Abstract
Coronavirus disease is a global infection presenting with a variety of clinical features, both pulmonary and extrapulmonary symptoms. Its diagnosis depend on clinical symptoms, laboratory tests, and the typical CT chest scan findings. In this report, a 72-year-old patient (known to have lung cancer) present with pleural effusion as possible sequel of COVID-19 pneumonia. Pleural effusion may present as a complication in a patient with coronavirus disease, but there is poor evidence to this claim in the medical literature.
Keywords: COVID-19, Pleural effusion, Coronavirus, Lung cancer, Bronchogenic carcinoma
1. Introduction
COVID-19 pneumonia is a worldwide viral infection that is cause by the SARS-COV-2 virus [1]. It affect many body systems, especially the pulmonary system [2]. There is no specific test to diagnose this newly spread infection, but this may be facilitate with RT-PCR [3] or with using CT chest scan [4]. Pneumonia and pleural effusion are one of the recognize complications of COVID-19 [5]. In this report, a 72-year-old patient with pleural effusion present as sequel of COVID-19 infection with a history of lung cancer diagnosed recently.
2. Case report
A 72-year-old male patient presented with shortness of breath and fever of ten days duration. He was diagnosed with stage IV bronchogenic carcinoma and lymphangitis carcinomatosis five months prior to his presentation. On the initial assessment, he appeared uncomfortable, dyspneic, tachypneic and cachetic. The blood pressure was 140/85 mmHg, heart rate: 124 beats/min, oxygen saturation: 79%, and body temperature: 37.7 Co. Chest expansion was reduced as well as the air entry on the left side of the chest; course crepitation on auscultating the other side.
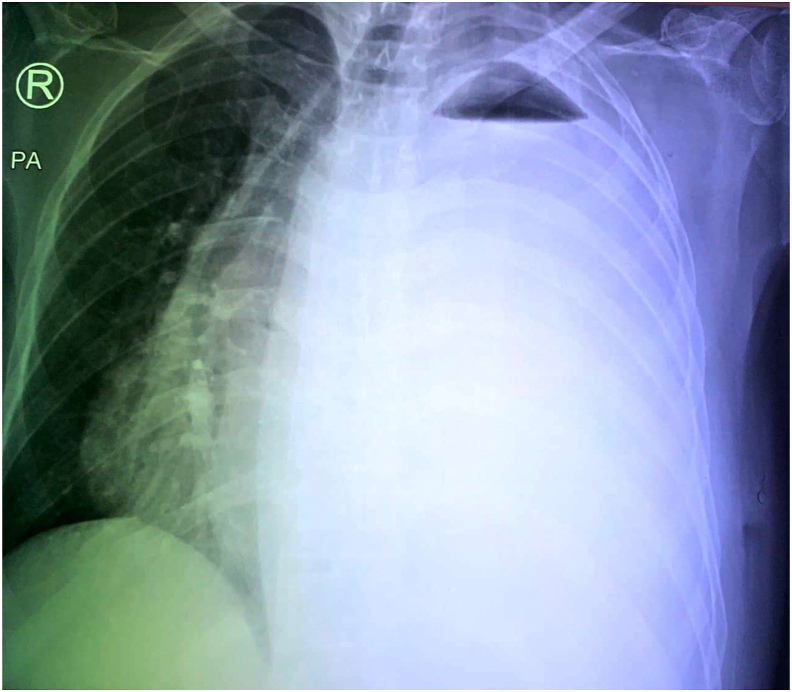
The chest radiograph showed left sided with multiple right sided chest opacifications demonstrating a massive pleural effusion (Fig. 1). Chest thoracostomy tube was inserted on the left side, draining a clear serous fluid. Fluid sample was sent for cytology, acid fast bacilli culture, biochemistry, and Gram-stain culture and sensitivity. The patient was admitted to the thoracic ward for gradual chest decompression. He was maintained on antibiotics, and analgesia. Due to COVID-19 pandemic, the patient was sent for a CT scan of the chest, and PCR for COVID-19 to look for any evidence of COVID-19. The PCR was obtained from two sites (nasopharyngeal, and oropharyngeal).
Fig. 1.
Chest radiograph showing multiple left and right sides opacifications with a massive pleural effusion on the left side.
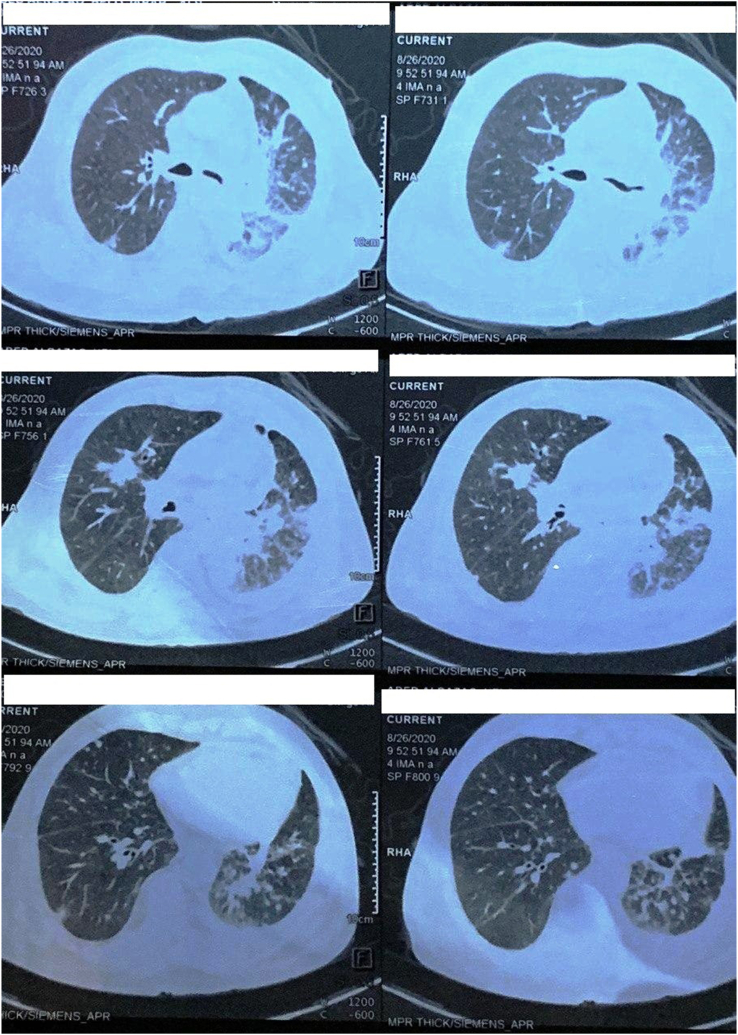
Unsurprisingly, the PCR test came back positive for COVID-19. The CT chest showed multiple ground glass opacifications on both lungs, and pleural effusion on the left side with irregular hilar mass (Fig. 2). The patient condition deteriorated; he became dyspneic and his oxygen saturation never exceeded 85% despite oxygen supply on the ward. He was transferred to ICU for ventilatory support. After three days, the result of pleural cytology was negative for metastasis, and AFB was negative for tuberculosis. The patient's condition gradually deteriorated in the following days with elevated renal parameters and progressive hypoxia. On the sixth, the patient unfortunately passed away due to severe hypoxia that led to a cardiac arrest.
Fig. 2.
CT scan of chest in day two post-intervention, showed multiple ground glass opacifications on both lungs, and pleural effusion on the left side with irregular hilar mass.
3. Discussion
Coronavirus infection has become a worldwide pandemic that affect many countries, including Iraq. In this case, the main differential diagnosis is malignant pleural effusion because the patient is previously diagnose with bronchogenic carcinoma. The diagnosis change to COVID-19 pneumonia in view of positive PCR test for COVID-19. Furthermore, the pleural fluid analysis was negative for malignant pleural effusion, tuberculosis and bacterial infection.
Pleural effusion is an uncommon finding in coronavirus infection. In Wong et al. study, there are only two cases out of 64 patients with COVID-19 pneumonia that have pleural effusion [6]. While it is of variable frequency in the Ye et al. study [7]. Our case is similar to Ahmadinejad et al., case [5]. Until this time, there is no clear evidence of how the virus can cause pleural effusion, but it carry an adverse prognostic sign that may indicate a bacterial super-infection in COVID-19 pneumonia [7].
About 20% of pleural effusions are of unknown aetiology despite fluid analysis, hence the requirement for more invasive diagnostic procedures like pleural biopsy under thoracoscopy guide [8].
The prevalence of pleural effusion is 5–10% [9]. Chong et al., has been well describe of the characteristics of SARS-CoV-1 or SARS-CoV-2-associated pleural effusions [9].
In our case, this is not carry out due to the critical condition of the patient.
4. Conclusion
Pleural effusion may present as a complication in patients with coronavirus disease; however, there is still scanty of data to support such a claim. More cases to be identified and studied to prove or refute this theory.
Statement of informed consent
Informed consent was obtained from the patient.
Contribution
AMF: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Resources; Software; Visualization; Roles/Writing - original draft; Writing - review & editing. HA: Formal analysis; Investigation; Supervision; Validation; Visualization; Roles/Writing - original draft; Writing - review & editing. YAAA: Validation; Visualization; Roles/Writing - original draft. YQMA: Formal analysis; Investigation; Writing - review & editing. ASA: Data curation; Formal analysis; Project administration; Writing - review & editing.
Grant information
The author(s) declared that no grants were involved in supporting this work.
Conflicts of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Funding support
None.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Fahad A.M., Mohammed A.A., Al-Khalidi H.A. Case report: COVID-19 in female patient who present with acute limb ischemia. F1000Research. 2020;9:778. [Google Scholar]
- 2.Fahad A.M., Mohammed A.A., Al-Khalidi H.A. Spontaneous pneumothorax as a complication in COVID-19 male patient: a case report. Clin. Case Rep. 2020:1–4. doi: 10.1002/ccr3.3378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goudouris E.S. Laboratory diagnosis of COVID-19. J. Pediatr. (Rio J) 2020 doi: 10.1016/j.jped.2020.08.001. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Awulachew E., Diriba K., Anja A. Computed Tomography Imaging features of patient with COVID-19: systematic review and meta-analysis. Radiol. Res. Pract. 2020;2020 doi: 10.1155/2020/1023506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ahmadinejad Z., Salahshour F., Dadras O. Jun 2020. Pleural Effusion as Sign of Coronavirus Disease 2019 (COVID-19) Pneumonia: A Case Report. [DOI] [PubMed] [Google Scholar]
- 6.Wong H.Y.F., Lam H.Y.S., Fong A.H. Frequency and distribution of chest radiographic findings in COVID-19 positive patients. Radiology. 2020 doi: 10.1148/radiol.2020201160. 201160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ye Z., Zhang Y., Wang Y. Chest CT manifestations of new coronavirus disease 2019 (COVID-19): a pictorial review. Eur. Radiol. 2020;19:1–9. doi: 10.1007/s00330-020-06801-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wilsher M.L., Veale A.G. Medical thoracoscopy in the diagnosis of unexplained pleural effusion. Respirology. 1998;3(2):77–80. doi: 10.1111/j.1440-1843.1998.tb00100.x. [DOI] [PubMed] [Google Scholar]
- 9.Chong W.H., Huggins J.T., Chopra A. Characteristics of pleural effusion in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pneumonia. Am. J. Med. Sci. 2020;S0002–9629(20):30413–30414. doi: 10.1016/j.amjms.2020.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]