Abstract
Background
Elective orthopaedic operations were suspended at the start of the COVID-19 lockdown. Three pathways were created to allow patients to undergo urgent elective operations in NHS Tayside as soon as it was deemed safe to do so.
Methods
We examined elective orthopaedic activity in NHS Tayside during and immediately after the Scottish lockdown. Elective operations performed between 27 March 2020 and 10 August 2020 were included and compared with cases performed between 27 March and 10 August in both 2018 and 2019. Primary outcomes were 30-day mortality, 30-day complications, and nosocomial infection rates of COVID-19.
Findings
Fewer elective operations were performed in 2020 (258) compared with 2019 (1196) and 2018 (1261). The rate of nosocomial infection in the 2020 cohort was 0%. The 30-day mortality rate was 0%. Over 98% of patients agreed to undergo surgery after a detailed consenting process.
Interpretation
We were able to re-start a safe elective orthopaedic service in the early stages of recovery from the COVID-19 pandemic, compatible with the guidelines set by the Royal College of Surgery of England and the British Orthopaedic Association. Our findings will serve to reassure regions with sufficient resources that it is acceptable to restart elective surgery for urgent priority cases. They may provide a template for planned surgical care in the event of further pandemics.
Keywords: Elective, Orthopaedics, SARS CoV 2, COVID-19, Pathway
Introduction
The World Health Organisation was first alerted that there were cases of viral pneumonia in Wuhan, People's Republic of China, on the 31 December 2019.1
Scotland went into “lockdown” on the 24 March 2020 with the intention of slowing the rate of infection so as not to overload the National Health Service (NHS). There were approximately 300 new cases of coronavirus disease 2019 (COVID-19) per day in Scotland during April and this number gradually reduced to under 10 new cases per day in July.2
An international consensus quickly developed that patients infected with COVID-19 should not undergo elective surgery due to increased morbidity and mortality.3 A variety of musculoskeletal symptoms have been attributed to infection with COVID-19 which may interfere with patients post-operative recovery.4 It was therefore considered appropriate to pause elective activity, both to free up resources to care for sick patients and to better understand the proposed risks to patients in undergoing operations. COVID-19 may have a prolonged incubation period during which transmission of the virus is possible, and reverse transcriptase polymerase chain reaction (RT-PCR) testing for the virus may have a false negative rate of up to 20%.5 These challenges mean there is no guaranteed method to ensure patients are disease free.
There was a huge decrease in planned operations performed in Scotland after lockdown was initiated, as demonstrated in Table 1 .6 Elective orthopaedic surgery in NHS Tayside was suspended on the 27th March 2020.
Table 1.
Planned operations performed in Scotland.
| Month | 2019 | 2020 | Reduction |
|---|---|---|---|
| January | 29,271 | 28,863 | |
| February | 27,762 | 27,645 | |
| March | 29,646 | 20,192 | 32% |
| April | 27,204 | 3406 | 87% |
| May | 29,672 | 4120 | 86% |
| June | 26,941 | 6984 | 74% |
Foregoing all planned surgery indefinitely, under the debatable assumption that it is “safer”, is simplistic and needs to be reviewed when new information on the risk of the disease is known. It is important to resume elective operations as soon possible to minimise unnecessary suffering. Guidelines have been prepared by the British Orthopaedic Association (BOA) and the Royal College of Surgeons of England (RCS Eng) to assist with safely resuming elective surgery.7 Key considerations are that there should be a sustained reduction in the local cases of COVID-19, sufficient testing resources for both staff and patients, adequate personal protective equipment (PPE) and adequate coordination to ensure a safe and efficient service.
It is important to employ a robust system reflecting clinical priority. Guidance was published by NHS England in collaboration with the British Orthopaedic Association and Royal Colleges of Surgery as shown in Table 2 .8
Table 2.
Classification of surgical priority during COVID-19.
| Priority Level | Details |
|---|---|
| 1a | Emergency operation needed within 24 h |
| 1b | Urgent operation needed within 72 h |
| 2 | Surgery that can be deferred for up to 4 weeks |
| 3 | Surgery that can be delayed for up to 3 months |
| 4 | Surgery that can be delayed for more than 3 months |
Priority 1 patients in NHS Tayside continued to be treated on daily trauma lists during lockdown. We sought to restart Priority 2 cases as soon possible. Two pathways for restarting elective cases were developed by a small working group within the NHS Tayside management team: a “green pathway” and a “yellow pathway” (appendices 1 and 2). The first yellow pathway patient underwent surgery on the 1st May and the first green pathway patient did so on the 29th June. A third pathway for outpatient local anaesthetic (OPLA) cases also began on the 29th June and included priority 2 and 3 patients.
Patients on the green pathway shielded for 14 days. They underwent RT-PCR testing on day 0 and day 12. Two negative tests meant they could be admitted on the morning of surgery. There were several patients for whom the green pathway was not suitable, such as patients relying on carers or unwilling to strictly self-isolate for 14 days. For these patients there was a yellow pathway, which consisted of the advice to self-isolate as far as possible and then have RT-PCR testing 48 h prior to surgery, with a negative result enabling admission on the day of surgery. The OPLA pathway involved a pre-operative questionnaire and temperature recording on the day of surgery, but no pre-operative RT-PCR testing (appendix 3).
In NHS Tayside there are three main hospitals. Hospital A was used to treat patients with COVID-19 and treated all Priority 1 patients. Hospital B was used for green and yellow pathway inpatients and Hospital C was used for OPLA cases in a specific day surgery area, and later some yellow pathway inpatients using the main theatre complex. A floor of Hospital B, consisting of 2 wards, a staff room and changing facilities was designated the “green floor”. This area was only used by green pathway staff. No part of Hospital B or C intentionally served patients with identified COVID-19, but absence of COVID-19 throughout the hospital could not be guaranteed due to the limitations of testing.5 Orthopaedic patients on the green pathway were nursed in the same ward, but in different bays, as urgent elective breast surgery patients who had gone through the same pathway. A small number of other surgical specialties utilised the second ward on the green floor of the hospital following identical pathways. Patients on the yellow pathway were admitted to a different ward, which was also only used for COVID-19 negative patients.
The aims of this paper were to clarify the number of patients who have undergone elective orthopaedic surgery since the suspension of elective services in March 2020 and to review the safety of re-starting elective orthopaedic surgery. This was in the context of considerable unease and uncertainty in resuming planned care. This study is on-going and will include Patient Reported Outcome Measures (PROMs) data at 6 months.
Methods
This study was designed according to the STROBE statement for observational studies. All patients undergoing any elective orthopaedic operation in NHS Tayside between 27 March 2020 and 10 August 2020 were included prospectively. All patients were consented appropriately for their operation in the context of the COVID-19 pandemic. Data of patients who underwent elective surgery during the same dates of 2018 and 2019 were retrieved retrospectively for comparison. The hospital waiting list team recorded details of the pathway used for each patient. All COVID-19 test data were retrieved from the regional reporting system (ICE Desktop, Sunquest Information Systems). Demographic and 30-day outcome data were collected from the hospital electronic patient record system on 30 August 2020 (Clinical Portal, Version 2·16·2-RC3, NHS Tayside). Data collected were ASA grade, patients' age, patients’ sex, operation performed, length of stay, readmissions within 30 days and complications within 30-days.
The primary outcomes were to measure the number of cases performed since the suspension of elective services, identify patients who developed nosocomial COVID-19 and establish 30-day mortality in this cohort. Secondary outcomes were to specifically look at patients undergoing primary arthroplasty and define length-of-stay and complications within 30-days of surgery compared with previous years. Primary arthroplasty was selected as it is a relatively homogeneous group for comparison.
A nosocomial infection was defined as diagnosis greater than 48 h after admission to hospital and during the hospital stay. There is no clear definition in the literature for the end point whereby an infection is no longer considered nosocomial. For this reason, we used a definition of 30 days after discharge to ensure complete capture of all such infections. Thirty-day mortality was defined as a death occurring within 30 days of surgery.
Statistical analysis was performed using SPSS v. 25·0 (IBM, Armonk, New York). The chi-square test was utilised when comparing between categorical variables. A p-value of <·05 was regarded as significant.
Results
There were 55 patients included in the green pathway and 96 in the yellow pathway. There were 107 patients included in the OPLA pathway. There were 47 patients with incomplete 30-day follow up due to their operation having taken place within the last 30 days.
Five patients who would have otherwise been treated on the green or yellow pathway declined surgery, each citing the pandemic as their reason. No patients on the OPLA pathway declined surgery. No patients on the OPLA pathway reported symptoms when completing their questionnaire or were pyrexial on the day of surgery and therefore all underwent surgery.
Ten patients on the yellow pathway were required to undergo their operation in Hospital A as there were no paediatric or level 3 care facilities in Hospital B or C. All were nursed in side-rooms on COVID-19 negative wards. All patients on the green pathway had two COVID-19 tests. All patients on the yellow pathway had one test sent but two were reported as “leaking sample containers not tested”. These two patients underwent surgery without a valid test at the discretion of the treating consultant with the agreement of the patients. Neither had a complication of surgery.
Primary outcomes
Table 3 demonstrates the frequency of elective operations performed in the 2020 cohort compared with previous years cohorts. No operations were bilateral. There was a statistically significant difference in the sex of patients in 2020 compared with 2019. There were no statistical differences in ASA in 2020 compared to 2018 or 2019. The proportion of revision arthroplasty and carpal tunnel decompression cases was significantly higher in 2020 compared with previous years.
Table 3.
Primary outcomes.
| Primary Outcomes | 2018 |
2019 |
2020 |
2020 vs. |
||||
|---|---|---|---|---|---|---|---|---|
| 2018 |
2019 |
|||||||
| n | % | n | % | n | % | p-value | ||
| Total Operative Cases | n1261 | n1196 | n258 | <0.0001 | <0.0001 | |||
| Pathway | ||||||||
| Green | 55 | 21.3% | ||||||
| Yellow | 96 | 37.2% | ||||||
| OPLA | 107 | 41.5% | ||||||
| Mean age/years | 56 | 56 | 59 | 0.254 | 0.582 | |||
| Females | 706 | 56.0% | 658 | 55.0% | 160 | 62.0% | 0.074 | 0.039 |
| Males | 555 | 44.0% | 538 | 45.0% | 98 | 38.0% | ||
| ASA | ||||||||
| 1 | 242 | 177 | 23 | 0.101 | 0.379 | |||
| 2 | 398 | 373 | 60 | |||||
| 3 | 94 | 114 | 15 | |||||
| 4 | 4 | 4 | 2 | |||||
| Missing | 523 | 528 | 158 | |||||
| Case Breakdown | ||||||||
| Primary THR | 191 | 15.1% | 194 | 16.2% | 32 | 12.4% | <0.0001 | <0.0001 |
| Revision THR | 28 | 2.2% | 16 | 1.3% | 14 | 5.4% | ||
| Primary TKR | 194 | 15.4% | 176 | 14.7% | 16 | 6.2% | ||
| Revision TKR | 12 | 1.0% | 8 | 0.7% | 7 | 2.7% | ||
| Carpal Tunnel Decompression | 130 | 10.3% | 127 | 10.6% | 95 | 36.8% | <0.0001 | <0.0001 |
| Other OPLA | 103 | 8.2% | 105 | 8.8% | 32 | 12.4% | ||
| Other - Upper Limb | 314 | 24.9% | 231 | 19.3% | 18 | 7.0% | ||
| Other - Lower Limb | 277 | 22.0% | 323 | 27.0% | 44 | 17.1% | ||
| Spinal | 12 | 1.0% | 16 | 1.3% | 0 | 0.0% | N/A | N/A |
| 30-day complications | n201 | |||||||
| Dislocation | 0 | 0.0% | ||||||
| Deep infection | 0 | 0.0% | ||||||
| Superficial infection | 3 | 1.5% | ||||||
| DVT/PE | 2 | 1.0% | ||||||
| Transfusion | 3 | 1.5% | ||||||
| Traumatic dehiscence | 1 | 0.5% | ||||||
| AKI 1 | 1 | 0.5% | ||||||
| Arrythmia | 1 | 0.5% | ||||||
| Total Complications | 11 | 5.5% | ||||||
| 30-day readmissions | 4 | 2.0% | ||||||
| Nosocomial COVID-19 | 0 | 0% | ||||||
| 30-day mortality | 0 | 0% | ||||||
Statistical tests used.
1. Chi square for categorical.
2. Mann Whitney U for continuous.
N/A - unable to perform statistical tests due to 0 value present.
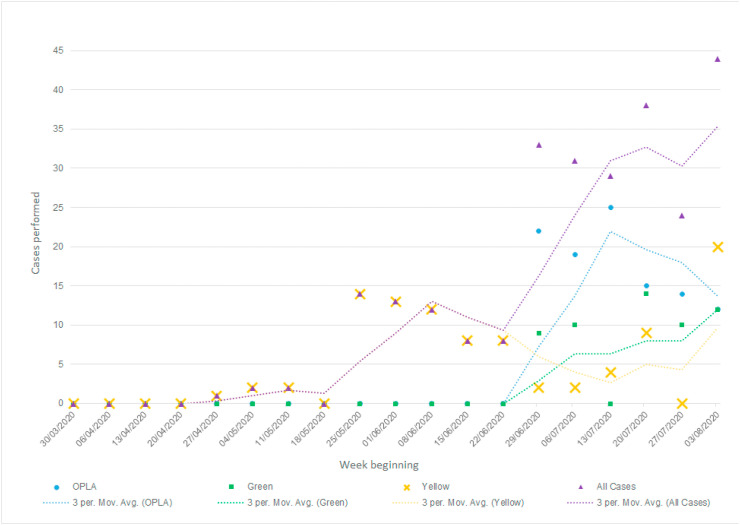
Figure 1 shows the number of operations performed per week during the study period, with each pathway represented by a separate series.
Fig. 1.
Operations performed per week on each pathway.
No patient was found to have a positive post-operative COVID-19 test conferring a nosocomial COVID-19 infection rate of 0%. One patient was documented to have had a positive test 3 months prior to their surgery and was documented to have a negative test preoperatively. This patient underwent an uncomplicated carpal tunnel decompression. No further positive COVID-19 tests were identified. No patients died within 30 days of their operation.
Secondary outcomes
Demographic data for patients undergoing primary arthroplasty of the hip and knee are displayed separately in Table 4 , along with mean length of stay and details regarding complications documented within 30 days of surgery. There was a significant difference in the sex of patients undergoing primary TKR in 2020 compared with 2018. There were no significant differences in ASA for primary TKR or THR between the cohorts. One patient who underwent primary total knee replacement was readmitted within 30 days of their surgery. This readmission was unrelated to the surgery or COVID-19. There were no significant differences in length of stay for primary TKR or THR in 2020 compared with previous cohorts but a trend towards fewer days was observed.
Table 4.
Secondary outcomes.
| Secondary Outcomes | 2018 |
2019 |
2020 |
2020 vs. |
||||
|---|---|---|---|---|---|---|---|---|
| 2018 |
2019 |
|||||||
| n | % | n | % | n | % | p-value | ||
| Primary Total Hip Replacement | n191 | n194 | n32 | <0.00001 | <0.00001 | |||
| Mean age/years | 69 | 70 | 65 | 0.161 | 0.126 | |||
| Females | 118 | 61.8% | 111 | 57.2% | 21 | 65.6% | 0.678 | 0.371 |
| Males | 73 | 38.2% | 83 | 42.8% | 11 | 34.4% | ||
| ASA | ||||||||
| 1 | 18 | 19 | 1 | 0.369 | 0.094 | |||
| 2 | 101 | 86 | 20 | |||||
| 3 | 31 | 45 | 4 | |||||
| 4 | 3 | 2 | 0 | N/A | N/A | |||
| Missing | 40 | 42 | 7 | |||||
| Mean length of Stay/days | 3.8 | 3.9 | 3.3 | 0.985 | 0.902 | |||
| 30-day complications | n27 | N/A | N/A | |||||
| Dislocation | 3 | 1.6% | 2 | 1.0% | 0 | 0.0% | ||
| Deep infection | 1 | 0.5% | 1 | 0.5% | 0 | 0.0% | ||
| Superficial infection | 5 | 2.6% | 5 | 2.6% | 0 | 0.0% | ||
| DVT/PE | 0 | 0.0% | 4 | 2.1% | 0 | 0.0% | ||
| Transfusion | 9 | 4.7% | 4 | 2.1% | 0 | 0.0% | ||
| Other complication | 8 | 4.2% | 12 | 6.2% | 1 | 3.7% | ||
| Total Complications | 26 | 12.6% | 28 | 14.4% | 1 | 3.7% | ||
| 30-day readmissions | 6 | 3.1% | 8 | 4.5% | 0 | 0.0% | ||
| Primary Total Knee Replacement | n194 | n176 | n16 | <0.00001 | <0.00001 | |||
| Mean age/years | 71 | 69 | 61 | 0.031 | 0.078 | |||
| Female | 105 | 54.1% | 97 | 55.1% | 8 | 50.0% | 0.750 | 0.694 |
| Males | 89 | 45.9% | 79 | 44.9% | 8 | 50.0% | ||
| ASA | N/A | N/A | ||||||
| 1 | 13 | 8 | 3 | 0.161 | 0.091 | |||
| 2 | 115 | 90 | 10 | |||||
| 3 | 23 | 27 | 0 | N/A | N/A | |||
| 4 | 0 | 0 | 0 | N/A | N/A | |||
| Missing | 43 | 51 | 3 | |||||
| Mean length of Stay/days | 3.3 | 3.8 | 3.1 | 0.152 | 0.350 | |||
| 30-day complications | n13 | |||||||
| Deep infection | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | ||
| Superficial infection | 6 | 3.1% | 7 | 4.0% | 0 | 0.0% | ||
| DVT/PE | 2 | 1.0% | 2 | 1.1% | 2 | 15.4% | ||
| Transfusion | 3 | 1.5% | 1 | 0.6% | 0 | 0.0% | ||
| Other complication | 5 | 2.6% | 21 | 11.9% | 1 | 7.7% | ||
| Total Complications | 16 | 8.2% | 31 | 17.6% | 3 | 23.0% | ||
| 30-day readmissions | 2 | 1.0% | 9 | 5.1% | 1 | 7.7% | ||
Discussion
There were approximately 80% fewer elective orthopaedic operations performed during the study period compared with previous years. Revision arthroplasty of the hip and knee were the only operations with similar numbers to previous years, possibly because these cases typically command high priority. A large proportion of cases were priority 3 carpal tunnel decompressions, as these could be performed in the separate day surgery unit of Hospital C with a minimum amount of staff and as such did not drain resources otherwise required for priority 2 inpatient operations.
The rate of nosocomial COVID-19 in our cohort was 0%, and the mortality within 30-days was also 0%. A study from New York indicated a 12·1% rate of positive COVID-19 RT-PCR testing of patients screened prior to elective surgery.9 Of those positive patients 58·3% were asymptomatic. Three asymptomatic patients developed post-operative hypoxia and two required intubation. It is estimated that the risk of an asymptomatic patient with a negative RT-PCR test being admitted for surgery and subsequently dying of COVID-19 is in the region of 1 in 140,000.10 Even with relatively small numbers, these findings do suggest that there may be considerable geographical variation in the percentage of asymptomatic carriers of COVID-19 in the general population.
Patients undergoing primary arthroplasty of the hip and knee were examined further. The mean length of stay for both operations was shorter compared to previous years, possibly reflecting an increased motivation for patients to get home. There was no evidence of a healthier cohort of patients being selected in 2020 compared to previous years. Although it is difficult to directly compare complications between cohorts due to the small numbers of patients involved, we observed no evident difference or negative trend.
Over 98% of patients agreed to undergo elective orthopaedic surgery, in contrast to a recent paper reporting only 61%.11 There are likely to be large numbers of willing patients available when resources become available to safely deliver elective surgery. All patients had pre-admission consenting telephone calls highlighting the risks of COVID-19 infection in the perioperative period by the surgical team and were required to sign a COVID-19 specific consent form on admission. It was clear from this that the extensive public health messaging in the UK had been understood and considered by our patient cohort. After the initial 6–8 weeks of lockdown there were increasing numbers of contacts from patients and their GP's seeking their planned surgery, indicating that genuine demand had not been nullified by the pandemic.
The data in Table 5 were extracted from Scottish Government websites.12, 13, 14 NHS Tayside experienced an average COVID-19 death rate relative to the rest of Scotland, ensuring our findings are relevant to other regions. It was vital to monitor the number of patients in the COVID-19 wards and ICU to ensure there was sustained capacity in the system before restarting elective surgery.
Table 5.
COVID infection rates in NHS Tayside compared with the Scottish average.
| NHS Tayside | Scotland | |
|---|---|---|
| Population estimate 201813 | 416,080 | 5,438,100 |
| Positive infections total14 | 1772 | 18,315 |
| ICU Days total14a | 276 | 8739 |
| Deaths registered with COVID-19 on certificate12 | 313 | 4173 |
| All cause deaths total12 | 2964 | 35,397 |
| Rates | ||
| Positive infections/population | 0.43% | 0.34% |
| ICU days/population | 0.0007 | 0.0016 |
| COVID death/population | 0.08% | 0.08% |
| All cause death/population | 0.71% | 0.65% |
<5 cases recorded as asterisk in government statistics, therefore estimates used.
Testing for COVID-19 was initially required to be performed within 48 h of admission for both green and yellow pathways. However, to allow the lab time to process the tests without resulting in large numbers of awaited test results at the time of admission, tests were collected 3 days before admission and reported the following day.
There was no specific protocol for the use of PPE in elective theatre and staff were advised to follow existing Government guidance whilst within the emergency theatre. Early in the pandemic, concerns were raised about aerosol generating procedures (AGPs) and the theoretical risk of spreading COVID-19 to personnel in the operating room by using high speed devices, pulsed lavage and diathermy.15 , 16 Theatre staff uniformly adopted the FFP3 mask with full-face visor in the initial phase of trauma practice during the pandemic. As the prevalence of the disease was reported to decrease, there was an consensus that patients on the green pathway could be treated as negative.5 The status of the yellow pathway patients was less conclusive. Staff had the freedom to make their own risk assessment as to when they wanted to stop using the FFP3 mask in favour of a standard fluid resistant type II surgical mask. Use of FFP3 masks is a compromise and has been reported to have detrimental effects with respect to fatigue and communication between staff in the operating department.17 There was no restriction in AGPs such as pulsed lavage on either pathway, which might otherwise have compromised the technical conduct of the operations.18
Adequate physiotherapy provision was available prior to re-starting orthopaedic elective services. Physiotherapy services across the world reported shifting their resources during lockdown from elective care to focus on unwell patients with COVID-19.19 It is currently unclear if physiotherapy services in other regions will return to normal practice in the near future, and the impact of a reduction in this service on elective surgical patients in other regions is not known.
Limitations
Our study period is very recent, and as such we have no data on mid or long-term complications incurred during the re start of elective services. We have compared with previous years using the same criteria for early complications to gain a comparison. The number of operations included in the 2020 cohort is small but constitutes one of the largest series of post COVID-19 elective orthopaedic cases reported in the literature to date. It will be prudent to continue monitoring patients undergoing elective surgery until COVID related protocols are no longer required to ensure complication rates remain acceptable.
It is recognised that elective orthopaedic surgery is not necessarily comparable, in terms of the physiological insult and effects on immune function, with some of the procedures employed in other surgical disciplines e.g. body cavity surgery and the surgical treatment of cancer.
Conclusions
We were able to safely re-start an elective orthopaedic service in the early stages of recovery from the COVID-19 pandemic, using a protocol compatible with the guidelines set by the Royal College of Surgery of England and the British Orthopaedic Association. We did not identify a single patient contracting COVID-19 as part of their treatment, and no increased risks were identified at this early stage compared with undergoing orthopaedic elective surgery in 2019 or 2018.
Our findings should give some reassurance to other regions that it may be acceptable to re-start elective surgery for urgent priority cases. Our results are generalisable to regions with similar COVID-19 prevalence, and healthcare resources.
In the event of further pandemics, we feel that there is the potential to maintain appropriately prioritised elective surgical activity during the pandemic period, if appropriate measures are taken with respect to physical separation, staff behaviour, patient testing and patient selection. Such a service may in theory expose patients to new risks and therefore the outcomes of such surgery should continue to be prospectively monitored.
Author contributions
PD - Inception of the idea, study design, data collection, analysis of data, data interpretation, writing manuscript, submitting manuscript.
RS – Data collection, data preparation, literature review, writing manuscript.
AM - Inception of the idea, literature review, study design, writing manuscript.
AF - Data analysis, literature review, editing the manuscript.
PH – Data collection, editing the manuscript, literature review.
SG – Data collection, data preparation, editing the manuscript.
LR - Data collection, pathway documentation, writing manuscript.
BC - Inception of the idea, negotiating the resumption of activity, study design, writing manuscript.
Declaration of competing interest
None.
Acknowledgements
Stephanie A Davies – Proof reading for spelling and grammar; Linda Johnston, Clinical Audit Manager – Verification of data; Dave Ridley, Systems Developer – Verification of data; Lorna O'Donnell, Clinical Audit and Research Nurse – Verification of data; Sarah Keogh, Clinical Audit and Research Nurse – Verification of data; Jennifer Scott, Clinical Audit and Research Nurse – Verification of data.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.surge.2020.10.002.
Appendix A. Supplementary data
The following are the supplementary data to this article:
References
- 1.World Health Organisation Timeline of WHO's response to COVID-19. https://www.who.int/news-room/detail/29-06-2020-covidtimeline
- 2.GOV.UK Coronavirus (COVID-19) in the UK. https://coronavirus.data.gov.uk/
- 3.Parvizi J., Gehrke T., Krueger C.A., Chisari E., Citak M., Van Onsem S. Resuming elective orthopaedic surgery during the COVID-19 pandemic: guidelines developed by the international consensus group (ICM) J Bone Joint Surg Am. 2020;102:1205–1212. doi: 10.2106/JBJS.20.00844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cipollaro L., Giordano L., Padulo J., Oliva F., Maffulli N. Musculoskeletal symptoms in SARS-CoV-2 (COVID-19) patients. J Orthop Surg. 2020;15:178. doi: 10.1186/s13018-020-01702-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weilongorska N.L., Ekwobi C.C. COVID-19: what are the challenges for NHS surgery? Curr Probl Surg. 2020 doi: 10.1016/j.cpsurg.2020.100856. Epub ahead of print 2 July 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Public Health Scotland Cancelled planned operations 7 July 2020 - data & intelligence from PHS. https://beta.isdscotland.org/find-publications-and-data/healthcare-resources/waiting-times/cancelled-planned-operations/
- 7.The British Orthopaedic Association Re-starting non-urgent trauma and orthopaedic care: summary guidance. https://www.boa.ac.uk/resources/boa-guidance-for-restart---summary---final-pdf.html
- 8.Royal College of Surgeons Clinical guide to surgical prioritisation during the coronavirus pandemic. https://www.rcseng.ac.uk/coronavirus/surgical-prioritisation-guidance/
- 9.Gruskay J.A., Dvorzhinskiy A., Konnaris M.A., LeBrun D.G., Ghahramani G.C., Premkumar A. Universal testing for COVID-19 in essential orthopaedic surgery reveals a high percentage of asymptomatic infections. J Bone Joint Surg Am. 2020;102:1379–1388. doi: 10.2106/JBJS.20.01053. [DOI] [PubMed] [Google Scholar]
- 10.Kader N., Clement N.D., Patel V.R., Caplan N., Banaszkiewicz P., Kader D. The theoretical mortality risk of an asymptomatic patient with a negative SARS-CoV-2 test developing COVID-19 following elective orthopaedic surgery. Bone Jt J. 2020:1–5. doi: 10.1302/0301-620X.102B9.BJJ-2020-1147.R1. [DOI] [PubMed] [Google Scholar]
- 11.Chang J., Wignadasan W., Kontoghiorghe C., Kayani B., Singh S., Plastow R. Restarting elective orthopaedic services during the COVID-19 pandemic. Bone Jt Open. 2020;1:267–271. doi: 10.1302/2633-1462.16.BJO-2020-0057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Records of Scotland Deaths involving coronavirus (COVID-19) in Scotland. https://www.nrscotland.gov.uk/covid19stats
- 13.The Scottish Public Health Observatory Population: estimates. https://www.scotpho.org.uk/population-dynamics/population-estimates-and-projections/data/population-estimates/
- 14.Scottish Government Coronavirus (COVID-19): trends in daily data. https://www.gov.scot/publications/coronavirus-covid-19-trends-in-daily-data/
- 15.Hirschmann M.T., Hart A., Henckel J., Henckel J., Sadoghi P., Mouton C. COVID-19 coronavirus: recommended personal protective equipment for the orthopaedic and trauma surgeon. Knee Surg Sports Traumatol Arthrosc. 2020:1–9. doi: 10.1007/s00167-020-06022-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schultz L. Can efficient smoke evacuation limit aerosolization of bacteria? AORN J. 2015;102:7–14. doi: 10.1016/j.aorn.2015.04.023. [DOI] [PubMed] [Google Scholar]
- 17.Yánez Benítez C., Güemes A., Aranda J., Ribeiro M., Ottolino P., Di Saverio S. Impact of personal protective equipment on surgical performance during the COVID-19 pandemic. World J Surg. 2020:1–6. doi: 10.1007/s00268-020-05648-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Norman G., Atkinson R.A., Smith T.A., Rowlands C., Rithalia A.D., Crosbie E.J. Intracavity lavage and wound irrigation for prevention of surgical site infection. Cochrane Database Syst Rev. 2017;10:CD012234. doi: 10.1002/14651858.CD012234.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prvu Bettger J., Thoumi A., Marquevich V., De Groote W., Rizzo Battistella L., Imamura M. COVID-19: maintaining essential rehabilitation services across the care continuum. BMJ Glob Health. 2020;5 doi: 10.1136/bmjgh-2020-002670. Epub ahead of print 5 May 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.