methods
A cross-sectional study was conducted between July 13 and 24, 2020 (the winter period) to investigate the prevalence of following the PA recommendations, SB, and their associations with sociodemographic factors in adults with chronic diseases (≥18 years) who were residents of Piranguinho during the COVID-19 pandemic.
Piranguinho is a small city in the state of Minas Gerais, located in the southern region of Brazil (latitude: 22° 24′ 3''/longitude: 45° 32′ 6″). The city occupies an area of 124.803 km2, with a demographic density of 64.23 inhab/km2. In 2010 (last population census—IBGE), the entire population consisted of 8016 inhabitants, and the urban population corresponded to 4953 residents. The human development index (HDI) was 0.717, and the dimension that most contributed to the HDI was life expectancy, with an index of 0.841, followed by per capita income with an index of 0.672, and education with an index of 0.651.
The first confirmed case of COVID-19 in Piranguinho was diagnosed on May 12, 2020. On April 13, the city officially recognized the state of public calamity resulting from the COVID-19 pandemic. Social distancing policies were implemented, including the closure of schools, gyms, churches, and non-essential businesses, and public and private events of any kind were prohibited. During the research period, the number of suspected cases reported were between 113 and 134, and confirmed cases were between 21 and 27.
The city has adopted the Family Health Strategy (FHS) for the reorganization of primary care and has three teams responsible for serving three areas of the city, which includes both the urban and rural territories. This study was developed in partnership with the local health department to help the FHS program, which is responsible for monitoring citizens with chronic diseases. The study sample size calculation was based on the numbers of adult patients registered in the FHS databases (n = 911), considering an estimated physical inactivity prevalence of 70%, a sampling error of 5%, and a 95% confidence interval. The minimum recommended sample size was 239 participants. The sampling process was conducted by an independent researcher who was responsible for coding and allocating 300 participants (100 participants in each of the three areas) using a random sequence generator (www.randomizer.org).
4 postgraduate students in Human Movement Science with previous research fieldwork experience accompanied the health agents and were responsible for the face-to-face interviews. A prior pilot study was conducted in a random sample (n = 20) to simulated the interviews and permitted a standardization of the researchers' approach. During visits, all research staff used safety equipment (laboratory coats, gloves, masks, and face shields), and the interviews were carried out at a safe distance (2 steps). The pens and clipboard used were cleaned with 70% alcohol after each interview.
In the first stage of the interview, sociodemographic and lifestyle factors data were collected, including age, sex, self-reported body weight and height (for calculating body mass index [BMI]), skin color (divided into white or nonwhite), employment status (retired, unemployed, employed), monthly total family income (≤R$ 1.039.00, between R$ 1039.01 and ≤R$ 3117.00, and >R$ 3117.00), education (primary or less, secondary and further), the number of people in the household, and current smoking (yes or no). The compliance with self-isolation was assessed using the question: “Concerning the social distancing that is being suggested by health authorities, that is, staying at home and avoiding contact with other people, how well do you think you are following these recommendations?” The alternatives were: (a) I am not following them; (b) sometimes I follow them; (c) I am following them.
In the second stage of the interview, information to determine states of polypharmacy and multimorbidity were collected. Briefly, the participants were asked to bring all containers of the medicines they had used in the last 15 days. For the analysis, we included only regularly consumed medicines prescribed by a physician or dentist, and polypharmacy was defined as the regular use of ≥5 drugs.18 The presence of chronic disease was based on self-reported physician diagnosis of one or more of the following conditions (except for obesity, determined by BMI ≥30 kg/m2): hypertension, diabetes, cardiovascular disease, hypercholesterolemia, pulmonary disease, renal disease, cancer, and depression. We defined multimorbidity as the presence of ≥3 conditions in one individual.19
In the third stage of the interview, the short version of the International Physical Activity Questionnaire (IPAQ) was applied, and the participants reported over the last 7 days the frequency and amount of time spent in moderate-to-vigorous physical activities (MVPA) in bouts ≥10 min.20 The responders received brief prompts to help them remember past physical activities events (type, intensity, and duration), when necessary, starting at the most recent day until complete the last week. The energy expenditure in walking activities (3.3 Metabolic Equivalents [METs]), in moderate activities (4.0 METs), and vigorous activities (8.0 METs) were quantified as MET-min/week.21 The cutoff point score used (<or ≥500 MET-min/week) was based on the most recent recommendations of the aerobic component proposed by the ACMS.22 The SB was determined by asking about the total time spent sitting in the last 7 days. The sedentary risk was defined as spending ≥4 h per day sitting.23
After the interviews, the participants were instructed on the importance of physical isolation measures during the COVID-19 pandemic and they were given a printed infographic (plasticized and sanitized) with instructions on how to stay active at home and avoid prolonged sedentary activities. This research was approved by the local Research Ethics Committee (protocol number 4.152.055) and complied with resolution 466/12 of the National Health Council. All participants that agreed to participate in the study signed a Free and Informed Consent Form after being informed about the research protocol.
For the analysis, the data were entered into an Excel datasheet, were double-checked, and then imported into SPSS software (version 20; Chicago, IL, USA). The categorical variables are presented as percentages and 95% confidence intervals (95% CI). Continuous variables are presented as the median and interquartile range (IQR; 25%–75%). The associations between sociodemographic and health factors (independent variables) with meeting the minimum PA recommendations (≥500 METs-min/week) and sedentary risk (sitting time ≥4 h) were assessed by logistic regression. Two models were calculated (odds ratio [OR] and 95% CI): (a) a non-adjusted (crude model) and (b) a model adjusted for sex, age, ethnic group, environment, employment, family income, education, number of people in the household, and current smoking. The significance level was set at p < 0.05.
Results
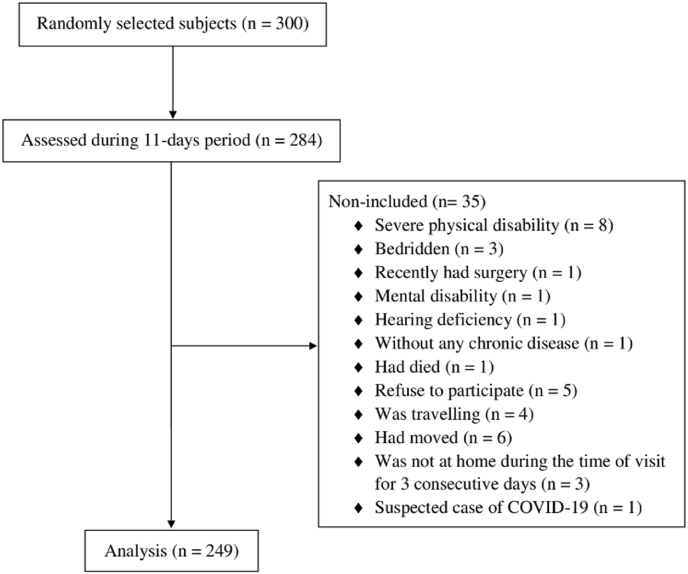
Of the 300 randomly selected subjects, the research team was able to meet with 284 during the eleven days of the study period, and 249 participants were finally included in the analysis. Fig. 1 shows the flowchart of the study.
Fig. 1.
Flowchart of the study.
The characteristics of the study participants are shown in the supplementary file. The median age of the participants was 64 years, ranging from 18 to 91 years. The median value of total PA was 198.0 METs-min/week, and 71.5% (95% IC: 65.6–76.7) of the participants did not meet the PA recommendations (≥500 METs-min/week). At the same time, 34.1% (95% IC: 28.5–40.2) of the participants did not ever perform any single MVPA in bouts ≥10 min. The median value of sitting weekday time was 4.0 h, and the prevalence of SB risk (≥4 h) was 62.7% (95% IC 56.5–68.4).
The majority of participants were female (61.4%), aged ≥60 years (60.2%), declared to have white skin (63.1%), lived in the urban area (63.1%), were retired (45.8%), has a monthly total family income between R$ 1039.00–3117.00 (53.4%), had only a primary education or less (54.6%), not currently smoking (85.9%), lived with three or more other residents (59.0%), and reported that they were in self-isolation during the period the data were being collected (67.1%). Regarding chronic diseases, the most frequent morbidities were hypertension (91.2%), hypercholesterolemia (40.2%), obesity (39.0%), and diabetes (35.7%). The prevalence of multimorbidity (≥3 conditions) was 48.6%, and polypharmacy (≥5 medications) was 25.7%.
The association of sociodemographic and health factors with PA recommendations and SB is presented in Table 1. The results of the adjusted logistic regression analysis indicated that male participants (OR: 1.89 [95% CI: 1.02–3.53]), living alone (OR: 2.92 [95% IC: 1.03–8.30]) or with two people in the household (OR: 2.32 [95% IC: 1.16–4.63]), and those who reported that sometimes they performed self-isolation (OR: 3.07 [95% IC: 1.47–6.40]) had a higher likelihood of meeting the minimum PA recommendations. On the other hand, current smoking participants had a lower chance (OR: 0.36 [95% IC: 0.14–0.95]) of meeting the PA recommendations. Regarding SB, older participants (OR: 2.18 [95% IC: 1.06–4.50]) and those with multimorbidity (OR: 1.92 [95% IC: 1.07–3.44]) had a higher likelihood of sitting ≥4 h per day.
Table 1.
Logistic association of sociodemographic and health factors with PA recommendations and sedentary behavior during the COVID-19 pandemic.
| Variables | ≥500 METs-min/week |
≥4 h Sitting |
||
|---|---|---|---|---|
| Crude Analysis |
Adjusted Analysis |
Crude Analysis |
Adjusted Analysis |
|
| OR (95% CI) | OR (95% CI) ∗ | OR (95% CI) | OR (95% CI) ∗ | |
| Sex | ||||
| Female | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Male | 1.86 (1.07–3.26) | 1.89 (1.02–3.53) | 0.69 (0.41–1.17) | 0.61 (0.34–1.11) |
| Age | ||||
| 18–59 y | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| ≥60 y | 0.74 (0.42–1.28) | 0.49 (0.23–1.06) | 2.04 (1.21–3.46) | 2.18 (1.06–4.50) |
| Ethnic Group | ||||
| White | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Others | 1.16 (0.65–2.04) | 1.41 (0.76–2.60) | 1.11 (0.65–1.89) | 1.11 (0.63–1.95) |
| Living Place | ||||
| Urban | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Rural | 1.07 (0.60–1.88) | 1.04 (0.56–1.96) | 0.77 (0.45–1.30) | 0.68 (0.38–1.22) |
| Employment | ||||
| Retired | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Unemployed | 0.75 (0.40–1.41) | 0.81 (0.36–1.78) | 0.83 (0.46–1.48) | 0.94 (0.44–1.97) |
| Employed | 1.18 (0.57–2.42) | 1.06 (0.41–2.73) | 0.48 (0.24–0.96) | 0.79 (0.32–1.94) |
| Family Income | ||||
| <R$1.039 | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| R$1039–3117 | 1.34 (0.68–2.64) | 1.48 (0.70–3.13) | 1.12 (0.60–2.07) | 1.28 (0.65–2.51) |
| >R$ 3117 | 1.34 (0.59–3.06) | 1.67 (0.63–4.42) | 0.62 (0.29–1.31) | 0.77 (0.33–1.83) |
| Education | ||||
| Primary or Less | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Secondary | 1.46 (0.82–2.57) | 1.44 (0.73–2.84) | 0.97 (0.57–1.66) | 1.61 (0.84–3.08) |
| Further | 1.50 (0.42–5.30) | 0.74 (0.17–3.18) | 0.40 (0.12–1.33) | 0.69 (0.17–2.88) |
| Household | ||||
| ≥3 people | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| ≤2 people | 1.76 (0.96–3.22) | 2.32 (1.16–4.63) | 1.53 (0.86–2.73) | 1.52 (0.80–2.88) |
| Living Alone | 1.69 (0.69–4.14) | 2.92 (1.03–8.30) | 3.15 (1.13–8.81) | 2.85 (0.93–8.74) |
| Current Smoking | ||||
| No | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Yes | 0.59 (0.23–1.41) | 0.36 (0.14–0.95) | 0.76 (0.37–1.58) | 0.86 (0.39–1.92) |
| Multimorbidity | ||||
| No | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Yes | 0.76 (0.44–1.32) | 0.79 (0.43–1.46) | 1.90 (1.12–3.20) | 1.92 (1.07–3.44) |
| Polypharmacy | ||||
| No | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Yes | 0.43 (0.21–0.89) | 0.47 (0.22–1.00) | 1.58 (0.86–2.91) | 1.30 (0.67–2.51) |
| Self-Isolation | ||||
| Yes | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Sometimes | 2.56 (1.35–4.84) | 3.07 (1.47–6.40) | 0.98 (0.52–1.85) | 1.19 (0.59–2.41) |
| No | 0.70 (0.25–1.96) | 0.61 (0.20–1.88) | 0.60 (0.27–1.37) | 0.61 (0.24–1.53) |
∗Adjusted for sex, age, ethnicity, living place, employment, family income, education, number of people in the household, and current smoking. Bold values denote statistical significance (p-value less than 0.05).
Discussion
The current study investigated a sample of adults with chronic diseases included in the public health care system in a small town in Brazil to describe the effects of the COVID-19 pandemic on compliance with PA recommendations and SB as assessed by an internationally validated questionnaire. The prevalence data of physical inactivity and SB risk indicated that 71.5% of adults with chronic diseases did not meet the minimum PA recommendations, and 62.7% spent at least 4 h sitting per day. One notable fact was that one-third of the participants did not perform any MVPA at all in bouts ≥10 min.
Although our cross-sectional study design is unable to reveal their physical inactivity and SB levels prior to the pandemic, they are likely to have increased due to the restrictions imposed by the COVID-19 pandemic. Online and telephone survey studies conducted in Spain indicated that responders with chronic diseases perceived decreases in PA and increases in SB.13,24 Briefly, López-Sánchez et al.13 observed a significant decrease in self-reported moderate-intensity physical activity in adults with chronic conditions (n = 163) during the COVID-19 quarantine compared to the before period (60.5 vs. 90.5 min/day). Furthermore, Ruiz-Roso et al.24 also showed that participants with type II Diabetes (n = 72) reported lower mean time spent in walking/moderate activities and increased sitting time per week assessed by the IPAQ questionnaire in the COVID-19 lockdown period compared to before. Direct comparison with these findings is complicated and should be interpreted with caution due to the difference in survey strategies, and the memory recalls to the period before the pandemic can undoubtedly present a high bias level. Thus, the current study expands on these findings showing that face-to-face interviews project a high level of physical inactivity in adults with chronic diseases during the COVID-19 pandemic.
Therefore, public health strategies that also mitigate the effects of a pandemic scenario on PA levels are urgent, and this study adds to our understanding of the factors associated with not meeting the PA recommendations and SB risk. Our findings indicated an association between not meeting the PA recommendations with current smoking and female sex, and this is consistent with previous studies that showed a higher rate of physical inactivity among smokers25 and women.26 We observed that the number of people in the household during the pandemic was also a factor that influenced not meeting the PA recommendations, and participants that lived alone or with only one other person were more likely to meet the minimum PA recommendations. This can possibly be related to a greater need for more household duties of light intensity when a larger number of people live in the household, limiting free time and decreasing motivation to perform MVPA.27
Additionally, participants that reported that they sometimes performed self-isolation were three times more likely to meet the minimum PA recommendation than those that were fully observing self-isolation after controlling for any potentially confounding factors. One may speculate that these participants may be performing some MVPA outdoors and therefore be more likely to remain physically active during the pandemic. On the other hand, the participants who reported not self-isolating were no more or less active than those who performed self-isolation. We hypothetically suggested that these participants could be involved in formal or informal work outside the home and could not perform continuous (≥10 min) MVPA.
It is important to note that these data are not related to a lockdown condition, even though most participants reported respecting the social isolation measures proposed by the local health authorities. The short version of the IPAQ questionnaire does not ask about light-intensity activities that are most predominant inside the house (i.e., cleaning the house, cooking, home office working) among self-isolating subjects. Recent studies have suggested that just replacing sedentary time with light-intensity activities reduces the risk of chronic diseases,28 but the instrument used in the current study cannot make this inference. Another aspect was that the survey was carried out during the winter period. Nevertheless, it is important to highlight that the city has an average annual temperature of 19.5 C° with little variation throughout the year (15.5 C° July and 22.3 °C February) and probably may not have drastically affected PA patterns due to weather.
SB is another PA domain that has attracted increased interest in recent years. It is characterized as any waking behavior of low energy expenditure (≤1.5 METs), while in a sitting, reclining or lying posture. Emerging evidence has shown that prolonged sedentary time is associated with health conditions and mortality, independent of PA levels.29 In our study, we used total sitting time as a proxy measure of SB, and the results indicated that older adult participants (≥60 years) had a two times higher chance of sitting ≥4 h. These findings are supported by other studies that reported that increasing age is associated with high sedentary risk.30 Our data also indicate that participants with ≥3 chronic conditions had higher odds of spending more time sitting, similar to those found by Kandola et al.31 Experimental studies have found that prolonged time spent sitting impacts acute metabolic and inflammatory responses that may contribute to the development of chronic diseases,32,33 and thus, it should be avoided.
The major strength of this study is that it used face-to-face interviews, and the sampling method adopted allowed for the inclusion of broad sociodemographic characteristics while avoiding bias selection, as is observed in studies using online surveys. The face-to-face interview technique can also minimize falsely and nonresponse rates and provide some other information that would not have been captured in an online survey. Another strength is the use of the IPAQ, a validated questionnaire that allows for comparisons with other regions of Brazil and with different countries. Among the limitations of the study, we can first highlight that no self-reported information was raised about PA and SB level before the COVID-19 pandemic, and we can not infer how much the behavior was affected. Second, the use of objectively measured physical activity monitors could provide a more accurate estimation of PA levels. Third, we considered only compliance with the aerobic component of the PA recommendations. Fourth, the multimorbidity analysis was limited to counts of self-reported cases, and the severity of the chronic diseases was not assessed. Last, the use of a cross-sectional design precludes any evaluation of a causal association regarding the results.
In conclusion, the results of the current study showed that more than half of adults with chronic diseases living in a small town in Brazil did not adhere to the minimum PA recommendations and had a high sedentary risk. Our study indicated that factors like male sex, fewer people in the household, and less adherence to self-isolation were associated with meeting the minimum PA recommendations. At the same time, increased age and multimorbidities were positively associated with a higher sedentary risk. Therefore, we suggest that public health policies should inform and encourage people with chronic diseases to maintain or increase their PA level safely at home to mitigate adverse effects of physical inactivity, especially during the periods of more severe control of the pandemic. Besides, older people or those with multimorbidities that may have physical limitations should be encouraged to reduce sitting time.
Ethical approval statement
This research was approved by the local Research Ethics Committee (protocol number 4.152.055), and all participants signed an informed consent form prior to participation.
Authors’ contributions
Jean Marinho da Silva: Conceptualization, Data curation, data collection. Rozangela Verlengia: Conceptualization, Project administration, administration. José Jonas de Oliveira: Data curation, data collection. Anna Gabriela Silva Vilela Ribeiro: Data curation, data collection. Carolina Gabriela Reis Barbosa: Data curation, data collection. Uliana Sbeguen Stotzer: Conceptualization, Project administration, administration. Alex Harley Crisp: Conceptualization, administration, Formal analysis, analysis. All authors interpreted the data and participated of critical revision and final approval.
Submission statement
The Manuscript has not been published and is not under consideration for publication elsewhere.
Conflict of interest
The authors have no conflict of interest to report.
Acknowledgments
The authors would like to thank the health department of the city Piranguinho, and CAPES for the financial support through scholarships – Finance Code 001.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.smhs.2020.11.002.
Appendix A. Supplementary data
The following is the supplementary data to this article:
References
- 1.Mahase E. Covid-19: WHO declares pandemic because of "alarming levels" of spread, severity, and inaction. BMJ. 2020;368:m1036. doi: 10.1136/bmj.m1036. [DOI] [PubMed] [Google Scholar]
- 2.Aquino E.M.L., Silveira I.H., Pescarini J.M., et al. Social distancing measures to control the COVID-19 pandemic: potential impacts and challenges in Brazil. Ciência Saúde Coletiva. 2020;25(suppl 1):2423–2446. doi: 10.1590/1413-81232020256.1.10502020. [DOI] [PubMed] [Google Scholar]
- 3.Peçanha T., Goessler K.F., Roschel H., Gualano B. Social isolation during the COVID-19 pandemic can increase physical inactivity and the global burden of cardiovascular disease. Am J Physiol Heart Circ Physiol. 2020;318(6):H1441–H1446. doi: 10.1152/ajpheart.00268.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Narici M., De Vito G., Franchi M., et al. Impact of sedentarism due to the COVID-19 home confinement on neuromuscular, cardiovascular and metabolic health: physiological and pathophysiological implications and recommendations for physical and nutritional countermeasures. Eur J Sport Sci. 2020:1–22. doi: 10.1080/17461391.2020.1761076. [DOI] [PubMed] [Google Scholar]
- 5.Krogh-Madsen R., Thyfault J.P., Broholm C., et al. A 2-wk reduction of ambulatory activity attenuates peripheral insulin sensitivity. J Appl Physiol. 1985;108(5):1034–1040. doi: 10.1152/japplphysiol.00977.2009. 2010. [DOI] [PubMed] [Google Scholar]
- 6.Knudsen S.H., Hansen L.S., Pedersen M., et al. Changes in insulin sensitivity precede changes in body composition during 14 days of step reduction combined with overfeeding in healthy young men. J Appl Physiol. 1985;113(1):7–15. doi: 10.1152/japplphysiol.00189.2011. 2012. [DOI] [PubMed] [Google Scholar]
- 7.Nolan P.B., Keeling S.M., Robitaille C.A., Buchanan C.A., Dalleck L.C. The effect of detraining after a period of training on cardiometabolic health in previously sedentary individuals. Int J Environ Res Publ Health. 2018;15(10) doi: 10.3390/ijerph15102303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen P., Mao L., Nassis G.P., Harmer P., Ainsworth B.E., Li F. Coronavirus disease (COVID-19): the need to maintain regular physical activity while taking precautions. J Sport Health Sci. 2020;9(2):103–104. doi: 10.1016/j.jshs.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lippi G., Henry B.M., Sanchis-Gomar F. Physical inactivity and cardiovascular disease at the time of coronavirus disease 2019 (COVID-19) Eur J Prev Cardiol. 2020;27(9):906–908. doi: 10.1177/2047487320916823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sallis J.F., Pratt M. Multiple benefits of physical activity during the Coronavirus pandemic. Rev Bras Ativ Fís Saúde. 2020 doi: 10.12820/rbafs.25e0112. 25e0112. [DOI] [Google Scholar]
- 11.Liu H., Chen S., Liu M., Nie H., Lu H. Comorbid chronic diseases are strongly correlated with disease severity among COVID-19 patients: a systematic review and meta-analysis. Aging Dis. 2020;11(3):668–678. doi: 10.14336/AD.2020.0502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.He M., Xian Y., Lv X., He J., Ren Y. Changes in body weight, physical activity, and lifestyle during the semi-lockdown period after the outbreak of COVID-19 in China: an online survey. Disaster Med Public Health Prep. 2020:1–6. doi: 10.1017/dmp.2020.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lopez-Sanchez G.F., Lopez-Bueno R., Gil-Salmeron A., et al. Comparison of physical activity levels in Spanish adults with chronic conditions before and during COVID-19 quarantine. Eur J Publ Health. 2020 doi: 10.1093/eurpub/ckaa159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schuch F.B., Bulzing R.A., Meyer J., et al. Associations of moderate to vigorous physical activity and sedentary behavior with depressive and anxiety symptoms in self-isolating people during the COVID-19 pandemic: a cross-sectional survey in Brazil. Psychiatr Res. 2020;292:113339. doi: 10.1016/j.psychres.2020.113339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smith L., Jacob L., Butler L., et al. Prevalence and correlates of physical activity in a sample of UK adults observing social distancing during the COVID-19 pandemic. 2020;6(1) doi: 10.1136/bmjsem-2020-000850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gunter B., Nicholas D., Huntington P., Williams P. Online versus offline research: implications for evaluating digital media. ASLIB Proc. 2002;54(4):229–239. doi: 10.1108/00012530210443339. [DOI] [Google Scholar]
- 17.Baqui P., Bica I., Marra V., Ercole A., van der Schaar M. Ethnic and regional variations in hospital mortality from COVID-19 in Brazil: a cross-sectional observational study. Lancet Glob Health. 2020;8(8):e1018–e1026. doi: 10.1016/S2214-109X(20)30285-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bielemann R.M., Silveira M.P.T., Lutz B.H., et al. Objectively measured physical activity and polypharmacy among Brazilian community-dwelling older adults. J Phys Activ Health. 2020:1–7. doi: 10.1123/jpah.2019-0461. [DOI] [PubMed] [Google Scholar]
- 19.Gnadinger M., Herzig L., Ceschi A., et al. Chronic conditions and multimorbidity in a primary care population: a study in the Swiss Sentinel Surveillance Network (Sentinella) Int J Publ Health. 2018;63(9):1017–1026. doi: 10.1007/s00038-018-1114-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Matsudo S., Araújo T., Matsudo V., et al. Questionário internacional de atividade física (Ipaq): estupo de validade e reprodutibilidade no Brasil. Rev Bras Ativ Fís Saúde. 2001;6(2):5–18. doi: 10.12820/rbafs.v.6n2p5-18. [DOI] [Google Scholar]
- 21.Cimarras-Otal C., Calderon-Larranaga A., Poblador-Plou B., et al. Association between physical activity, multimorbidity, self-rated health and functional limitation in the Spanish population. BMC Publ Health. 2014;14:1170. doi: 10.1186/1471-2458-14-1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Garber C.E., Blissmer B., Deschenes M.R., et al. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334–1359. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 23.Werneck A.O., Baldew S.S., Miranda J.J., et al. Physical activity and sedentary behavior patterns and sociodemographic correlates in 116,982 adults from six South American countries: the South American physical activity and sedentary behavior network (SAPASEN) Int J Behav Nutr Phys Activ. 2019;16(1):68. doi: 10.1186/s12966-019-0839-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ruiz-Roso M.B., Knott-Torcal C., Matilla-Escalante D.C., et al. COVID-19 lockdown and changes of the dietary pattern and physical activity habits in a cohort of patients with type 2 diabetes mellitus. Nutrients. 2020;12(8) doi: 10.3390/nu12082327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kaczynski A.T., Manske S.R., Mannell R.C., Grewal K. Smoking and physical activity: a systematic review. Am J Health Behav. 2008;32(1):93–110. doi: 10.5555/ajhb.2008.32.1.93. [DOI] [PubMed] [Google Scholar]
- 26.Mielke G.I., da Silva I.C.M., Kolbe-Alexander T.L., Brown W.J. Shifting the physical inactivity curve worldwide by closing the gender gap. Sports Med. 2018;48(2):481–489. doi: 10.1007/s40279-017-0754-7. [DOI] [PubMed] [Google Scholar]
- 27.Puciato D. Sociodemographic associations of physical activity in people of working age. Int J Environ Res Publ Health. 2019;16(12) doi: 10.3390/ijerph16122134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Del Pozo-Cruz J., Garcia-Hermoso A., Alfonso-Rosa R.M., et al. Replacing sedentary time: meta-analysis of objective-assessment studies. Am J Prev Med. 2018;55(3):395–402. doi: 10.1016/j.amepre.2018.04.042. [DOI] [PubMed] [Google Scholar]
- 29.Panahi S., Tremblay A. Sedentariness and health: is sedentary behavior more than just physical inactivity? Front Public Health. 2018;6:258. doi: 10.3389/fpubh.2018.00258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Diaz K.M., Howard V.J., Hutto B., et al. Patterns of sedentary behavior in US middle-age and older adults: the REGARDS study. Med Sci Sports Exerc. 2016;48(3):430–438. doi: 10.1249/MSS.0000000000000792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kandola A., Stubbs B., Koyanagi A. Physical multimorbidity and sedentary behavior in older adults: findings from the Irish longitudinal study on ageing (TILDA) Maturitas. 2020;134:1–7. doi: 10.1016/j.maturitas.2020.01.007. [DOI] [PubMed] [Google Scholar]
- 32.Yates T., Edwardson C.L., Celis-Morales C., et al. Metabolic effects of breaking prolonged sitting with standing or light walking in older south asians and white Europeans: a randomized acute study. J Gerontol A Biol Sci Med Sci. 2020;75(1):139–146. doi: 10.1093/gerona/gly252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Grace M.S., Formosa M.F., Bozaoglu K., et al. Acute effects of active breaks during prolonged sitting on subcutaneous adipose tissue gene expression: an ancillary analysis of a randomised controlled trial. Sci Rep. 2019;9(1):3847. doi: 10.1038/s41598-019-40490-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.