Abstract
Introduction
This study aims to systematically evaluate vertical and horizontal equity in the Chinese healthcare financing system over the period 2008–2018 during the progress towards Universal Health Coverage (UHC), and to examine how both types of equity have changed during this period.
Methods
Household information on healthcare payments was collected from 2398 households involving 7021 individuals in 2008, 3600 households involving 10 466 individuals in 2013 and 3660 households involving 11 550 individuals in 2018. Redistributive effects of healthcare financing system were decomposed into progressivity, pure horizontal inequity and reranking. Progressivity analysis and the Aronson-Johnson-Lambert decomposition method were adopted to measure the vertical equity and horizontal equity of healthcare financing.
Results
Over the period 2008–2018, healthcare financing through indirect taxes showed a slightly prorich structure and healthcare financing through direct taxes showed a propoor structure in both urban and rural areas. Urban Employee Basic Medical Insurance experienced redistribution from the poor to the rich during the period 2008–2013, but then experienced redistribution from the rich to the poor during the period 2013–2018. Urban Resident Basic Medical Insurance (URBMI), New Rural Cooperative Medical Scheme (NRCMS), Urban and Rural Resident Basic Medical Insurance (URRBMI) and out-of-pocket payments experienced redistribution from the poor to the rich over the entire period.
Conclusion
China’s healthcare financing has experienced redistribution from the poor to the rich during 10 years of progress toward the UHC. UHC improved access to and utilisation of healthcare in urban areas. The flat rate contribution mechanism should be renovated for URBMI, NRCMS and URRBMI.
Keywords: health insurance, health policy, health services research, health systems
Key questions.
What is already known?
Previous studies on China’s healthcare financing mainly focused on vertical equity.
The benefits package of the health insurance scheme in rural China needs further improvements.
Flat rate contributions pose a challenge to health insurance premiums in China.
What are the new findings?
This study is the first to systemically examine the vertical and horizontal equity of healthcare financing in China.
Healthcare financing experienced redistribution from the poor to the rich during 10 years of progress towards Universal Health Coverage (UHC) in China.
UHC has contributed to reducing horizontal inequity in relation to out-of-pocket payments in China’s urban areas.
What do the new findings imply?
Issues of horizontal inequity arose with more people covered by health insurance programmes in China.
UHC improved access to and utilisation of healthcare in urban China.
The health insurance benefits package in rural China needs further improvements.
Introduction
In 2009, the Chinese government announced a healthcare reform plan that aimed to achieve Universal Health Coverage (UHC) by expanding social health insurance to provide coverage for more than 90% of the population.1 Urban Employee Basic Medical Insurance (UEBMI), Urban Resident Basic Medical Insurance (URBMI) and the New Rural Cooperative Medical Scheme (NRCMS) are the main types of social health insurance that cover the urban and rural populations. These insurance schemes involve different contribution schedules. UEBMI is a universal health insurance scheme for workers and retirees. Contributions to the UEBMI scheme are a fixed proportion of the employee’s salary. URBMI provides cover for urban residents who are not employed, and thus ineligible for the UEBMI scheme. Target groups for the URBMI scheme were children, the elderly, the disabled, laid-off workers and other non-working urban residents. The scheme was mainly financed by government subsidies for premiums, together with flat rate household contributions. The NRCMS was implemented to meet the needs of rural populations. Since 2016, URBMI and NRCMS have been merged into a new type of resident medical insurance, Urban and Rural Resident Basic Medical Insurance (URRBMI), which covered the population in the previous URBMI and NRCMS. Similar to URBMI, the NRCMS and URRBMI featured flat rate contributions. However, although all enrollees paid the same premiums to the NRCMS, the benefit packages varied geographically.
In addition to social health insurance, taxation and out-of-pocket (OOP) payments are the two other sources of finance for healthcare in China.2 However, the impact of these sources on healthcare financing is likely to vary. Contributions towards the financing of healthcare may redistribute household income within a given population. This redistribution can be both vertical and horizontal. Vertical redistribution occurs when payments are disproportionately related to ability to pay (ATP). Horizontal redistribution occurs when people with equal ATP contribute unequally to healthcare payments because of differential treatment. Vertical and horizontal redistributions are generally defined as redistributive effects (REs). The total RE can be quantitatively decomposed into three portions: vertical equity, pure horizontal equity and reranking. Vertical equity implies that people with greater economic ability ought to pay more. Pure horizontal equity implies that people with equal economic ability should pay the same. Reranking occurs when people change rank order after payments.
With regard to UEBMI, contributions are correlated with the enrollee’s salary. Thus, the rich make a larger contribution, which contributes to vertical equity. However, the contribution is not solely linked to salary, but is also correlated with factors such as the enrollee’s age and location. Thus, the UEBMI contribution at a given income level is uncertain, and the extent of this horizontal inequity is unclear. With regard to URBMI, NRCMS and URRBMI, the flat rate contributions mean that the rich and poor pay the same premium, thereby contributing to horizontal equity and vertical inequity. Regarding finance from taxation, payments for healthcare are linked to whatever tax bases are used. For example, much higher income tax rates are imposed on high-income individuals. This tax schedule is both horizontally inequitable and vertically equitable. However, with regard to some indirect taxes, such as consumption tax, the tax burden can be transferred from one person to another, and thus the horizontal and vertical equities of this form of finance should be empirically explored.
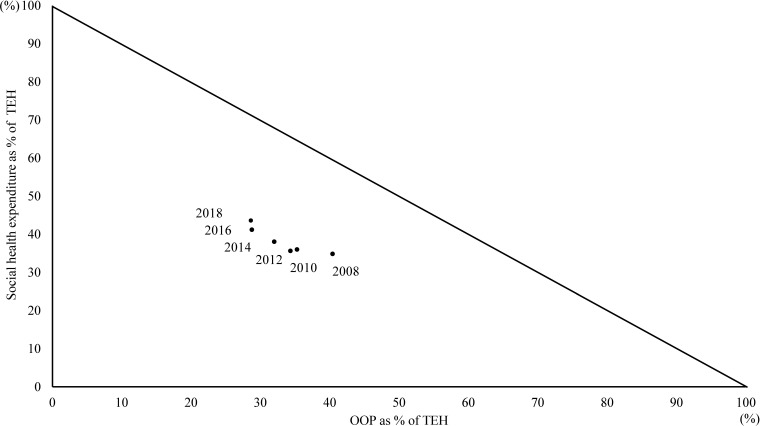
It can be seen from the health-financing triangle presented in figure 1 that the ratio of OOP payments to total expenditure on health decreased over the period 2008–2018 in China, while social health insurance made a more substantial contribution over the same period. Thus, UHC has largely been achieved, with more than 95% of the Chinese population being covered by health insurance since 2013,3 but the overall picture of China’s healthcare financing equity has never been fully explored. First, no studies have evaluated financing equity during the 10 years of progress towards UHC in China. Second, the equity of healthcare financing depends not only on its degree of progressivity, but also on the extent of any pure horizontal inequity and reranking resulting from it.4 5 Previous studies on healthcare financing in China have only focused on vertical equity, and a comprehensive analysis of healthcare financing equity has never been undertaken. To our knowledge, only one study has examined the horizontal equity of healthcare financing in China between 2003 and 2008.6 To date, no studies have systemically examined both vertical and horizontal equity during the progress towards UHC in China. This is a serious omission. This study seeks to address this gap in the literature by evaluating the progressivity, horizontal equity and reranking associated with healthcare financing in China during the progress towards UHC. We conducted three surveys in 2008, 2013 and 2018. The aim of our analysis is to systemically evaluate equity of healthcare financing during the 10 years of progress toward UHC in China, including vertical equity, pure horizontal equity and reranking.
Figure 1.
Healthcare financing triangle. Finance from out-of-pocket (OOP) payments and social health expenditure as a percentage of total expenditure on health (TEH).
Methods
Data sources
Data for our study were collected via three rounds of household surveys conducted in Jiangsu province in eastern China. Socioeconomic development varied geographically in Jiangsu: the overall economic status is more advanced in the south, but modest and underdeveloped in the middle and north of the province. A multistage stratified random sampling procedure was used. In 2008, the survey involved four randomly selected cities or counties. Five communities or towns were then sampled in each city or county. Two neighbourhoods or villages were then selected from each community or town. In each neighbourhood or village, 60 households were randomly selected. In 2013 and 2018, the sampling method was the same, but the sample size was expanded to include six cities or counties. These surveys contained observations from 2400 households involving 7023 individuals in 2008, 3600 households involving 10 466 individuals in 2013 and 3660 households involving 11 550 individuals in 2018. However, in 2008, two households did not report their household income and 2398 households were included in the final analysis (tables 1 and 2).
Table 1.
Characteristics of the study participants in urban areas
| Variable | 2008 | 2013 | 2018 | ||||||
| Obs | Mean/ percentage |
SD | Obs | Mean/ percentage |
SD | Obs | Mean/ percentage |
SD | |
| Female | 815 | 51.84% | 2666 | 51.83% | 2898 | 51.32% | |||
| Age | 1572 | 45.91 | 20.93 | 5144 | 47.38 | 20.97 | 5647 | 43.80 | 23.10 |
| 0–14 years | 129 | 6.13 | 4.35 | 425 | 5.85 | 4.24 | 808 | 5.02 | 4.45 |
| 14–60 years | 1000 | 40.38 | 12.99 | 3090 | 41.34 | 12.81 | 3161 | 39.71 | 12.18 |
| 60+ years | 443 | 70 | 7.55 | 1629 | 69.66 | 7.52 | 1678 | 70.18 | 7.42 |
| No of household members | 598 | 2.62 | 1.03 | 1800 | 2.86 | 1.24 | 1860 | 3.04 | 1.35 |
| Equivalent household expenditure (RMB)* | 598 | 21 979.17 | 13 736.49 | 1800 | 25 125.56 | 16 384.83 | 1860 | 32 775.08 | 24 294.23 |
| First quintile | 118 | 9574.10 | 2231.37 | 360 | 11 426.1 | 2599.803 | 372 | 12 427.32 | 3366.51 |
| Second quintile | 121 | 14 881.62 | 1233.78 | 360 | 17 361.4 | 1465.791 | 372 | 20 565.18 | 1850.79 |
| Third quintile | 120 | 19 307.01 | 1305.50 | 360 | 22 552.58 | 1355.419 | 372 | 27 502.79 | 2121.26 |
| Fourth quintile | 120 | 24 749.88 | 2049.34 | 360 | 28 379.04 | 2136.814 | 372 | 35 914.46 | 3351.26 |
| Fifth quintile | 119 | 41 397.45 | 18 475.26 | 360 | 45 908.67 | 25 118.75 | 372 | 67 550.70 | 33 438.75 |
| Health insurance | |||||||||
| None | 171 | 10.88% | 151 | 2.94% | 201 | 3.56% | |||
| Any | 1401 | 89.12% | 4993 | 97.06% | 5446 | 96.44% | |||
*All year 2008’s and 2013’s nominal prices have been adjusted to real prices in year 2018 by using China’s Consumer Price Index.
RMB, renminbi.
Table 2.
Characteristics of the study participants in rural areas
| Variable | 2008 | 2013 | 2018 | ||||||
| Obs | Mean/ percentage |
SD | Obs | Mean/ percentage |
SD | Obs | Mean/ percentage |
SD | |
| Female | 2722 | 49.95% | 2656 | 49.91% | 2946 | 49.91% | |||
| Age | 5449 | 40.98 | 20.44 | 5322 | 42.89 | 21.50 | 5903 | 43.33 | 22.00 |
| 0–14 years | 637 | 6.85 | 4.27 | 733 | 5.75 | 4.02 | 964 | 6.88 | 4.10 |
| 14–60 years | 3883 | 39.50 | 12.86 | 3389 | 41.52 | 12.40 | 3416 | 42.22 | 11.93 |
| 60+ years | 929 | 70.60 | 7.80 | 1200 | 69.43 | 7.27 | 1523 | 68.89 | 7.05 |
| No of household members | 1800 | 3.03 | 1.27 | 1800 | 2.96 | 1.38 | 1800 | 3.28 | 1.56 |
| Equivalent household expenditure (RMB)* | 1800 | 8394.83 | 5591.66 | 1800 | 15 047.99 | 10 778.83 | 1800 | 18 018.70 | 18 265.18 |
| First quintile | 360 | 3293.27 | 1020.40 | 360 | 4903.31 | 1731.12 | 6065.40 | 1592.97 | |
| Second quintile | 360 | 5638.88 | 526.55 | 360 | 9394.71 | 1066.94 | 10 395.08 | 1150.26 | |
| Third quintile | 360 | 7329.28 | 509.88 | 361 | 12 938.77 | 1120.44 | 14 214.81 | 1294.99 | |
| Fourth quintile | 360 | 9466.41 | 829.23 | 359 | 17 493.37 | 1682.92 | 19 334.17 | 1811.64 | |
| Fifth quintile | 360 | 16 246.29 | 7522.89 | 360 | 30 522.48 | 13 717.24 | 39 906.29 | 30 950.13 | |
| Health insurance | |||||||||
| None | 436 | 8.00% | 108 | 2.03% | 87 | 1.47% | |||
| Any | 5013 | 92.00% | 5214 | 97.97% | 5816 | 98.53% | |||
*All year 2008’s and 2013’s nominal prices have been adjusted to real prices in year 2018 by using China’s Consumer Price Index.
RMB, renminbi.;
The surveys collected detailed information on a series of individual and family characteristics, including age, gender, marital status, highest education level attained, employment status, urban/rural classification, household expenditure, consumption of healthcare, individual and household OOP expenditure, and geographical location. Regarding household expenditure, monthly expenditure on food, clothing, traffic, communication, housing, water, electricity, fuel, education, travel, entertainment, medical care and other items were recorded. In addition, information was recorded in relation to any unexpected expenditure. Per capita household expenditure, adjusted to obtain an adult-equivalent (AE) estimate, was used as the measure of living standards.7
Regarding healthcare payments, two sources of data were used. The first involved the above-mentioned surveys, while the other source was local statistical yearbooks (which mainly provided data on tax revenues and social health insurance copayments). Indirect taxes mainly include alcohol tax, cigarette tax, electricity and gas tax, entertainment tax, excise on food, drinks, and lodging, and other consumption taxes. These indirect taxes were approximated by applying specific tax rates to the corresponding expenditures. Direct taxes for households mainly consisted of personal income tax. Personal income tax was imposed on employees, and was deducted from their pay. The personal income rates were determined by the Chinese central government and they were adjustable according to the socioeconomic development. In 2011, the government adjusted the personal income rates from 9 grades to 7 grades. Accordingly, the pre-2011 personal income tax rates were used to calculate the personal income tax in 2008 and the post-2011 rates were used for 2013 and 2018 (online supplemental table 1A, B).
bmjgh-2020-003570supp001.pdf (60.3KB, pdf)
As there were no taxes earmarked for healthcare in China, indirect and direct taxes were allocated on a prorata basis using information from the Chinese National Health Accounts. In 2008, tax-funded expenditure represented 91.92% of the government’s expenditure on health, which in turn accounted for 4.51% of general government expenditure. Therefore, in 2008, the proportion of household tax payments going to the health sector was 4.15%. In 2013 and 2018, the proportion of household tax payments going to the health sector was 5.29% and 6.60%, respectively.8 Regarding social health insurance, UEBMI financing contributions were measured by applying contribution rates to the earnings of the covered workers. Financing contributions on URBMI, NRCMS and URRBMI were measured by the sum of the premiums paid. Data on OOP payments included OOP expenditure on prescriptions and outpatient and inpatient services.
Outcome variables
Vertical equity was measured using a progressivity analysis, and the Kakwani Index (KI) was adopted to evaluate the degree of vertical equity. Horizontal inequity was measured by the sum of pure horizontal inequity (H) and reranking (R), which were directly calculated using the Aronson-Johnson-Lambert (AJL) decomposition method. Vertical equity, pure horizontal inequity and reranking calculations were transformed into percentages of the total RE.
Analyses
The unit for analysis was the household. Expenditure and healthcare payments were aggregated at the household level. Household expenditure was used as the measurement of ATP.9 Household expenditure was adjusted for household size and composition using an AE estimate. The number of AE household members was defined as
where A is the number of adults in the household, α is the cost per child, K is the number of children and β is the degree of economies of scale.9 The values of α and β were assumed to be 0.5 and 0.75, respectively.10 The population was ranked by socioeconomic status and grouped into quintiles of equal size. Household healthcare payments were also adjusted for household size and composition using an AE estimate.
Progressivity analysis
In this study, progressivity was measured by computing the Concentration Index (CI) and the Gini coefficient (GC), which required directly relating the covariance between variables and household fractional ranks based on people’s ATP.7 Estimates of the CI and GC can be obtained from a ‘convenient regression’ of a transformation of ATP or the healthcare payment on the fractional rank in the ATP distribution.9 Specifically,
where is the healthcare payment or ATP of household i, is the mean healthcare payment or ATP, is the household fractional rank based on the ATP distribution, and is the variance of the household fractional rank. The ordinary least squares regression estimate of β is an estimate of CI or GC. α is the intercept and ε is the residual.
The progressivity of the healthcare payments was then estimated using the KI, which is the difference between the CI and the GC. If the difference is positive (negative), it indicates that the payments are progressive (regressive). If the difference equals 0, it indicates that the payments are proportional. Progressivity (regressivity) means that the rich (poor) contribute a larger proportion of healthcare payments than the poor (rich) in comparison with their ATP.9
AJL decomposition
The horizontal inequity of the healthcare payments was measured using AJL decomposition.4 The RE of healthcare financing can be calculated as the difference in the GC caused by the healthcare payments:
and are the prepayment and postpayment GC respectively, where X denotes prepayment income, and P denotes the healthcare payment.
The AJL decomposition method shows that this difference can be written as:
where V is the vertical redistribution, H is the pure horizontal inequity and R is the degree of reranking.
V can be decomposed into a payment rate effect and a progressivity effect:
where g is the sample average healthcare payment rate (as a proportion of income) and is the KI value of the payments computed under the assumption of within-group equality.
Pure horizontal inequity was measured by the weighted sum of the group j-specific postpayment GC, with the weights being calculated as the product of the group’s population share and its postpayment income share, :
R captured the extent of reranking of households that occurred in the move from prepayment to postpayment income distributions, and was measured as the difference between and . is the postpayment GC, and is the postpayment income CI. To calculate the postpayment income CI, we ranked all households by the prepayment incomes and then, by their postpayment income within each group of prepayment ‘equals’.
Patient and public involvement
No patients or members of the public were directly involved in this study. There are no plans to involve patients or the public in the dissemination of results.
Results
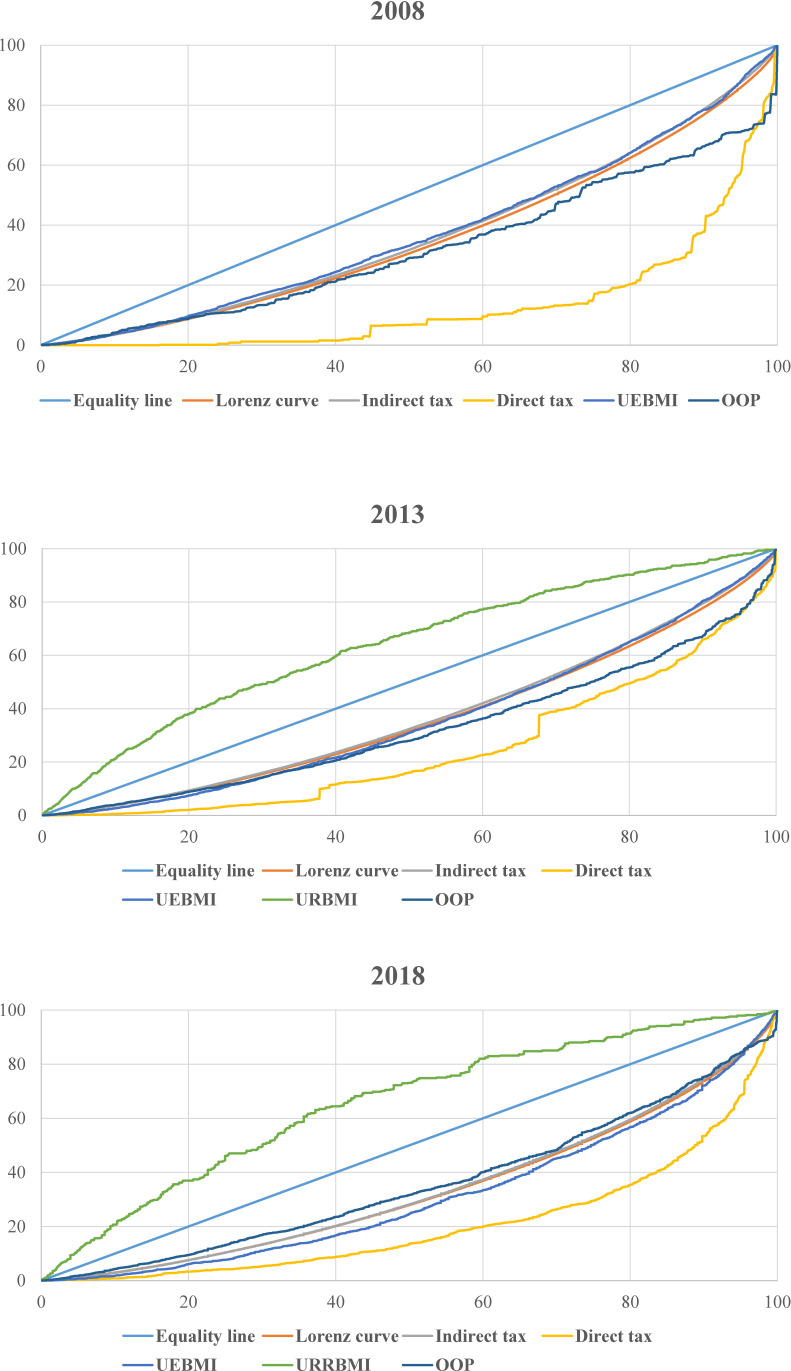
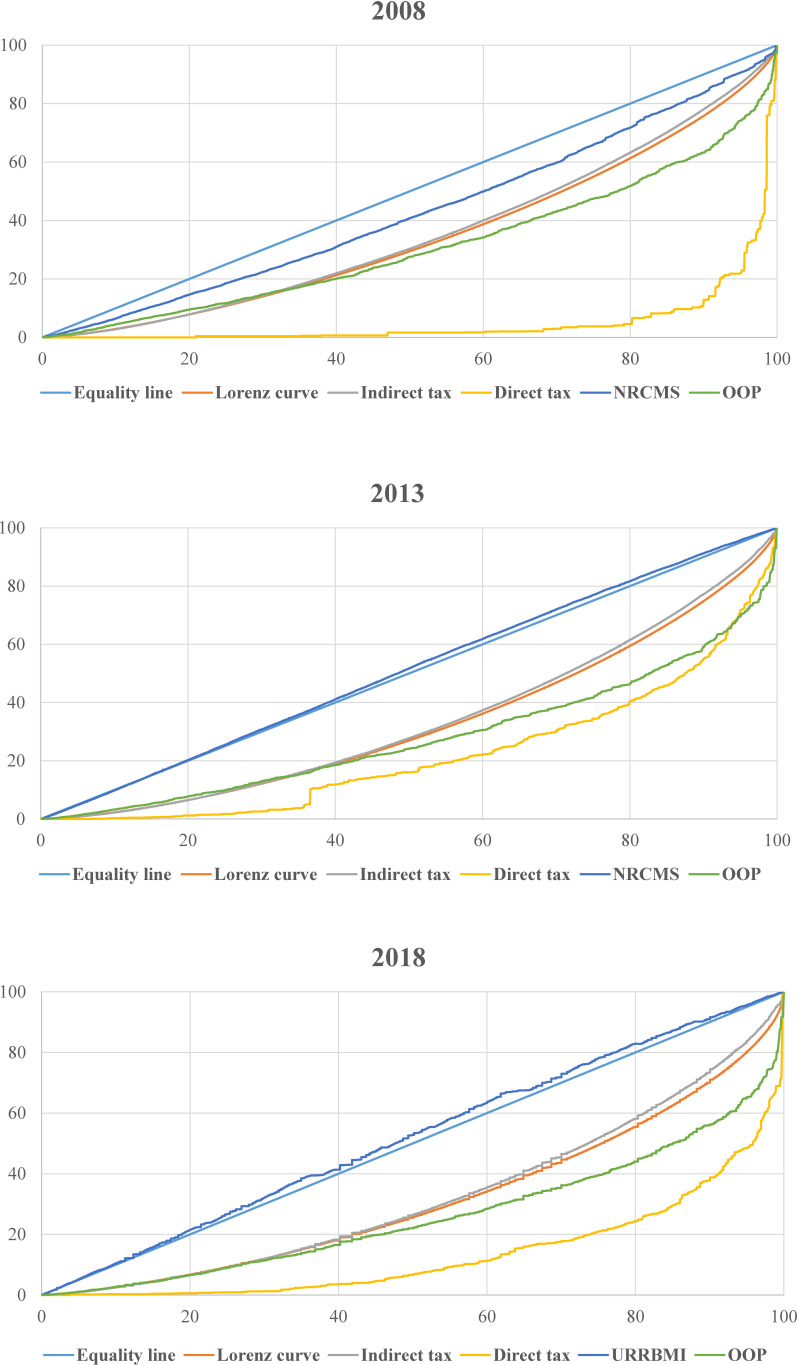
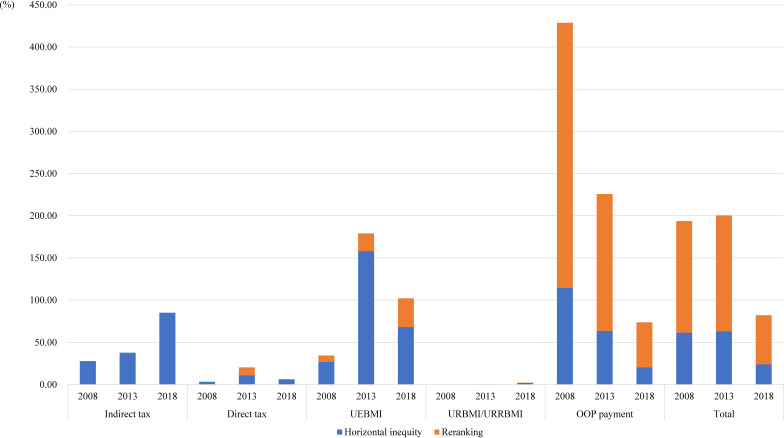
The results regarding the progressivity, pure horizontal inequity and reranking associated with healthcare financing are presented in tables 3–5). Figures 2 and 3 show the Lorenz curve and the concentration curves associated with each healthcare financing source. Figures 4 and 5 show the degree of horizontal inequity and reranking for financing sources.
Table 3.
Progressivity, pure horizontal equity and reranking associated with the Chinese healthcare financing system in 2008
| Income quintiles/index | Per capita household expenditure | Indirect tax | Direct tax | UEBMI† | NRCMS‡ | OOP payment | Total | |||||
| Urban | Rural | Urban | Rural | Urban | Rural | Urban | Rural | Urban | Rural | |||
| Gini/CI | 0.2874** | 0.3061** | 0.2661** | 0.2875** | 0.7360** | 0.8981** | 0.2546** | 0.1405** | 0.3577** | 0.3764** | 0.3077** | 0.3634** |
| 95% CI | (0.2698 to 03050) | (0.2953 to 0.3169) | (0.2516 to 0.2807) | (0.2773 to 0.2977) | (0.5521 to 0.9199) | (0.5690 to 1.2273) | (0.2281 to 0.2811) | (0.1094 to 0.1717) | (0.1526 to 0.5627) | (0.3132 to 0.4396) | (0.2053 to 0.4101) | (0.3052 to 0.4217) |
| KI | −0.0213** | −0.0186** | 0.4486** | 0.5921** | −0.0328* | −0.1656** | 0.0703 | 0.0703* | 0.0203 | 0.0574* | ||
| 95% CI | (−0.0354 to –0.0071) | (−0.0262 to –0.0110) | (0.2708 to 0.6265) | (0.2658 to 0.9184) | (−0.0601 to –0.0055) | (−0.1963 to –0.1348) | (−0.1250 to 0.2655) | (0.0117 to 0.1290) | (−0.0721 to 0.1126) | (0.0037 to 0.1110) | ||
| g | 0.003961 | 0.003886 | 0.000568 | 0.000141 | 0.061934 | 0.005741 | 0.067174 | 0.115690 | 0.133835 | 0.125458 | ||
| V | −0.000061 | −0.000054 | 0.000263 | 0.000086 | −0.001768 | −0.000940 | 0.005529 | 0.009940 | 0.004102 | 0.009019 | ||
| H | 0.000024 | 0.000019 | 0.000008 | 0.000003 | 0.000726 | 0.000026 | 0.001926 | 0.002889 | 0.002688 | 0.002965 | ||
| R | 0.000000 | 0.000000 | 0.000000 | 0.000000 | 0.000205 | 0.000001 | 0.005285 | 0.010473 | 0.005792 | 0.010627 | ||
| RE | −0.000085 | −0.000073 | 0.000254 | 0.000083 | −0.002698 | −0.000967 | −0.001682 | −0.003422 | −0.004377 | −0.004573 | ||
| RE/RE (%) | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | ||
| V/RE (%) | 72.18 | 73.88 | 103.32 | 103.05 | 65.51 | 97.23 | −328.75 | −290.49 | −93.72 | −197.24 | ||
| H/RE (%) | −27.82 | −26.12 | 3.32 | 3.05 | −26.91 | −2.65 | −114.50 | −84.42 | −61.41 | −64.84 | ||
| R/RE (%) | 0.00 | 0.00 | 0.00 | 0.00 | −7.58 | −0.12 | −314.25 | −306.06 | −132.31 | −232.40 | ||
*P<0.05, **p<0.01.
†UEBMI was exclusively implemented in urban areas.
‡NRCMS was exclusively implemented in rural areas.
CI, Concentration Index; g, payments as fraction of income; H, horizontal inequity; KI, Kakwani Index; NRCMS, New Rural Cooperative Medical Scheme; OOP, out of pocket; R, reranking; RE, total redistributive effect; UEBMI, Urban Employee Basic Medical Insurance; V, vertical redistribution effect.
Table 4.
Progressivity, pure horizontal equity and reranking associated with the Chinese healthcare financing system in 2013
| Income quintiles/index | Per capita household expenditure | Indirect tax | Direct tax | UEBMI† | URBMI‡ | NRCMS§ | OOP payment | Total | |||||
| Urban | Rural | Urban | Rural | Urban | Rural | Urban | Rural | Urban | Rural | ||||
| Gini/CI | 0.2739** | 0.3392** | 0.2563** | 0.3210** | 0.5024** | 0.5571** | 0.2777** | −0.2702** | −0.0209** | 0.3502** | 0.4360** | 0.3149** | 0.4127** |
| 95% CI | (0.2620 to 0.2859) | (0.3282 to 0.3501) | (0.2435 to 0.2691) | (0.3109 to 0.3310) | (0.3781 to 0.6268) | (0.4649 to 0.6492) | (0.2565 to 0.2988) | (−0.3134 to –0.2270) | (−0.0287 to –0.0132) | (0.2849 to 0.4156) | (0.3534 to 0.5187) | (0.2755 to 0.3542) | (0.3389 to 0.4866) |
| KI | −0.0177** | −0.0182** | 0.2285** | 0.2179** | 0.0037 | −0.5441** | −0.3601** | 0.0763* | 0.0969* | 0.0409* | 0.0736** | ||
| 95% CI | (−0.0245 to –0.0109) | (−0.0273 to –0.0091) | (0.1095 to 0.3474) | (0.1287 to 0.3072) | (−0.0187 to 0.0262) | (−0.5888 to –0.4995) | (−0.3740 to –0.3462) | (0.0138 to 0.1388) | (0.0198 to 0.1740) | (0.0046 to 0.0772) | (0.0054 to 0.1418) | ||
| g | 0.004831 | 0.005025 | 0.003183 | 0.002244 | 0.051526 | 0.003095 | 0.005390 | 0.096436 | 0.106196 | 0.159070 | 0.118856 | ||
| V | −0.000054 | −0.000068 | 0.000721 | 0.000512 | 0.000562 | −0.001713 | −0.001952 | 0.009450 | 0.012458 | 0.009548 | 0.010936 | ||
| H | 0.000033 | 0.000024 | 0.000066 | 0.000033 | 0.001123 | −0.000005 | 0.000000 | 0.004776 | 0.002512 | 0.005979 | 0.002592 | ||
| R | 0.000000 | 0.000000 | 0.000056 | 0.000015 | 0.000149 | 0.000000 | 0.000000 | 0.012186 | 0.011150 | 0.013067 | 0.011266 | ||
| RE | −0.000086 | −0.000092 | 0.000599 | 0.000463 | −0.000710 | −0.001708 | −0.001953 | −0.007512 | −0.001204 | −0.009498 | −0.002921 | ||
| RE/RE (%) | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | ||
| V/RE (%) | 62.22 | 73.84 | 120.30 | 110.47 | −79.13 | 100.29 | 99.98 | −125.79 | −1034.41 | −100.52 | −374.39 | ||
| H/RE (%) | −37.78 | −26.16 | 10.95 | 7.13 | −158.14 | 0.31 | −0.02 | −63.57 | −208.58 | −62.95 | −88.73 | ||
| R/RE (%) | 0.00 | 0.00 | 9.35 | 3.34 | −20.99 | −0.02 | 0.00 | −162.21 | −925.83 | −137.58 | −385.67 | ||
*P<0.05, **p<0.01.
†UEBMI was exclusively implemented in urban areas.
‡URBMI was exclusively implemented in urban areas.
§NRCMS was exclusively implemented in rural areas.
CI, Concentration Index; g, payments as fraction of income; H, horizontal inequity; KI, Kakwani Index; KI, Kakwani Index; NRCMS, New Rural Cooperative Medical Scheme; OOP, out of pocket; R, reranking; RE, total redistributive effect; UEBMI, Urban Employee Basic Medical Insurance; URBMI, Urban Resident Basic Medical Insurance; V, vertical redistribution effect.
Table 5.
Progressivity, pure horizontal equity and reranking associated with the Chinese healthcare financing system in 2018
| Income quintiles/index | Per capita household expenditure | Indirect tax | Direct tax | UEBMI† | URRBMI | OOP payment | Total | ||||||
| Urban | Rural | Urban | Rural | Urban | Rural | Urban | Rural | Urban | Rural | Urban | Rural | ||
| Gini/CI | 0.3310** | 0.3719** | 0.3246** | 0.3491** | 0.5834** | 0.7277** | 0.3747** | −0.3052** | −0.0376** | 0.2855** | 0.4757** | 0.3093** | 0.3888** |
| 95% CI | (0.3186 to 0.3433) | (0.3510 to 0.3928) | (0.3126 to 0.3367) | (0.3312 to 0.3671) | (0.5149 to 0.6520) | (0.5375 to 0.9179) | (0.3475 to 0.4020) | (−0.3532 to –0.2572) | (−0.0513 to –0.0239) | (0.2175 to 0.3536) | (0.3880 to 0.5634) | (0.2697 to 0.3490) | (0.3209 to 0.4567) |
| KI | −0.0063 | −0.0228** | 0.2525** | 0.3558** | 0.0438** | −0.6361** | −0.4095** | −0.0454 | 0.1038** | −0.0216 | 0.0169 | ||
| 95% CI | (−0.0148 to 0.0022) | (−0.0391 to –0.0065) | (0.1863 to 0.3186) | (0.1749 to 0.5367) | (0.0169 to 0.0706) | (−0.6848 to –0.5875) | (−0.4348 to –0.3842) | (−0.1092 to 0.0184) | (0.0283 to 0.1793) | (−0.0567 to 0.0135) | (−0.0385 to 0.0722) | ||
| g | 0.0062664 | 0.005887 | 0.007438 | 0.005833 | 0.065123 | 0.005916 | 0.040412 | 0.115949 | 0.178104 | 0.200692 | 0.230235 | ||
| V | −0.000006 | −0.000104 | 0.001978 | 0.002161 | 0.003425 | −0.003777 | −0.017012 | −0.005087 | 0.025145 | −0.003869 | 0.008298 | ||
| H | 0.000035 | 0.000034 | 0.000106 | 0.000093 | 0.001156 | 0.000076 | 0.000403 | 0.003937 | 0.007489 | 0.005222 | 0.008269 | ||
| R | 0.000000 | 0.000000 | 0.000014 | 0.000001 | 0.000574 | 0.000009 | 0.000053 | 0.010351 | 0.019535 | 0.012655 | 0.020656 | ||
| RE | −0.000041 | −0.000137 | 0.001857 | 0.002067 | 0.001695 | −0.003862 | −0.017468 | −0.019375 | −0.001880 | −0.021746 | −0.020628 | ||
| RE/RE (%) | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | ||
| V/RE (%) | 14.86 | 75.44 | 106.49 | 104.56 | 202.07 | 97.80 | 97.39 | 26.26 | −1337.78 | 17.79 | −40.23 | ||
| H/RE (%) | −85.12 | −24.56 | 5.73 | 4.50 | 68.21 | −1.97 | −2.31 | −20.32 | −398.44 | −24.01 | −40.09 | ||
| R / RE (%) | 0.00 | 0.00 | 0.77 | 0.06 | 33.86 | −0.23 | −0.30 | −53.42 | −1039.34 | −58.19 | −100.14 | ||
*P<0.05, **p<0.01.
†UEBMI was exclusively implemented in urban areas.
CI, Concentration Index; g, payments as fraction of income; H, horizontal inequity; KI, Kakwani Index; OOP, out of pocket; R, reranking; RE, total redistributive effect; UEBMI, Urban Employee Basic Medical Insurance; URRBMI, Urban and Rural Resident Basic Medical Insurance; V, vertical redistribution effect.
Figure 2.
Concentration curve of healthcare payments and Lorenz curve in urban areas. The figure shows actual cumulative concentration curves for healthcare payments (including those associated with indirect taxes, direct tax, UEBMI, URBMI, URRBMI and OOP payments) and the Lorenz curve in urban areas in 2008, 2013 and 2018. OOP, out of pocket; UEBMI, Urban Employee Basic Medical Insurance; URBMI, Urban Resident Basic Medical Insurance; URRBMI, Urban and Rural Resident Basic Medical Insurance.
Figure 3.
Concentration curve of healthcare payments and Lorenz curve in rural areas. The figure shows actual cumulative concentration curves for healthcare payments (including those associated with indirect taxes, direct tax, the NRCMS, URRBMI and OOP payments) and the Lorenz curve in rural areas in 2008, 2013 and 2018. NRCMS, New Rural Cooperative Medical Scheme; OOP, out of pocket; URRBMI, Urban Resident Basic Medical Insurance.
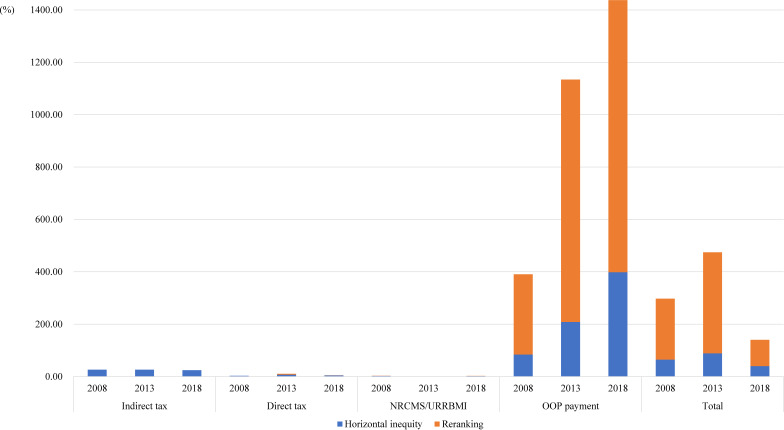
Figure 4.
Horizontal inequity and reranking for financing sources in urban areas in 2008, 2013 and 2018. Horizontal inequity and reranking are presented as percentages of the redistributive effect associated with each healthcare financing source in urban areas. OOP, out of pocket; UEBMI, Urban Employee Basic Medical Insurance; URBMI, Urban Resident Basic Medical Insurance; URRBMI, Urban Resident Basic Medical Insurance.
Figure 5.
Horizontal inequity and reranking for financing sources in rural areas in 2008, 2013 and 2018. Horizontal inequity and reranking are presented as percentages of the redistributive effect associated with each healthcare financing source in rural areas. NRCMS, New Rural Cooperative Medical Scheme; OOP, out of pocket; URRBMI, Urban Resident Basic Medical Insurance.
Sample characteristics
This study included 2398, 3600 and 3660 households in 2008, 2013 and 2018, respectively. Sample characteristics are shown in tables 1 and 2.
Total healthcare financing
Total healthcare payments as a proportion of household income increased over the period 2008–2018 (urban areas: 13.38% in 2008, 15.91% in 2013, and 20.07% in 2018; rural areas: 12.55% in 2008, 11.89% in 2013 and 23.02% in 2018). The RE values were all negative over the period 2008–2018 (urban areas: –0.004377 in 2008, –0.009498 in 2013 and –0.021746 in 2018; rural areas: –0.004573 in 2008, –0.002921 in 2013 and –0.020628 in 2018). The KI values increased over the period 2008–2013 and decreased over the period 2013–2018 (urban areas: 0.0203 in 2008, 0.0409 in 2013 and –0.0216 in 2018; rural areas: 0.0574 in 2008, 0.0736 in 2013 and 0.0169 in 2018). Horizontal inequity increased over the period 2008–2013 and decreased over the period 2013–2018 (urban areas: 193.72% in 2008, 200.52% in 2013 and 82.20% in 2018; rural areas: 297.24% in 2008, 474.40% in 2013 and 140.23% in 2018).
Indirect taxes
The RE values were all negative over the period 2008–2018 (urban areas: –0.000085 in 2008, –0.000086 in 2013 and –0.000041 in 2018; rural areas: –0.000073 in 2008, –0.000092 in 2013 and –0.000137 in 2018). The KI values remained almost unchanged, and were basically slightly regressive (it was negative but not statistically significantly so in urban areas in 2018). Horizontal inequity increased in urban areas and remained almost unchanged in rural areas over the entire period (urban areas: 27.82% in 2008, 37.78% in 2013 and 85.12% in 2018; rural areas: 26.12% in 2008, 26.16% in 2013, and 24.56% in 2018).
Direct taxes
The RE values were all positive over the period 2008–2018 (urban areas: 0.000254 in 2008, 0.000599 in 2013 and 0.001857 in 2018; rural areas: 0.000083 in 2008, 0.000463 in 2013 and 0.002067 in 2018). The direct taxes were strongly progressive. The KI values decreased over the period 2008–2013 and increased over the period 2013–2018 (urban areas: 0.4486 in 2008, 0.2285 in 2013 and 0.2525 in 2018; rural areas: 0.5921 in 2008, 0.2179 in 2013 and 0.3558 in 2018). Horizontal inequity remained almost unchanged (urban areas: 3.32% in 2008, 20.30% in 2013 and 6.50% in 2018; rural areas: 3.05% in 2008, 10.47% in 2013 and 4.56% in 2018).
Urban Employee Basic Medical Insurance
The RE values were negative in 2008 (–0.002698) and 2013 (–0.000710), but positive in 2018 (0.001695). UEBMI was regressive in 2008, near proportional in 2013, and progressive in 2018 (–0.0328 in 2008, 0.0037 in 2013, and 0.0438 in 2018). Horizontal inequity was small in 2008, but it increased in 2013 and 2018 (34.49% in 2008, 179.13% in 2013, and 102.07% in 2018).
Urban Employee Basic Medical Insurance, New Rural Cooperative Medical Scheme and Urban and Rural Resident Basic Medical Insurance
We compared and discussed the URBMI, NRCMS and URRBMI over the period 2008–2018 considering that they shared the same financing mechanism and covered the same target population in urban and rural areas, respectively. In addition, given that URBMI was piloted in 2007, only a minority of the population was covered by URBMI. Consequently, URBMI in 2008 was not included in the analysis. In urban areas, the RE values of URBMI/URRBMI were negative over the period 2013–2018 (–0.001708 in 2013, and –0.003862 in 2018). The KI values were all statistically significantly negative, and were strongly regressive (–0.5441 in 2013 and –0.6361 in 2018). Horizontal inequity as a percentage of the total RE was very close to 0. In rural areas, the RE values of NRCMS/URRBMI were all negative over the period 2008–2018 (–0.000967 in 2008,–0.001953 in 2013 and –0.017468 in 2018). The KI values were all statistically significantly negative, and were strongly regressive (–0.1656 in 2008,–0.3601 in 2013 and –0.4095 in 2018). Horizontal inequity as a percentage of the total RE was very close to 0.
OOP payments
The RE values were all negative over the period 2008–2018 (urban areas: –0.001682 in 2008, –0.007512 in 2013 and –0.019375 in 2018; rural areas: –0.003422 in 2008, –0.001204 in 2013 and –0.001880 in 2018). The KI values in urban areas increased during the period 2008–2013 but decreased during the period 2013–2018 (0.0703 in 2008, 0.0763 in 2013 and –0.0454 in 2018). Conversely, the KI values in rural areas increased during the entire period (0.0703 in 2008, 0.0969 in 2013 and 0.1038 in 2018). Horizontal inequity decreased in urban areas and increased in rural areas over the entire period (urban areas: 428.75% in 2008, 225.78% in 2013 and 73.74% in 2018; rural areas: 390.48% in 2008, 1134.41% in 2013 and 1437.78% in 2018).
Discussion
Overall, healthcare financing in both urban and rural areas over the period 2008–2018 underwent redistribution from the poor to the rich. In other words, healthcare financing increased the wealth inequality between the rich and the poor. Vertical equity, as measured by the KI, increased over the period 2008–2013 and decreased over the period 2013–2018 in both urban and rural areas. Horizontal inequity increased over the period 2008–2013 and decreased over the period 2013–2018 in both urban and rural areas.
Healthcare financing through indirect taxes resulted in redistribution from the poor to the rich. Vertical equity remained almost unchanged, and was basically slightly regressive in both urban and rural areas (it was negative but not statistically significantly so in urban areas in 2018). Horizontal inequity increased in urban areas and remained almost unchanged in rural areas over the period 2008–2018. Indirect tax was not propoor because the rich could transfer the tax burden to the poor. In most developed countries, indirect taxes only account for a minority of general taxation. For example, in 2018, indirect taxes accounted for 9.3%, 26.5%, and 21.5% of overall taxation revenue in the USA, Australia and Canada, respectively.11 Conversely, in China, indirect tax accounts for the majority of general taxation revenue. Within the region of interest within the current study, indirect tax accounted for 61.08%, 61.18% and 54.73% of general taxation revenue in 2008, 2013 and 2018, respectively.8
Direct tax experienced redistribution from the rich to the poor, and was strongly progressive in both urban and rural areas. Horizontal inequity remained almost unchanged. For households, direct tax primarily consisted of personal income tax, which was paid based on the grade of the taxpayer’s income. As shown in online supplemental tables 1 and 2, personal income tax was a progressive mechanism that was particularly focused on the rich. Individuals with a monthly income below a specified level were either not required to pay personal income tax or paid a lower tax rate than the rich, which resulted in a propoor distribution of the tax burden in relation to healthcare financing. Specifically, in 2008, nine grades of progressive tax rates were levied on monthly incomes greater than ¥1600. From 2012, seven grades of progressive tax rates were levied on monthly incomes greater than ¥3500. This policy adjustment aimed to reduce the tax burden on the poor by decreasing the number of grades, reducing the tax rates for the lower grades, and increasing the tax rates for the higher grades. This could explain why the progressivity of direct tax decreased during the first half of the study period and increased during the second half of the study period.
UEBMI experienced redistribution from the poor to the rich during the period 2008–2013, but then experienced redistribution from the rich to the poor during the period 2013–2018, and became increasingly progressive over the entire period 2008–2018 in terms of vertical equity. The finding of UEBMI progressivity is supported by earlier WHO research showing that social health insurance tended to be regressive during progress toward UHC as the health insurance scheme began to cover the previously uninsured.12 China began to establish social health insurance at the end of 1998, and the first health insurance scheme, UEBMI, provided universal health insurance for public sector workers and retirees at the local government level. UEBMI premiums are a fixed proportion (about 2%) of the employee’s salary. 13 However, workers in non-public sectors were not covered by UEBMI. In addition, government staff and workers in important state-owned enterprises remained enrolled in the Free Medical Service programme and the Labour Medical Service programme, which were medical benefits schemes that required no employee contributions. Thus, the government has gradually expanded UEBMI to cover all types of workers, including employees working in public and private enterprises, Chinese–foreign joint ventures, social organisations and private non-enterprise units, as well as migrant workers. Moreover, the Free Medical Service programme and the Labour Medical Service programme were abolished, and individuals who were previously insured under these programmes were required to enrol in the UEBMI scheme and commence individual contributions. Because employees working in private enterprises, international joint ventures, key state-owned enterprises, and government departments generally receive higher-than-average salaries, this resulted in the progressive nature of UEBMI when China began to move toward UHC. The horizontal inequity of UEBMI was small in 2008, but increased in 2013 and 2018. Since the expansion of health insurance coverage, UEBMI has covered employees in the public, private and almost all other sectors. However, UEBMI enrollees with equivalent incomes may have different income sources. For instance, the main source of income for workers in the public sector is their salary, but migrant workers and workers in the private sector tend to have other sources of income in addition to their salaries. UEBMI premiums are based on the enrollee’s monthly salary, and thus this resulted in an increase in horizontal inequity in relation to UEBMI.
URBMI, which was established in 2007, provided cover for people in urban areas who were not covered by UEBMI, such as students, the unemployed and the aged. The NRCMS, which was established in 2003, provided cover for the general population in rural areas. URBMI premiums were ¥131.0 and ¥400.5 in 2008 and 2013, respectively.14 NRCMS premiums were ¥96.2 and ¥370.6 in 2008 and 2013, respectively.15 Since 2016, URBMI and NRCMS have been merged into URRBMI and the flat rate premium was set at ¥723.2.15 URBMI, NRCMS and URRBMI premiums were flat rate contributions, meaning that each insured individual paid the same premium, regardless of their ATP. In other words, lower-income groups contributed a greater proportion of their income than higher-income groups. This resulted in an inequitable healthcare financing distribution for URBMI, NRCMS and URRBMI, although horizontal inequity as a percentage of the total RE was 0 or very close to 0 for URBMI, NRCMS and URRBMI. Although URBMI, NRCMS and URRBMI were very horizontally equitable, they experienced redistribution from the poor to the rich because they were both very regressive. This implies that a healthcare financing system with zero horizontal inequity is not necessarily equitable because flat rate contributions result in a high level of vertical inequity. Nevertheless, the optimal range of horizontal equity for a healthcare system remains unknown at present, and thus further research should be conducted in an effort to identify the optimum balance between vertical equity and horizontal equity.
OOP payments experienced redistribution from the poor to the rich over the period 2008–2018. Progressivity in urban areas increased during the period 2008–2013 but decreased during the period 2013–2018. Conversely, progressivity in rural areas increased during the entire period 2008–2018. Owing to the nature of postpaid payments, caution is necessary when interpreting the progressivity of OOP payments. In countries where OOP payments dominate healthcare financing, the rich can afford to pay for healthcare services via OOP payments, even for high-cost medical services,16 17 while it is difficult for the poor to make OOP payments for even basic medical services.18 19 This situation is obviously inequitable, and yet the associated healthcare financing distribution has been found to be progressive. In the first half of the period covered in our study, China’s move towards UHC emphasised expanding social health insurance coverage to all of the population.20 However, during this phase, social health insurance schemes focused on providing coverage for those with a lower reimbursement level.21 22 China’s social health insurance was organised and implemented at the city or county level, and thus fragmentation limited the scope for pooling of funding and failed to provide sufficient financial protection.23 24 Local officials were forced to choose between expanding coverage to a broader population and updating benefits packages. Based on the priority underlying UHC, health insurance was provided to more people at the cost of providing appropriate benefits package.25 Moreover, the reimbursement policy was not attractive. Although deductible was not high for the insured to get reimbursed, copayment was high and ceiling was also very low, and thus most of the cost of healthcare was paid for by the patients themselves. The scope for reimbursement was very limited.26 Healthcare services were only eligible for reimbursement if they were provided by designated hospitals and pharmacies, and reimbursement was subject to the health insurance lists. However, some common and extensively used medicines and medical devices were not covered by the lists, while some expensive medicines were covered by the lists and were recommended by the hospitals. Meanwhile, retrospective payment methods, such as fee-for-service reimbursement for hospitals, might encourage overtreatment as payment to providers was mainly based on volume rather than quality of services.27 These resulted in a high level of copayments by patients. Further, URBMI and NRCMS only covered inpatient services until the end of 2011.28 Although coverage has since gradually been expanded to include outpatient services, patients remained liable for 60%–70% of their outpatient costs and more than 50% of their inpatient costs.26 Thus, OOP payments meant that the cost of medical care was prohibitive for the poor, resulting in the development of a more progressive distribution of financing in both urban and rural areas during the period 2008–2013. Subsequently, after achieving nearly universal coverage, the government has continually improved the benefits packages of health insurance schemes by expanding service coverage, reducing copayments and raising the reimbursement ceiling to provide additional financial risk protection.28 Thus, residents tended to consume more medical services during the period 2013–2018. Urban residents, especially the poor, accounted for a greater proportion of OOP payments during this period compared with the period 2008–2013, which resulted in a decrease in progressivity. However, there were significant differences among health insurance schemes in terms of benefits. For example, in 2018, reimbursements under UEBMI, URRBMI (urban) and URRBMI (rural) were ¥3379.52 (US$510.70), ¥692.36 (US$104.63) and ¥629.40 (US$95.11) per person, respectively.3 29 Consequently, poor rural residents were less able to pay for medical services than urban residents, resulting in the continuous increase in progressivity during the period 2013–2018.
During the period 2008–2018, horizontal inequity decreased in urban areas and increased in rural areas. The extent of the horizontal inequity reflects the medical benefits provided by health insurance schemes. As part of the progress towards UHC in urban areas during the period 2008–2018, the benefits package and reimbursement levels of the main health insurance scheme, UEBMI, were continually improved. Although OOP payments increased and progressivity decreased, healthcare utilisation was improved and horizontal inequity was reduced over this period. Moreover, reranking associated with OOP payments indicated the economic rank order of individuals who funded healthcare via OOP payments. The fact that reranking decreased over this period indicates that impoverishment incurred by medical expenditure was alleviated in urban areas. Conversely, the benefits package and reimbursement levels in the main rural health insurance scheme were not improved. Thus, horizontal inequity associated with OOP payments, including reranking, continually increased during the period 2008–2018.
Strengths and limitations
Previous studies have only focused on the vertical equity in China’s healthcare financing system, and the overall picture in relation to healthcare financing equity has never been explored. We used standardised methods to analyse data from three waves of household surveys during the 10 years of progress towards implementation of UHC, systematically evaluating the vertical and horizontal equity of the Chinese healthcare financing system. Thus, our study not only provides the most recent evidence of China’s healthcare financing distribution, but also identifies the effects of health-system financing during progress towards UHC for the first time. A limitation of our study is that we only examined one province in China, the results might not fully represent the case in other parts of China. This limitation is, however, composed of by the fact that we used percentages and indices to evaluate the implementation of national policies and programmes across the entire population. In addition, as there is a variation in economic development across geographical locations in Jiangsu which is similar to the case in China, our findings in Jiangsu might reflect the national financing distribution. Another limitation is that data collections were conducted in 2008, 2013 and 2018 cross-sectionally to evaluate the change of healthcare financing equity, therefore, the observed trend during these three time points might not fully reflect the continuous change in healthcare financing equity.
Conclusions
China’s healthcare financing has experienced redistribution from the poor to the rich during 10 years of progress toward UHC. The flat rate contribution mechanism should be renovated for URBMI, NRCMS and URRBMI. In urban areas, the progressivity of OOP payments indicated that UHC improved access to and utilisation of healthcare, and horizontal inequity, including reranking, reflected adequate benefits package of UEBMI.
Footnotes
Handling editor: Sanni Yaya
Contributors: LS led and designed the study. GZ led the data collection, analysis and interpretation. MC contributed to the study design and data analysis, and wrote the first draft of the manuscript. LS contributed to the data analysis, reviewed the manuscript and helped write the final draft manuscript. All authors reviewed the content of the final version of the manuscript.
Funding: This study is funded by the National Natural Science Foundation of China (grant number: 71503137, 71874086) and the China Medical Board (grant number: 19-346). LS is supported by an NHMRC Early Career Fellowship (grant number: GNT1139826).
Disclaimer: The funding bodies were not involved in the design of the study, or data collection, analysis, and interpretation or in writing the manuscript.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available on request. The authors will make data available to scientists planning specified and agreed further analyses; for access, contact the corresponding author.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
References
- 1.Chen Z. Launch of the health-care reform plan in China. The Lancet 2009;373:1322–4. 10.1016/S0140-6736(09)60753-4 [DOI] [PubMed] [Google Scholar]
- 2.Chen M, Palmer AJ, Si L. Improving equity in health care financing in China during the progression towards universal health coverage. BMC Health Serv Res 2017;17:852 10.1186/s12913-017-2798-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Healthcare Security Administration Statistical bulletin on healthcare security 2018. Available: http://www.nhsa.gov.cn/art/2019/2/28/art_7_942.html [Accessed 09 Feb 2020].
- 4.Aronson JR, Johnson P, Lambert PJ. Redistributive effect and unequal income tax treatment. Econ J 1994;104:262–70. 10.2307/2234747 [DOI] [Google Scholar]
- 5.Wagstaff A, van Doorslaer E. Progressivity, horizontal equity and reranking in health care finance: a decomposition analysis for the Netherlands. J Health Econ 1997;16:499–516. 10.1016/S0167-6296(97)00003-9 [DOI] [PubMed] [Google Scholar]
- 6.Wang Z, Zhou X, Gao Y, et al. . Did expansion of health insurance coverage reduce horizontal inequity in healthcare finance? A decomposition analysis for China. BMJ Open 2019;9:e025184 10.1136/bmjopen-2018-025184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wilde PE. The analysis of household surveys: a microeconometric approach to development policy. American Journal of Agricultural Economics 2000;82:780–2. [Google Scholar]
- 8.Jiangsu Provincial Bureau of Statistics Jiangsu statistical Yearbook 2019; 2019.
- 9.O'Donnell O, Ev D, Wagstaff A, et al. . Analyzing health equity using household survey data: a guide to techniques and their implementation. Washington: World Bank, 2007. [Google Scholar]
- 10.Deaton AS, Zaidi S. Guidelines for constructing consumption aggregates. Washington: World Bank, 2002. [Google Scholar]
- 11.World Bank Taxes on income, profits and capital gains (% of total taxes). Available: https://data.worldbank.org/indicator/GC.TAX.YPKG.ZS?name_desc=false&view=chart [Accessed 09 Feb 2020].
- 12.World Health Organization Sustainable health financing, universal coverage and social health insurance. Available: http://www.who.int/health_financing/documents/cov-wharesolution5833/en/index.html [Accessed 13 Feb 2020].
- 13.Liu GG, Zhao Z, Cai R, et al. . Equity in health care access to: assessing the urban health insurance reform in China. Soc Sci Med 2002;55:1779–94. 10.1016/S0277-9536(01)00306-9 [DOI] [PubMed] [Google Scholar]
- 14.Department of Population and Employment Statistics, National Bureau of Statistics, Department of Planning and Finance, Ministry of Human Resources and Social Security China labour statistical Yearbook 2009; 2009.
- 15.National Bureau of Statistics of China China health statistical Yearbook 2019; 2019.
- 16.Nguyen MT. Re‐examining the effects of public health insurance: the case of nonpoor children in Vietnam. Health Econ 2020;29:294–305. 10.1002/hec.3980 [DOI] [PubMed] [Google Scholar]
- 17.Piyasena MMPN, Murthy GVS, Yip JLY, et al. . Systematic review on barriers and enablers for access to diabetic retinopathy screening services in different income settings. PLoS One 2019;14:29. 10.1371/journal.pone.0198979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Braimah JA, Sano Y, Atuoye KN, et al. . Access to primary health care among women: the role of Ghana’s community-based health planning and services policy. Prim Health Care Res Dev 2019;20:7 10.1017/S1463423619000185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mulyanto J, Kringos DS, Kunst AE. Socioeconomic inequalities in healthcare utilisation in Indonesia: a comprehensive survey-based overview. BMJ Open 2019;9:e026164 10.1136/bmjopen-2018-026164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yip W, Fu H, Chen AT, et al. . 10 years of health-care reform in China: progress and gaps in universal health coverage. The Lancet 2019;394:1192–204. 10.1016/S0140-6736(19)32136-1 [DOI] [PubMed] [Google Scholar]
- 21.Liu GG, Vortherms SA, Hong X. China’s Health Reform Update. Annu Rev Public Health 2017;38:431–48. 10.1146/annurev-publhealth-031816-044247 [DOI] [PubMed] [Google Scholar]
- 22.Meng Q, Yang H, Chen W, et al. . People’s Republic of China Health System Review. Manila: World Health Organization, 2015. [Google Scholar]
- 23.Meng Q, Xu L, Zhang Y, et al. . Trends in access to health services and financial protection in China between 2003 and 2011: a cross-sectional study. The Lancet 2012;379:805–14. 10.1016/S0140-6736(12)60278-5 [DOI] [PubMed] [Google Scholar]
- 24.Chen W, Zhang Q, Renzaho AMN, et al. . Social health insurance coverage and financial protection among rural-to-urban internal migrants in China: evidence from a nationally representative cross-sectional study. BMJ Global Health 2017;2:e000477 10.1136/bmjgh-2017-000477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen M, Fang G, Wang L, et al. . Who benefits from government healthcare subsidies? an assessment of the equity of healthcare benefits distribution in China. PLoS One 2015;10:e0119840. 10.1371/journal.pone.0119840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yip WC, Hsiao WC, Chen W, et al. . Early appraisal of China’s huge and complex health-care reforms 2012;379:833–42. [DOI] [PubMed] [Google Scholar]
- 27.Chen Y, Schweitzer SO. Issues in drug pricing, reimbursement, and access in China with references to other Asia-Pacific region. Value Health 2008;11 Suppl 1:S124–9. 10.1111/j.1524-4733.2008.00376.x [DOI] [PubMed] [Google Scholar]
- 28.Ministry of Health Notice to implement NRCMS in 2011. Available: http://www.nhc.gov.cn/jws/s3581sg/201104/549c057f822147988cbc72ce70750842.shtml [Accessed 13 Feb 2020].
- 29.National Bureau of Statistics of China Statistics on China’s Basic Medical Insurance, 2018. Available: http://data.stats.gov.cn/easyquery.htm?cn=C01
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2020-003570supp001.pdf (60.3KB, pdf)