Abstract
Objective
To report the effectiveness of physiotherapist-led interventions in improving pain and function in young and middle-aged adults with hip-related pain.
Design
Systematic review and meta-analysis.
Data sources
A comprehensive, reproducible search strategy was performed on five databases in May 2019. Reference lists and grey literature were also searched.
Eligibility criteria for selecting studies
Population: people aged ≥18 years with hip-related pain (with or without a diagnosis of femoroacetabular impingement syndrome). Intervention(s): physiotherapist-led interventions for hip pain. Comparators: sham treatment, no treatment or other treatment (eg, hip arthroscopic surgery). Outcomes: primary outcomes included patient-reported hip pain and function. Secondary outcomes included physical function measures.
Results
1722 papers were identified. After exclusion criteria were applied, 14 studies were included for analysis. They had varied risk of bias. There were no full-scale placebo-controlled randomised controlled trials (RCTs) of physiotherapist-led treatment. Pooled effects ranged from moderate effects (0.67 (95% CI 0.07 to 1.26)) favouring physiotherapist-led intervention over no treatment post-arthroscopy, to weak effects (−0.32 (95% CI 0.57 to 0.07)) favouring hip arthroscopy over physiotherapist-led treatment.
Conclusion
Physiotherapist-led interventions might improve pain and function in young and middle-aged adults with hip-related pain, however full-scale high-quality RCT studies are required.
PROSPERO registration number
CRD42018089088.
Keywords: rehabilitation, physiotherapy, hip, exercise, arthroscopy
Background
Musculoskeletal conditions, such as hip-related pain, are leading causes of pain and disability in the community, and the second largest global contributor to years lived with disability.1 Hip and groin injuries are common in active individuals, for example, accounting for up to 18% of professional male football injuries.2–4 The true prevalence of non-arthritic hip pain in the general population is unknown, however the burden of hip pain is high, with younger adults with hip-related pain reporting poor patient-reported outcome scores for pain, physical activity and quality of life5–8 at a time of life where work and family commitments are large.
Hip-related pain may be classified into three categories, including femoroacetabular impingement (FAI) syndrome, acetabular dysplasia and other pathology without morphological variants (labral, chondral and ligamentum teres pathology).9 Of these, FAI syndrome is the most commonly diagnosed clinical condition10 and is evident in 49% of people with hip pain.11 Patients with FAI syndrome present with pain, a morphological variant in hip shape on radiographs, with or without intra-articular imaging findings such as labral and/or chondral pathology,12 and reduced activity and quality of life.13 14
Non-surgical treatment approaches should be the first-line options for musculoskeletal pain conditions (evident from clinical guidelines for osteoarthritis (OA)15 16 and low back pain,17 due to the far greater costs and risks associated with surgery. Establishing the efficacy of non-surgical treatments for hip pain is critical. Physiotherapist-led interventions have the potential to reduce the burden of hip pain, with current evidence guiding physiotherapist-led treatments to target characteristic modifiable physical impairments18 (strength, range of motion, functional task performance, neuromuscular/motor/movement control). At present, the level of evidence supporting the efficacy of physiotherapist-led interventions for hip pain and FAI syndrome is unclear.
Review aim
This systematic review aimed to identify the effectiveness of physiotherapist-led interventions in improving pain and function in young and middle-aged adults who experience hip pain, when compared with sham treatment, no treatment and other treatment. This included non-operative and postoperative patient groups. This review specifically used the participants, interventions, comparators, outcomes (PICO) format.
Methods
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. Literature search criteria and methods were proposed and agreed on by two authors (JK, SC), and were established a priori to minimise selection bias.
Eligibility criteria for selecting studies
Studies were eligible for inclusion if they were reported in English; reported level IV evidence or above; contained human subjects with hip pain; had at least 10 participants in the overall study sample (5 per group in studies with more than one group) and examined the effectiveness of physiotherapist-led interventions. All quantitative study designs were considered, including randomised controlled trials (RCTs), prospective or retrospective approaches.19 Studies were excluded if: hip pain was due to hip OA, dysplasia or congenital disorder; greater trochanteric pain syndrome and other conditions that are not related to the hip joint; the study evaluated other therapies that were not physiotherapist-led interventions; the study included populations of children or older adults (aged >50 years) or the study was a published abstract, non-peer-reviewed or was written in a language other than English.
Participants/Population
People aged 18–50 years with hip pain (based on the mean or median age of the study sample), including studies that included a diagnosis of FAI syndrome.
Intervention(s), exposure(s)
Studies reporting physiotherapist-led interventions for hip pain and/or function were included.
Comparator(s)/Control
Studies using sham treatment, no treatment or other treatment (eg, hip arthroscopy surgery) as the comparator/control treatment were included.
Outcomes
Primary outcomes included patient-reported hip pain and function. Secondary outcomes included: hip joint range of motion, hip muscle strength, functional task performance, electromyography (EMG) and motor control, balance and proprioception, biomechanics and gait analysis and other patient-reported outcome measures.
Search strategy
A comprehensive, reproducible search strategy was performed on the following databases from earliest available to 6 November 2017 and was then repeated on 20 May 2019: Medline, CINAHL, Cochrane library, EMBASE and PEDro. Reference lists of included studies were also manually searched for relevant papers. Grey literature, including the Clinical Trials database and the Australia and New Zealand Clinical Trials Registry were searched to identify potential studies that may have been published. Where data were insufficient, authors were contacted and asked to provide missing data. The search terms used PICO format and full search strategy of each database is contained in online supplementary appendix 1. The search strategy was conducted by two reviewers (JK, SC) and used the PICO format, and included:
bjsports-2019-101690supp001.pdf (131.1KB, pdf)
P=human adults (18–50 years) with hip pain.
I=physiotherapist-led interventions.
C=sham treatment, no treatment, other treatment (eg, surgery).
O=pain, function, other patient-reported outcome measures. Function may include hip joint range of motion, hip muscle strength, measures of functional task performance, EMG, gait analysis.
We also used Web of Science to track the forward and backward citations and reference lists of included studies. The strategy was adapted as appropriate for each database. The full search strategy used is contained in online supplementary appendix 1.
Title, abstract and full-text screening was conducted by two independent reviewers (JK, HH) using Covidence (Veritas Health Innovation, Australia) software. Any disagreements were resolved by a third independent reviewer (KC).
Risk of bias assessment
The Cochrane Collaboration Risk of Bias tool for Clinical Trials was used to appraise risk of bias. Included studies were rated by two independent reviewers (MB, MJS). Any disagreements between reviewers were discussed in a consensus meeting and an independent arbitrator (JK) was employed when consensus could not be met. Agreement between raters was determined using Cohen’s Kappa (κ). If risk of bias was high in >three out of five categories, overall study risk was rated as high, if risk was high in three out of five categories, study risk was moderate and if risk was high in <three out of five categories, overall study risk was rated as low.20 All studies were included in subsequent analyses, and sensitivity analyses were performed as appropriate.
Data extraction, synthesis and analyses
All potential references were imported into Endnote X7 (Thomson Reuters, Carlsbad, California, USA) and duplicates removed. Data were extracted by two independent reviewers (JK, ABM). Any discrepancies in data extraction were resolved by an independent arbitrator (KC).
Findings were summarised and population characteristics (age, gender, type and description of hip OA, duration of symptoms), and details of outcome measures, length of follow-up and type intervention undertaken were collated. We have reported main findings only for studies where the physiotherapist-led intervention was compared with a comparator/control intervention (RCT design) in order to ensure only higher quality evidence was included.
For studies of RCT design, follow-up scores were compared with the published Patient Acceptable Symptom State (PASS) scores for that outcome (if known) and change scores were compared with the published minimal important change (MIC) score for that outcome (if known). The proportion of people who achieve a PASS from follow-up scores was estimated using previously published methods, incorporating means, SD, sample size and z-scores.21 Previously published relevant PASS scores include 88 points (Hip Osteoarthritis and disability Outcome Score (HOOS)-pain)22 and 83 points (HOOS-quality of life (QOL))22 1-year posthip arthroplasty; 58 points (International Hip Outcome Tool (IHOT)-33)23 1–5 years posthip arthroscopy and 98 points (Hip Outcome Score (HOS)-activity of daily living (ADL))24 and 94 points (HOS-Sport)24 1-year posthip arthroscopy. Previously published MIC scores include 9 points (HOOS-pain),25 11 points (HOOS-QOL),25 10 points (IHOT-33)25 1–2 years posthip arthroscopy; 15 points (HOS-ADL)24 1-year posthip arthroscopy and 28 points (HOS-Sport) 6 months posthip arthroscopy.24
Data analyses were conducted by two investigators (AIS and JK). The ‘meta’ package (V.4.9–5), from the R statistical software package (V.3.5.1) was used to calculate relevant effect sizes, produce forest plots and pool data in a meta-analysis where relevant (https://www.r-project.org/). Standardised mean differences (SMD) were calculated for the studies of RCT design, to determine the magnitude of the effect of any interventions within groups or between groups. Where data were deemed statistically and clinically homogenous, meta-analyses were undertaken using a random effects model. In order to undertake SMD calculations in studies where non-normally distributed data were presented, the IQR was calculated.26 For analysis of outcomes that reported within group (pre-intervention to post-intervention), the standardised paired difference (SPD) was calculated from the sample size, mean and SD of the difference from pre-intervention to post-intervention time points. An additional requirement for SPD calculation was to account for the within-person correlation (r) between the two time points. If between-limb correlation was not reported, a conservative estimate of r=0.5 was used.27 Standardised mean/paired difference magnitude was interpreted as: ≥0.8 large effect; 0.5–0.79 moderate effect and 0.2–0.49 weak effect.28 Where SMDs could not be calculated, study conclusions were presented in tables, and best evidence synthesis was performed. For the best evidence synthesis, evidence was categorised as ‘strong’ if there were multiple high-quality clinical trials or cohort studies; ‘moderate’ if there was either one high-quality clinical trial or cohort study and more than two high-quality case-control studies or pilot clinical trials, or more than three high-quality case-control studies; ‘limited’ if there were either one or two case-control studies or pilot clinical trials, or multiple cross-sectional studies and ‘insufficient’ if there was not more than one cross-sectional study.20 All data used in calculations of SMDs and SPDs have been shared publicly at Figshare (https://figshare.com/s/d18bcb066f1de48861cf).
Results
Search strategy
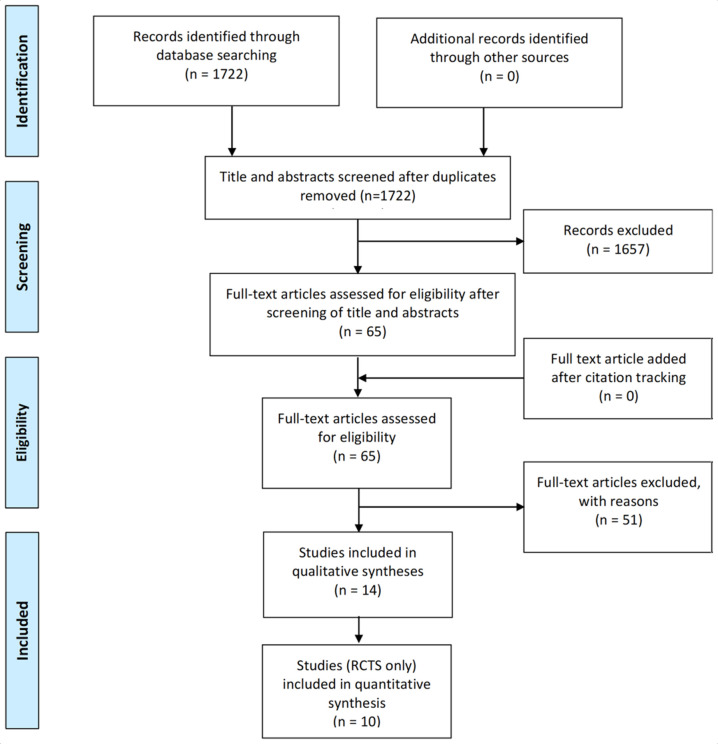
The search yielded 1722 titles and abstracts for screening. Sixty-five full texts were screened and 51 were excluded. There were 14 papers in the final analyses. An overview of the study identification process is provided in figure 1. Characteristics of the included studies are presented in table 1. The number of studies excluded along with reasons is provided in online supplementary appendix 2.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow chart of study inclusion. RCT, randomised controlled trial.
Table 1.
Summary of included studies
| Study | Title | Study type | Overall risk of bias | Inclusion criteria | Exclusion criteria | Number (PT/control) at baseline | Number (PT/control) at follow-up | Age mean (SD) (PT/control) | Sex (M/F) (PT/control) | BMI kg/m2 mean (SD) (PT/control) | Intervention type | Control type | Primary end point | Other follow-up | Primary outcomes | Secondary outcomes | Included in SMD calculation (Y/N) |
| Bennell, et al 2017 33 | Efficacy of adding a physiotherapy rehabilitation programme to arthroscopic management of femoroacetabular impingement syndrome: a randomised controlled trial | Pilot RCT | Moderate | Aged >16 years; FAI; scheduled for arthroscopy | Hip OA (Tönnis >grade 1); professional athlete; concurrent injury; unable to attend study physiotherapist; unwilling refrain from rehab | 14/16 | 11/13 | 31 (7) 29 (8) |
12/2 12/4 |
24.6 (2.2) 25.2 (3.2) |
7 PT sessions (1×pre-op; 6×postoperative) education manual therapy deep hip rotator retraining, stretching, bike, pool jog | No therapy allowed | 14 weeks | 24 weeks | IHOT-33; HOS-Sport subscale | HAGOS subscales; Tegner; HSAS; HOS-ADL |
Y |
| Coppack, et al 2016 30 | Physical and functional outcomes following multidisciplinary residential rehabilitation for prearthritic hip pain among young active UK military personnel | Case series | High | Non-surgical and postsurgical military personnel attending for Physical therapy for of hip pain | Not reported | 40 | 40 | 33 (7) | 27/13 | 25.8 (4.5) | 5 hours/day 3 weeks. Hip ROM and strength, core and trunk muscle function, deep hip stabiliser exercise, correct gait balance retraining weight management, patient education | NA | 3 weeks | NA | HAGOS subscales Pain VAS |
Y-balance flexion ROM IR ROM; shuttle test |
N |
| Emara, et al 2011 31 | Conservative treatment for mild femoroacetabular impingement | Case series | High | Men and women with unilateral hip pain; alpha angle <60 | Aged >55 years; skeletally immature; hip disease or hip surgery; alpha angle >60; hip OA | 37 | 37 | NR | 27/10 | NR | Stage 1=rest, NSAIDs Stage 2=stretching exercise Stage 3 and 4=ADL modification |
NA | 6 months | 24 months | HHS NAHS VAS |
Flexion ROM Extension ROM Abduction ROM Adduction ROM ER in flexion ROM ER in extension ROM IR in flexion ROM IR in extension ROM |
N |
| Grant, et al 2017 34 | The HAPI ‘Hip Arthroscopy Prehabilitation Intervention’ study: does prehabilitation affect the outcomes in patients undergoing hip arthroscopy for femoroacetabular impingement? |
Pilot RCT | Moderate | Men and women aged >18 years with FAI, awaiting hip arthroscopy | Radiographic evidence of hip dysplasia; grades 3–4 OA; AVN; rheumatology disorders; <18 years; previous hip surgery |
9/9 | 8/8 | 38 (6) | 4/4 1/7 |
NR | Five visits, points of interest were two pre-operative exercise for hip strength | Five visits, two pre-operative, same as intervention group except no pre-operative exercise advice | 2 weeks pre-operative | NA | NAHS | Abduction strength Adduction strength Flexion strength ER strength Knee extension strength |
Y |
| Griffin, et al 2018 7 | Hip arthroscopy vs best conservative care for the treatment of femoroacetabular impingement syndrome (UK FASHIoN): a multicentre randomised controlled trial | RCT | Moderate | Men and women aged 16+ years with hip pain, suitable for hip arthroscopy | Hip OA (Tönnis >1) significant hip pathology past hip surgery | 177/171 | 162/157 | 35 (9)/35 (10) | 113/64 100/71 |
NR | Personalised hip therapy between 6 and 10 treatments over 12–24 weeks of assessment, education, exercises (core, neuromotor control, progressive strength, stretching) pain relief | Hip arthroscopy surgery as pragmatically determined by surgeon, including acetabular rim trimming, labral dedridement or repair, femoral osteoplasty | 12 months | 6 months | IHOT-33 | EQ-5D-5L EQ-5D VAS SF-12 PCS SF-12 MCS |
Y |
| Guenther, et al 2017 35 | A pre-operative exercise intervention can be safely delivered to people with femoroacetabular impingement and improve clinical and biomechanical outcomes | Case series | Moderate | FAI on MRA; positive impingement test; anterior groin pain | Hip OA; CSI within last month; hip surgery; significant lower body injuries or conditions; osteonecrosis of the hip; planned commencement or current enrolment in a hip strengthening exercise programme | 20 | 20 | 30 (7) | 18/2 | 24.1 (2.9) | Progressive phased strength programme, bilateral intervention. Exercises at home 4×week Phase I—activation, neuromuscular control, endurance Phase II—strength and intensity Phase III—strength and function |
NA | 10 weeks | NA | HOOS Symptoms HOOS-Pain HOOS-ADL HOOS-Sport HOOS-QOL |
Abduction strength Adduction strength Extension strength Flexion strength ER strength IR strength timed stair climb test |
N |
| Harris-Hayes, et al 201639 | Movement pattern training to improve function in people with chronic hip joint pain: a feasibility randomised clinic trial | Pilot RCT | Low | Aged 18–40 years; anterior hip or groin pain >3 months; positive FADIR test | Previous hip surgery or fracture; contraindication to MRI; pregnancy; neurological involvement; knee or low back pain; BMI >30 | 18/17 | 16/16 | 27 (5)/29 (5) | 1/15 4/12 |
24.2 (3.0) 24.4 (2.6) |
Movement pattern retraining; task-specific training for basic functional tasks; progressive strengthening of hip musculature. 6×1 hour visits over 6 weeks individualised and progressed |
Wait list control | 6 weeks | NA | HOOS Symptoms HOOS-Pain HOOS-ADL HOOS-Sport HOOS-QOL |
ABD strength ER 0 strength ER 90 strength Adduction single leg squat |
Y |
| Hunt, et al 2012 32 | Clinical outcomes analysis of conservative and surgical treatment of patients with clinical indications of prearthritic, intra-articular hip disorders | Case-control | High | Anterior or lateral hip pain; pain on activity; pain-associated mechanical symptoms; pain at rest; positive anterior hip impingement test, FABER test, log roll or resisted straight leg-raise test | Aged >50 years; history hip surgery; inflammatory arthropathy, hip infection or tumour, current lumbar radiculopathy; hip OA (Tönnis 2–3) | 27/29 | 27/29 | 33 (11)/36 (11) | 2/23 27/29 |
25.3 (7) 25.9 (5) |
Conservative interventions, patient education, activity modification, directed physical therapy protocol medications | Same as PT plus injection and surgery (when patient not satisfied with PT) | 12 months | NA | Numeric pain scale HHS WOMAC Baecke Questionnaire SF-12 PCS SF-12 MCS NAHS |
NA | N |
| Kemp, et al 201836 | A pilot randomised clinical trial of physiotherapy (manual therapy, exercise and education) for early onset hip osteoarthritis posthip arthroscopy | Pilot RCT | Moderate | Aged 18–50 years; 4–14 months posthip arthroscopy for early hip OA (chondropathy outerbridge grade ≥1); pain ≥30/100 |
Hip bursitis or tendinopathy; surgical complications; planned further surgery in the following 12 months | 10/7 | 9/6 | 32 (10)/31 (6) | 6/4 2/5 |
26.3 (5.3) 24.4 (4.7) |
8×30 min sessions over 12 weeks, and home exercise programme 4×week (i) Manual hip joint and soft tissue mobilisation and stretching; (ii) hip muscle retraining; (iii) trunk muscle retraining; (iv) functional, proprioceptive and sports-specific or activity-specific retraining; (v) enhancing physical activity and (vi) education |
8×30 min sessions over 12 weeks, education only | 12 weeks | NA | HOOS Symptoms HOOS-Pain HOOS-ADL HOOS-Sport HOOS-QOL IHOT |
Abduction strength Adduction strength Extension strength Flexion strength ER Strength IR Strength Flexion ROM |
Y |
| Kemp, et al 201840 | The Physiotherapy for Femoroacetabular Impingement Rehabilitation Study: a pilot randomised controlled trial | Pilot RCT | Low | Aged 18–50 years; no surgery; FAI (pain >3/10, >6 weeks, in hip or groin; alpha angle >60) | Past surgery; significant other hip disease; significant other disease; pregnancy; physiotherapy within past 3 months | 17/7 | 14/6 | 37 (8)/38 (10) | 5/12 2/5 |
25.1 (3.7) 26.1 (2.4) |
Individualised, progressive programme 8×30 min 1:1 and 12×30 min supervised gym, 2×HEP (12-week intervention). Hip strength, trunk strength, functional retraining, manual therapy, education, fitness programme | Standardised programme 8×30 min 1:1 and 12×30 min supervised gym, 2×HEP (12-week intervention). Stretching, manual therapy, education | 12 weeks | Nil | IHOT | HOOS-QOL HOOS-Pain Adduction strength Abduction strength Extension strength ER strength Flexion ROM Single leg hop Side bridge |
Y |
| Mansell, et al 2018 8 | Arthroscopic surgery or physical therapy for patients with femoroacetabular impingement syndrome | RCT | Low | Military personnel and families, FAI and/or labral tear (pain in hip or groin; pain on flexion, pain on FADIR; pain relief after injection), candidate for surgery (failed 6/52 conservative; positive cross-over or alpha angle >50) | Hip OA; other concurrent hip disease; workers compensation; positive LBP findings; pregnancy; past surgery; physiotherapy within previous 6 months | 40/40 | 33/29 | 31 (7)/30 (7) | 21/19 26/14 |
27.5 (4.3) 28.2 (4.4) |
Standardised, supervised PT, 2×week for 6 weeks. Included elements=manual therapy (joint mob, MWM, soft tissue therapy), stretching, therapeutic and motor control exercises |
Pragmatic hip arthroscopy surgery (acetabular rim trimming, labral dedridement or repair, femoral osteoplasty) | 2 years | 6, 12 months | HOS-ADL HOS-Sport |
IHOT Global rating of change |
Y |
| Palmer, et al 2019 41 | Arthroscopic hip surgery compared with physiotherapy and activity modification for the treatment of symptomatic femoroacetabular impingement: multicentre randomised controlled trial | RCT | Low | Aged 18–60 years, referred to secondary or tertiary care. Clinically and radiologically diagnosed FAIS (no imaging thresholds used. Instead surgeons qualitatively assessed morphology). | Physiotherapy in past 12 months, past hip surgery, hip OA (KL≥2), hip dysplasia (LCEA<20). | 110/112 | 88/100 | 36 (10)/36 (10) | 37/73 38/74 |
26.6 (4.8)/25.9 (4.8) | Goal-based supervised PT, up to 8 sessions over 5 months. Patient goals supplemented with programme focusing on muscle strength, core stability and movement control. Avoidance of extreme ROM encouraged. No specific programme details available | Pragmatic hip arthroscopy surgery (osteochondroplasty, labral repair or debridement, chondral debridement and microfracture as deemed appropriate by surgeon) | 8 months | HOS-ADL | HOS-Sport NAHS OHS HAGOS IHOT-33 EQ-5D-3L PainDETECT HADS Hip flexion ROM Hip extension ROM Hip abduction ROM Hip adduction ROM Hip ER ROM Hip IR ROM |
||
| Smeatham, et al 2017 37 | Does treatment by a specialist physiotherapist change pain and function in young adults with symptoms from femoroacetabular impingement? A pilot project for a randomised controlled trial | Pilot RCT | Moderate | FAI diagnosed Surgeon (FAI on X-ray; Aged 18 and 50 years; groin/anterolateral hip pain; mechanical symptoms; pain FADIR); willing for treatment by a specialist physiotherapist, and abstain from treatment outside study protocol |
Previous hip surgery to the hip or pelvis; other significant hip pathology; back symptom; chronic pain; inability to comply with the physiotherapy protocol |
15/15 | 11/12 | 36/33 | 7/8 5/10 |
NR | Pragmatic care from specialist physio. Any number of sessions allowed. Manual therapy and exercise to address movement deficits | Routine care (analgesia, continuation self-management or exercise previously given | 3 months | NA | NAHS HOS LEFS VAS |
NA | Y |
| Wright, et al 2016 38 | Non-operative management of femoroacetabular impingement: a prospective, randomised controlled clinical trial pilot study | Pilot RCT | Moderate | Aged 18–50 years clinical diagnosis FAI (hip flexion <95°, internal rotation <10°, positive FADIR or FABER) radiological diagnosis FAI (alpha angle >55°; lateral centre edge angle >35; crossover sign) | Previous hip surgery; other surgical procedure of lower limb in the prior 6 months; pre-existing hip disease pregnancy; opioid analgesia or CSI past 30 days; advanced osteoporosis; BMI >38; cardiopulmonary disease | 8/7 | 8/7 | 31 (5)/36 (12) | 3/4 1/7 |
25.6 (3.7) 24.1 (7.4) |
Manual therapy and supervised exercise | Advice and home exercise | 7 weeks | NA | HOS-ADL HOS-Sport NPRS LEFS SANE-ADL SANE-Sport |
Depth of squat Triple hip Hip flexion ROM Hip flexion Strength FABER |
Y |
ADL, activity of daily living; AVN, avascular necrosis; BMI, body mass index; CSI, corticosteroid injection; EQ-5D-5L, Euroquol Questionnaire; ER, external rotation; F, female; FABER, flexion-abduction-external rotation test; FADIR, flexion-adduction-internal rotation test; FAI, femoroacetabular impingement; HAGOS, Copenhagen Hip and Groin Outcome Score; HHS, Harris Hip Score; HOOS, Hip Osteoarthritis and disability Outcome Score; HOS, Hip Outcome Score; HSAS, Hip Sports Activity Scale; IHOT, International Hip Outcome Tool; IR, internal rotation; KL, Kellgren Lawrence; LCEA, lateral centre edge angle; LEFS, lower extremity functional scale; m, metre; M, male; MCS, emotional function subscale; MRA, magnetic resonance arthrogram; n, no; NA, not applicable; NAHS, Non-Arthritic Hip Score; NPRS, Numeric Pain Rating Scale; NR, not reported; NSAIDs, non-steroidal anti-inflammatory drugs; OA, osteoarthritis; PA, physical activity; PCS, physical function subscale; PT, physiotherapy/physical therapy; QOL, quality of life; RCT, randomised controlled trial; ROM, range of motion; SANE, single assessment numeric evaluation; SF-12, Short Form-12 Questionnaire; SMD, standardised mean difference; VAS, Visual Analogue Scale; WOMAC, Western Ontario and McMaster Universities Arthritis Index; Y, yes.
bjsports-2019-101690supp002.pdf (41.4KB, pdf)
Risk of bias
Online supplementary appendix 3 contains the results of risk of bias assessment using the Cochrane Risk of Bias Tool. Agreement between raters occurred on 54 out of 70 items, where κ=0.65, which represents moderate agreement.29 Following discussion, consensus was obtained for all items. Overall results for the risk of bias assessment are mentioned in table 1. Three studies had a high risk of bias,30–32 seven studies had a moderate risk of bias7 33–38 and four studies had a low risk of bias.8 39–41 In the included studies, the overall risk of performance bias (blinding of participants and personnel) and detection bias (blinding of outcome assessors) was high (high in ≥nine studies); the risk of attrition bias (incomplete outcome data) and the risk of selection bias (random sequence generation and allocation concealment) was moderate (high in six to eight studies) and the risk of reporting bias (selective reporting of outcomes) was low (high in <six studies).
bjsports-2019-101690supp003.pdf (47KB, pdf)
Participants
The 14 included studies contained 542 patients (283 men, 259 women) with sample sizes of the physiotherapist-led intervention groups ranging from 8 patients38 to 177 patients.7 Ten studies were of RCT design. Mean participant age ranged from 27 to 38 years, while the mean body mass index (BMI) ranged from 24.1 to 27.5 kg/m2. Ten studies included participants based on a diagnosis of FAI syndrome,8 10 30 31 33–35 37 38 40 41 with the remaining four studies including subjects based on a diagnosis of hip pain.30 32 36 39 Methods used for diagnostic inclusion criteria comprised surgical findings,28 clinical examination results8 10 14 30–32 35–41 and radiological findings.31 35 37 38 40 41 Two studies did not specify how FAI syndrome was diagnosed for inclusion33 34 (table 1). One study provided information about level of sports/physical activity,41 and no study provided detail about the duration of symptoms.
Outcomes measured
All included studies used a patient-reported outcome measure (PROM) as the primary outcome measure, but there was large heterogeneity in the PROMs used. The PROMs used included: the IHOT-33, the Copenhagen Hip and Groin Outcome Score (HAGOS), HOOS, the Oxford Hip Score (OHS), the Non-Arthritic Hip Score (NAHS), HOS, the Harris Hip Score (HHS), a pain Visual Analogue Scale (VAS), a Numeric Pain Rating Scale (NPRS), the Hip Sports Activity Scale (HSAS), a Global Rating of Change (GROC) score, the Hospital Anxiety and Depression Scale (HADS), the University of California, Los Angeles (UCLA) activity score, the European Quality of Life-5 Dimensions (EQ-5D) and the 36-item Short Form survey (SF-36) score.
Secondary outcomes measured were mostly measures of physical function, and included: hip muscle strength, trunk muscle strength, standardised hopping tests, measures of performance on a double-leg and single-leg squat, hip range of motion tests, the timed stair climb test and the Y-balance test. The methods used to measure these impairment-based outcomes varied widely between studies. Primary follow-up time points also varied and ranged from 3 weeks30 to 2 years.8 Most studies undertook a 3-month primary follow-up period (table 1).
Physiotherapist-led interventions performed
Seven studies included participants who had not undergone hip surgery,31 32 35 37–40 while three studies examined physiotherapist-led interventions posthip arthroscopy surgery,33 34 36 one study included both postsurgical and non-surgical participants30 and three studies compared physiotherapist-led interventions to hip arthroscopic surgery.7 8 41 The duration of physiotherapist-led interventions ranged from 3 weeks30 to 5 months.34 41
There was a large variety in the types of physiotherapist-led interventions performed. Nine studies included a strengthening programme,7 10 30 34–37 39–41 four studies included stretching/ROM exercises,7 8 10 31 five included ‘core stability’,7 30 38 39 41 eight studies included manual therapy,8 30 33 34 36–38 40 two studies included cardiovascular and return to sport retraining,33 40 two studies included functional retraining39 40 and six studies included neuromotor control exercises7 8 30 36 38 39 (table 1). Five studies did not report the interventions in sufficient detail to allow replication of the interventions.30–32 37 41
There was large heterogeneity in the control/comparator interventions used in the 10 RCTs. Control/comparator interventions used included (i) sham treatments, such as exclusion of pre-operative exercise advice,34 a standardised minimal intervention,40 education only,36 usual care (including medication and continuation of previous exercises)37 and a home-based unsupervised exercise programme38; (ii) no-treatment group33 or waiting-list control group39 and (iii) hip arthroscopy surgery7 8 41 (table 1).
Main findings
Between-group differences were generated for physiotherapist-led interventions compared with the comparator intervention in four studies in patients who had not undergone surgery37–40; in three studies posthip arthroscopy33 34 36 and compared with hip arthroscopic surgery7 8 41 in three studies (table 2).
Table 2.
Summary of results of between-group SMD for primary outcomes of included randomised controlled trials
| Study | Title, journal | Baseline M (SD) PT | Baseline M (SD) control | Primary FU M (SD) PT | Primary FU M (SD) control | Other FU M (SD) PT | Other FU M (SD) control | Did primary FU score reach ? | Proportion of participants with FU score greater than PASS score | PT group change score (primary outcome primary end point) | Control group change score primary outcome primary end point) | Did primary change score reach MIC? | Between-group SMD (95% CI) for primary outcomes (positive SMD favours PT intervention) |
| Studiescomparing physiotherapist-led treatment with sham or control treatment innon-surgical cohorts | |||||||||||||
| Grant, et al 2017 34 | The HAPI ‘Hip Arthroscopy Pre-habilitation Intervention’ study: does prehabilitation affect the outcomes in patients undergoing hip arthroscopy for femoroacetabular impingement? |
NAHS 60 (23.6) | NAHS 54.4 (24.5) | NAHS 56.3 (18.5) | NAHS 48.8 (20.6) | NA | NA | Unknown | NA | Author did not provide data | Author did not provide data | Unknown | NAHS NC |
| Harris-Hayes, et al39 | Movement pattern trainingto improve function in people with chronic hip joint pain: a feasibility randomised clinic trial | HOOS-Pain 78.2 (12.3) HOOS-QOL 65.1 (13.0) |
HOOS-Pain 73.9 (13.8) HOOS-QOL 55.3 (19.2) |
HOOS-Pain 81.5 (13.2) HOOS-QOL 71.3 (18.3) |
HOOS-Pain 75.8 (13.4) HOOS-QOL 63.1 (19.7) |
NA | NA | No No |
5/16 (31%) 4/16 (25%) |
HOOS-Pain 3.3 (9.9) HOOS-QOL 6.2 (10.6) |
HOOS-Pain 1.9 (10.4)) HOOS-QOL 7.8 (11.8) |
No No |
HOOS-Pain 0.13 (−0.53 to 0.80) HOOS-QOL −0.14 (−0.80 to 0.52) |
| Kemp, et al40 | The Physiotherapy for Femoroacetabular Impingement Rehabilitation Study: a pilot randomised controlled trial | IHOT 60 (26) HOOS-QOL 54 (21) |
IHOT 56 (25) HOOS-QOL 50 (17) |
IHOT 87 (12) HOOS-QOL 76 (13) |
IHOT 67 (24) HOOS-QOL 62 (24) |
NA | NA | Yes No |
6/7 (86%) 2/7 (29%) |
IHOT 22 (26) HOOS-QOL 11 (8) |
IHOT 11 (8) HOOS-QOL 12 (8) |
Yes Yes |
IHOT 0.68 (−0.22 to 1.58) HOOS-QOL 0.54 (−0.36 to 1.43) |
| Smeatham, et al 2017 37 | Does treatment by a specialist physiotherapist change pain and function in young adults with symptoms from femoroacetabular impingement? A pilot project for a randomised controlled trial | NAHS Total 50.1 (19.1) | NAHS Total 54.4 (13.3) | NAHS Total 62.2 (16.1) | NAHS Total 55.2 (15.0) | NA | NA | Unknown | NA | NAHS Total 12.7 (19.1) | NAHS Total 1.8 (13.3) | Unknown | NAHS Total 0.64 (−0.09 to 1.38) |
| Wright, et al 2016 38 | Non-operative management of femoroacetabular impingement: a prospective, randomised controlled clinical trial pilot study | HOS-ADL 74.3 (13.1) HOS-Sport 59.4 (18.0) |
HOS-ADL 73.8 (11.3) HOS-Sport 51.4 (16.2) |
HOS-ADL 81.1 (20.3) HOS-Sport 70.0 (29.3) |
HOS-ADL 85.1 (6.0) HOS-Sport 72.4 (15.3) |
NA | NA | No No |
2/8 (25%) 2/8 (25%) |
HOS-ADL 6.4 (13.1) HOS-Sport 10.6 (18) |
HOS-ADL 11.4 (11.3) HOS-Sport 21.0 (16.2) |
No No |
HOS-ADL −0.34 (−1.37 to 0.68) HOS-Sport −0.57 (−1.61 to −0.47) |
| Studiescomparing physiotherapist-led treatment with sham or control treatment in postsurgicalcohorts | |||||||||||||
| Bennell, et al 2017 33 | Efficacy of adding a physiotherapy rehabilitation programme to arthroscopic management of femoroacetabular impingement syndrome: a randomised controlled trial (FAIR) | IHOT-33 40.9 (15.7) HOS-Sport 50.9 (17.1) |
IHOT-33 42.0 (17.5) HOS-Sport 52.1 (16.7) |
IHOT-33 78.8 (17.8) HOS-Sport 83.6 (18.1) |
IHOT-33 66.4 (20.5) HOS-Sport 70.8 (18.6) |
IHOT-33 84.4 (12.1) HOS-Sport 85.0 (17.8) |
IHOT-33 78.1 (16.4) HOS-Sport 86.0 (12.4) |
Yes No |
10/11 (90%) 3/11 (27%) |
IHOT 38.0 (14.0) HOS-Sport 32.7 (18.5) |
IHOT 22.5 (22.3) HOS-Sport 16.7 (24.5) |
Yes No |
IHOT 0.80 (0.05 to 1.55) HOS-Sport 0.71 (−0.03 to 1.45) |
| Kemp, et al 201836 | A pilot randomised clinical trial of physiotherapy (manual therapy, exercise and education) for early onset hip osteoarthritis posthip arthroscopy | HOOS-QOL 49.0 (25.0) IHOT 62.6 (23.7) |
HOOS-QOL 51.0 (15.5) IHOT 58.1 (17.3)) |
HOOS-QOL 51 (23) IHOT 64 (18) |
HOOS-QOL 55 (20) IHOT 57 (23) |
NA | NA | No Yes |
1/9 (11%) 6/9 (67%) |
IHOT-33 7 (23) HOOS-Pain 10(17) |
IHOT-33 −4(24) HOOS-Pain −2(17) |
No No |
IHOT 0.45 (−0.53 to 1.43) HOOS-QOL 0.67 (−0.33 to 1.67) |
| Studies comparing physiotherapist-led treatment with hip arthroscopy surgery | |||||||||||||
| Griffin, et al 2018 7 | Hip arthroscopy vs best conservative care for the treatment of femoroacetabular impingement syndrome (UK FASHIoN): a multicentre randomised controlled trial | IHOT-33 35.6 (18.2) | IHOT-33 39.2 (20.9) | IHOT-33 49.7 (25) | IHOT-33 58.8 (27) | IHOT-33 45.6 (23) | IHOT-33 46.6 (25) | No | 60/162 (37%) | IHOT-33 14.1 (25) | IHOT-33 19.3 (27) | Yes | IHOT-33 −0.21 (−0.43 to 0.01) |
| Mansell, et al 2018 8 | Arthroscopic surgery or physical therapy for patients with femoroacetabular impingement syndrome | HOS-ADL 64.6 (14.2) HOS-Sport 53.2 (16.8) IHOT 29.4 (16.1) |
HOS-ADL 65.6 (15.2) HOS-Sport 52.1 (18.1) IHOT 28.5 (16.1) |
HOS-ADL 73.1 (37.1) HOS-Sport 57.1 (29.7) IHOT 44.9 (29.0) |
HOS-ADL 68.4 (22.3) HOS-Sport 43.4 (29.3) IHOT 51.2 (28.1) |
HOS-ADL 6M 68.4 (18.1) HOS-Sport 6M 53.1 (27.8) IHOT 6M 37.5 (27.7) HOS-ADL 12M 72.5 (27.8) HOS-Sport 12M 52.4 (27.8) IHOT 12M 43.9 (29.3) |
HOS-ADL 6M 68.5 (18.7) HOS-Sport 6M 45.2 (28.3) IHOT 6M 43.8 (27.1) HOS-ADL 12M 67.7 (19.7) HOS-Sport 12M 51.8 (29.7) IHOT 12M 48.9 (29.0) |
No No No |
8/33 (24%) 4/33 (12%) 11/33 (33%) |
HOS-ADL 12.1 (34.0) HOS-Sport 9.1 (47.3) IHOT NR |
HOS-ADL 18.2 (32.9) HOS-Sport 11.3 (45.6) IHOT NR |
Yes No |
HOS-ADL −0.18 (−0.64 to 0.28) HOS-Sport −0.05 (−0.50 to 0.41) IHOT NC |
| Palmer, et al 2019 41 | Arthroscopic hip surgery compared with physiotherapy and activity modification for the treatment of symptomatic femoroacetabular impingement: multicentre randomised controlled trial | HOS-ADL 65.7 (18.9) | HOS-ADL 66.1 (18.5) | HOS-ADL 69.2 (19.1) | HOS-ADL 78.4 (19.9) | NA | NA | No | 6/88 (7%) | HOS-ADL 69.2 (19.1)* | HOS-ADL 78.4 (19.9)* | No | HOS-ADL −0.47 (−0.76 to −0.18) |
*Data reported as follow-up score rather than change score.
ADL, activity of daily living; ER, external rotation; FABER, flexion-abduction-external rotation test; FADIR, flexion-adduction-internal rotation test; FU, follow-up time point; HAGOS, Copenhagen Hip and Groin Outcome Score; HHS, Harris Hip Score; HOOS, hip osteoarthritis disability outcome score; HOS, Hip Outcome Score; HSAS, hip sport and activity score; IHOT, International Hip Outcome Tool; IR, internal rotation; LEFS, lower extremity functional scale; 12M, 12-month follow-up; M, mean SD; 6M, 6-month follow-up; MIC, minimal important change; NA, not applicable; NAHS, Non-Arthritic Hip Score; NC, not calculated (insufficient data); NPRS, Numeric Pain Rating Scale; NR, not reported; PA, physical activity; PASS, Patient Acceptable State Score; PT, physiotherapy/physical therapy; QOL, quality of life; ROM, range of motion; SANE, single assessment numeric evaluation; SMD, standardised mean difference; VAS, Visual Analogue Scale.
Between-group comparisons of physiotherapist-led interventions compared with sham/no treatment in non-surgical patients
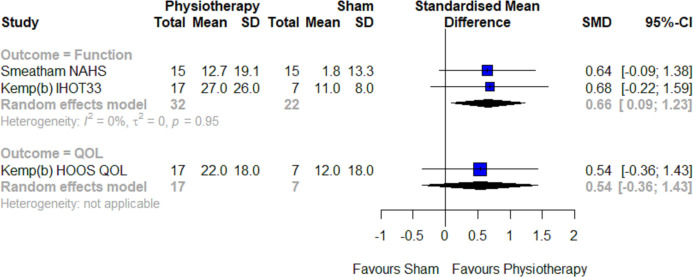
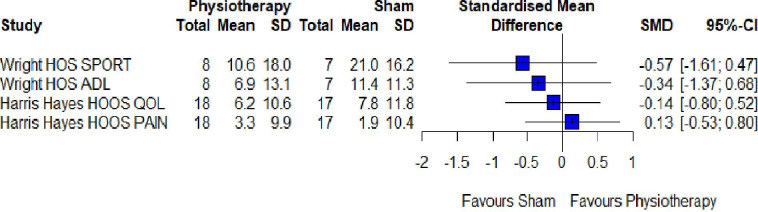
The level of evidence was limited, with two high-quality39 40 and two moderate-quality37 38 pilot RCTs included. In patients with hip pain (non-surgical), physiotherapist-led interventions of 3 months duration that included targeted strengthening programmes showed moderate pooled effects for function (SMD (95% CI): 0.66 (0.09 to 1.23)) favouring the physiotherapist-led intervention group37 40 (figure 2). For physiotherapist-led interventions of shorter duration (6–8 weeks), effects showed no significant differences between groups (figure 3). One study achieved a follow-up score greater than the PASS score, and change score greater than the MIC for the primary outcome.40
Figure 2.
Between-group differences for physiotherapist-led treatment compared with sham/no treatment in non-surgical populations at 3 months follow-up. HOOS, Hip Osteoarthritis and disability Outcome Score; IHOT, International Hip Outcome Tool; QOL, quality of life; SMD, standardised mean difference; total, number of participants.
Figure 3.
Between-group differences for physiotherapist-led treatment compared with sham/no treatment in non-surgical populations at 6 weeks follow-up.ADL, Activity of Daily Living; HOOS, Hip Osteoarthritis and disability Outcome Score; HOS, Hip Outcome Score; QOL, quality of life; SMD, standardised mean difference; total, number of participants.
Between-group comparisons of physiotherapist-led interventions compared with sham/no treatment in post-hip arthroscopy patients
The level of evidence was limited, with two moderate-quality pilot RCTs included.33 36 Data could not be pooled due to heterogeneity in outcomes assessed. Moderate positive effects for patient-reported function (0.67; 95% CI 0.07 to 1.26) were reported in the two RCTs, favouring the physiotherapist-led interventions (figure 4). Both studies achieved a follow-up score greater than the PASS score and change score greater than the MIC for the primary outcome. The proportion of participants undertaking physiotherapist-led interventions achieving a score greater than the PASS score ranged from 11%36 to 90%.33
Figure 4.
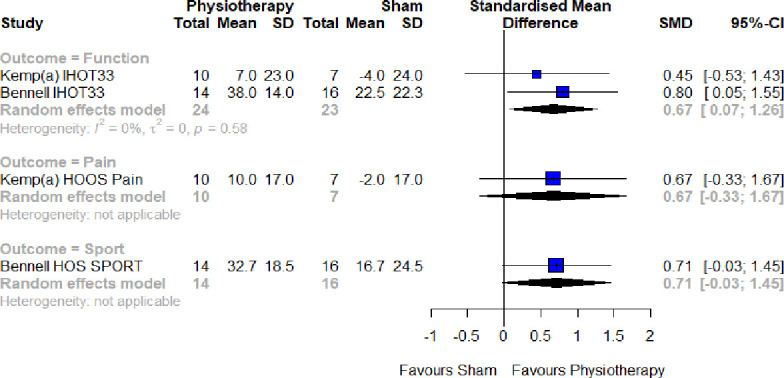
Between-group differences for physiotherapist-led treatment compared with sham/no treatment in posthip arthroscopy populations at 3-month follow-up. HOOS, Hip Osteoarthritis and disability Outcome Score; HOS, Hip Outcome Score; IHOT, International Hip Outcome Tool; SMD, standardised mean difference; total, number of participants.
Between-group comparisons of physiotherapist-led interventions compared with hip arthroscopic treatment
The level of evidence was strong, with two high-quality RCTs8 41 and one moderate-quality RCT7 included (figure 5). In studies comparing physiotherapist-led interventions with hip arthroscopic surgery, at 8–12 months, weak positive pooled effects (−0.32; 95% CI −0.57 to −0.07) favoured hip arthroscopy surgery. At 24 months, there was only one moderate-quality RCT and thus the level of evidence is limited. There was no significant difference between groups (−0.18; 95% CI −0.64 to 0.28). For the physiotherapist-led intervention groups, no studies achieved a follow-up score greater than the PASS score, and only one study had a change score greater than the MIC for the primary outcome.7 The proportion of participants undertaking physiotherapist-led interventions achieving a score greater than the PASS score ranged from 7%41 to 37%.7
Figure 5.
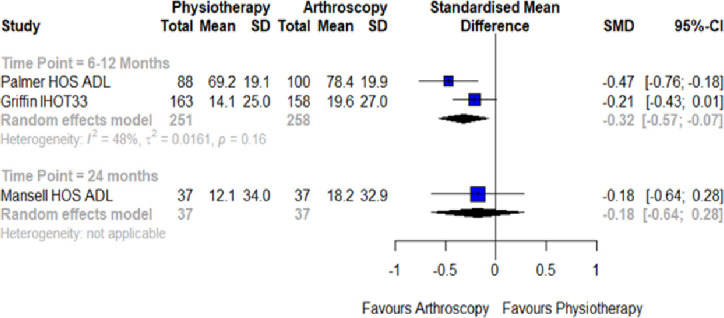
Between-group differences for physiotherapist-led treatment compared with hip arthroscopy surgery. ADL, Activity of Daily Living; HOS, Hip Outcome Score; IHOT, International Hip Outcome Tool; SMD, standardised mean difference; total, number of participants.
Within-group change for patient-reported outcome measures for physiotherapist-led interventions in non-operative patient groups
Within-group effects for physiotherapist-led interventions on PROMS in patients with hip pain were able to be calculated for nine of the included studies7 8 30–32 37–40 (table 3). The level of evidence overall was moderate, with one high-quality RCT and several high-quality pilot RCTs included in the analyses. Positive SPDs ranged from moderate effects for patient-reported function (0.57; 95% CI 0.03 to 1.12)37 following a 3-month intervention, to large positive effects for function (3.85; 95% CI 2.91 to 4.78)31 following a 6-month intervention. Data were not able to be pooled due to heterogeneity between time points and the outcomes measured. The proportion of participants undertaking physiotherapist-led interventions achieving a score greater than the PASS score ranged from 25%38 39 to 86%.40
Table 3.
Summary of results of within-group standardised paired differences for physiotherapist-led treatment in non-operative patients (randomised and non-randomised studies)
| Study | Title | Baseline M (SD) PT | Prim FU M (SD) PT | Within-group SPD (95% CI) for primary outcomes (positive SPD favours postintervention improvement) |
| Randomised studies | ||||
| Grant, et al 2017 34 | The HAPI ‘Hip Arthroscopy Pre-habilitation Intervention’ study: does prehabilitation affect the outcomes in patients undergoing hip arthroscopy for femoroacetabular impingement? |
Abduction strength 16.6 (11.8 Adduction strength 13.4 (4.8) Flexion strength 27.3 (23.1) ER strength 15.3 (5.3) Knee extension strength 37.1 (23.0) |
Abduction strength 20.9 (11.6) Adduction strength 19.3 (9.9) Flexion strength 32.9 (16.6) External rotation strength 19.0 (6.3) Knee extension strength 49.0 (40.2) |
Abduction strength not calculated as follow-up dataset not complete Adduction strength not calculated as follow-up dataset not complete Flexion strength not calculated as follow-up dataset not complete External rotation strength not calculated as follow-up dataset not complete Knee extension strength not calculated as follow-up dataset not complete |
| Griffin, et al 2018 7 | Hip arthroscopy vs best conservative care for the treatment of femoroacetabular impingement syndrome (UK FASHIoN): a multicentre randomised controlled trial | IHOT−33 35.6 (18.2) | IHOT−33 49.7 (25) | IHOT−33 0.63 (0.46 to 0.79) |
| Harris−Hayes, et al 201639 | Movement pattern training to improve function in people with chronic hip joint pain: a feasibility randomised clinic trial | HOOS Symptoms 75.0 (17.0) HOOS−Pain 78.2 (12.3) HOOS−ADL 90.7 (9.9) HOOS−Sport 77.1 (17.5) HOOS−QOL 65.1 (13.0) Abduction strength 6.7 (1.8) ER 0 strength 2.9 (0.9) ER 90 strength 3.4 (0.8) Flexion in single leg squat 67.4 (14.0) Adduction in single leg squat 20.2 (6.6) IR in single leg squat 2.5 (7.7) |
HOOS Symptoms 85.0 (13.6) HOOS−Pain 81.5 (13.2) HOOS−ADL 93.5 (10.9) HOOS SP 84.6 (19.6) HOOS−QOL 71.3 (18.3) Abduction strength 7.2 (2.3) ER 0 strength3.2 (0.8) ER 90 strength 3.9 (0.9) Flexion in single leg squat 61.7 (15.9) Adduction in single leg squat17.6 (5.7) IR in single leg squat 2.7(6.3) |
HOOS Symptoms 0.61 (0.11 to 1.12) HOOS−Pain 0.25 (−0.22 to 0.72) HOOS−ADL 0.26 (−0.21 to 0.73) HOOS SP 0.38 (−0.09 to 0.86) HOOS−QOL 0.36 (−0.11 to 0.84) Abduction strength 0.23 (−0.24 to 0.70) ER 0 strength 0.10 (−0.36 to 0.56) ER 90 strength 0.78 (0.25 to 1.31) Flexion in single leg squat 0.36 (0.11 to 0.84) Adduction in single leg squat 0.40 (−0.08 to 0.88) IR in single leg squat −0.02 (−0.49 to 0.44) |
| Kemp et al, 201840 | The Physiotherapy for Femoroacetabular Impingement Rehabilitation Study: a pilot randomised controlled trial | IHOT 60(26) HOOS−QOL 54(21) Adduction strength 0.85 (0.17) Abduction strength 0.94 (0.23) Extension 0.92 (0.28) ER strength0.48 (0.11) Flexion ROM 109(14) Single leg hop 1.14 (0.26) Side bridge 59(42) |
IHOT 87(12) HOOS−QOL 76(13) Adduction strength 1.1 (0.22) Abduction strength 1.16 (0.23) Extension strength 1.17 (0.32) ER strength 0.57 (0.19) Flexion ROM 123(9) Single leg hop 1.34 (0.32) Side bridge 98(35) |
IHOT 1.14 (0.53 to 1.75) HOOS−QOL 1.14 (0.53 to 1.75) Adduction strength 1.19 (0.57 to 1.81) Abduction strength 0.91 (0.35 to 1.48) Extension strength 0.79 (0.24 to 1.33) ER strength 0.52 (0.01 to 1.03) Flexion ROM 1.08 (0.49 to 1.68) Single leg hop 0.65 (0.12 to 1.17) Side bridge 0.95 (0.38 to 1.53) |
| Mansell, et al 2018 8 | Arthroscopic surgery or physical therapy for patients with femoroacetabular impingement syndrome | HOS−ADL 64.6 (14.2) HOS−Sport 53.2 (16.8) |
HOS−ADL 73.1 (37.1) HOS−Sport 57.1 (29.7) |
HOS−ADL 0.26 (−0.06 to 0.57) HOS−Sport 0.15 (−0.16 to 0.46) |
| Palmer, et al 2019 41 | Arthroscopic hip surgery compared with physiotherapy and activity modification for the treatment of symptomatic femoroacetabular impingement: multicentre randomised controlled trial | Hip Flexion ROM 95.7 (19.1) Hip extension ROM 17.9 (7.9) Hip Abduction ROM 27.5 (11.9) Hip adduction ROM 21.6 (7.9) Hip ER ROM 25.0 (11.8) Hip IR ROM 24.0 (11.2) |
Hip Flexion ROM 99.7 (17.5) Hip extension ROM 15.7 (8.0) Hip Abduction ROM 29.6 (11.7) Hip adduction ROM 23.2 (8.9) Hip ER ROM 27.4 (9.7) Hip IR ROM 28.9 (11.2) |
Hip Flexion ROM not calculated as follow−up dataset not complete Hip extension ROM not calculated as follow−up dataset not complete Hip Abduction ROM not calculated as follow−up dataset not complete Hip adduction ROM not calculated as follow−up dataset not complete Hip ER ROM not calculated as follow−up dataset not complete Hip IR ROM not calculated as follow−up dataset not complete |
| Smeatham, et al 2017 37 | Does treatment by a specialist physiotherapist change pain and function in young adults with symptoms from femoroacetabular impingement? A pilot project for a randomised controlled trial | NAHS Total 50.1 (19.1) HOS−ADL 69 (39) HOS−Sport 51.5 (19.7) |
NAHS Total 62.2 (16.1) HOS−ADL 90 (27) HOS−Sport 68 (21.6) |
NAHS Total 0.64 (0.09 to 1.20) HOS−ADL 0.57 (0.03 to 1.12) HOS−Sport 0.75 (0.18 to 1.33) |
| Wright, et al 2016 38 | Non−operative management of femoroacetabular impingement: a prospective, randomised controlled clinical trial pilot study | HOS−ADL 74.3 (13.1) HOS−Sport 59.4 (18.0) Depth squat 54.1 (12.5) Triple hop 11.4 (5.1) Flexion ROM 100.3 (20.5) Flexion strength 9.9 (4.2) |
HOS−ADL 81.1 (20.3) HOS−Sport 70.0 (29.3) Depth squat 43.1 (15.5) Triple hop 13.3 (5.3) Flexion ROM 122.4 (18.8) Flexion strength 13.2 (4.4) |
HOS−ADL 0.34 (−0.37 to 1.05) HOS−Sport 0.37 (−0.35 to 1.08) Depth squat 0.69 (0.08 to 1.46) Triple hop 0.32 (−0.39 to 1.04) Flexion ROM 1.00 (0.15 to 1.84) Flexion strength 0.68 (−0.08 to 1.45) |
| Non−randomised studies | ||||
| Coppack, et al 2016 30 | Physical and functional outcomes following multidisciplinary residential rehabilitation for prearthritic hip pain among young active UK military personnel | HAGOS Pain 37.7 (20.9) HAGOS Symptoms 45.8 (23.2) HAGOS ADL 32.2 (24.1) HAGOS Sport 51.0 (28.1) HAGOS PA 84.7 (24.9) HAGOS QOL 69.5 (24.0) Y BALANCE 240.5 (26.9) Flexion ROM 110.2 (24.3) IR ROM 25.2 (13.7) |
HAGOS Pain 35.1 (23.7) HAGOS Symptoms 46.3 (24.2) HAGOS ADL 31.0 (24.7) HAGOS Sport 48.5 (28.6) HAGOS PA 77.5 (31.2) HAGOS QOL 64.9 (23.3) Y BALANCE 256.3 (20.8) Flexion ROM 116.7 (23.3) IR ROM 29.8 (12.4) |
HAGOS Pain −0.11 (−0.42 to 0.19) HAGOS Symptoms 0.02 (−0.29 to 0.33) HAGOS ADL −0.05 (−0.36 to 0.26) HAGOS Sport −0.09 (−0.40 to 0.22) HAGOS PA −0.25 (−0.56 to 0.07) HAGOS QOL −0.19 (−0.50 to 0.12) Y BALANCE 0.63 (0.29 to 0.97) Flexion ROM 0.27 (−0.05 to 0.58) IR ROM 0.34 (0.03 to 0.66) |
| Emara, et al 2011 31 | Conservative treatment for mild femoroacetabular impingement | HHS 72(6) NAHS 72(4) VAS 6 (1) Flexion ROM 95.0 (0.4) Extension ROM 4.0 (1.6) Abduction ROM 37.0 (0.4) Adduction ROM 17.0 (7.0) ER in flexion ROM 28.5 (0.5) ER in extension ROM 25.3 (0.3) IR in flexion ROM 9.4 (0.3) IR in extension ROM 15.8 (0.4) |
HHS 91(4) NAHS 90(5) VAS 3 (1) Flexion ROM 88.0 (3.5) Extension ROM 3.7 (2.2) Abduction ROM 36.0 (1.4) Adduction ROM 17.0 (9.0) ER in flexion ROM 28.4 (1.2) ER in extension ROM 24.5 (1.0) IR in flexion ROM 11.3 (0.5) IR in extension ROM 15.7 (0.7) |
HHS 3.52 (2.65 to 4.38) NAHS 3.85 (2.91 to 4.78) VAS 2.94 (2.19 to 3.68) Flexion ROM −2.07 (−2.64 to −1.50) Extension ROM −0.15 (−0.47 to 0.17) Abduction ROM –0.78 (−1.15 to −0.41) Adduction ROM 0.00 (−0.32 to 0.32) ER in flexion ROM −0.09 (−0.41 to 0.23) ER in extension ROM −0.88 (−1.26 to −0.50) IR in flexion ROM 4.27 (3.24 to 5.29) IR in extension ROM −0.16 (−0.48 to 0.16) |
| Guenther, et al 2017 35 | A pre−operative exercise intervention can be safely delivered to people withfemoroacetabular impingement and improve clinical and biomechanical outcomes | HOOS Symptoms 56.1 (13.2) HOOS−Pain 64.1 (12.3) HOOS−ADL 73.0 (14.4) HOOS−Sport 51.7 (12.2) HOOS−QOL 35.3 (17.2) Abduction strength 1.53 (0.35) Adduction strength 1.40 (0.38) Extension strength 1.81 (0.46) Flexion strength 1.89 (0.45) ER strength 0.75 (0.23) IR strength 0.76 (0.36) Timed stair climb test 2.96 (0.66) |
HOOS Symptoms 63.9 (14.6) HOOS−Pain 72.5 (12.3) HOOS−ADL 83.4 (11.0) HOOS−Sport 63.4 (14.0) HOOS−QOL 42.8 (22.0) Abduction strength 1.67 (0.34) Adduction strength 1.53 (0.39) Extension strength 1.93 (0.50) Flexion strength 2.04 (0.43) ER strength 0.77 (0.18) IR strength 0.89 (0.36) Timed stair climb test 2.61 (0.46) |
HOOS Symptoms HOOS−Pain HOOS−ADL HOOS−Sport HOOS−QOL Abduction strength 0.39 (−0.07 to 0.84) Adduction strength 0.32 (−0.13 to 0.77) Extension strength 0.24 (−0.21 to 0.68) Flexion strength 0.33 (−0.12 to 0.78) ER strength 0.09 (−0.35 to 0.53) IR strength0.35 (−0.10 to 0.80) Timed stair climb test 0.57 (0.10 to 1.05) |
| Hunt, et al 2012 32 | Clinical outcomes analysis of conservative and surgical treatment of patients with clinical indications of pre−arthritic, intra−articular hip disorders | HHS 61.3±13 WOMAC 29.2±16 NAHS 63.2±14 |
HHS 78.9±14 WOMAC 13.5±14 NAHS 81.6±12 |
HHS 1.26 (0.76 to 1.77) WOMAC 1.01 (0.54 to 1.47) NAHS 1.36 (0.84 to 1.89) |
ADL, activity of daily living; ER, external rotation; FU, follow-up time point; HAGOS, Copenhagen Hip and Groin Outcome Score; HHS, Harris Hip Score; HOOS, Hip Osteoarthritis and disability Outcome Score; IR, internal rotation; M, mean SD; MCS, emotional function subscale; NAHS, Non-Arthritic Hip Score; NPRS, Numeric Pain Rating Scale; NR, not reported; PA, physical activity; PCS, physical function subscale; PT, physiotherapy/physical therapy; QOL, quality of life; ROM, range of motion; SF-12, Short Form-12 Questionnaire; SMD, standardised mean difference; VAS, Visual Analogue Scale.
Within-group change for physical impairments for physiotherapist-led interventions in non-operative patient groups
Nine studies reported the effects of physiotherapist-led interventions on physical impairments on people with hip pain30 31 34 35 37–41 (table 3), with SPDs able to be calculated for seven of the nine studies. The level of evidence was limited, with no high-quality, full-scale RCTs included in any of the analyses relating to physical impairments. The impairment measures included hip range of motion,30 31 38 40 hip muscle strength,35 38–40 depth of squat,38 balance,30 trunk endurance,40 control during single leg squat39 and hopping performance.38 40 Data were not able to be pooled for within-group change in physical impairment measures, due to heterogeneity between time points and the methods by which outcomes were measured.
For hip flexion range of motion, SPDs varied, and ranged from large negative changes (2.07, 95% CI –2.64 to −1.50) following a 6-month intervention consisting of rest, stretching and activity modification31 to large positive change (1.08, 95% CI 0.49 to 1.68) following a 3-month intervention comprising strengthening exercise, manual therapy and education.40
Hip muscle strength was recorded in four studies,35 38–40 and SPDs ranged from weak, non-significant effects (0.09,–0.35 to 0.53) for an 10 week intervention comprising progressive strengthening exercises,35 to large positive SMDs (1.19, 0.57 to 1.81) for a 12 week intervention comprising targeted strengthening and functional retraining exercises.40
There were varied within-group changes in functional task performance. Positive SPDs ranged from moderate improvements in the timed stair climb test (0.57, 95% CI 0.10 to 1.05),35 single-leg hop test (0.65, 95% CI 0.12 to 1.17)40 and Y-balance test (0.63, 95% CI 0.29 to 0.97)30 with movement retraining and functional exercise programmes, to large improvements for trunk endurance (0.95, 95% CI 0.38 to 1.53) following a 3-month targeted trunk-strengthening programme.40
Discussion
Our systematic review evaluated the effectiveness of physiotherapist-led interventions to improve pain and function in young and middle-aged adults experiencing hip-related pain, including those with FAI syndrome. The 14 studies included 7 pilot and 3 full-scale RCTs, and demonstrated considerable variability in the risk of bias, the outcomes reported and the interventions performed, which limited opportunities for meta-analysis. Included studies had poor transparency in reporting of interventions, inconsistency in PROMs and methods used to measure physical impairments.
Our findings suggest that in people with hip pain, physiotherapist-led interventions may improve function and strength, however the effects on pain and QOL were unclear. There was limited evidence that interventions with targeted strengthening exercise programmes that were at least 3 months duration might have the best effect. Hip arthroscopy surgery had a small positive benefit compared with a physiotherapist-led intervention at 8–12 months. At 24 months, the level of evidence was limited indicating no difference between the hip arthroscopy surgery and physiotherapist-led interventions. Very few of the physiotherapist-led interventions in this review achieved follow-up and change scores that surpassed previously published PASS and MIC scores.
Physiotherapist-led interventions for those who had and had not undergone hip arthroscopy surgery for hip pain primarily comprised exercise therapy, where the types of exercise described included strength training, movement pattern retraining, range of motion exercises and stretching. However, specific details of the programmes were rarely well described. The moderate effect observed for these interventions were hampered by small sample sizes and require full-scale RCTs to confirm findings. Extending the outcome measurement beyond the 3-month mark would determine whether improvements seen would be maintained in the medium-term to long-term. A recent consensus meeting reported considerable discord in the type, duration, intensity and modality of posthip arthroscopy rehabilitation provided by physiotherapists.42 The consensus group suggested that full-scale RCTs are required in order to gain clarification on the composition of optimal postarthroscopic rehabilitation programmes.42
Physiotherapist-led intervention was inferior to hip arthroscopy surgery with small between-groups differences at 12-month follow-up.7 8 41 Not surprisingly, despite the small difference favouring surgery, physiotherapy was far more cost-effective (£155 for physiotherapist-led treatment compared with £2372 for hip arthroscopy).7 Arthroscopic surgery could be recommended as a second-line treatment for patients who have not responded adequately to a physiotherapist-led treatment programme.42 However, the mean effects beyond that of physiotherapy were weak and may not be clinically meaningful. The within-group improvements for the physiotherapist-led interventions in these studies were modest, with only one study achieving the PASS, and they may not represent optimal treatment.18 Further studies might shed more light on the relative effectiveness of surgery and physiotherapy particularly in the medium-term and long-term.43
Multimodal, physiotherapist-led interventions,7 8 30 33 34 36–38 40 including exercise therapy combined with manual therapy, medication, activity modification, advice and education, were most commonly studied. Manual therapy is effective when combined with exercise for hip OA,44 45 but there is debate whether contemporary physiotherapist-led interventions for musculoskeletal pain should include multimodal treatment additions such as manual therapy.42 Further studies are required to confirm whether additional treatment elements, such as manual therapy, impart a greater benefit than exercise-therapy alone for young and middle-aged adults with hip pain.
Physiotherapist-led interventions on physical impairments had variable effects. For hip range of motion, the largest positive effects pre-physiotherapist-led to post-physiotherapist-led treatment were seen following a 3-month intervention strengthening exercise, manual therapy and education.40 The greatest hip muscle strength gain was seen with a strengthening exercise programme of 3 months duration,40 and largest in hip adductor muscles. Greater hip adductor strength following hip arthroscopy is associated with better hip-related QOL,46 suggesting that it may be an important target. However, this was a pilot study, and the most effective type, dose and progression of exercise is unknown. The American College of Sports Medicine47 guidelines for exercise prescription contain information about the dosage, volume and progression of exercises that may be useful for clinicians and researchers when developing strength programmes for patients with hip pain. In studies measuring changes in functional task performance, had positive effects30 35 40 with movement retraining and functional exercise programmes. These programmes may improve patient self-efficacy as well as increase the capacity for load, thus enabling participation in more challenging activity. Larger, future studies including evaluating the potential of effect mediators and moderators may provide insight into the most effective physiotherapist-led interventions to improve physical impairments.
Returning to pre-injury sport and activity is important to young and middle-aged people with hip pain, and often the reason they seek surgical and/or non-surgical treatment.10 48 However, only two studies in this review had a specific return to sport/return to physical activity component within the physiotherapist-led intervention.33 40 Only 17% of people returned to optimal performance and full sports participation at 33±16 months following hip arthroscopy.48 Given the importance of returning to sport in this active patient group and the disappointing rates of returning to optimal performance reported,48 future studies should incorporate key functional and sporting components.49 These could include: valid and consistent definitions of what comprises a successful return to sport and return to activity50; fully powered RCTs that include a specific, targeted return to sport programme throughout the duration of the intervention50 and inclusion of return to sport outcomes as a continuum.40 Until physiotherapist-led interventions include high-quality return to sport elements, outcomes are unlikely to improve beyond those reported by Ishoi et al.48
Transparency and reproducibility are critical when reporting the efficacy of clinical interventions. Guidelines such as the Consensus on Exercise Reporting Template51 and Template for Intervention Description and Replication checklist52 should be used in all trials reporting interventions to ensure adequate transparency and reproducibility. In addition, describing targeted strengthening interventions should use detailed procedures such as those described by Toigo and Boutellier.53 The documentation of adherence to exercise programmes is also critical. Such guidelines allow researchers to evaluate interventions and clinicians to reproduce efficacious interventions in clinical practice. Very few studies used these guidelines to report interventions in the current review. As such, it was not possible to pool findings to complete a meta-analysis, limiting the scope of the review. We recommend that future studies report physiotherapist-led interventions using guidelines such as those described above to maximise transparency and utility of study findings by researchers and clinicians alike.
This review contains several limitations that should be acknowledged. First, the methodological quality of the studies was variable, with only 4/14 (29%) studies considered to have a low risk of bias. In the studies with a higher risk of bias, inflated effect sizes are possible, raising questions about the strength of the findings of these studies. Second, most of the included RCTs were pilot studies and as such were underpowered to detect statistically significant differences between groups. In addition, as there were no fully powered studies comparing physiotherapist-led interventions with sham interventions, adequately powered studies that undertake a head-to-head comparison of physiotherapist-led interventions are required to determine the optimal management strategies for hip pain in young and middle-aged adults. Furthermore, the terminology used to describe hip disorders is not clear, and the populations that were included in this review may be heterogenous. The recent Zurich consensus statement on hip-related pain has provided some guidance in classifying hip disorders as FAI syndrome, acetabular dysplasia and ‘other’.9 At present, there are not enough studies published to be able to analyse data separately for each of these three classifications. However, as the field evolves, this may be an approach that is appropriate for future reviews. As with all reviews of intervention studies, publication bias may have existed where studies with negative findings were not published. We also excluded studies not written in English, which may have led to inclusion bias. Finally, the PROMs and physical impairment-based outcome measures used in the studies were inconsistent, which limited the pooling of data. A recent consensus54 determined that the HAGOS and IHOT were the most appropriate PROM for use in young and middle-aged people with hip pain, and future studies using these measures may make stratification and pooling of data based on these measures in future reviews possible. Furthermore, it is not yet clear what is considered an acceptable level of improvement in a patient’s condition. We compared the findings of our review to previously published PASS and MIC scores, to provide some context to clinical relevance of the effects reported. We acknowledge that the previously published PASS and MIC scores were determined in studies of posthip arthroscopy and posthip arthroplasty patients. It is not known what constitutes a PASS and MIC in non-surgical cohorts of people with hip-related pain. The inclusion of PASS questions at specific time points in future studies may help determine whether patients are gaining acceptable improvement when undergoing physiotherapist-led interventions.
Conclusion
There were no full-scale RCTs comparing physiotherapist-led interventions with other non-surgical treatments or sham treatments. The risk of bias in included studies, as well as limitations in included study methodology should be considered in the interpretation of the results of this systematic review. Physiotherapist-led interventions may improve pain and function in young and middle-aged adults experiencing hip pain, including those with FAI syndrome. There was limited evidence of larger effects for interventions that included targeted strengthening exercise programmes and were of 3 months duration. Hip arthroscopy surgery had a weak positive effect compared with a physiotherapist-led intervention at 8–12 months. Future full-scale RCTs undertaking a head-to-head comparison of physiotherapist-led interventions for hip pain are required.
Summary box.
What is already known?
Hip-related pain is common in young, active adults.
Non-surgical treatments such as physiotherapist-led treatments should be first-line treatment for musculoskeletal conditions including hip-related pain, but effectiveness of these treatments is unclear.
What are the new findings?
There is a paucity of literature in this field.
Physiotherapist-led interventions improve function and strength.
Effects of physiotherapist-led interventions on pain and quality of life are uncertain.
Targeted strengthening exercise programmes and at least 3-month duration might have the best effect.
Hip arthroscopy surgery had a small positive benefit compared with a physiotherapist-led intervention at 8–12 months.
At 24 months, there was limited evidence suggesting no difference between groups.
Footnotes
Twitter: @JoanneLKemp, @AndreaBMosler, @MarkScholes85, @ASemciw
Correction notice: This article has been corrected since it published Online First. An ORCID ID has been added for author Steven Chang.
Contributors: JK, AMB, KMC developed the research question and concept. JK and SC performed the search. JK, HH, MB, MJS performed risk of bias assessment. JK and AMB performed data extraction. JK and AIS performed data analyses. All authors contributed to drafting of manuscript.
Funding: JK is supported by an NHMRC (Australia) ECF 1119971.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: Institutional ethical approval was not required as no data were collected on humans or animals in this review.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data extracted are shared at Figshare (https://figshare.com/s/d18bcb066f1de48861cf).
References
- 1. Vos T, Flaxman AD, Naghavi M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the global burden of disease study 2010. Lancet 2012;380:2163–96. 10.1016/S0140-6736(12)61729-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Werner J, Hägglund M, Waldén M, et al. UEFA injury study: a prospective study of hip and groin injuries in professional football over seven consecutive seasons. Br J Sports Med 2009;43:1036–40. 10.1136/bjsm.2009.066944 [DOI] [PubMed] [Google Scholar]
- 3. Werner J, Hägglund M, Ekstrand J, et al. Hip and groin time-loss injuries decreased slightly but injury burden remained constant in men's professional football: the 15-year prospective UEFA elite Club injury study. Br J Sports Med 2019;53:539-546. 10.1136/bjsports-2017-097796 [DOI] [PubMed] [Google Scholar]
- 4. Mosler AB, Weir A, Eirale C, et al. Epidemiology of time loss groin injuries in a men's professional football League: a 2-year prospective study of 17 clubs and 606 players. Br J Sports Med 2018;52:292–7. 10.1136/bjsports-2016-097277 [DOI] [PubMed] [Google Scholar]
- 5. Kierkegaard S, Langeskov-Christensen M, Lund B, et al. Pain, activities of daily living and sport function at different time points after hip arthroscopy in patients with femoroacetabular impingement: a systematic review with meta-analysis. Br J Sports Med 2017;51:572–9. 10.1136/bjsports-2016-096618 [DOI] [PubMed] [Google Scholar]
- 6. Thorborg K, Kraemer O, Madsen AD, et al. Patient-Reported outcomes within the first year after hip arthroscopy and rehabilitation for femoroacetabular impingement and/or Labral injury: the difference between getting better and getting back to normal. Am J Sports Med 2018;363546518786971. [DOI] [PubMed] [Google Scholar]
- 7. Griffin DR, Dickenson EJ, Wall PDH, et al. Hip arthroscopy versus best conservative care for the treatment of femoroacetabular impingement syndrome (UK fashion): a multicentre randomised controlled trial. Lancet 2018;391:2225–35. 10.1016/S0140-6736(18)31202-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mansell NS, Rhon DI, Meyer J, et al. Arthroscopic surgery or physical therapy for patients with femoroacetabular impingement syndrome: a randomized controlled trial with 2-year follow-up. Am J Sports Med 2018;46:1306–14. 10.1177/0363546517751912 [DOI] [PubMed] [Google Scholar]
- 9. Reiman MP, Agricola R, Kemp JL, et al. Consensus recommendations on the classification, definition and diagnostic criteria of hip-related pain in young and middle-aged active adults from the International Hip-related pain research network, Zurich 2018. British Journal of Sports Medicine 2019. [DOI] [PubMed] [Google Scholar]
- 10. Griffin DR, Dickenson EJ, O'Donnell J, et al. The Warwick agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med 2016;50:1169–76. 10.1136/bjsports-2016-096743 [DOI] [PubMed] [Google Scholar]
- 11. Mascarenhas VV, Rego P, Dantas P, et al. Imaging prevalence of femoroacetabular impingement in symptomatic patients, athletes, and asymptomatic individuals: a systematic review. Eur J Radiol 2016;85:73–95. 10.1016/j.ejrad.2015.10.016 [DOI] [PubMed] [Google Scholar]
- 12. Ganz R, Parvizi J, Beck M, et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 2003;417:112–20. 10.1097/01.blo.0000096804.78689.c2 [DOI] [PubMed] [Google Scholar]
- 13. Agricola R, Waarsing JH, Arden NK, et al. Cam impingement of the hip: a risk factor for hip osteoarthritis. Nat Rev Rheumatol 2013;9:630–4. 10.1038/nrrheum.2013.114 [DOI] [PubMed] [Google Scholar]
- 14. Kemp JL, Makdissi M, Schache AG, et al. Hip chondropathy at arthroscopy: prevalence and relationship to labral pathology, femoroacetabular impingement and patient-reported outcomes. Br J Sports Med 2014;48:1102–7. 10.1136/bjsports-2013-093312 [DOI] [PubMed] [Google Scholar]
- 15. McAlindon TE, Bannuru RR, Sullivan MC, et al. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage 2014;22:363–88. 10.1016/j.joca.2014.01.003 [DOI] [PubMed] [Google Scholar]
- 16. Fernandes L, Hagen KB, Bijlsma JWJ, et al. EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis. Ann Rheum Dis 2013;72:1125–35. 10.1136/annrheumdis-2012-202745 [DOI] [PubMed] [Google Scholar]
- 17. Koes BW, van Tulder M, Lin C-WC, et al. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J 2010;19:2075–94. 10.1007/s00586-010-1502-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kemp JL, King MG, Barton C, et al. Is exercise therapy for femoroacetabular impingement in or out of fashion? we need to talk about current best practice for the non-surgical management of FAI syndrome. Br J Sports Med 2019;53:1205 10.1136/bjsports-2018-100173 [DOI] [PubMed] [Google Scholar]
- 19. Portney L, Watkins M. Foundations of Clinical Research - Applications to Clinical Practice. 3rd ed Upper Saddle River, New Jersey: Pearson Education, 2009. [Google Scholar]
- 20. van Tulder M, Furlan A, Bombardier C, et al. Updated method guidelines for systematic reviews in the Cochrane collaboration back review group. Spine 2003;28:1290–9. 10.1097/01.BRS.0000065484.95996.AF [DOI] [PubMed] [Google Scholar]
- 21. Wallis JA, Webster KE, Levinger P, et al. What proportion of people with hip and knee osteoarthritis meet physical activity guidelines? A systematic review and meta-analysis. Osteoarthritis Cartilage 2013;21:1648–59. 10.1016/j.joca.2013.08.003 [DOI] [PubMed] [Google Scholar]
- 22. Paulsen A, Roos EM, Pedersen AB, et al. Minimal clinically important improvement (MCII) and patient-acceptable symptom state (pass) in total hip arthroplasty (THA) patients 1 year postoperatively. Acta Orthop 2014;85:39–48. 10.3109/17453674.2013.867782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Maxwell S, Pergaminelis N, Renouf J, et al. Identification of a patient acceptable symptomatic state score for the International hip outcome tool in people undergoing hip arthroscopy. Arthroscopy 2018;34:3024–9. 10.1016/j.arthro.2018.06.049 [DOI] [PubMed] [Google Scholar]
- 24. Chahal J, Thiel GSV, Mather RC, et al. The minimal clinical important difference (MCID) and patient acceptable symptomatic state (pass) for the modified Harris hip score and hip outcome score among patients undergoing surgical treatment for femoroacetabular impingement. Orthop J Sports Med 2014;2:2325967114S0010 10.1177/2325967114S00105 [DOI] [PubMed] [Google Scholar]
- 25. Kemp JL, Collins NJ, Roos EM, et al. Psychometric properties of patient-reported outcome measures for hip arthroscopic surgery. Am J Sports Med 2013;41:2065–73. 10.1177/0363546513494173 [DOI] [PubMed] [Google Scholar]
- 26. Wan X, Wang W, Liu J, et al. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 2014;14:135. 10.1186/1471-2288-14-135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Dang TM, Peters MJ, Hickey B, et al. Efficacy of flattening-filter-free beam in stereotactic body radiation therapy planning and treatment: a systematic review with meta-analysis. J Med Imaging Radiat Oncol 2017;61:379–87. 10.1111/1754-9485.12583 [DOI] [PubMed] [Google Scholar]
- 28. Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed Hillsdale, N.J: Lawrence Erlbaum Associates, 1988. [Google Scholar]
- 29. Landis JR, Koch GG. Agreement methods for categorical data. Biometrics 1977;33:159–74. [PubMed] [Google Scholar]
- 30. Coppack RJ, Bilzon JL, Wills AK, et al. Physical and functional outcomes following multidisciplinary residential rehabilitation for prearthritic hip pain among young active UK military personnel. BMJ Open Sport Exerc Med 2016;2:e000107. 10.1136/bmjsem-2015-000107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Emara K, Samir W, Motasem ELH, et al. Conservative treatment for mild femoroacetabular impingement. Journal of Orthopaedic Surgery 2011;19:41–5. 10.1177/230949901101900109 [DOI] [PubMed] [Google Scholar]
- 32. Hunt D, Prather H, Harris-Hayes M, et al. Clinical outcomes analysis of conservative and surgical treatment of patients with clinical indications of Prearthritic, intra-articular hip disorders. PM&R 2012;4:479–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bennell KL, Spiers L, Takla A, et al. Efficacy of adding a physiotherapy rehabilitation programme to arthroscopic management of femoroacetabular impingement syndrome: a randomised controlled trial (fair). BMJ Open 2017;7:e014658 10.1136/bmjopen-2016-014658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Grant LF, Cooper DJ, Conroy JL. The HAPI ‘Hip Arthroscopy Pre-habilitation Intervention’ study: does pre-habilitation affect outcomes in patients undergoing hip arthroscopy for femoro-acetabular impingement? J Hip Preserv Surg 2017;50:hnw046–92. 10.1093/jhps/hnw046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Guenther JR, Cochrane CK, Crossley KM, et al. A pre-operative exercise intervention can be safely delivered to people with femoroacetabular impingement and improve clinical and biomechanical outcomes. Physiotherapy Canada 2017;69:204–11. 10.3138/ptc.2016-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kemp J, Moore K, Fransen M, et al. A pilot randomised clinical trial of physiotherapy (manual therapy, exercise, and education) for early-onset hip osteoarthritis post-hip arthroscopy. Pilot and Feasibility Studies 2018;4 10.1186/s40814-017-0157-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Smeatham A, Powell R, Moore S, et al. Does treatment by a specialist physiotherapist change pain and function in young adults with symptoms from femoroacetabular impingement? A pilot project for a randomised controlled trial. Physiotherapy 2017;103:201–7. 10.1016/j.physio.2016.02.004 [DOI] [PubMed] [Google Scholar]
- 38. Wright AA, Hegedus EJ, Taylor JB, et al. Non-Operative management of femoroacetabular impingement: a prospective, randomized controlled clinical trial pilot study. J Sci Med Sport 2016;19:716–21. 10.1016/j.jsams.2015.11.008 [DOI] [PubMed] [Google Scholar]
- 39. Harris-Hayes M, Czuppon S, Van Dillen LR, et al. Movement-Pattern training to improve function in people with chronic hip joint pain: a feasibility randomized clinical trial. J Orthop Sports Phys Ther 2016;46:452–61. 10.2519/jospt.2016.6279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kemp JL, Coburn SL, Jones DM, et al. The physiotherapy for femoroacetabular impingement rehabilitation study (physioFIRST): a pilot randomized controlled trial. J Orthop Sports Phys Ther 2018;48:307–15. 10.2519/jospt.2018.7941 [DOI] [PubMed] [Google Scholar]
- 41. Palmer AJR, Ayyar Gupta V, Fernquest S, et al. Arthroscopic hip surgery compared with physiotherapy and activity modification for the treatment of symptomatic femoroacetabular impingement: multicentre randomised controlled trial. BMJ 2019;9:l185 10.1136/bmj.l185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Kemp JL, Risberg MA, Mosler A, et al. Physiotherapist-led treatment for young to middle-aged active adults with hip-related pain: consensus recommendations from the International Hip-related pain research network, Zurich 2018. Br J Sports Med 2020;54:504–11. 10.1136/bjsports-2019-101458 [DOI] [PubMed] [Google Scholar]
- 43. Risberg MA, Ageberg E, Nilstad A, et al. Arthroscopic surgical procedures versus sham surgery for patients with femoroacetabular impingement and/or Labral tears: study protocol for a randomized controlled trial (HIPARTI) and a prospective cohort study (HARP). J Orthop Sports Phys Ther 2018;48:325–35. 10.2519/jospt.2018.7931 [DOI] [PubMed] [Google Scholar]
- 44. Beumer L, Wong J, Warden SJ, et al. Effects of exercise and manual therapy on pain associated with hip osteoarthritis: a systematic review and meta-analysis. Br J Sports Med 2016;50:458–63. 10.1136/bjsports-2015-095255 [DOI] [PubMed] [Google Scholar]
- 45. Abbott JH, Wilson R, Pinto D, et al. Incremental clinical effectiveness and cost effectiveness of providing supervised physiotherapy in addition to usual medical care in patients with osteoarthritis of the hip or knee: 2-year results of the moa randomised controlled trial. Osteoarthritis and Cartilage 2019;27:424–34. 10.1016/j.joca.2018.12.004 [DOI] [PubMed] [Google Scholar]
- 46. Kemp JL, Makdissi M, Schache AG, et al. Is quality of life following hip arthroscopy in patients with chondrolabral pathology associated with impairments in hip strength or range of motion? Knee Surgery, Sports Traumatology. Arthroscopy 2015:1–7. [DOI] [PubMed] [Google Scholar]
- 47. ACoS M. ACSM's guidelines for exercise testing and prescription. 10th ed Philadelphia, PA: Wolters Kluwer/Lippincott Williams & Wilkins, 2017. [Google Scholar]
- 48. Ishoi L, Thorborg K, Kraemer O, et al. Return to sport and performance after hip arthroscopy for femoroacetabular impingement in 18- to 30-year-old athletes: a cross-sectional cohort study of 189 athletes. Am J Sports Med 2018;363546518789070. [DOI] [PubMed] [Google Scholar]
- 49. Mosler AB, Kemp J, King M, et al. Standardised measurement of physical capacity in young and middle-aged active adults with hip-related pain: recommendations from the first international Hip-related pain research network (IHiPRN) meeting, Zurich, 2018. Br J Sports Med 2019:bjsports-2019-101457 10.1136/bjsports-2019-101457 [DOI] [PubMed] [Google Scholar]
- 50. Ardern CL, Glasgow P, Schneiders A, et al. 2016 consensus statement on return to sport from the first world Congress in sports physical therapy, Bern. Br J Sports Med 2016;50:853–64. 10.1136/bjsports-2016-096278 [DOI] [PubMed] [Google Scholar]
- 51. Slade SC, Dionne CE, Underwood M, et al. Consensus on exercise reporting template (CERT): explanation and elaboration statement. Br J Sports Med 2016;50:1428–37. 10.1136/bjsports-2016-096651 [DOI] [PubMed] [Google Scholar]
- 52. Hoffmann TC, Glasziou PP, Boutron I, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014;348:g1687. 10.1136/bmj.g1687 [DOI] [PubMed] [Google Scholar]
- 53. Toigo M, Boutellier U. New fundamental resistance exercise determinants of molecular and cellular muscle adaptations. Eur J Appl Physiol 2006;97:643–63. 10.1007/s00421-006-0238-1 [DOI] [PubMed] [Google Scholar]
- 54. Impellizzeri FM, Jones DM, Griffin D, et al. Patient-Reported outcome measures for hip-related pain: a review of the available evidence and a consensus statement from the International Hip-related pain research network, Zurich 2018. Br J Sports Med 2020:bjsports-2019-101456. 10.1136/bjsports-2019-101456 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bjsports-2019-101690supp001.pdf (131.1KB, pdf)
bjsports-2019-101690supp002.pdf (41.4KB, pdf)
bjsports-2019-101690supp003.pdf (47KB, pdf)